Back to Journals » Advances in Medical Education and Practice » Volume 11
Expanding Medical Education for Local Health Promoters Among Remote Communities of the Peruvian Amazon: An Exploratory Study of an Innovative Program Model
Authors Ebbs D, Hirschbaum JH , Mika A, Matsushita SC, Lewis JH
Received 10 January 2020
Accepted for publication 2 March 2020
Published 19 March 2020 Volume 2020:11 Pages 215—223
DOI https://doi.org/10.2147/AMEP.S245491
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Balakrishnan Nair
Daniel Ebbs,1 Julian H Hirschbaum,2 Amanda Mika,3 Starr C Matsushita,4 Joy H Lewis5
1Resident Physician Valley Children’s Hospital, Madera, CA, USA; 2Resident Physician Los Angeles County USC Medical Center, Los Angeles, CA, USA; 3Resident Physician Saint Joseph Hospital, Denver, CO, USA; 4Resident Physician Samaritan Health Services, Corvalis, OR, USA; 5Still University, Mesa, AZ, USA
Correspondence: Daniel Ebbs
Resident Physician Valley Children’s Hospital, 9300 Valley Childrens Place, Madera, CA 93636, USA
Tel +1-559-353-3000
Email [email protected]
Purpose: Community health workers (CHWs) play integral roles in primary health care provision in low- and middle-income countries (LMICs). This is particularly true in underdeveloped areas where there are acute shortages of health workers. In this study, we evaluated the development and community utilization of a CHW training program in the Loreto province of Peru. Additionally, a community-oriented training model was designed to augment access to basic health information in underserved and isolated areas of the Amazon.
Methods: Health resource utilization was compared in each community by surveying community members before and after implementation of the CHW training program, which utilized a community participatory program development (CPPD) model.
Results: All communities demonstrated significantly increased CHW utilization (p = 0.026) as their initial point of contact for immediate health concerns following CHW training implementation. This increase in CHW utilization was accompanied by trends toward decreased preferences for local shamans or traveling to the closest health post as the initial health resource.
Conclusion: The community-focused, technology-oriented model utilized in this study proved an effective way to promote the use of CHWs in the Amazon region of Loreto, and could prove valuable to CHW capacitation efforts within other Peruvian provinces and in other LMICs around the world.
Keywords: community health worker, promotores, human resources for health, mobile health technology, expanding access to healthcare, rural health
Introduction
Infrastructure, health technologies, and human resources for health (HRH) are primarily concentrated in urban centers, while people living in poorer and more rural areas tend to have less access to health care, despite their greater need.1 This phenomenon, referred to as the “human resources for health” crisis, can result in excess rates of mortality occurring at home, before a health facility can be reached.2 One approach being employed to combat this issue is the implementation of community health worker (CHW) training programs. CHWs, also known as community health promoters, lay health workers, or promotores, are representatives of their communities who are elected and trained to provide basic healthcare services and to establish important connections between communities and local formal health and social services systems.3,4 Programs often include community education to reduce health risks, promote healthy behaviors, and establish deeper connections between community members and health facilities such as rural health clinics or health posts.3
CHWs play an integral role in the delivery of essential health services, particularly in remote and rural areas of low- and middle-income countries (LMICs). Their scope of practice has included malaria diagnosis and treatment, recognition of emergency warning signs in children, and basic health education regarding disease prevention, such instruction on building proper latrines.1,3 Many studies have shown that creating, augmenting, and sustaining networks of CHWs in underserved communities leads to improved health outcomes, including in diabetes and asthma control across a variety of parameters.5,6 CHWs have also been found to facilitate measures in reducing mortality in children due to pneumonia and improving quality of and access to HIV services.7,8
Loreto, the northernmost province of Peru, is an example of both a rural province in a middle-income country and an HRH crisis zone. Loreto is one of Peru’s most sparsely populated regions as well as one of its most geographically isolated.9,10 Approximately 45% of its inhabitants live in Iquitos, the provincial capital, while the remaining 55% live in small and often remote river-edge communities along the Amazon.9 Notably, in a 2014 study examining characteristics of healthcare access in remote rural areas of Loreto, 38.5% of respondents reported never having consulted a doctor. Moreover, 57% reported not being able to seek medical attention when necessary, secondary to financial and geographic barriers.9 In addition, Loreto had the highest overall recorded prevalence and incidence of Dengue and Malaria in Peru between 2001 and 2016.11
