Back to Journals » Clinical Epidemiology » Volume 7
Existing data sources for clinical epidemiology: the Danish Patient Compensation Association database
Authors Tilma J, Nørgaard M, Mikkelsen KL, Paaske Johnsen S
Received 7 March 2015
Accepted for publication 4 May 2015
Published 17 July 2015 Volume 2015:7 Pages 347—353
DOI https://doi.org/10.2147/CLEP.S84162
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Professor Henrik Sørensen
Jens Tilma,1 Mette Nørgaard,1 Kim Lyngby Mikkelsen,2 Søren Paaske Johnsen1
1Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus, 2Danish Patient Compensation Association, Copenhagen, Denmark
Abstract: Any patient in the Danish health care system who experiences a treatment injury can make a compensation claim to the Danish Patient Compensation Association (DPCA) free of charge. The aim of this paper is to describe the DPCA database as a source of data for epidemiological research. Data to DPCA are collected prospectively on all claims and include information on patient factors and health records, system factors, and administrative data. Approval of claims is based on injury due to the principle of treatment below experienced specialist standard or intolerable, unexpected extensiveness of injury. Average processing time of a compensation claim is 6–8 months. Data collection is nationwide and started in 1992. The patient's central registration system number, a unique personal identifier, allows for data linkage to other registries such as the Danish National Patient Registry. The DPCA data are accessible for research following data usage permission and make it possible to analyze all claims or specific subgroups to identify predictors, outcomes, etc. DPCA data have until now been used only in few studies but could be a useful data source in future studies of health care-related injuries.
Keywords: public health care, treatment injuries, no-fault compensation, registries, research, Denmark
Introduction
The majority of the population in developed countries has at least one contact with the health care system each year. In the US, 82.1% of adults and 92.8% of children were in contact with the health care system in 2012.1 In Denmark, 95% of all residents are in contact with the health care system corresponding to 1.1 million admissions to hospitals, 11.5 million outpatient visits at hospitals, 11.5 million visits to privately practicing specialists, and 40.5 million general practitioner visits in 2012.2 The high activity will inevitably lead to health care-related patient injuries as a result of either adverse events (AEs) or errors. The reported incidence of AEs varies between countries and health care systems (ie, from 2.9% of all admissions in Utah and Colorado, US, to 16.6% in New South Wales and South Australia).3,4
Globally, the awareness and focus on patient safety have increased over the last decades.5 Several procedures and initiatives (eg, safety checklists before surgical procedures6 and programs for prevention of central line-associated blood stream infections)7 have been launched and implemented in order to improve patient safety and quality of care. Still, data on the effectiveness of interventions aimed at reducing the risk of AEs and errors remain sparse. Preferably, we would have data documenting the effects of interventions by showing the change of risk in the intervened areas of health care. If sufficiently detailed, these data might also reveal the characteristics of injuries and the patients to whom they occur. A potential source of insights into patient safety is the growing amounts of data on health care-related injuries, which are collected as part of patient insurance and compensation administration.8 Herein often included are incidence, high-risk regions, and specialties, and differences among these categories may be observed – all valuable information when building a dataset to help understand the challenges in patient safety and decide where to focus preventive effort and thereby improve health care.
Data gathering is easier when high-completeness registries are present and ongoing updated. Denmark has a long tradition of collecting information on health care for the entire population in publicly governed registries. It is possible to link the registries at the individual level by the Civil Registration System (CRS)-number – a personal identifier given to every citizen at birth or immigration.9–12
With this paper, we aim to present the Danish Patient Compensation Association (DPCA) database and outline the research potential in the database. The DPCA is the organization responsible for managing the claims and compensation of injured patients in Denmark.
Danish health care system
The health care system in Denmark guarantees free access to hospital admissions, outpatient treatment, and visits to general practitioners. It is publicly funded in the vast majority of its function as only approximately 15% of the costs are paid by own expense, mainly out-of-pocket expenditure on pharmaceuticals and dentistry. If a citizen contracts an illness, he/she will usually be seen by a general practitioner who is a part of the primary health care. From there, it is possible to be referred to a specialist or a hospital. A patient is intended to be treated on the least specialized level to maintain an effective and relevant treatment without too much or too expensive actions, in order to give all patients the best treatment.13
DPCA
The DPCA was founded in 1992 in order to improve the patients’ access to compensation following the passing of the Patient Insurance Act. According to the act, patients are to be compensated if they unexpectedly suffer injury while being treated anywhere in the entire Danish health care system. The DPCA functions as a no-fault system of claims, and the claimants are not charged any expenses for the casework.
