Back to Journals » Psoriasis: Targets and Therapy » Volume 6
Excimer laser for the treatment of psoriasis: safety, efficacy, and patient acceptability
Authors Abrouk M, Levin E, Brodsky M, Gandy JR, Nakamura M, Zhu TH, Farahnik B, Koo J, Bhutani T
Received 23 August 2016
Accepted for publication 3 November 2016
Published 12 December 2016 Volume 2016:6 Pages 165—173
DOI https://doi.org/10.2147/PTT.S105047
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Uwe Wollina

Michael Abrouk,1 Ethan Levin,2 Merrick Brodsky,1 Jessica R Gandy,1 Mio Nakamura,2 Tian Hao Zhu,3 Benjamin Farahnik,4 John Koo,2 Tina Bhutani2
1Irvine School of Medicine, Irvine, 2Department of Dermatology, Psoriasis and Skin Treatment Center, University of California, San Francisco, 3Department of Dermatology, University of Southern California Keck School of Medicine, Los Angeles, CA, 4Department of Dermatology, University of Vermont College of Medicine, Burlington, VT, USA
Introduction: The 308 nm excimer laser is a widely used device throughout the field of dermatology for many diseases including psoriasis. Although the laser has demonstrated clinical efficacy, there is a lack of literature outlining the safety, efficacy, and patient acceptability of the excimer laser.
Methods: A literature search on PubMed was used with combinations of the terms “excimer”, “excimer laser”, “308 nm”, “psoriasis”, “protocol”, “safety”, “efficacy”, acceptability”, “side effects”, and “dose”. The search results were included if they contained information pertaining to excimer laser and psoriasis treatment and description of the safety, efficacy, and patient acceptability of the treatment.
Results: The 308 nm excimer laser is generally safe and well tolerated with minimal side effects including erythema, blistering, and pigmentary changes. It has a range of efficacies depending on the protocol used with several different treatment protocols, including the induration protocol, the minimal erythema dose protocol, and the newer minimal blistering dose protocol.
Conclusion: Although the excimer laser is not a first-line treatment, it remains an excellent treatment option for psoriasis patients and has been demonstrated to be an effective treatment with little to no side effects.
Keywords: excimer, laser, 308 nm, psoriasis, safety, efficacy
Introduction
The 308 nm excimer laser is a widely used device throughout the field of dermatology for many diseases, including psoriasis, vitiligo, hypopigmented disorders, alopecia areata, atopic dermatitis, and in many other dermatologic diseases such as cutaneous T-cell lymphoma, other lymphoproliferative disorders, granuloma annulare, Langerhans cell histiocytosis, lichen planus, and localized scleroderma.1,2 The term excimer is derived from “excited dimer,” which describes the mixture of the noble gas xenon and the halogen chloride gas (XeCl) that is utilized. The dissociation of these excited dimers produces a 308 nm ultraviolet (UV) monochromatic coherent wavelength, which lies within the UVB spectrum.1,3 Although the excimer laser can be used in the treatment of many dermatologic conditions, this study will focus on the treatment of psoriasis.
Psoriasis is a chronic, inflammatory disease that primarily manifests with cutaneous findings and affects ~3% of the American population.4 The current understanding of the pathogenesis and pathophysiology of psoriasis is continuing to evolve, but the majority of knowledge surrounds the most classical variant, psoriasis vulgaris. Psoriasis vulgaris compromises more than 80% of cases, usually present with raised, well-demarcated, erythematous oval plaques with adherent silvery scale. It is a complex immune-mediated disease propagated by abnormal interactions between T lymphocytes, dendritic cells, keratinocytes, neutrophils, and proinflammatory cytokines.
The initiation of psoriasis begins with an amalgamation between environment and genetic factors. The innate immune system provides an early, preformed response as a mechanism against harm to the host and has been implicated in the development of psoriasis. Cytokines produced from innate immune cells activate myeloid dendritic cells, which in turn present antigens and secrete mediators leading to Th17 and Th1 differentiation. These T cells secrete mediators that activate keratinocytes and induce production of antimicrobial peptides, proinflammatory peptides, and chemokines that create a positive feedback loop and maintain an active psoriatic disease cycle.5,6 These psoriatic lesions arise from alterations in the skin consisting of decreased keratinocyte maturation, increased keratinocyte proliferation, and vascular changes consistent with proliferation and dilatation.4 Histologically, acanthosis, parakeratosis, elongated rete ridges, and a mixed cellular infiltrate characterize psoriasis. More specifically, inflammatory cells such as dendritic cells, macrophages, and CD3+ T cells and CD8+ T cells are detected in the dermis, whereas neutrophils and some CD3+ T cells and CD8+ T cells are detected in the epidermis.5 The aforementioned synopsis of the pathogenesis and pathophysiology of psoriasis will be crucial for the understanding of the mechanism of action of the excimer laser.