Beginning in the 1990s, there have been significant efforts to establish effective CHW programs in the province of Loreto. Indeed, during this period, the Regional Branch of the Health Ministry (DIRESA, Dirección Regional de Salud) registered more than 1900 CHWs and skilled birth attendants within Loreto alone. However, despite their availability, complicating issues preventing widespread utilization of these health workers remained. In particular, there was a lack of skill unification because CHW capacitation programs did not employ comprehensive training. Certain health workers were trained in family planning, others in the diagnosis and treatment of several specific diseases, and others in health education. In addition, previous training programs were fragmented, with little to no follow-up, ongoing training, or medical supplies provided. This ultimately rendered previously appointed health workers unequipped to proceed with their respective health duties.12
Many CHW programs, in general, fail to provide ongoing support, which is recognized as one of the most important aspects of program growth and sustainability.3 Complicating matters further, hundreds of charity-oriented foreign medical organizations with varying missions have resulted in decreased reliance on domestic health resources among rural underserved regions. While temporary aid helps in the short term, it can inhibit the growth of the necessary infrastructure to provide long-term programs. This, in addition to the rapid expansion of medical volunteerism, has opened opportunities for financially constrained ministries of health to rely on and work with non-sustainable forms of healthcare provision, with little evidence base.13–15 Unfortunately, the social and economic impacts of this reliance remain unknown.13,14
Overall, the Loreto region of the Peruvian Amazon lacks the infrastructure and economic capacity to meet the high demand for care. CHWs have thus served as access points to health within their communities but have not been supported with adequate resources. In this study, we utilized the Community Participatory Program Development (CPPD) framework. CPPD utilizes fundamental elements of community-based participatory research (CBPR) by utilizing a framework that incorporates equitable partnership among community members, capacity building, a focus on working with the strengths and resources of each individual community, and a sustainable process to core medical knowledge retention.16,17 This framework, at its core, has demonstrated successes in the process of empowering underserved health workers both in developed and developing countries.17
Prior to the implementation of a comprehensive training program, we assessed the baseline level of community utilization of CHWs in three rural communities along the Orosa River in Loreto and compared this to the level observed after the community-based training program was implemented and sustained for 1 year. We hypothesized that following the implementation of the health promoter training program, community-wide utilization of health promoters as the first resource for medical information would increase.
Methods
Prior to CHW Training Program
This prospective study was conducted over the course of a 2-year period: 1 year prior and 1-year post-implementation of the CHW training program. Three rural communities (Santo Tomas, Nuevo Israel, and Comandancia), approximately 125 km northeast of Iquitos in the Loreto region of the Peruvian Amazon, were selected to participate in this study. Each community had an average population of 200 residents. Community selection was based on (1) there being similar distances between each community and its local health post (approximately 2 hrs if a boat is available), (2) the presence of a Shaman, and (3) the presence of at least one community-appointed health promoter. Of note, each health promoter was literate in Spanish.
The study location was also chosen in accordance with two non-governmental organizations (NGOs) central to the development of the CHW training program: MGY (mathematical formula for potential energy in Physics) and Project Amazonas. MGY has been working in the Peruvian Amazon to build health capacity through innovative CHW training programs, while Project Amazonas has established roots working with and employing local community members in the Peruvian Amazon over the past two decades. Prior to program implementation, both organizations worked alongside community members to assess and address the need for CHW capacitation and training program development.
After community members and both NGOs jointly decided that further health promoter training programs were desired, citizens of each community were surveyed to determine a baseline of health resource utilization. Surveys were administered by three researchers, identified via a numerical marker, and the results input onto a computer where the file was password protected. A goal of 10% of the members from each of the three communities were asked one multiple choice question: Q1. What health resource (Shaman, Yanashi Health Clinic, Health Promoter) do you utilize first for medical information regarding immediate health concerns? Community members were randomly selected from each of the three communities based on the proximity of their place of residence to the village boat dock. Every other household along the river was then approached until a minimum of 10–15% of the community population had responded. Individuals less than 14 years of age were excluded from the survey. If a residence was found to be vacant, the immediate next residence was approached.
