Back to Journals » Research Reports in Clinical Cardiology » Volume 12
Exaggeration of Non-Culprit Coronary Artery Stenosis in the Setting of Primary Percutaneous Coronary Intervention: A Single Center Observational Study
Authors Othman F , Abid AR, AlQahtani A, Gehani A, Al Suwaidi J, Arabi A
Received 12 October 2020
Accepted for publication 18 January 2021
Published 15 November 2021 Volume 2021:12 Pages 67—73
DOI https://doi.org/10.2147/RRCC.S280661
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Kones
Fahmi Othman,1 Abdul Rehman Abid,1 Awad AlQahtani,1 Abdurrazzak Gehani,2 Jassim Al Suwaidi,1 Abdulrahman Arabi1
1Heart Hospital, Hamad Medical Corporation, Doha, Qatar; 2Al-Ahli Hospital, Doha, Qatar
Correspondence: Fahmi Othman
Heart Hospital, Hamad Medical Corporation, PO Box 3050, Doha, Qatar
Tel +97466580459
Email [email protected]
Objective: We sought to evaluate if the non-culprit coronary artery stenosis severity is affected by primary percutaneous coronary intervention (PPCI) compared with non-PPCI settings.
Methods: Review of all the PPCI angiograms was performed at our catheterization laboratory between 15th October 2013 and 15th October 2014. All patients with severe multi-vessel coronary artery disease (MV CAD) who underwent second angiograms (either during the same admission or after discharge) were analyzed. Non-culprit lesions in the PPCI and non-PPCI angiograms were compared. Two investigators blinded to the procedure dates analyzed the severity of the lesions using validated quantitative coronary angiography software (QCA).
Results: Among 777 patients who underwent PPCI, 458 had multi-vessel disease. Additional angiography to treat non-culprit lesions was performed in 104, of these, 69 patients had a combined total of 74 lesions suitable for QCA analysis. The second angiogram was performed during the same admission (mean 4± 2.7 days) and after discharge (mean 115± 84 days) for 48 and 21 patients, respectively. Compared to PPCI angiograms, the non-PPCI angiograms showed a statistically significant reduction in the percentage of stenosis (71.6± 14.4% vs 64.5± 14.4%, p≤ 0.001), and an increase in minimal luminal diameter (0.82± 0.45 mm vs 1.00± 0.44 mm, p≤ 0.001) of non-culprit lesion. However, no significant difference was observed in the reference diameter (2.89± 0.69 mm vs 2.83± 0.64 mm, p=0.1) of the non-culprit lesion in both angiograms. Furthermore, these differences in the lesion parameters remain constant whether the second angiogram was performed during the same admission or performed after discharge (73.3± 14% and 66.2± 12.9% vs 68.4± 15% and 61.2± 16%, p=0.1).
Conclusion: The severity of non-culprit lesion is exaggerated in the PPCI setting. The non-culprit lesion exaggeration remains constant whether the second angiogram was performed early within a few days or later after several weeks.
Keywords: acute myocardial infarction, coronary angiogram, minimal lumen diameter, non-culprit lesion, primary percutaneous coronary intervention
Introduction
Multi-vessel coronary artery disease (CAD) has been observed in more than 50% of cases presenting with ST segment elevation myocardial infarction (STEMI) treated by PPCI. These cases have worse outcomes as compared to those with single-vessel disease.1
PCI for culprit artery versus multi-vessel PCI has been compared by observational studies, randomized controlled trials (RCTs), and meta-analyses with conflicting results.2–18
The experts recommend that ischemia should be relieved in the culprit and non-culprit related arteries at the time of PPCI.19
The best treatment strategy nevertheless for the non-culprit related artery (IRA) in patients presenting with STEMI and MV CAD remains unresolved. This issue has an important impact on potential improvement in clinical outcomes in these patients. PCI strategies include: (1) IRA only primary PCI with medical treatment of non-culprit arteries except if there is spontaneous angina or myocardial ischemia induced on stress testing; (2) to perform multi-vessel PCI at the time of primary PCI; or (3) IRA primary PCI, then staged PCI of non-culprit related arteries later during the same admission or early after discharge.20
New studies have reported that complete revascularization at the time of PPCI would be beneficial. The AHA ACC guidelines have Class IIb recommendation to do PCI for non-culprit related lesion at the time of PPCI, however the writing committee emphasizes that this change should not be considered as a routine for multi-vessel PCI in all patients with STEMI and MV CAD. To determine the optimal strategy physicians should keep in mind clinical data, lesion severity/complexity, and risk of contrast induced nephropathy prior to considering the timing of multi-vessel PCI.2
To further shed light on the controversy, we had an impression that the severity of non-culprit lesions was often overestimated at the time of PPCI, which affects the clinical decision making regarding non-culprit lesion revascularization. A retrospective analysis was performed for patients who underwent coronary angiography at the time of PPCI, followed by another coronary angiogram within nine months, in order to evaluate the severity of non-culprit lesions.