The mechanism of action of the excimer laser, similar to the action of UVB light, induces apoptosis in keratinocytes and T lymphocytes. The absorption of 308 nm wavelength induces DNA breakage, upregulation of the tumor suppressor gene p53, and subsequent reduction of proto-oncogene Bcl-2, leading to cell cycle arrest in keratinocytes and T lymphocytes.1 This breaks the positive feedback loop and halts the psoriatic disease cycle created by the activated T lymphocytes. Furthermore, Kagen et al demonstrated that very high doses of excimer laser treatment in psoriatic lesions reduced the numbers of pathogenic memory/effector T cells infiltrating lesional epidermis and dermis.7
While the importance of the excimer laser in the treatment of psoriasis will be discussed, it is interesting to note the origins of the excimer laser. The excimer laser was invented in 1970 by Nikolai Basov et al by using a xenon dimer (Xe2). This Xe2 excimer laser emitted at 172 nm, and with this a new class of lasers were invented.8 The first applications of the excimer lasers were within various research laboratories, including Avco Everett Research Laboratory, Sandia Laboratories, the Northrop Research and Technology Center, and the United States Government’s Naval Research Laboratory.9
The initial application of the excimer laser in the medical field emerged in 1983 from the collaboration of Rangaswamy Srinivasan and the ophthalmic surgeon Stephen Trokel.10,11 This collaboration led to the development of LASIK surgery procedure, which has been performed over 28 million times worldwide as of 2009. The excimer laser has been adopted by other medical disciplines such as cardiology, dentistry, and orthopedics.12–14
Bonis et al were the first to study the use of the 308 nm XeCl excimer laser in the field of dermatology in 1997. They investigated the use of excimer laser for treatment of 10 patients with chronic plaque psoriasis and concluded that it was an effective treatment option.15 Since its initial introduction to dermatology, use of the excimer laser as a treatment option has expanded to applications in many dermatologic diseases. Psoriasis treatment with excimer laser has proven to be effective even in early studies with Feldman et al demonstrating 84% of patients achieving a 75% or better improvement after 10 or fewer treatments (Figures 1 and 2). Excimer laser is currently indicated for adult and pediatric patients with mild, moderate, or severe psoriasis with <10% body surface area involvement and the American Academy of Dermatology states the level of evidence is II and the strength of recommendation is B. A literature search on PubMed was used with combinations of the terms “excimer”, “excimer laser”, “308 nm”, “psoriasis”, “protocol”, “safety”, “efficacy”, acceptability”, “side effects”, and “dose”. The search results were included if they contained information pertaining to excimer laser and psoriasis treatment and description of the safety, efficacy, and patient acceptability of the treatment.
  | Figure 1 Plaque type psoriasis on lower extremity prior to treatment with excimer laser. |
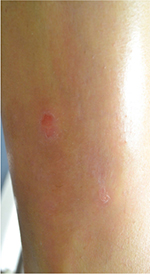  | Figure 2 Plaque type psoriasis on lower extremity after eight treatments with excimer laser according to MED protocol. Abbreviation: MED, minimal erythema dose. |
In this study, the main relevant literature pertaining to the excimer laser for the treatment of psoriasis will be reviewed.
Safety
Initially used in the treatment of refractory moderate plaque psoriasis, the 308 nm excimer laser uses UVB light to induce apoptosis, break DNA strands and, ultimately, decrease T-lymphocyte proliferation. The UVB emitted from the laser helps regulate the p53 tumor suppressor pathway inducing cell cycle arrest and deterring inflammatory processes.15 As a result, repigmentation of the treated areas is thought to occur due to elevated levels of peptide ET-1, as well as melanocyte re-migration and proliferation.1 With this knowledge, the utilization of the excimer laser has been expanded to include a host of various cutaneous diseases. In general, four main categories of cutaneous diseases can be currently treated with the 308 nm excimer laser: psoriatic lesions—which will be the focus of this review—apigmented and hypopigmented lesions, pruritic disorders, and follicular diseases.