Before 1992, compensation for an injury could only be obtained through the courts based on legal proof of an error by a health care professional. In practice, this meant that only a minority of patients with injuries received compensation. Following the passing of the Patient Insurance Act, legal proofs of errors are no longer required, but it is highly likely that the injury is related to the patient’s treatment or examination. The DPCA as an institution gathers information on the case and decides the outcome, thereby assuring legal compensation in accordance with the Patient Insurance Act. In 1996, it was accompanied by the Act on Compensation for Medicine-Related Injuries. Since then, the area covered by the law has been expanded to include almost all areas and functions of the public and private health service. Both laws are now collected in the Danish Act on the Right to Complain and Receive Compensation within the Health Service, and claims are ruled according to this. The covered health care areas are listed in Table 1.
  | Table 1 The health care areas covered by the Danish Patient Compensation Association |
All patients who suffer injury in the public and private health care system can file a claim as long as the health care person is authorized by the National Board of Health. The DPCA is predominately tax funded through two sources: the Danish Regions, who finance the compensation for the public treatment injuries, and the Ministry of Health and Prevention, who finance the compensation for the medicine-related injuries. Private health care providers besides funded from public health care must take out a health care provider insurance on their own; however, this does not affect the process of filing a claim from a patient’s perspective. The tortfeasors (committer of the tort; commonly the hospital, administratively governed and financed by the region) account for the administration fee.
In 2012, a total of 9,628 claims were made to the DPCA. Of these, 33.1% were accepted and granted a total of 143,949,117 USD.14 Figure 1 shows the annual number of approved and dismissed claims from 1996 to 2013.
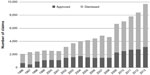  | Figure 1 The number of claims closed by the Danish Patient Compensation Association per year from 1996 to 2013, shown as approved and dismissed. |
DPCA database
The DPCA database consists of claims from all of Denmark. Digital data collection has been made since the start of DPCA in 1992. Until 2006, there were no systematic digital data on medical records, diagnostic imaging, specialist doctor’s assessment, legal justification for decision, and additional material for case disclosure; however, data were stored in an analog form and are accessible upon payment of transport expenses. Table 2 shows the data recorded in the DPCA database, which includes information on the patient, the alleged injury, and information used to resolve the ruling.
When a claim is filed, a new folder is made for each case coded with a unique case number in addition to the CRS-number. Information is obtained from the patient’s claim, medical records, a report from the place of treatment, remarks from the patient about the report, and possibly additional information from other places of treatment and specialist assessments. An overview of the distribution of reasons for approving claims among the approved treatment injury claims in 2012 is presented in Figure 2A. The development of this distribution was somewhat constant in the years 2007–2012, which is shown in Figure 2B. The most common cause was suboptimal diagnosis and/or treatment, below experienced specialist standard. For example:
- A 53-year-old man was treated with corticosteroids for COPD. Six years later, he needed surgery because of vertebral compression fractures. It was considered below specialist standard that he was not followed up by a bone density scan and treated with vitamin-D, calcium, and possibly bisphosphonates.
- A 35-year-old woman received smoking cessation treatment. First time, she started smoking again. Second time, she experienced adverse effect in the form of short-lasting faints and stopped treatment. She was started up a third time on the same drug because of a persistent wish for smoking cessation, but experienced breast pain and died from a coronary artery blood clot. The DPCA considered the incident most likely to stem from the treatment. Giving the same treatment the third time was considered below specialist standard.
The approved treatment injury claims constituted 33.1% of all closed claims in 2012 (2,783 out of 8,408). We only included data until the year 2012, because it is the most recent year with sufficient data due to the data lag arising from the often long time period from the time of the injury to the final decision of making the claim. The lag time may be up to a few years.
