Back to Journals » Clinical Interventions in Aging » Volume 11
Evidence of functional declining and global comorbidity measured at baseline proved to be the strongest predictors for long-term death in elderly community residents aged 85 years: a 5-year follow-up evaluation, the OCTABAIX study
Authors Formiga F, Ferrer A , Padrós G, Montero A, Gimenez-Argente C, Corbella X
Received 28 November 2015
Accepted for publication 11 February 2016
Published 18 April 2016 Volume 2016:11 Pages 437—444
DOI https://doi.org/10.2147/CIA.S101447
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Francesc Formiga,1,2 Assumpta Ferrer,3 Gloria Padros,4 Abelardo Montero,1,2 Carme Gimenez-Argente,1 Xavier Corbella1,2,5
On behalf of the Octabaix study members
1Internal Medicine Department, Geriatric Unit, Hospital Universitari de Bellvitge, Institut Català de la Salut, 2Bellvitge Biomedical Research Institute, IDIBELL, L’Hospitalet de Llobregat, 3Primary Care Centre “El Plà”, Direcció d’Atenció Primària Costa de Ponent, Institut Català de la Salut, Sant Feliu de Llobregat, 4South Metropolitan Clinical Laboratory, Direcció d’Atenció Primària Costa de Ponent, Institut Català de la Salut, L’Hospitalet de Llobregat, 5Albert J Jovell Institute of Public Health and Patients, Faculty of Medicine and Health Sciences, Universitat Internacional de Catalunya, Barcelona, Spain
Objective: To investigate the predictive value of functional impairment, chronic conditions, and laboratory biomarkers of aging for predicting 5-year mortality in the elderly aged 85 years.
Methods: Predictive value for mortality of different geriatric assessments carried out during the OCTABAIX study was evaluated after 5 years of follow-up in 328 subjects aged 85 years. Measurements included assessment of functional status comorbidity, along with laboratory tests on vitamin D, cholesterol, CD4/CD8 ratio, hemoglobin, and serum thyrotropin.
Results: Overall, the mortality rate after 5 years of follow-up was 42.07%. Bivariate analysis showed that patients who survived were predominantly female (P=0.02), and they showed a significantly better baseline functional status for both basic (P<0.001) and instrumental (P<0.001) activities of daily living (Barthel and Lawton index), better cognitive performance (Spanish version of the Mini-Mental State Examination) (P<0.001), lower comorbidity conditions (Charlson) (P<0.001), lower nutritional risk (Mini Nutritional Assessment) (P<0.001), lower risk of falls (Tinetti gait scale) (P<0.001), less percentage of heart failure (P=0.03) and chronic obstructive pulmonary disease (P=0.03), and took less chronic prescription drugs (P=0.002) than nonsurvivors. Multivariate Cox regression analysis identified a decreased score in the Lawton index (hazard ratio 0.86, 95% confidence interval: 0.78–0.91) and higher comorbidity conditions (hazard ratio 1.20, 95% confidence interval: 1.08–1.33) as independent predictors of mortality at 5 years in the studied population.
Conclusion: The ability to perform instrumental activities of daily living and the global comorbidity assessed at baseline were the predictors of death, identified in our 85-year-old community-dwelling subjects after 5 years of follow-up.
Keywords: oldest old, mortality, comorbidity, instrumental activity of daily living
Introduction
Despite the increasing number of oldest old population worldwide, longitudinal studies specifically designed to assess mortality in subjects aged over 85 years (the current fastest growing population subgroup in many countries) are still scarce in medical literature.1–3
The ability to predict mortality by measuring functional status, on contrary to chronic conditions or usual laboratory tests, may increase as age increases.4 In younger subjects, aged 65 years or less, chronic conditions have been reported to predict mortality better rather than functional limitations, which were stronger predictors of death in people aged ≥90 years.5,6 However, elderly subjects aged ≥85 years are frequently unable to perform functional tests; thus, it has been suggested that the assessment of activities of daily living (ADL), rather than chronic conditions or laboratory biomarkers, may be a useful tool for short- and long-term prognostication of survival in such oldest old people.1
Predictive properties of chronic conditions, functional limitations, and several laboratory tests used as prognostic markers of survival in the oldest old community residents have been addressed separately in previously published studies. In the present study, our aim was to evaluate the predictive value of 5-year mortality by looking at different characteristics included in the geriatric assessment and by analyzing laboratory data carried out on 328 community residents included in the OCTABAIX study, aged 85 years at baseline. The global assessments included evaluation of functional and cognitive status, comorbidity, nutritional and falls risk, quality of life, social risk, long-term drug prescription, and laboratory analysis (including vitamin D, hemoglobin, cholesterol profile, CD4/CD8 ratio, and serum thyrotropin).