Following the baseline health resource utilization survey collection, MGY and Project Amazonas aggregated health data from an annual mobile clinic along the Orosa River and identified the most prevalent chief complaints among the three communities which included diarrheal disease, respiratory illness, and malaria. Four formal meetings were undertaken with community members, community presidents, and representatives from Project Amazonas and MGY. Themes were introduced by Dr. Ebbs and in-depth discussions were undertaken for each topic. Meetings included discussions on perceived health threats which were compared to the aforementioned clinic data results. General consensus identified for themes of fundamental importance to the overall training. These were not rank ordered. Additionally, the NGOs worked with community leaders and community-appointed health promoters to create the main health promoter curriculum using a community participatory model. The NGOs together with the community leaders and health promoters determined the following four themes to be of fundamental importance to the overall training program: (1) integration of technology with handheld tablet computers; (2) ongoing sustainable training and recurring education; (3) provision of medical supplies and medications; and (4) education in community and pediatric health. As each community has open monthly meetings, regular discussions on the type of training began 6 months prior to program implementation. Communities agreed to have each community president present for the first day of training to supervise and give further updates to the community. Furthermore, the appointed health promoter in each community was expected to attend these monthly meetings as they uphold the responsibility as the community health resource.
CHW Training Program
The CHW training program was implemented in November 2014. Training was provided by six MGY and PA volunteers. The volunteers included two physicians and four medical students. All of the volunteers were provided detailed training and instruction by MGY. Four of the volunteers were fluent in Spanish, and although the other two spoke Spanish, a local interpreter was utilized to facilitate communication. The program included a training curriculum (Table 1) that utilized a community participatory program development model (CPPD) that incorporated a similar methodology to community-based participatory research (CBPR) but with program development instead of research. At its core, this methodology relies heavily on community input steering program development, evaluation, and training. This was an intensive, four-day health promoter training program. The program consisted of both didactic and hands-on educational training components that included vital sign measurement and analysis, wound care, disease prevention, fever management, and osteopathic manipulative treatment (OMT) for musculoskeletal complaints. The curriculum design was planned several months ahead of the training session, in conjunction with Project Amazonas, local community members, and MGY (Table 1).
 |
Table 1 Training Curriculum for Intensive Four-Day Health Promoter Training Program |
The training was completed with hands-on skills assessment and competency testing. Additionally, each health promoter received medical equipment essential for carrying out training protocols, which included rapid malaria assays, blood pressure cuffs, stopwatches, waterproof backpacks, thermometers, wound cleaning supplies, and basic medications such as Tylenol. Throughout the four-day training program, each health promoter was also outfitted with an Android computer tablet uploaded with pre-recorded lectures in Spanish for training. Nightly assignments were given based on the lectures that would be introduced the following day. This methodology, termed “flipped classroom,” has demonstrated usefulness in augmenting retention in learning.18–20 The flipped classroom approach was utilized to expose health promoters to the instructional material prior to classroom sessions and to augment retention of medical information following training.
Beyond training purposes, Android tablets were used for recording patient encounter data and for maximizing health promoter adherence to medical protocols. This was accomplished via the development of Selva, a step-by-step protocol tablet application that utilizes integrated patient-care reporting. Once opened on the tablet, Selva prompts the health promoter to input patient name, community, sex, and age. Next, the health promoter chooses one chief complaint from a drop-down menu (Figure 1). Once a chief complaint is chosen, the health promoter will input how many cups of water the patient is drinking daily and will check whether or not the water is treated. The health promoter then proceeds to measure vital signs including, in an adult, temperature with oral thermometer, brachial blood pressure, radial pulse, respiratory rate, and mental status. The next several questions relate specifically to the chief complaint. For example, if the health promoter chose “fever” on the “Chief Complaint” menu, the next question is the duration of fever (Figure 2). Red flags, or alerts, are programmed to appear when any danger vital signs are recorded. The health promoter is also prompted with a message to make an immediate referral to the closest health clinic if there are danger signs present. After all chief complaint-specific questions are answered, a drop-down menu provides recommended treatment such as oral rehydration solution and zinc administration for pediatric diarrheal illness and dehydration. All this information is recorded on the Android tablet for retrospective analysis, and all data are saved until the internet is available for upload.