A caseworker and usually an in-house specialist doctor will decide whether an injury has occurred, and if so, whether it is entitled to compensation. The average processing time of a claim is 6–8 months regarding compensability. To determine the size of compensation, additional information is often requested, eg, receipts of drugs, transportation expenses, a doctor statement(s) regarding the degree of injury, and loss of earning capacity. This process might take up to 1 year, though most of the compensation is paid immediately after compensability decision. Figure 3 describes the casework of a claim.
  | Figure 3 Flowchart of casework. |
Data linkage possibilities
Linking data from the DPCA database with other population-based health care registers is a relatively simple yet powerful way of increasing the depths of the claims data. Data in the DPCA database always include a patient’s CRS-number. Since this number is included in all public registries and databases in Denmark, it is feasible to link the data from the DPCA database to a wide range of other data sources. Numerous registries are kept in Denmark spanning from birth to death of every Danish citizen, and therefore, through record linkage, it is possible to obtain more detailed data on patients characteristics (including data on clinical, demographic, geographic, and socioeconomic variables) and to perform long-term follow-up (eg, on mortality, readmissions, or return to work) on the patients registered in the DPCA database.9 The Danish National Registry of Patients is an example of a registry that will often be relevant to consider in relation to record linkage with the DPCA database as it holds detailed data on all admissions to Danish hospitals since 1977 and also on visits to outpatient clinics and emergency room visits since 1995.15
The DPCA database covers treatment injuries reflected by compensation claims. Another separate agency, the National Agency for Patients’ Rights and Complaints (NAPRC), receives all complaints regarding the health care system, the appeals from the DPCA rulings, and the reports of AEs for registration and learning. Reported AEs go into the Danish Patient Safety Database (DPSD) under the NAPRC; however, the DPSD does not contain CRS-numbers and record linkage with other data sources; individual identification is therefore not possible. The AE data comprise major, minor, or even trivial (potential and actually occurred) injuries; hence, the number of AE reports is substantially higher than the number of compensation claims. Data linkage to other registries from the DPSD would potentially give insight into causes of AEs in general and highlight high-risk patient groups on a broader scale than treatment injuries eligible for compensation. The DPCA data relate to NAPRC data in the way that approved compensation claims in the DPCA ought to be a subset of AEs in the DPSD, if the registration of both compensation claims and reporting AEs was complete. Complaints to the NAPRC do not necessarily reflect treatment injuries, but is often caused by dissatisfaction (eg, due to poor communication); however, an overlap is possible, since the systems for complaints and claims are separate.
Strengths and limitations
The DPCA database holds detailed data, which, except for trivial cases, are evaluated by specialist doctors on the different medical areas. However, only patients who actually file a claim are registered in the DPCA database, and therefore, estimates based on DPCA data will underestimate the true incidence of injuries occurring in the Danish health care system. Unfortunately, the potential underreporting of eligible compensation claims to the DPCA and the influencing factors has not yet been evaluated. Underreporting is known from other health care systems, eg, in New York State, only 1.53% (95% CI 0.00;3.24) of AEs caused by medical negligence resulted in a claim.16 Likewise, a study from New Zealand found that only 0.4% of AEs and 4% of the preventable AEs resulted in a complaint.17 Patients with permanent and fatal injuries were more likely to file a complaint than patients with temporary injuries (odds ratio 11.4, 95% CI 5.9;22.1 and odds ratio 17.9, 95% CI 9.3;34.2, respectively).17 Another study from New Zealand reported that only 2.9% of patients eligible for compensation actually filed a claim to their no-fault system of treatment injury compensation.18
Although AEs in the Danish health system are to be reported to the DPSD, this is not always fulfilled. A survey of the DPSD reporting system in 2006 suggested a maximum reporting of 85% of the AEs. In 2010, the proportion of reported AEs was estimated to be as low as 15%14,19 despite increasing report counts of 12,370 in 2006 to 155,791 in 2012.20 The real number of AEs and treatment injuries in the Danish health care system therefore remains unknown. A contributing factor to the rise of AE reports and compensation claims is an increasing public knowledge of the existence of the compensation system and increased willingness to report injuries and seek compensation. The true incidence of AEs and injuries may therefore not be increasing or at least not as much as the increasing number of reports suggests.21 Still, the fact that a substantial proportion of the complaints that are being filed concerns severe and potentially preventable injuries,17 and the minor effort needed to file a claim together with no financial demands to do so, indicates that the DPAC database gives a potentially valuable insight on serious threats to patient safety. Furthermore, the de minimis threshold for compensation is 10,000 DKR (≈1,500 USD), filtering off minor and potential (AEs includes potentially harmful events) injuries from the approved claims and selecting more serious cases in the database. Therefore, DPCA data may potentially guide injury preventive efforts to improve health care quality.