Methods
The OCTABAIX study
As described elsewhere, the OCTABAIX study was a cohort study that included a randomized controlled trial, undertaken with a primary purpose of falls and malnutrition prevention by intervention in 85-year-old subjects from the community.1,7 All community-dwelling inhabitants born in 1924 and registered at one of the seven primary health care centers in Baix Llobregat in Barcelona, Spain, were contacted. The combined population served by these health care teams includes ~210,000 inhabitants out of a total of 800,000 inhabitants in Baix Llobregat. The seven voluntary health care centers involved in other elderly assessments were of the same geographical area and had similar data regarding immigration percentage (11%) or population served. The study was double-blinded, and included 328 noninstitutionalized subjects. No criteria related to baseline health or cognitive status was applied to exclude patients. The only exclusion critera was to be institutionalized. There were no differences among respondents and nonresponders for the participation contact in terms of sex, health care center, or physician in charge. The institutional ethics committee of Fundació Gol i Gorina approved the design of the study and all patients – or the caregivers for those cognitively impaired subjects gave their written informed consent before enrollment. After recruitment, all subjects and caregivers were interviewed at their home or health care center by a nurse or a physician of the research team, all of them trained in geriatric care. The intervention consisted in providing exercise and nutritional recommendations to the subject and caregiver, as well as their primary care physician, for reducing the incidence of falls and the risk of undernutrition in this population. Control subjects only received a general primary care assessment. All participants were followed for a 3-year period, and received during the follow-up period two in-home visits from a member of the research team, who assessed falls and nutritional risk factors as primary outcome by using an algorithm. Secondary outcomes included a wide range of different geriatric characteristics. Sociodemographic data (sex, marital status, place of residence, studies, and living alone), comorbidity, and a comprehensive geriatric evaluation (functional, cognitive and nutritional status, social risk, gait, and risk of falls) were used for this evaluation.
Present study
On the basis of the OCTABAIX study, the present investigation evaluated the usefulness to predict mortality of the geriatric assessment carried out 5 years before, based on tools that are currently used in geriatric practice. Furthermore, we assessed if these results were modified by including laboratory tests, such as vitamin D levels, cholesterol, CD4/CD8 ratio, hemoglobin, and serum thyrotropin, of which may be associated with a higher risk of mortality in an older population.
Geriatric assessment at baseline
Functional status was measured using the Barthel index (BI)8 for basic ADL and the Lawton index9 (LI) for instrumental ADL. BI measures include questions about seven areas: feeding, bathing, personal hygiene, dressing, bowel/bladder control, getting on/off the toilet, and locomotion. A maximum score of 100 indicates that the subject is independent in physical function and the lowest score of 0 indicates a totally dependent state. The LI is an easy to administer assessment instrument that provides self-reported information about functional skills necessary to live in the community. LI score ranges from 0 (low function, dependent) to 8 (high function, independent). Historically, female were scored on all eight areas of function; males were not scored in the domains of food preparation, housekeeping, and laundering. However, we applied the current recommendations to assess all domains for both sexes.10 A limitation of the instrument includes the self-report or surrogate report method of administration rather than a demonstration of the functional task. Cognitive function was measured by the Spanish version of the Mini-Mental State Examination (MEC), which has a total score of 35. As recommended, we considered MEC scores ≤23 to indicate the presence of cognitive impairment.11 Nutritional status was assessed using the Mini Nutritional Assessment (MNA).12 The MNA score is based on 18 items covering four component subscores. The MNA score obtained (maximum 30 points) classifies the assessed subjects into three categories: 24–30, well-nourished; 17–23.5, at risk of malnutrition; and <17, malnourished. Gait was evaluated with the gait rating scale from the Tinetti Performance-Oriented Mobility Assessment that provides a final score, which ranges from 0 to 12, with a higher score indicating better gait performance.13 Patients and/or caregivers were asked about the number of falls in the last year. The Gijon scale was used for the social assessment.14 This scale is scored on a maximum of 24 points. Social risk scores are those between 10 and 14 and social problems exist with scores >15. Quality of life was assessed using the visual analogue scale of the quality of life test (EQ-VAS) of perceived health.15 The EQ-VAS records the respondent’s self-rated health on a 20 cm vertical, visual analogue scale with endpoints labeled “the best health you can imagine” (100) and “the worst health you can imagine” (0).