Methods
We examined our PPCI database and included all patients who had coronary angiography at the time of admission with acute STEMI (within 12 hours of chest pain with a view to primary PCI) between the 15th October 2013 and the 15th October 2014 and had a following coronary angiogram within a nine month period performed by using validated quantitative coronary angiography software (QCA).
All acute STEMI angiograms were reviewed by two experienced operators in the field to identify those patients who had a 70% obstruction lesions in the non-IRA (by visual estimation). The culprit lesion was identified as the site of acute occlusion in an epicardial coronary artery or an impaired (TIMI [Thrombolysis In Myocardial Infarction] 3) flow with conjunction of ST elevation at the ECG.
Non-culprit lesions were defined as lesions in non-infarct related artery with smooth angiographic borders and no associated thrombus. The additional angiograms were then assessed to ensure that the images were obtained in matching projections of the index angiogram. If there was a difference of more than 15° in any plane, they were excluded.
Patients were excluded if non-IRA lesions were revascularized at the time of PPCI either by PCI or CABG. Using the QCA-CMS system, end-diastolic images in the least foreshortened view were used to measure lesion severity.21 From both studies the first angiographic images were used. Two readers who were to the procedure data performed the analyses. Baseline characteristics recorded for every patient included age, gender, CAD risk factors (diabetes mellitus, hypertension, smoking history, dyslipidemia), previous history of coronary artery disease (past angina, AMI, PCI, or CABG), and hemodynamics at the start of each procedure (blood pressure and heart rate).
The data were analyzed using Statistical Package for Social Sciences (SPSS) version 19.0. Categorical variables were expressed as frequencies and percentages while continuous variables were mentioned as means±standard deviations. Paired t-test was used to compare lesion characteristics on angiography and hemodynamic data between the two studies. Student’s t-test was used to compare continuous variables between patient groups. Chi-square test was used to compare categorical variables between patient groups and p values were calculated. A p value of less than or equal to 0.05 was taken as significant.
Ethics
This study was approved by the Medical Research Council of Hamad Medical Corporation (IRB number #14493/14), since it was a retrospective study so the waiver of informed consent by patients was approved by the Medical Research Council. Patient data confidentiality was strictly observed as per the Institutional guidelines. The study complied with the Declaration of Helsinki.
Results
During the study period, 777 patients underwent coronary angiography at the time of acute STEMI for PPCI. Among these, 458 patients had multi-vessel disease. Additional angiography to treat non-culprit lesion was performed in 104 patients within nine months. Of these 104, 35 were excluded as the angiographic views were not matching. Leaving 69 patients with 74 non-culprit lesions suitable for analysis as shown in Figure 1.