Examples of studies using DPCA data
Data from the DPCA database have been used in a number of studies within recent years. In a study based on all closed claims concerning medical-related deaths in the Danish primary health care and hospital setting from 1996 to 2008, Hove et al identified 836 deaths caused by treatment or lack of treatment in the period of 1996–2008 with a total cost of compensation at 55 million USD. According to the DPCA, 435 (52%) deaths were preventable.22
Another study examined patient safety at labor wards according to ward size (number of deliveries per year). The study was based on DPCA data on approved claims of obstetric injuries linked with data from the National Birth Registry. The approval rate of claims was lowest in large labor units (34.2%), higher in very large (38.6%) and intermediate labor units (41.7%), and highest in small labor units (50.0%). The study concluded that the results might reflect that large labor units are living up to the principle of best practice to a greater degree.23
An updated list of scientific publications based on DPCA data is available at the website http://patienterstatningen.dk/da/Udgivelser-og-tal/Faglige-artikler.aspx.
Compensation claims contribute to the organization of the health care system on different levels. On a single case level, a compensation claim can function as a feedback system, eg, a general practitioner and practicing specialist missed a breast cancer diagnosis due to an inappropriate procedure of pathology responses. Because of the awareness from the compensation claim, they changed the information flow channels in both clinics. Studies based on multiple claims offer the foundation of knowledge to better organize health care, eg, the question of consolidating specific departments, especially labor wards, in central units with a higher volume of contacts has been influenced by these patients’ safety evaluations.
A further research potential of the DPCA database is large, because individual level identification, medical records, and data linkage are available. The DPCA data might be used to validate approved compensation claims as a measure of the treatment injuries, to investigate predictors of treatment injuries in general, to identify high-risk areas and quality of health care, and to compare information value from these data compared to AEs, complaints, and others.
Other databases arising from compensation claims are present internationally, eg, those in the People’s Republic of China described by Li et al,24 in New Zealand used by Davis et al,25 and in the US used by Brown et al.26
Accessing DPCA data
Data files are stored by the DPCA (http://www.patienterstatningen.dk). From the database, the data are accessed by the lawyers and doctors of the DPCA to rule in the claims, and the data are coded and published in annual reports by the DPCA and in medical journals by researchers. Authorized health care researchers can be granted access to the database by contacting the medical coordinator at DPCA, Kim Lyngby Mikkelsen ([email protected]).
The use of any personal data, including health data, is protected by the Danish Act on Processing of Personal Data, and a specific permission from the Data Protection Agency is required (http://www.datatilsynet.dk). This permission is a formality if the project satisfies the following: follows the data protection legislation, the objectives are relevant from a clinical and societal perspective, and the project is affiliated to a Danish research institution.
Conclusion
The DPCA database holds valuable information on treatment injuries in the Danish health care system. The approved closed claims are indicative of partly or totally preventable injuries and are therefore of great interest in designing efficient preventive initiatives and a health care system with better patient safety.
Acknowledgment
This work was supported by a grant from the Tryg Foundation.
Disclosure
The authors report no conflict of interests.
References
FASTSTATS – doctor visits. Available from: http://www.cdc.gov/nchs/fastats/physician_visits.htm. Accessed June 4, 2014. | |
Regioner – fakta om sundhedsvæsenet – sundhedsvæsenet i tal. [Regions – facts in the health care system – health care in numbers]. Available from: http://www.regioner.dk/aktuelt/temaer/fakta+om+regionernes+effektivitet+og+økonomi/kopi+af+fakta+om+sundhedsvæsenet. Accessed March 27, 2014. Danish. | |
Thomas EJ, Studdert DM, Burstin HR, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care. 2000;38(3):261–271. | |
Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD. The quality in Australian health care study. Med J Aust. 1995;163(9):458–471. | |