When compared to the narrow band UVB laser, the 308 nm laser has an increased induction rate of T-cell apoptosis.1 Compared with traditional narrow band UV therapy, the excimer laser requires on average less number of treatment sessions and thus a smaller amount of cumulative UVB exposure. This aspect potentially reduces the patient’s skin cancer risk and can feasibly improve patient compliance.1 Furthermore, the excimer laser has the ability to target difficult to reach areas and administer site-specific dosing.16 Also, it can operate with the ability to change the energy level (in millijoules) delivered during treatment. Few adverse reactions have been reported, and they are consistent with adverse reactions associated with other forms of phototherapy including erythema, blistering, hyperpigmentation, and hypopigmentation (Figure 3).
  | Figure 3 Common side effects of the 308 nm excimer laser in the treatment of psoriasis. |
The 308 nm excimer laser was initially studied for the treatment of moderate plaque psoriasis by Bonis et al in 1997. This study suggests that nine sessions on average equating to a mean cumulative dose of 4.45 J UVB are adequate for complete plaque resolution. This dose was found to be lower than the dose reached with narrow band UVB treatment.15 Kemeny and colleagues further investigated the laser and found that patients treated at this dose remain lesion free for ~2 years.17 These initial studies were of smaller scale (n = 10). In the recent past, several groups have focused on larger scale studies that demonstrate the safety and use of the laser for individuals with mild to moderate localized plaque psoriasis. The laser is particularly useful if these individuals have a suboptimal response or contraindications to topical or intralesional treatments. These studies also confirm that an average of 10 treatments should clear the plaques.18–22
In addition to plaque psoriasis, the 308 nm laser is useful in the treatment of intertriginous psoriasis as demonstrated by a few case reports.23,24 Recently, split scalp studies have shown beneficial results of the laser in treating scalp psoriasis. Resolution in these patients generally requires more treatments than non-intertriginous psoriatic lesions. For example, one study demonstrated improvement with 21 sessions.25,26
Adjunctive topical therapies can also be used to augment the laser’s results. Several topicals have been studied including dithranol ointment, flumetasone/salicylic acid ointment, calcipotriol ointment, clobetasol spray, and calcitriol ointment.27–30 In one study by Rogalski et al, addition of dithranol ointment to the excimer laser protocol resulted in a reduced Psoriasis Area and Severity Index (PASI) score.27 Furthermore, use of flumetasone/salicylic acid ointment resulted in a lower cumulative UVB dose, as well as plaque improvement. Finally, use of clobetasol spray and ointment in conjunction with the excimer laser resulted in a safer side effect profile, as well as improved clearance of lesions in the long term.30
The 308 nm can also be used in the treatment of mild to moderate plaque psoriasis in children. A recent study by Pahlajani et al compares the safety and efficacy of the excimer laser for the treatment of mild to moderate plaque localized psoriasis in adults and children. On average, 12.5 (SD 2.64) treatments were needed for resolution in children, while 9.7 (SD 2.53) sessions were needed for adults. Common side effects associated with the laser were consistent with side effects seen in adult patients and included: hyperpigmentation, blistering, erosions, pain, and koebnerization.31 In general, side effects were more typical in the adult population with the most common one being erosions. Hyperpigmentation was the most common side effect in the pediatric group. Future studies pertaining to the safety of the 308 nm laser in the treatment of psoriasis will presumably include continued modification of the treatment protocol to reduce the number of treatments needed for plaque resolution, while still resulting in longer periods of plaque remission.