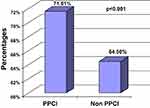 |
Figure 1 Minimal luminal diameter percentage stenosis in PPCI vs non-PPCI angiogram. |
Patient demographics in the study group are shown in Table 1. None of the patients received any vasopressor agents at the time of PPCI or follow-up coronary angiogram.
 |
Table 1 Demographics of Study Participants (N=69) |
Comparing the PPCI and non-PPCI angiograms there was a statistically significant reduction in percentage of stenosis (71.6±14.4% vs 64.5±14.4%, p≤0.001) and increase in minimal luminal diameter (0.82 ±0.45 mm vs 1.00±0.44 mm, p≤0.001) of the non-culprit lesion as shown in Figure 1. Furthermore, no statistically significant difference was observed in the reference diameter (2.89±0.69 mm vs 2.83±0.64 mm, p=0.1) of the non-culprit lesion among PPCI and non-PPCI angiograms. Comparing the PPCI and non-PPCI angiograms, the diastolic blood pressure was significantly higher, and there was a rising trend of systolic blood pressure with statistically insignificant association as shown in Table 2.
 |
Table 2 Non-Culprit Lesion Characteristics |
In order to study whether doing the non-PPCI angiogram during the same admission had an effect on the severity of non-culprit artery stenosis compared with after discharge, the patients were divided into two groups; the first group of 48 patients had their non-PPCI angiogram during the same admission (2 to 7 days from the day of admission) with a mean of 4 days, and the second group of 26 patients had the non-PPCI angiogram (between 1–9 months from discharge). The percentage of stenosis of non-culprit lesion between the PPCI and non-PPCI angiograms had decreased by 7.07% for the same index admission vs 7.13% in the after-discharge groups (Table 3). The findings were consistent among those who had the non-PPCI angiogram during the same admission vs after discharge; therefore, the severity of stenosis was 73.3±14% and 66.2±12.9% vs 68.4±15% and 61.2±16%, p=0.1 (Figure 2).
 |
Table 3 Timing of Second Angiogram |
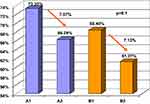 |
Figure 2 Stenosis severity in the same admission vs after discharge group. |
Patients who had their second angiogram during the same admission tended to have more severe stenosis as compared to those who had their angiogram after discharge (73.35% vs 68.40%).
Discussion
There are few studies that had shown exaggeration of non-culprit lesions in PPCI angiogram setting; and in most of these studies the second angiogram was performed weeks to months after discharge.
However, our study is the first in which the majority of second angiograms were done during the same admission (2 to 7 days).
Furthermore, those who had their second angiogram during the same admission tended to have more severe stenosis as compared to those after discharge (73.35% vs 68.40%).
This emphasized that the likely cause of non-culprit exaggeration is the unfavorable acute myocardial infarction (AMI) metabolic milieu. This unfriendly AMI situation and hypercoagulable status could possibly lead to vasoconstriction and slow flow in the non-culprit artery. Thus, suggesting a plausible etiology of non-IRA lesion exaggeration.
PPCI for the IRA has been a standard treatment in patients with STEMI. Multi-vessel disease can occur in approximately 50% of STEMI.1 Non-IRA lesions have a significance, as a pathophysiological inflammatory process in AMI could cause plaque instability.22
This study has demonstrated that the severity of non-culprit lesion is exaggerated in the AMI setting, however, there was no difference in the degree of exaggeration whether the angiogram was performed before or after discharge.
Hanratty et al23 observed that between primary PCI and follow-up angiographic studies there was a significant increase in minimal luminal diameter and a reduction in the percentage of stenosis of the non-IRA lesion without a significant change in the reference segment diameter – this was not a result of changes in medications or hemodynamics. It was observed that 21% of patients had >50% stenosis at PPCI angiogram that decreased to <50% in the second angiogram. PPCI versus non-PPCI setting was the only significant independent predictor of regression in non-IRA stenosis. The results of this study are in accordance with Hanratty et al. The number of patients was greater in our study as compared to Hanratty et al, 69 and 48 patients respectively. Furthermore, the stenosis percentage was greater in our study as compared to Hanratty et al, 71.6±14.4% and 49.3±14.5 respectively. This could explain the lower number of patients who had non-significant stenosis in the second angiogram, 6% in our study as compared to 21% in Hanratty et al.