 |
Figure 1 Chief complaint drop-down menu on tablet application. |
 |
Figure 2 History of present illness information for fever on tablet application. |
One Year After CHW Training Program
One year post-program implementation and initial training session, community members were asked the same survey question: Q1. What health resource (Shaman, Yanashi Health Clinic, Health Promoter) do you utilize first for medical information regarding immediate health concerns? Each community was again surveyed and the same procedure and exclusion criteria were followed. Two of the same three researchers collected the data. Every other residency was approached while moving to the immediate next residence if any homes were vacant.
Statistical Analysis
The pre-training and post-training survey answers from all three communities were grouped together and SPSS software was used to analyze the data. A paired t-test (p-values < 0.05 were considered significant) was utilized to compare responses regarding each type of initial health resource (Shaman, Yanashi Health Clinic, Health Promoter) before and after training implementation.
Results
A total of 131 randomly selected community members from Santo Tomas, Nuevo Israel, and Comandancia received and responded to Q1 prior to program implementation and the initial training session. The average population of these three communities is 200. As such, the average number of respondents (44 per community) to the survey question represented >10% of each community. No community members approached refused survey participation. While small numbers of community members indicated the use of health promoters (7/131, 5%; Table 2) or Shamans/traditional healers (13/131, 10%) as a first health resource, the vast majority of respondents (111/131, 85%) to the initial questionnaire indicated travel to the closest medical health post in Yanashi as the preferred initial medical service.
 |
Table 2 Number of Respondents in Each Community Who Visited a Health Promoter First for Medical Consult/Education |
Health promoters were identified as already in existence and appointed by community members as the health advocate of each of the three communities of this study. Each community agreed to appoint the same health promoter to the training program with community supervision of training activities for oversight. MGY and Project Amazonas trained a total of five health promoters during this initial training period, representing five communities. Each of the five health promoters completed the course and passed all skills examinations with competency, as defined by the program as a score greater than 79.4% per test.
One year after program implementation, 136 randomly selected community members from the same communities were administered and responded to questionnaires. The results of the second questionnaire demonstrated a significant increase (89/136, 65%; p = 0.02613; Table 3; Figure 3) in the number of respondents selecting health promoters as an initial source of medical information. Moreover, each of the three communities also now selected health promoters as the preferred choice for initial information. There was a concurrent decrease (40/136, 30%; Table 3; Figure 3) in the number of community members who selected travel to the medical health post in Yanashi as a first treatment option; however, this decrease was not statistically significant (p = 0.07005; Table 3). Meanwhile, similar to pre-program implementation, only a small number of community members (7/136, 5%; p = 0.63819; Table 3; Figure 3) indicated a preference for a Shaman as a first health resource.
 |
Table 3 Recorded Community Averages to Questionnaire Response on First Health Resource Utilized Pre- and Post-Program Implementation |
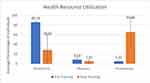 |
Figure 3 Average first health resource utilization pre- and post-program implementation. |
Discussion
Health promoters help to bridge the gap between the formal healthcare system and underserved regions of LMICs with significant medical needs. They have been shown to improve population health outcomes and reduce urban-rural health inequities.21 In isolated areas such as Loreto, their impact on improving community health and providing basic medical education may indeed be substantial.
In this study, we found that the implementation of the MGY CHW training program significantly increased community utilization of health promoters among three Amazonian communities within the province of Loreto. With this expanded health promoter utilization, community members living within Santo Tomas, Comandancia, and Nuevo Israel, respectively, reported increased access to a local health resource for medical information, healthcare management, emergency care provision, malaria diagnosis, and recommendations regarding appropriate referral to the nearest health post. Furthermore, our results suggest that community co-development of the CHW training program utilizing a CPPD model may contribute to overall community awareness, acceptance, and utilization of the trained health promoters. It is interesting to note that the CHWs did not change their routines or availability. Instead, they were more equipped to address the important health needs of community members. Furthermore, the community-based approach to develop this program heightened awareness among community members of the CHW’s capabilities. We believe this increased awareness, along with the CHW's skills and the specific tools provided to them by the program helped them address local needs more effectively. These factors were jointly responsible for the observed changes in utilization.