In addition to psoriasis, a vast number of other cutaneous diseases can also be treated with the excimer laser. As previously postulated, the 308 nm excimer laser plays a role in melanocyte re-migration and thus has been shown to be beneficial in the treatment of vitiligo and hypopigmented disorders. Various pruritic lesions treated with the 308 nm excimer laser have also demonstrated positive results. The stigmata of atopic dermatitis, including: erythema, infiltration, lichenification, excoriations and pruritus can severely impact a patient’s quality of life. Other conditions like lymphomatoid papulosis, granuloma annulare, Langerhans cell histiocytosis lichen planus, lichen planopilaris and localized scleroderma can also be treated with the excimer laser. Complete remission of cutaneous T-cell lymphoma has been demonstrated with biweekly excimer treatments. Finally, alopecia areata can be treated with the 308nm excimer laser. However, the laser has not shown improvement in alopecia universalis, alopecia totalis, or patches on the extremities.32
Efficacy
First described in 1997 by Bonis et al, the 308 nm excimer laser has become a major tool in the armamentarium of the dermatologist in treating various types of cutaneous diseases. Over the years the excimer laser has evolved in its clinical usage, and appropriately, so have the treatment protocols that are used in clinical practice. Several different treatment protocols have been developed and optimized to more effectively treat psoriatic lesions and to achieve greater improvements in the PASI score with fewer treatments. The three main protocols used for the treatment of psoriasis include: the minimal erythema dose (MED) protocol, the induration protocol, and the newer minimal blistering dose (MBD) protocol.30
MED protocol
The MED is established by first testing healthy, non-psoriatic skin and determining the minimal dose (millijoules) that causes a well-demarcated, minimally erythematous pink macule.33 Typically, with this method, the patient the will require two initial visits to calibrate the MED, with a total of 12 treatments sessions thereafter to reach PASI-75.18 Information pertaining to exact treatment dosages in terms of millijoules is limited, as studies only report cumulative doses at the end of the patient treatment course. One study by Asawanonda et al extrapolates dosing in millijoules from a mean MED of 203.3 mJ to correlate with ~3.248 mJ.21,22
Induration protocol
The induration-based protocol is another method for determining treatment dosing. Taneja and colleagues innovated this method whereby an initial dose is based on the induration component of the modified PASI and subsequent doses are based on the change in induration. Compared to the MED protocol, the induration method allows for clinicians to modify the dose as plaques begin to change in response to treatment. On average, plaques treated with this protocol achieved PASI-75 after 10 treatments.34
MBD protocol
One report published by Debbaneh et al describes using a minimal blister dose (MBD) for excimer laser treatment. This protocol identifies the minimum dose at which the patient will blister, and then subsequent treatments are administered at doses less than the MBD. In theory, this achieves the maximum possible dose that a plaque can sustain without blistering the skin. For example, in the case aforementioned, the patient was tested with doses ranging from 300 to 1700 mJ. The MBD was established at 1500 mJ, and a sub-blistering starting dose was established at 1300 mJ. The patient was then treated for 12 days following the initial treatment at a sub-blistering does of 800 mJ. At his 1-week follow up, the patient was noted to have achieved PASI-75.17
Patient acceptability
Although there have been no studies formally evaluating patient acceptability of the excimer laser treatment, the previously mentioned safety profile for excimer laser treatment of psoriasis makes it a generally well-tolerated treatment. The most commonly observed side effects are erythema, blistering, hyperpigmentation, and hypopigmentation.32 These side effects are typically observed only at the sites of treatment, they do not occur in all treatments, and are often well tolerated by patients. The excimer laser has been demonstrated to be an effective treatment option for psoriasis variants and locations that may be more difficult to treat with topical modalities.32
Scalp psoriasis
The scalp is involved in up to 80% of patients with psoriasis, and the excimer laser can be useful in the treatment of scalp psoriasis. Scalp psoriasis, especially when involving the hairline, can cause significant impairment in quality of life due to its visibility. Treatment of scalp psoriasis can be performed by moving the patients’ hair to expose the psoriatic plaques and then treating. This is often useful for patients with limited scalp involvement.35
Treatment of scalp psoriasis has been reported, but this modality presents challenges due to the difficulty of penetrating the laser through the hair. It must be noted however that the forehead, hairline, and retroauricular areas are not entirely covered by hair, and often treatment with the excimer laser is a viable option.36 Wong et al present a case of a 68-year-old female patient with generalized plaque psoriasis, also involving the hairline of the scalp. This scalp psoriasis was refractory to topical corticosteroids and acitretin. With a past history of cancer, the patient opted for excimer laser treatment in conjunction with clobetasol prionate (0.05%) spray twice daily. After 5 weeks of therapy (receiving a total of nine excimer laser treatments and clobetasol spray twice daily) the patients’ hairline psoriasis was completely cleared. It was reported that there were no side effects experienced, and the patients’ hairline remained clear during the entire duration of follow up, which was 3 months after therapy was completed.36
In a comparative study involving 13 patients with treatment refractory scalp psoriasis, the excimer laser was used for treatment in conjunction with a hair blow-dryer to help move the hair and deliver optimum laser penetration. Half of the scalp received excimer laser treatment, whereas the other half of the scalp served as a control. Over 15 weeks the difference in mean modified PASI scores between the excimer laser-treated site and the control site was statistically significant (P<0.001) with the excimer treatment group showing substantial improvement and clearance.37