Thim et al24 reported on STEMI patients in a cohort study, 24% were planned for re-evaluation of non-IRA lesions. Among these, 66% required further revascularization. Re-evaluation was performed either during the same admission or after discharge based on individual assessment. No events were reported in the non-IRA lesions during the waiting time for re-evaluation. Among 116 patients planned for follow-up evaluation, 100 patients underwent a new coronary angiogram as part of their evaluation. There were 146 non-IRA lesions in these 100 patients. Furthermore, this angiographic analysis was supported by using FFR, instantaneous wave-free ratio, intravascular ultrasound, and positron emission tomography. In contrast to Thim et al, we performed coronary angiogram to evaluate all patients and QCA was used for assessment of stenosis severity reviewed by two interventional cardiologists blinded to the study.
In the study by Thim et al, 34% of patients with STEMI and MVD, the same admission re-evaluation of non-IRA lesions did not exhibit significant regression at re-evaluation angiograms. Data by Thim et al suggest that supplementary functional assessment is frequently needed to distinguish the significant non-IRA lesions from those that are non-significant.
Thim et al provide real-time data on the management of non-IRA lesions detected during STEMI angiogram. Thim et al’s data support that staged evaluation in accordance with current guidelines is safe, with re-evaluation performed within 30 days; thus should be considered as the relevant control treatment for future randomized clinical trials focusing on complete primary revascularization in STEMI.
Our study results support the current AHA/ACC guidelines to treat the IRA lesion only during PPCI and are consistent with previous studies.
Findings based on recent RCTs,16,25–27 with regard to multi-vessel primary PCI in hemodynamically stable patients with STEMI, lead to change of the prior Class III recommendations to a Class IIb, to consider multi-vessel PCI, either at the time of PPCI or as a staged procedure. These four RCTs have suggested that a strategy of multi-vessel PCI, either at the time of PPCI or as a staged procedure, may benefit and be shown to be safe in selected patients with STEMI.16,25–27
Performing multi-vessel PCI during PPCI has several potential disadvantages. First, the procedure time is prolonged and incurs increased radiation exposure. Second, higher contrast volume administration during the procedure increases the risk of contrast-induced nephropathy, as well as acute volume overload, which can potentially lead to increased morbidity and mortality.28 Third, non-IRA stenosis severity may be acutely exaggerated because of circulating catecholamine-mediated vasoconstriction, and this can result in doing PCI for functionally insignificant stenoses.23 Fourth, the risk of inflicting injury to remote viable myocardium during PCI of non-IRA stenosis (distal embolization, no-reflow, side branch occlusion and loss of collateral circulation) could result in hemodynamic instability. Finally, in a prothrombotic and proinflammatory state there may be increased risk for acute and subacute stent thrombosis. Having more time to appropriately decide on the risks and benefits of additional revascularization may possibly result in better patient selection which is an advantage of the staged PCI strategy.29
Compared to patients with stable coronary artery disease, the degree of stenosis in non-IRA lesions at the time of STEMI is completely different. Subsequent adverse events can occur due to the “pro-inflammatory environment.” It is well known that in acute coronary syndrome vulnerable plaque distribution is generally not only limited to culprit lesions. Therefore, non-IRA lesions may not be stable.30
The desirable goal in multi-vessel disease patients is complete revascularization. However, the incomplete revascularization strategy may be preferred since it is easier to achieve and carries lower immediate risks, therefore it could be considered as a common clinical practice in many selected cases. Among these incompletely revascularized patients, the stenosis severity of non-IRA is expected to regress in subsequent evaluation.
Study Limitations
This study has a few limitations. Firstly, the study design is retrospective, where the study group may be subject to a selection bias. Secondly, 34 of 114 patients were excluded because of having >15º variation in the view’s angulation. Finally, the number of patients included in the final analysis was quite small.
Clinical Implications
Non-IRA PCI at the time of PPCI may lead to stenting lesions which may not require revascularization due to the lesion’s exaggeration. Furthermore, planning to perform PCI for non-IRA lesion several days after PPCI may be a reasonable option as the exaggeration of non-culprit lesions is likely going to improve.
Acknowledgments
The publication of this article was funded by the Qatar National Library. The abstract of this paper was presented as an oral presentation with interim findings at the AHA Scientific Sessions, 2015 Orlando, FL, USA.
There are no relationships with industry related to this study.