Comorbidity assessment
The Charlson score (CS) was used to measure overall comorbidity.16 It ranges from 0 to a theoretical maximum of 33, depending on the presence of certain diseases with assigned values. Age-adjusted CS was not used since all participants were 85 year olds. Cardiovascular risk factors such as high blood pressure, diabetes mellitus, and dyslipidemia were also recorded. Disease prevalence for ischemic cardiopathy, heart failure, chronic obstructive pulmonary disease (COPD), stroke, and dementia was determined on the basis of a data review from general practice records. The number of drugs used by prescription on a chronic basis was also recorded. In most cases, the physician who obtained the information was at the same time the one who usually cared for the patient, comorbidity data was therefore, not only derived from self-reports but also from chart reviews, test results, and prescription drug indications.
Laboratory measurements
Blood samples were drawn between 9 and 10 am. Hemoglobin, total leukocytes, and lymphocytes were measured on an automated counter. The World Health Organization’s definition of anemia defines this entity as a hemoglobin concentration below 12 g/dL in female and 13 g/dL in males and was used to determine the presence of anemia. T-lymphocyte subsets were determined by flow cytometry. Aliquots from peripheral blood samples were stained with the following fluorochrome-conjugated monoclonal antibodies in double combinations: anti-CD3-FITC (clone SK7)/anti-CD4-PE (clone SK3) and CD3-FITC (clone SK7)/anti-CD8-PE (clone SK1) were purchased from Becton Dickinson (San Jose, CA, USA). A minimum of 2,000 events per sample were acquired on a FACScalibur flow cytometer (Becton Dickinson). Forward light scatter and side light scatter parameters were used to gate viable lymphocytes. These gated lymphocytes were then analyzed by two-color immunofluorescence with CellQuest software (Becton Dickinson). A CD4:CD8 ratio (numbers of CD4 and CD8 cells) of ≤1.00 was used to identify individuals with a possible immune risk phenotype. The use of CD4 and CD8 percentages resulted in identical CD4:CD8 ratio categorization.17 Total cholesterol (CHOD-PAP, Roche Diagnostics, Basel, Switzerland) and serum HDL-C concentrations (HDL-C Plus, Roche Diagnostics) were measured by a direct enzymatic colorimetric method. Serum LDL-C concentrations were calculated using the Friedewald equation. The interassay coefficient of variation for HDL-C was <5.0%. All procedures were carried out with a modular system analyzer (Roche Diagnostics).18 Serum levels of 25(OH)D (25-hydroxyvitamin D) (radioimmunoanalyses, DiaSorin, Stillwater, MN, USA) were considered normal between 25 and 95 ng/mL.19 The detection limit of serum 25(OH)D was 5 nmol/L, the intraassay coefficient of variation was 5.6%, and the interassay coefficient was 9.2%. Serum 25(OH)D concentrations were used to assess vitamin D status. Hypovitaminosis D was considered as <25 ng/mL and deficiency <11 ng/mL. Plasma concentrations of thyrotropin (TSH) and free thyroxine (FT4) were measured using an electrochemiluminescence immunoassay based on the sandwich principle with monoclonal antibodies (Roche Diagnostics).20 The reference range was 0.25–5.0 mU/L for TSH and 10–26 pmol/L for FT4. Interassay coefficients of variation were 1.96%–3.56% for TSH and 1.91–3.68 for FT4. All laboratory measurements were carried out in the primary care Laboratori Clínic L’Hospitalet, while T-lymphocytes subsets and serum 25(OH)D concentrations were processed in the referral Laboratori Clínic of the Hospital Universitari de Bellvitge (Immunology and Biochemistry Services).
Outcome events
Mortality, measured as time-to-event data, was the main outcome of the present study. For that purpose, the vital status of the participants was annually evaluated during the 5 years of follow-up. Subjects were categorized as alive after 60 months of follow-up, or censored when they died, whichever occurred first. Mortality status and causes were determined by trained physician adjudicators on the basis of medical records from hospitalizations, emergency room visits, death certificates, and autopsy and coroner’s reports, when available. There was no loss of follow-up. Patients who survived were compared with those deceased.