In another study by Morison et al 35 patients with scalp psoriasis who had failed prior intensive topical therapy were treated with the excimer laser. Manual separation of the hair was used to provide access, and starting doses ranged from 300 to 1000 mJ depending on Fitzpatrick skin type. Treatment with the excimer laser was twice weekly, with a mean of 21 total treatments. All patients improved, and 49% of the patients cleared completely. Phototoxicity in the form of erythema and blistering occurred in all patients and was noted to be more prominent around the nape of the neck and on the ears.38
Nail psoriasis
The excimer laser can also be an excellent option for nail psoriasis, which can often be difficult to treat. In a comparison study the excimer laser versus the pulsed dye laser (PDL) was evaluated for the treatment of nail psoriasis in 42 patients. The right-hand nails were treated with excimer laser twice weekly for 12 weeks and the left-hand nails were treated with PDL once every 4 weeks for a total of 12 weeks. The patients were assessed with the Nail Psoriasis Severity Index (NAPSI). Although the PDL laser performed better than the excimer laser for the treatment of nail psoriasis, 38% of hands treated with the excimer laser achieved NAPSI-50, an improvement of at least 50% in nail psoriasis.39
Palmoplantar psoriasis
Palmoplantar pustular psoriasis is another subtype of psoriasis that can often be difficult to treat. There have been five prospective studies investigating the use of excimer laser in the treatment of palmoplantar pustular psoriasis. The combined analysis of these studies showed that $64 of patients with palmoplantar pustular psoriasis experienced an improvement of at least 70% at the end of treatment. This makes the excimer laser a viable treatment option for patients with palmoplantar pustular psoriasis.40,41
Combination therapy
Another advantageous aspect of the excimer laser is that it can be used in combination with other treatment modalities, and these often have a synergistic effect. Levin et al utilized a novel combination of excimer laser and clobetasol propionate spray and calcitriol ointment for the treatment of moderate to severe generalized psoriasis. In their 12-week study, patients received twice weekly treatment with the 308 nm excimer laser combined with clobetasol propionate twice daily for a month followed by calcitriol ointment twice daily for the subsequent month. Of the 30 patients enrolled 83% achieved PASI-75 or greater. This demonstrated that the combination of excimer laser with alternating clobetasol spray and calcitriol ointment is a promising option and can easily be implemented in any treatment involving the excimer laser.30
In another 12-week study Levin et al treated moderate to severe psoriasis patients with twice weekly excimer treatments combined with twice daily clobetasol propionate followed by calcitriol ointment twice daily. Of the 21 patients who completed the protocol, 76% achieved at least PASI-75 by week 12. This again supports the viability of using the excimer laser in combination treatment with other treatment modalities for psoriasis.42
Furthermore, Dong et al demonstrated that combination therapy with the excimer laser and flumetasone ointment achieved greater improvements in PASI scoring than excimer laser monotherapy, with combination treatment patients achieving an average PASI improvement of 82.51 and excimer monotherapy patients achieving an average PASI improvement of 72.01. This suggests that not only can the excimer laser be used in combination therapy, but it may even be more efficacious to utilize the laser in combination.43
Refractory treatment
Although the excimer laser is often not a first-line treatment for psoriasis patients, it can be useful in combination or in the treatment of patients who are refractory to other treatments (Figure 4). It has been demonstrated that the excimer laser can be an effective treatment option even for psoriasis that has failed treatment with biologic agents. Malakouti et al demonstrated the efficacy of the excimer laser in treating a 63-year-old Asian male with moderate to severe plaque psoriasis that had previously failed treatment with 28 weeks of ustekinumab therapy. The patient was subsequently treated with high-dose excimer laser therapy and demonstrated a rapid improvement in PASI scoring. Additionally, pretreatment and post-treatment biopsies were performed, and it was demonstrated that after treatment with high-dose excimer laser there was a 3-fold reduction in the number of live T cells found in the post-treatment biopsy. Although treatment with biologic agents can decrease the levels of inflammatory cytokines, the excimer laser has the ability to directly cause apoptosis of T cells and induce DNA damage in the antigen-presenting cells, which the authors attribute to the superior response observed from the excimer laser compared to ustekinumab.44
  | Figure 4 Psoriasis therapeutic armamentarium. |
It has also been demonstrated that patients with moderate to severe plaque psoriasis who have been refractory to treatment with etanercept and phototherapy have been successfully treated with the excimer laser. Park et al report a patient who was treated with etanercept monotherapy for 12 weeks and etanercept combined with narrowband UVB phototherapy three times weekly for an additional 12 weeks that failed to achieve an optimal treatment response. The patient was subsequently discontinued from all prior treatments and started on excimer laser treatments twice weekly. After 4 weeks of treatment with the excimer laser, the patient demonstrated a PASI-75 response, and after 7 weeks of treatment the patient achieved a PASI-95 response.45
Discussion
The 308 nm excimer laser is an excellent option for the treatment of psoriasis and has been demonstrated to be effective in many different ways. When considering the excimer laser for the treatment of psoriasis, it has become apparent that appropriate patient selection must be made. By the nature of the excimer laser, it is not as practical for monotherapy use in patients with severe plaque psoriasis, as the treatment field and practical application of the laser would make treatment a very time consuming and difficult process. However, when considering patients with mild to moderate psoriasis, it can be an extremely useful treatment. Patients who were assessed in the aforementioned studies were often patients with mild to moderate psoriasis. When treating patients with the excimer laser it is important to identify both the optimal patient candidate and the appropriate treatment protocol.