The authors deeply acknowledge the support provided by the Cath Lab team at Heart Hospital during the study period.
Disclosures
The authors report no conflicts of interest in this work.
References
1. Sorajja P, Gersh BJ, Cox DA, et al. Impact of multivessel disease on reperfusion success and clinical outcomes in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Eur Heart J. 2007;28:1709–1716. doi:10.1093/eurheartj/ehm184
2. Levine GN, Bates ER, Blankenship JC, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2016;133(11):1135–1147.
3. Hannan EL, Samadashvili Z, Walford G, et al. Culprit vessel percutaneous coronary intervention versus multivessel and staged percutaneous coronary intervention for ST-segment elevation myocardial infarction patients with multivessel disease. JACC Cardiovasc Interv. 2010;3:22–31. doi:10.1016/j.jcin.2009.10.017
4. Zhang D, Song X, Lv S, et al. Culprit vessel only versus multivessel percutaneous coronary intervention in patients presenting with ST-segment elevation myocardial infarction and multivessel disease. PLoS One. 2014;9(3):e92316. doi:10.1371/journal.pone.0092316.
5. Toma M, Buller CE, Westerhout CM, et al. Non-culprit coronary artery percutaneous coronary intervention during acute ST-segment elevation myocardial infarction: insights from the APEX-AMI trial. Eur Heart J. 2010;31:1701–1707. doi:10.1093/eurheartj/ehq129
6. Cavender MA, Milford-Beland S, Roe MT, et al. Prevalence, predictors, and in hospital outcomes of non-infarct artery intervention during primary percutaneous coronary intervention for ST-segment elevation myocardial infarction (from the National Cardiovascular Data Registry). Am J Cardiol. 2009;104:507–513. doi:10.1016/j.amjcard.2009.04.016
7. Corpus RA, House JA, Marso SP, et al. Multivessel percutaneous coronary intervention in patients with multivessel disease and acute myocardial infarction. Am Heart J. 2004;148:493–500. doi:10.1016/j.ahj.2004.03.051
8. Dziewierz A, Siudak Z, Rakowski T, et al. Impact of multivessel coronary artery disease and noninfarct-related artery revascularization on outcome of patients with ST-elevation myocardial infarction transferred for primary percutaneous coronary intervention (from the EUROTRANSFER Registry). Am J Cardiol. 2010;106:342–347. doi:10.1016/j.amjcard.2010.03.029
9. Engstrøm T, Kelbæk H, Helqvist S, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI 3-PRIMULTI): an open-label, randomised controlled trial. Lancet. 2015;386:665–671. doi:10.1016/S0140-6736(15)60648-1
10. Gershlick AH, Khan JN, Kelly DJ, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel Disease: the CvLPRIT trial. J Am Coll Cardiol. 2015;65:963–972. doi:10.1016/j.jacc.2014.12.038
11. Kornowski R, Mehran R, Dangas G, et al. Prognostic impact of staged versus “one-time” multivessel percutaneous intervention in acute myocardial infarction: analysis from the HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trial. J Am Coll Cardiol. 2011;58:704–711. doi:10.1016/j.jacc.2011.02.071
12. Manari A, Varani E, Guastaroba P, et al. Long-term outcome in patients with ST segment elevation myocardial infarction and multivessel disease treated with culprit-only, immediate, or staged multivessel percutaneous revascularization strategies: insights from the REAL registry. Catheter Cardiovasc Interv. 2014;84:912–922. doi:10.1002/ccd.25374
13. Politi L, Sgura F, Rossi R, et al. A randomised trial of target-vessel versus multi-vessel revascularisation in ST-elevation myocardial infarction: major adverse cardiac events during long-term follow-up. Heart. 2010;96:662–667. doi:10.1136/hrt.2009.177162
14. Bravo CA, Hijri SA, Bhatt DL, et al. Complete versus culprit-only revascularisation in ST elevation myocardial infarction with multi-vessel disease. Cochrane Database Syst Rev. 2017;5:CD011986. doi:10.1002/14651858.CD011986.pub2
15. Varani E, Balducelli M, Aquilina M, et al. Single or multivessel percutaneous coronary intervention in ST-elevation myocardial infarction patients. Catheter Cardiovasc Interv. 2008;72:927–933. doi:10.1002/ccd.21722
16. Wald DS, Morris JK, Wald NJ, et al. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med. 2013;369:1115–1123. doi:10.1056/NEJMoa1305520
17. Hlinomaz O. Multivessel coronary disease diagnosed at the time of primary PCI for STEMI: complete revascularization versus conservative strategy. Prague 13 trial. Available from: http://sbhci.org.br/wp-content/uploads/2015/05/PRAGUE-13-Trial.pdf.