Statistical analysis
Normally distributed continuous variables are reported as mean ± standard deviation (SD). Categorical variables are reported as proportions. The Student’s t-test was used to compare continuous variables, with a previous Levene test for equality of variances, while either the chi-square statistic or Fisher’s exact test was used to compare categorical or dichotomous variables. Cox models were adjusted between main outcome variables and predictors. The semiparametric Cox proportional hazards model analyses the relationship between a time-to-event response variable and adjusted baseline covariates. Proportional hazards and linearity (on continuous variables) assumptions were evaluated for the Cox models to determine the variables associated with 5-year mortality.
The variables entered into the model using a backward-stepwise approach were sex and all the geriatric and global comorbidity (not simple diseases as heart failure or COPD) variables with significant differences in the bivariate analysis, such as the BI, LI, MEC, Charlson comorbidity index, MNA, Tinetti gait scale, and chronic drugs prescription. The significance level was fixed at 5%. Since this is mainly an exploratory analysis and covariates associated with the main outcome variable are unknown or not fully understood, we performed an algorithm variable selection based solely on backward-stepwise approach. The variable selection process was supervised by clinical criterion in order to ensure the result’s reliability and meaningfulness. We repeated the model five times adding values of lipid profile (cholesterol total, HDL-C, and LDL-C), or adding vitamin D, hemoglobin, CD4/CD8 ratio, or serum thyrotropin, and the results did not change. An adjusted hazard ratio (HR) with a 95% confidence interval (CI) was used. The results were considered significant when P<0.05. All analyses were performed using SPSS version 15.0 statistical software (SPSS Inc., Chicago, IL, USA).
Results
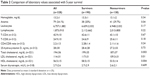
At baseline, the sample included 328 community-dwelling subjects aged 85 years, 202 (61.6%) of them were female. Geriatric assessment tools, cardiovascular risk factors, and comorbidity conditions are shown in Table 1. Table 2 shows the results of the laboratory analysis, which included hemoglobin, CD4/CD8 ratio, vitamin D, cholesterol profile, and serum thyrotropin.
Evaluation after 5-year follow-up
Of the total 328 participants, 138 (42.07%) died during the 5-year follow-up period; and of these, 75 (45.7%) belonged to the control group, those who only received a general primary care assessment, and 63 (38.4%) to the intervention group (P=0.18). The annual average mortality rate was 8.4% which was distributed as follows: 4.9% within the first year, 5.8% in the second, 6.7% in the third, 10.6% in the fourth, and 14% during the fifth year of follow-up. The comparison of death distribution by sex showed statistical significant differences: 75 (37.1%) females died out of the total 202, compared with 63 (50%) males who died out of the total 126 (P=0.02).
Predictors of mortality
The bivariate analysis of baseline variables associated with 5-year survival is shown in Table 1. Patients who survived were predominantly female and had a significantly better baseline functional status for both basic and instrumental ADL, better cognitive performance, lower comorbidity, lower nutritional risk, lower risk of falls, less percentage of heart failure and COPD, and they were taking less chronic prescription drugs. Table 2 shows laboratory test values associated with 5-year mortality compared between survivors and nonsurvivors. Among those variables that were significant at the bivariate level; multivariate Cox regression analysis (Table 3) identified two clinical variables that maintained significance – LI and Charlson comorbidity indexes – as independent predictors of 5-year risk of mortality in our cohort of elderly community residents aged 85 years at baseline. The addition to the Cox model of the serum values of hemoglobin, CD4:CD8 ratio, vitamin D, and cholesterol levels did not modify the value of the previously selected LI and Charlson index variables for predicting 5-year mortality, in the cohort of oldest old community-dwelling participants from the OCTABAIX study.