There were a variety of treatment protocols that were identified for the treatment of psoriasis with the excimer laser. The three main protocols that were identified were the MED protocol, the Induration protocol, and the MBD protocol. Each of these protocols make use of different features of the patients’ psoriasis to help determine the optimal dosimetry when utilizing the excimer laser. It became clear in assessing these various protocols that the most efficacious protocol was the MBD protocol, in which patients were treated all the way up to a sub-blistering starting dose, and followed accordingly with dose modulation as needed. This allowed researchers to achieve greater improvements in PASI score in a faster period of time. However, it is important to consider patient goals in treatment when identifying the appropriate treatment protocol. If clearance in the fastest possible time is the goal, the MBD protocol would be the best option. However, if patients are more concerned with side effects of blistering, erythema, and tenderness, then the MED or Induration protocols may be more advantageous. This is a discussion that should be had with patients and clinicians before treatment. Additionally, there is currently no long-term safety data on the effects of the more aggressive MBD treatment with regard to side effects and risk for long-term skin damage with high-dose treatments.
Overall, the 308 nm excimer laser is a very well tolerated treatment option for patients with psoriasis. The major side effects identified were erythema, tenderness, and blistering at the sites of treatment. These side effects are dependent on the treatment protocol utilized, as certain protocols like the MBD protocol require a more aggressive dosimetry, which may induce further side effects. Nonetheless, even with a sub-blistering dose, patients tolerated the treatment very well and in clinical experience even the blistering and erythema are often well tolerated compared to their untreated psoriasis. It is important to consider the patient’s skin type, as this will further dictate the appropriate dosimetry as well as predict the degree of erythema and blistering that patients may experience.
The excimer laser has also been demonstrated to be an excellent treatment option for difficult to treat psoriasis subtypes. The excimer laser can be used to treat palmoplantar pustular psoriasis, as well as scalp and nail psoriasis, which are historically hard to treat subtypes. Even psoriasis that has been refractory to systemic treatments have been demonstrated to show improvement with the excimer laser. It is possible that this is all related to the different mechanisms of action for the excimer laser compared to more systemic or biologic agents. Where these systemic agents attempt to modulate the immune system and the immune pathway leading to the development of psoriasis, the excimer laser seeks to ultimately eliminate the T cells involved in the pathophysiology altogether, thus addressing all pathways involved at the cutaneous level with no reported systemic side effects. Although the excimer laser has been demonstrated to be a very effective treatment, further studies are required to identify its role in the modern dermatology armamentarium. With the recent development of highly effective biologic and systemic agents, it may be difficult to justify the monotherapy of excimer laser alone in patients with moderate to severe psoriasis, but with the demonstrated efficacy in combination with topicals and the ability to improve symptoms of refractory psoriasis, the excimer laser should continue to remain an excellent treatment option.
Conclusion
Although the excimer laser is not a first-line treatment, it remains an excellent treatment option for psoriasis patients and has been demonstrated to be an effective treatment with little to no side effects. The excimer laser has been shown to be effective in difficult to treat psoriasis subtypes like palmoplantar pustular psoriasis, scalp, and nail psoriasis. It has been shown to be an effective treatment option in combination therapy with topicals as well as a treatment option for psoriasis refractory to systemic treatment. Appropriate patient selection is important when considering excimer laser treatment for psoriasis. Although it may be difficult to justify excimer laser monotherapy especially with the advent of highly efficacious biologic agents, the excimer laser remains an excellent option for the treatment of psoriasis and should be considered an adjunct treatment option with topical or systemic agents.
Acknowledgments
The authors thank Kristina Lee (University of California–San Francisco, Department of Dermatology, Psoriasis and Skin Treatment Center, San Francisco, CA, USA) and Rasnik Singh (University of California–Los Angeles, David Geffen School of Medicine, Los Angeles, CA, USA). This article has no funding source.