18. Vlaar PJ, Mahmoud KD, Holmes DR
19. Hochman JS, Sleeper LA, Webb JG, et al. Early revascularization in acute myocardial infarction complicated by cardiogenic shock. SHOCK Investigators. Should we emergently revascularize occluded coronaries for cardiogenic shock. N Engl J Med. 1999;341:625–634. doi:10.1056/NEJM199908263410901
20. Bates ER, Tamis-Holland AJ, Bittl JA, O’Gara PT, Levine GN. PCI strategies in patients with ST-segment elevation myocardial infarction and multivessel coronary artery disease. J Am Coll Cardiol. 2016;68:1066–1081. doi:10.1016/j.jacc.2016.05.086
21. Keane D, Haase J, Slager CJ, et al. Comparative validation of quantitative coronary angiography systems. Results and implications from a multicenter study using a standardized approach. Circulation. 1995;91:2174–2183. doi:10.1161/01.CIR.91.8.2174
22. Kubo T, Imanishi T, Kashiwagi M, et al. Multiple coronary lesion instability in patients with acute myocardial infarction as determined by optical coherence tomography. Am J Cardiol. 2010;105(3):318–322. doi:10.1016/j.amjcard.2009.09.032
23. Hanratty CG, Koyama Y, Rasmussen HH, Nelson GIC, Hansen PS, Ward MR. Exaggeration of nonculprit stenosis severity during acute myocardial infarction: implications for immediate multivessel revascularization. J Am Coll Cardiol. 2002;40:911–916. doi:10.1016/S0735-1097(02)02049-1
24. Thim T, Egholm G, Olesen KKW, et al. Staged re-evaluation of non-culprit lesions in ST segment elevation myocardial infarction: a retrospective study. Open Heart. 2016;3:e000427. doi:10.1136/openhrt-2016-000427
25. Dambrink JH, Debrauwere JP, van ‘T Hof AW, et al. Non-culprit lesions detected during primary PCI: treat invasively or follow the guidelines? EuroIntervention. 2010;5:968–975. doi:10.4244/EIJV5I8A162
26. Stone GW, Maehara A, Witzenbichler B, et al. Intracoronary Abciximab and aspiration thrombectomy in patients with large anterior myocardial infarction: the INFUSE-AMI randomized trial. JAMA. 2012;307:1817–1826. doi:10.1001/jama.2012.421
27. Svilaas T, Vlaar PJ, van der Horst IC, et al. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med. 2008;358:557–567. doi:10.1056/NEJMoa0706416
28. Marenzi G, Assanelli E, Campodonico J, et al. Contrast volume during primary percutaneous coronary intervention and subsequent contrast induced nephropathy and mortality. Ann Intern Med. 2009;150:170–177.
29. Patel MR, Dehmer GJ, Hirshfeld JW, et al. ACCF/SCAI/STS/AATS /AHA/ASNC/HFSA/SCCT 2012 appropriate use criteria for coronary revascularization focused update: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, American Society of Nuclear Cardiology, and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2012;59:857–881.
30. Li-Xiang MA, Zhen-Hua LU, Le WANG, Xin DU, Chang-Sheng MA. Culprit vessel only versus “one-week” staged percutaneous coronary intervention for multivessel disease in patients presenting with ST-segment elevation myocardial infarction. J Geriatr Cardiol. 2015;12:226–231. doi:10.11909/j.issn.1671-5411.2015.03.001
 © 2021 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2021 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