Stelfox HT, Palmisani S, Scurlock C, Orav EJ, Bates DW. The “to err is human” report and the patient safety literature. Qual Saf Health Care. 2006;15(3):174–178. | |
Bergs J, Hellings J, Cleemput I, et al. Systematic review and meta- analysis of the effect of the World Health Organization surgical safety checklist on postoperative complications. Br J Surg. 2014;101(3):150–158. | |
Berenholtz SM, Lubomski LH, Weeks K, et al; On the CUSP: Stop BSI Program. Eliminating central line-associated bloodstream infections: a national patient safety imperative. Infect Control Hosp Epidemiol. 2014;35(1):56–62. | |
Pegalis SE, Bal BS. Closed medical negligence claims can drive patient safety and reduce litigation. Clin Orthop Relat Res. 2012;470(5):1398–1404. | |
Frank L. When an entire country is a cohort. Science. 2000; 287(5462):2398–2399. | |
Storm HH, Michelsen EV, Clemmensen IH, Pihl J. The Danish cancer registry – history, content, quality and use. Dan Med Bull. 1997;44(5):535–539. | |
Thygesen LC, Daasnes C, Thaulow I, Bronnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health. 2011; 39(7 Suppl):12–16. | |
Pedersen CB. The Danish civil registration system. Scand J Public Health. 2011;39(7 Suppl):22–25. | |
Ministry of Health and Prevention. Health care in Denmark. [Danish Health Care]; 2008. Available from: http://www.sum.dk/Aktuelt/Publikationer/~/media/Filer%20-%20Publikationer_i_pdf/2008/UK_Healthcare_in_dk/pdf.ashx. Accessed March 18, 2014. | |
Danish Patient Insurance Association. DPIA annual report of 2010–2012 in numbers regarding claims and compensations; 2013. Available from: http://patienterstatningen.dk/da/Udgivelser-og-tal/Statistik/%/media/Files/Statistik/Statistik%202012/hel%C3%A5rstal_2010_2012_12.ashx. | |
Andersen TF, Madsen M, Jorgensen J, Mellemkjoer L, Olsen JH. The Danish national hospital register. A valuable source of data for modern health sciences. Dan Med Bull. 1999;46(3):263–268. | |
Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence. Results of the Harvard medical practice study III. N Engl J Med. 1991;325(4):245–251. | |
Bismark MM, Brennan TA, Paterson RJ, Davis PB, Studdert DM. Relationship between complaints and quality of care in New Zealand: a descriptive analysis of complainants and non-complainants following adverse events. Qual Saf Health Care. 2006;15(1):17–22. | |
Bismark MM, Brennan TA, Davis PB, Studdert DM. Claiming behavior in a no-fault system of medical injury: a descriptive analysis of claimants and non-claimants. Med J Aust. 2006;185(4):203–207. | |
Rambøll Management. Evaluation on act on patient safety [Evaluering af lov om patientsikkerhed]. Danish Domestic and Health Ministry; 2006. Available from: http://dpsd.demo.privatsite.dk/~/media/Foundry/Sites/DPSD/Files/Informationsmateriale/rapportevaluering.ashx. Accessed June 17, 2015. Danish. | |
Patientombuddet. Årsberetning 2012, dansk patientsikkerheds database del 1; 2013. [The National Agency for Patients’ Rights and Complaints. Annual Report 2012, the Danish Patient Compensation Association Database, part 1]. Available from: http://dpsd.demo.privatsite.dk/~/media/Foundry/Sites/DPSD/Files/Aarsrapporter/2012_%C3%A5rsberetning_dpsd_del_1_001.aspx. Accessed March 27, 2014. Danish. | |
Bast K, Graugaard O, Rasmussen C, Mortensen L. Stigningen i anmeldelser til og erstatningstilkendelser fra Patientforsikringen 2006–2011 – analyse af baggrunden og prognose for 2012–2015. [The increase in claims to and compensations from the Danish Patient Compensation Association 2006–2011 – analysis of the background and prediction for 2012–2015]. The Danish Patient Compensation Association; 2011. Available from: http://patienterstatningen.dk/da/Udgivelser-og-tal/~/media/Files/Artikler/Rapport%2009032012.ashx. Accessed June 17, 2015. Danish. | |
Hove L, Bock J, Christoffersen J, Dam H. An analysis of closed claims related to death in the Danish health care system. Int J Med Med Sci. 2012;2(10):197–203. | |
Milland M, Christoffersen JK, Hedegaard M. The size of the labor wards: is bigger better when it comes to patient safety? Acta Obstet Gynecol Scand. 2013;92(11):1271–1276. | |
Li H, Wu X, Sun T, et al. Claims, liabilities, injures and compensation payments of medical malpractice litigation cases in China from 1998 to 2011. BMC Health Serv Res. 2014;14:390. | |
Davis P, Lay-Yee R, Fitzjohn J, Hider P, Briant R, Schug S. Compensation for medical injury in New Zealand: does ”no-fault” increase the level of claims making and reduce social and clinical selectivity? J Health Polit Policy Law. 2002;27(5):833–854. | |
Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010; 17(5):553–560. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