Disclosure
The authors report no conflicts of interest in this work.
References
Beggs S, Short J, Rengifo-Pardo M, Ehrlich A. Applications of the excimer laser: a review. Dermatol Surg. 2015;41(11);1201–1211. | ||
Mehraban S, Feily A. 308 nm excimer laser in dermatology. J Lasers Med Sci. 2014;5:8–12. | ||
Spencer JM, Hadi SM. The excimer lasers. J Drugs Dermatol. 2004:3;522–525. | ||
Lebwohl M. Psoriasis. The Lancet. 2003;361:1197–1204. | ||
Nestle F, Kaplan D, Barker J. Psoriasis. New Engl J Med. 2009;361:496–509. | ||
Gordon KB, Ruderman EM. Psoriasis and Psoriatic Arthritis. Physica-Verlag, Springer: Heidelberg. | ||
Kagen M, Cao LY, Oyetakin-White P, Tacastacas JD, Yan C, McCormick TS, Cooper KD. Single administration of lesion-limited high-dose (TURBO) UVB using the excimer laser: clinical clearing in association with apoptosis of epidermal and dermal T cell subsets in psoriasis. Photodermatol, Photoimmunol, Photomed. 2012;28:293–298. | ||
Basov N, Townes C, Prokhorov A. The Nobel Prize in Physics 1964. | ||
Stamm, U. et al. Excimer Laser. 2002;1010–1013. | ||
Trokel SL, Srinivasan R, Braren B. Excimer laser surgery of the cornea. Am J Ophthalmol. 1983;96(8):710–715. | ||
IBM News Room. Loughran M. President Obama honors IBM scientists with National Medal Of Technology And Innovation for Breakthrough That Enabled LASIK Surgery. [press release]. 2012. Available from https://www-03.ibm.com/press/us/en/pressrelease/39829.wss. 21 December 2012. | ||
Linsker R, Srinivasan R, Wynne JJ, Alonso DR. Far-ultraviolet laser ablation of atherosclerotic lesions. Lasers Surg Med. 1984;4:201–206. | ||
Glossop ND, Jackson RW, Koort HJ, Reed SC, Randle JA. The excimer laser in orthopaedics. Clin Orthop Relat Res. 1995;72–81. | ||
Frentzen M, Koort HJ, Thiensiri I. Excimer lasers in dentistry: future possibilities with advanced technology. Quintessence Int. 1992;23:117–133. | ||
Bonis B, Kemeny L, Dobozy A, et al. 308 nm UVB excimer laser for psoriasis. The Lancet. 1997;350:1522. | ||
Debbaneh MG, Levin E, Sanchez Rodriguez R, Leon A, Koo J, Rosenblum MD. Plaque-based sub-blistering dosimetry: reaching PASI-75 after two treatments with 308-nm excimer laser in a generalized psoriasis patient. J Dermatolog Treat. 2015;26:45–48. | ||
Kemeny L, Bonis B, Dobozy A, Bor Z, Szabó G, Ignácz F. 308-nm excimer laser therapy for psoriasis. Arch Dermatol. 2001;137:95–96. | ||
Feldman SR, Mellen BG, Housman TS, et al. Efficacy of the 308-nm excimer laser for treatment of psoriasis: results of a multicenter study. J Am Acad Dermatol. 2002;46:900–906. | ||
Menter A, Korman N, Elmets C, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis. J Am Acad Dermatol. 2010;62:114–135. | ||
Mudigonda T, Dabade T, Feldman S. A review of targeted ultraviolet B phototherapy for psoriasis. J Am Acad Dermatol. 2012;66:664–672. | ||
Asawanonda P, Anderson RR, Chang Y, Taylor CR. 308-nm excimer laser for the treatment of psoriasis: a dose-response study. Arch Dermatol. 2000;136:619–624. | ||
Trehan M, Taylor CR. High-dose 308-nm excimer laser for the treatment of psoriasis. J Am Acad Dermatol. 2002;46:732–737. | ||
Mafong EA, Friedman PM, Kauvar AN, et al. Treatment of inverse psoriasis with the 308 nm excimer laser. Dermatol Surg. 2002;28:530–532. | ||
Carrascosa JM, Soria X, Domingo H, Ferrandiz C. Treatment of inverse psoriasis with excimer therapy and tacrolimus ointment. Dermatol Surg. 2007;33:361–363. | ||
Gupta SN, Taylor CR. 308-nm excimer laser for the treatment of scalp psoriasis. Arch Dermatol. 2004;140:518–520. | ||
Morison WL, Atkinson D, Werthman L. Effective treatment of scalp psoriasis using the excimer (308 nm) laser. Photodermatol Photoimmunol Photomed. 2006;22:181–183. | ||