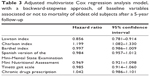  | Table 3 Adjusted multivariate Cox regression analysis model, with a backward-stepwise approach, of baseline variables associated or not to mortality of oldest old subjects after a 5-year follow-up |
Discussion
According to the present study, functional declining and global comorbidity are the strongest predictors for 5-year mortality in elderly community-dwelling subjects aged 85 years at baseline, rather than the measurement of usual blood laboratory tests classically associated with death. Results reaffirmed the clinical prognostic properties of comprehensive geriatric assessment in elderly community residents, in whom a better ability to perform instrumental ADL and the presence of a less number of comorbidity conditions, predict a chance for 5-year survival. In our population-based sample of community residents aged 85 years, we found a considerable mortality rate (42.07%) after a long-term follow-up of 5 years. This finding was consistent with the 46% reported in the Leiden 85+ study (5-year follow-up)21 and the 47.6% reported in the Newcastle 85+ study (6-year follow-up),2 two recent reports of reference in a population aged 85 years or older. As would be expected according to these earlier studies, our results also showed that annual average mortality rates clearly grew throughout the 5 years of follow-up, and were in accordance with the results of a previous study we took in other sample of nonagenarian individuals, which showed a mortality rate of 75% after 5 years of follow-up.6
Chronic conditions have been reported to be more predictive of all-cause mortality among younger individuals (aged 50–60 years) than functional limitations, which have been more predictive of mortality among elderly subjects (aged 80–99 years).1 Interestingly, results from the Leiden 85+ study showed that instrumental ADL ability (assessed using the Groningen activity restriction scale) was associated with an increased risk of mortality after 2 and 12 years of follow-up (HR 6.11 and 2.75, respectively).2 Our results suggested that both functional status and chronic conditions measured at baseline were the strongest predictors for 5-year mortality in our OCTABAIX study cohort of elderly community-dwelling adults aged 85 years. Furthermore, the extension from 3 to 5 years of follow-up in this cohort of subjects, clearly reaffirmed the previously documented prognostic properties of current geriatric assessment tools for predicting of living till 85- or 90-years old. In this cohort the instrumental had a better discriminative ability than the basic ADL, may be partly due to the high proportion of individuals with normal or almost normal baseline BI values. This hierarchical relationship between basic and instrumental ADL comported that disability in instrumental ADL was a more sensitive predictor of functional decline.22
In this group of very old patients, it was not surprising to find that the association between global comorbidity (Charlson Index) and 5-year mortality was stronger than other common diseases or cardiovascular risk factors. Furthermore, none of the variables associated with lower 5-year mortality, which lost significance in the multivariate analysis, was also surprising. Patients aged 85 years at baseline who survived 5 years of follow-up were predominantly female and they had significantly better baseline functional status for basic ADL, better cognitive performance, lower nutritional risk, lower risk of falls, less percentage of heart failure and COPD, and were taking less chronic prescription drugs, an item closely related to comorbidity.
A recently published Leiden 85+ study reported that the number of abnormalities in seven routine laboratory measurements predicts 5-year mortality as accurately as gait speed and instrumental ADL disability.21 When we evaluated blood laboratory tests that individually could be associated with increased risk of mortality, results found that anemia and low levels of total cholesterol, HDL cholesterol, and LDL cholesterol were associated with a higher risk of 5-year mortality; while CD4/CD8 ratio, levels of vitamin D and thyroid hormone were not. When each of these variables were incorporated separately in the logistic regression model for 5-year mortality analysis, all of them resulted in changing the model, and reaffirmed the significance of the previously identified IL and Charlson index as the associated independent variables.
In accordance with the previous results of several published studies in persons aged ≥85 years, anemia increased mortality in these population, with a mortality HR reported of 1.41 for prevalent anemia and 2.08 for incident anemia.23 Similarly, previously results of the OCTABAIX cohort showed that mortality was higher among the group of patients with anemia, and this finding reached statistically significant differences after 3 years of follow-up.24 In the present study, a new evaluation after 5 years of follow-up, showed that the association persisted but with less statistical power, and the signification was lost after the multivariate analysis.
Recent data evaluating the relationship between cholesterol and mortality in the oldest old pointed out a line of thinking that could explain some of the results found in our present study. Conversely as it occurs in younger people, it has been suggested that low levels of total cholesterol – and even lower LDL cholesterol – might determine a worse prognosis in very old people, while high concentrations of HDL would be protective as it is in normal populations.25,26 Thus, in our case, the contradictory results found may justify the loss of statistical significance.