The principal limitation of this study was the relatively small number of communities sampled. Although this study assessed an adequate number of members of each community, the population of these communities is small. This limits generalizability to other communities, as there is great variance among Peruvian Amazon communities. At the forefront of this variance is whether or not a community has appointed a health promoter and how much training that person has received. This variable can impact the efficacy of the individual CHW and her or his ability to successfully interact with the community members.
Given the geographic isolation of each community, inhabitants can often be situated in remote settings away from the center of the community, where the boat dock is located. This could further influence the accuracy of data collected, as a selection in each community began with the residences nearest to the boat dock. Additionally, data regarding why community members decided to change their utilization of health resources, or how often members used health promoters after the training program, were not collected. For instance, community members’ awareness of the training program and the presence of foreign researchers could have introduced bias into community responses based on their presence.
Conclusions
In response to the globally increased emphasis on health promoter utilization as a means of achieving the Millennium Development Goals,22 one of this study’s primary aims was to develop a sustainable and scalable model of health promoter capacitation suitable for a wide range of rural Amazonian communities and other rural, underserved communities across the globe. Larger studies exploring the impact of innovative training methodologies on overall CHW program sustainability and the effects of these CHW cadres on population health, while methodologically difficult, must still be carried out. Exploring the topics of community participation with a CPPD model can help guide best practices for future program development and execution. Additionally, future studies should focus on how to sustain programs and medical skill retention when health promoters, such as those in the Peruvian Amazon, operate in hard-to-reach geographic locations with extreme health challenges.
The program utilized in this exploratory study opens new doors to assessing how the combination of mobile health applications, community participation, ongoing commitment to training, and train-the-trainer with flipped classroom methodology can coalesce to form a cohesive training program designed to meet the needs of each individual community. Furthermore, it demonstrates the importance of community-oriented program design and how co-development of the training program to meet the individual needs of communities can positively impact the overall utilization and acceptance of the CHW program. As this training program continues to expand to date, continued reevaluation with community input remains critical to its sustainability.
Abbreviations
HRH, human resources for health; CHW, community health worker; LMIC, low- and middle-income country; NGO, non-governmental organization.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics and Consent Statement
IRB permission was granted through the ATSU, Arizona IRB Committee; IRB #2105-155.
Acknowledgments
We acknowledge support from the non-governmental organization, 501(c)(3), Project Amazonas, and in particular Dr. Devon Graham, for facilitating this research, community meetings, lodging at Madre Selva, outreach, training facility accommodations, and mobile clinic data. We acknowledge the 501(c)(3) MGY, and in particular David Tseng, Sam Waggoner, and Guadalupe Chavez for their commitment to the development and persistent reassessment of mobile health programs. We also acknowledge A.T. Still University School of Osteopathic Medicine in Arizona, and the University’s Institutional Review Board for working with us. We acknowledge and give tremendous thanks to the community health workers, community leaders, and residents of Comandancia, Nuevo Israel, and Santo Tomas along the Orosa River in Loreto, Peru.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
There were no outside sources of funding for the research reported in this manuscript.
Disclosure
The authors declare they have no competing interests in this work.