Rogalski C, Grunewald S, Schetschorke M, Bodendorf MO, Kauer F, Simon JC, Paasch U. Treatment of plaque-type psoriasis with the 308 nm excimer laser in combination with dithranol or calcipotriol. Int J Hyperthermia. 2012;28:184–190. | ||
Dong J, He Y, Zhang X, Wang Y, Tian Y, Wang J. Clinical efficacy of flumetasone/salicylic acid ointment combined with 308-nm excimer laser for treatment of psoriasis vulgaris. Photodermatol Photoimmunol Photomed. 2012;28:133–136. | ||
Wong JW, Nguyen TV, Bhutani T, Koo JY. Treatment of psoriasis and long-term maintenance using 308 nm excimer laser, clobetasol spray, and calcitriol ointment: a case series. J Drugs Dermatol. 2012;11:994–996. | ||
Levin E, Debbaneh M, Malakouti M, et al. Supraerythemogenic excimer laser in combination with clobetasol spray and calcitriol ointment for the treatment of generalized plaque psoriasis: interim results of an open label pilot study. J Dermatol Treat. 2015;26:16–18. | ||
Pahlajani N, Katz BJ, Lozano AM, Murphy F, Gottlieb A. Comparison of the efficacy and safety of the 308 nm excimer laser for the treatment of localized psoriasis in adults and in children: a pilot study. Pediatr Dermatol. 2005;22:161–165. | ||
Beggs S, Short J, Rengifo-Pardo M, Ehrlich A. Applications of the excimer laser: a review. Dermatol Surg. 2015;41(11):1201–1211. | ||
Mudigonda T, Dabade TS, Feldman SR. A review of protocols for 308 nm excimer laser phototherapy in psoriasis. J Drugs Dermatol. 2012;11:92–97. | ||
Taneja A, Trehan M, Taylor CR. 308-nm excimer laser for the treatment of psoriasis: induration-based dosimetry. Arch Dermatol. 2003;139:759–764. | ||
Guenther L. Current management of scalp psoriasis. Skin Therapy Lett. 2015;20:5–7. | ||
Wong JW, Kamangar F, Nguyen TV, Koo JY. Excimer laser therapy for hairline psoriasis: a useful addition to the scalp psoriasis treatment algorithm. Skin Therapy Lett. 2012;17:6–9. | ||
Taylor CR, Racette AL. A 308-nm excimer laser for the treatment of scalp psoriasis. Lasers Surg Med. 2004;34:136–140. | ||
Morison WL, Atkinson DF, Werthman L. Effective treatment of scalp psoriasis using the excimer (308 nm) laser. Photodermatol Photoimmunol Photomed. 2006;22:181–183. | ||
Al-Mutairi N, Noor T, Al-Haddad A. Single blinded left-to-right comparison study of excimer laser versus pulsed dye laser for the treatment of nail psoriasis. Dermatol Ther (Heidelb). 2014;4:197–205. | ||
Goldberg DJ, Chwalek J, Hussain M. 308-nm excimer laser treatment of palmoplantar psoriasis. J Cosmet Laser Ther. 2011;13:47–49. | ||
Sevrain M, Richard MA, Barnetche T, et al. Treatment for palmoplantar pustular psoriasis: systematic literature review, evidence-based recommendations and expert opinion. J Eur Acad Dermatol. 2014;28:13–16. | ||
Levin E, Debbaneh M, Malakouti M, et al. Supraerythemogenic excimer laser in combination with clobetasol spray and calcitriol ointment for the treatment of generalized plaque psoriasis: Interim results of an open label pilot study. J Dermatolog Treat. 2015;26:16–18. | ||
Dong J, He Y, Zhang X, Wang Y, Tian Y, Wang J. Clinical efficacy of flumetasone/salicylic acid ointment combined with 308-nm excimer laser for treatment of psoriasis vulgaris. Photodermatol Photoimmunol Photomed. 2012;28:133–136. | ||
Malakouti M, Brown GE, Sorenson E, Leon A, Koo J, Levin EC. Successful use of the excimer laser for generalized psoriasis in an ustekinumab non-responder. Dermatol Online J. 2015;21. | ||
Park KK, Swan J, Koo J. Effective treatment of etanercept and phototherapy-resistant psoriasis using the excimer laser. Dermatol Online J. 2012;18:2. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