Even though it has been found in several studies in elderly people aged 85 years or older,3 hypovitaminosis D – which was showen in more than a half of our participants aged 85 years at baseline27 – was not able by itself to demonstrate association with mortality at either 3 years,19 nor at 5 years of follow-up. Moreover, an inverted CD4:CD8 ratio as an immune risk phenotype has been correlated with survival rates in elderly people;28 however, after 5 years of follow-up, these results could not be confirmed in our cohort of elderly community residents, as it had also not been shown during the first 3 years of follow-up.17 Finally, even it has been reported as an association between low thyroid function (high levels of thyrotropin) and longevity,29 it could not be demonstrated in our 85-year-old inhabitants in whom the thyroid function was normal at baseline in majority of the cases.20
Limitations
There are some limitations that have to be considered: first, despite the study being an extremely homogeneous study sample of subjects, its size was relative small, a fact that makes difficult the extension and generalization of the results showen; second, geriatric measurements were taken at baseline, so it remains unknown whether periodic performance of geriatric assessment and/or laboratory tests throughout the age-decline follow-up might better predict mortality, also keeping in mind that the laboratory test included were analyzed individually and not grouped to build a score;30 and finally, the analysis did not take into account the impact of possible beneficial or harmful external interventions applied during the 5-year follow-up, such as those related to the caregivers’ support given to subjects for preventing falls and malnutrition, or the occurrence of adverse events related to hospital admission episodes.
Conclusion
In conclusion, even 5 years later, the present study reaffirmed the clinical value of a comprehensive geriatric assessment performed in elderly community residents. In the difficult step to reach from 85 to 90 years (four out of ten do not get there), a better ability to perform instrumental ADL and the presence of a less number of comorbidity conditions at baseline are the predictors for 5-year mortality identified in oldest old community-dwelling subjects aged 85 years, instead of the individual measurement of usual laboratory tests classically associated with death.
Acknowledgments
Members of the OCTABAIX Study: J Almeda (Unitat de Suport a la Recerca de Costa de Ponent, IDIAP J Gol), T Badia (ABS Martorell Urbano), A Lobato (ABS Sant Andreu de la Barca), C Fernández (CAP Rambla), A Ferrer (CAP El Pla), F Formiga (UFISS de Geriatría, Servicio de Medicina Interna, Hospital Universitari de Bellvitge), A Gil (ABS Sant Andreu de la Barca), MJ Megido (ABS Just Oliveras), G Padrós (Laboratori Clínic L’Hospitalet), M Sarró (CAP Florida Nord), and A Tobella (ABS Martorell Rural)
Disclosure
The authors report no conflicts of interest in this work.
References
Formiga F, Ferrer A, Chivite D, Montero A, Sanz H, Pujol R; Octabaix Study Members. Utility of geriatric assessment to predict mortality in the oldest old: the Octabaix study 3-year follow-up. Rejuvenation Res. 2013;16:279–284. | ||
Taekema DG, Gussekloo J, Westendorp RG, de Craen AJ, Maier AB. Predicting survival in oldest old people. Am J Med. 2012;125:1188–1194. | ||
Granic A, Aspray T, Hill T, et al. 25-hydroxyvitamin D and increased all-cause mortality in very old women: the Newcastle 85+ study. J Intern Med. 2015;277:456–467. | ||
Lee SJ, Go AS, Lindquist K, Bertenthal D, Covinsky KE. Chronic conditions and mortality among the oldest old. Am J Public Health. 2008;98:1209–1214. | ||
Formiga F, Ferrer A, Mascaró J, Ruiz D, Olmedo C, Pujol R. Predictive items of one-year mortality in nonagenarians. Aging Clin Exp Res. 2007;19:265–268. | ||
Formiga F, Ferrer A, Chivite D, Rubio-Rivas M, Cuerpo S, Pujol R. Predictors of long-term survival in nonagenarians: the NonaSantfeliu study. Age Ageing. 2011;40:111–116. | ||
Formiga F, Ferrer A, Sanz H, Marengoni A, Alburquerque J, Pujol R; Octabaix study members. Patterns of comorbidity and multimorbidity in the oldest old: the Octabaix study. Eur J Intern Med. 2013;24:40–44. | ||
Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. A simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Md State Med J. 1965;14:61–65. | ||