References
1. Lopes S, Cabral AJ, de Sousa B. Community health workers: to train or to restrain? A longitudinal survey to assess the impact of training community health workers in the Bolama Region, Guinea-Bissau. Hum Resour Health. 2014;12(1):8. doi:10.1186/1478-4491-12-8
2. Liu A, Sullivan S, Khan M, Sachs S, Singh P. Community health workers in global health: scale and scalability. Mt Sinai J Med. 2011;78:419–435. doi:10.1002/msj.20260
3. Pallas SW, Minhas D, Pérez-Escamilla R, Taylor L, Curry L, Bradley EH. Community health workers in low-and middle-income countries: what do we know about scaling up and sustainability? Am J Public Health. 2013;103(7):e74–e82. doi:10.2105/AJPH.2012.301102
4. Singh P, Sachs JD. 1 million community health workers in sub-Saharan Africa by 2015. Lancet. 2013;382(9889):363–365. doi:10.1016/S0140-6736(12)62002-9
5. Kane EP, Collinsworth AW, Schmidt KL, et al. Improving diabetes care and outcomes with community health workers. Fam Pract. 2016;33(5):523–528. doi:10.1093/fampra/cmw055
6. Margellos-Anast H, Gutierrez MA, Whitman S. Improving asthma management among African-American children via a community health worker model: findings from a Chicago-based pilot intervention. J Asthma. 2012;49(4):380–389. doi:10.3109/02770903.2012.660295
7. Chinbuah MA, Abbey M, Kager PA, et al. Assessment of the adherence of community health workers to dosing and referral guidelines for the management of fever in children under 5 years: a study in Dangme West District, Ghana. Int Health. 2013;5(2):148–156. doi:10.1093/inthealth/ihs008
8. Mwai GW, Mburu G, Torpey K, Frost P, Ford N, Seeley J. Role and outcomes of community health workers in HIV care in sub-Saharan Africa: a systematic review. J Int AIDS Soc. 2013;16(1):18586. doi:10.7448/IAS.16.1.18586
9. Brierley CK, Suarez N, Arora G, Graham D. Healthcare access and health beliefs of the indigenous peoples in remote Amazonian Peru. Am J Trop Med Hyg. 2014;90:180–183. doi:10.4269/ajtmh.13-0547
10. Instituto Nacional de Estadistica e Informatica [website]. Día Mundial de la Población, 11 de Julio. Available from: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1251/Libro.pdf.
11. Red Nacional de Epidemiología [website]. Dirreción General de Epidemiología: Casos de malaria por departmentos, Perú. 2016. Available from: http://www.dge.gob.pe/portal/docs/vigilancia/boletines/2016/51.pdf.
12. Dirrecíon Regional de Salud Loreto [website]. Perfil de Competencias del Promotor(a) de Salud de Loreto. Available from: http://bvs.minsa.gob.pe/local/minsa/1484.pdf.
13. Asgary R, Junck E. New trends of short-term humanitarian medical volunteerism: professional and ethical considerations. J Med Ethics. 2013;39(10):625–631. doi:10.1136/medethics-2011-100488
14. Caldron PH, Impens A, Pavlova M, Groot W. A systematic review of social, economic and diplomatic aspects of short-term medical missions. BMC Health Serv Res. 2015;15(1):380. doi:10.1186/s12913-015-0980-3
15. Stone GS, Olson KR. The ethics of medical volunteerism. Med Clin North Am. 2016;100(2):237–246. doi:10.1016/j.mcna.2015.09.001
16. Israel BA, Eng E, Schulz AJ, Parker EA. Introduction to methods for CBPR for health. In: Israel BA, Eng E, Schulz AJ, Parker EA, Eds. Methods for Community-Based Participatory Research for Health. San Francisco: Jossey-Bass; 2013:3–38.
17. Wallerstein N, Duran B, Oetzel JG, Minkler M. Community-Based Participatory Research for Health. Vol. 3. San Francisco: Jossey-Bass; Chapter 1. 2018: 18.
18. McLaughlin JE, Roth MT, Glatt DM, et al. The flipped classroom: a course redesign to foster learning and engagement in a health professions school. Acad Med. 2014;89(2):236–243. doi:10.1097/ACM.0000000000000086
19. Pierce R, Fox J. Vodcasts and active-learning exercises in a “flipped classroom” model of a renal pharmacotherapy module. Am J Pharm Educ. 2012;76(10):196. doi:10.5688/ajpe7610196
20. Ryan MD, Reid SA. Impact of the flipped classroom on student performance and retention: a parallel controlled study in general chemistry. J Chem Educ. 2015;93(1):13–23. doi:10.1021/acs.jchemed.5b00717
21. Javanparast S, Baum F, Labonte R, Sanders D, Rajabi Z, Heidari G. The experience of community health workers training in Iran: a qualitative study. BMC Health Serv Res. 2012;12(1):291. doi:10.1186/1472-6963-12-291
22. WHO. Global Health Workforce Alliance 2014 Annual Report [website]. 2015. Available from: http://www.who.int/workforcealliance/knowledge/resources/annual_report2014/en/.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