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. | ||
Vergara I, Bilbao A, Orive M, Garcia-Gutierrez S, Navarro G, Quintana JM. Validation of the Spanish version of the Lawton IADL Scale for its application in elderly people. Health Qual Life Outcomes. 2012;10:130. | ||
Lobo A, Saz P, Marcos G, et al. Revalidación y normalización del Mini-Examen Cognoscitivo (primera versión en castellano del Mini-mental Status Examination) en la población general geriátrica. [Revalidation and standardization of the cognition mini-exam (first Spanish version of the Mini-Mental Status Examination) in the general geriatric population]. Med Clin (Barc). 1999;112:767–774. | ||
Guigoz Y, Vellas B, Garry PJ. Assessing the nutritional status of the elderly: the Mini Nutritional Assessment as part of the geriatric evaluation. Nutr Rev. 1996;54 (suppl):59–65. | ||
Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34;119–126. | ||
Alarcón MT, González JI. La escala sociofamiliar de Gijón, instrumento útil en el hospital general. [The sociofamiliar scale of Gijon, useful instrument in the general hospital]. Rev Esp Geriatr Gerontol. 1998; 33:178–180. | ||
Herdman M, Badia X, Berra S. El EuroQol-5D: Una alternativa sencilla para medir calidad de vida relacionada con salud en atención primaria. [EuroQol-5D: a simple alternative for measuring health-related quality of life in primary care]. Aten Primaria. 2001;28:425–430. | ||
Charlson ME, Pompei P, Ales KL, MacKenzie CR.A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. | ||
Formiga F, Ferrer A, Padros G, Cintra A, Pujol R. Inverted CD4:CD8 ratio is not associated with three-year mortality in a sample of community-dwelling oldest old: the OCTABAIX immune study. J Nutr Health Aging. 2014;18:425–428. | ||
Formiga F, Ferrer A, Chivite D, et al. Serum high-density lipoprotein cholesterol levels correlate well with functional but not with cognitive status in 85-year-old subjects. J Nutr Health Aging. 2012;16:449–453. | ||
Formiga F, Ferrer A, Megido MJ, Boix L, Contra A, Pujol R; Octabaix study members. Low serum vitamin D is not associated with an increase in mortality in oldest old subjects: the Octabaix three-year follow-up study. Gerontology. 2014;60:10–15. | ||
Formiga F, Ferrer A, Padros G, Contra A, Corbella X, Pujol R; Octabaix Study Group. Thyroid status and functional and cognitive status at baseline and survival after 3 years of follow-up: the OCTABAIX study. Eur J Endocrinol. 2013;170:69–75. | ||
van Houwelingen AH, den Elzen WP, Mooijaart SP, et al. Predictive value of a profile of routine blood measurements on mortality in older persons in the general population: the Leiden 85-plus study. PLoS One. 2013;8:e58050. | ||
Spector WD, Katz S, Murphy JB, Fulton JP. The hierarchical relationship between activities of daily living and instrumental activities of daily living. J Chronic Dis. 1987;40:481–489. | ||
den Elzen WP, Willems JM, Westendorp RG, de Craen AJ, Assendelft WJ, Gussekloo J. Effect of anemia and comorbidity on functional status and mortality in old age: results from the Leiden 85-plus Study. CMAJ. 2009;181:151–157. | ||
Contreras MD, Formiga F, Ferrer A, Chivite D, Padrós G, Montero A; Grupo Octabaix. Perfil y pronóstico del paciente con anemia mayor de 85 años que vive en la comunidad. [Serum high-density lipoprotein cholesterol levels correlate well with functional but not with cognitive status in 85-year-old subjects]. Estudio Octabaix. Rev Esp Geriatr Gerontol. 2015;50:211–215. | ||
Takata Y, Ansai T, Soh I, et al. Serum total cholesterol concentration and 10-year mortality in an 85-year-old population. Clin Interv Aging. 2014;9:293–300. | ||
Lv YB, Yin ZX, Chei CL, et al. Low-density lipoprotein cholesterol was inversely associated with 3-year all-cause mortality among Chinese oldest old: data from the Chinese Longitudinal Healthy Longevity Survey. Atherosclerosis. 2015;239:137–142. | ||
Formiga F, Ferrer A, Almeda J, San Jose A, Gil A, Pujol R. Utility of geriatric assessment tools to identify 85-years old subjects with vitamin D deficiency. J Nutr Health Aging. 2011;15:110–114. | ||
Strindhall J, Nilsson BO, Löfgren S, et al. No immune-risk profile among individuals who reach 100 years of age: findings from the Swedish NONA immune longitudinal study. Exp Gerontol. 2007;42:753–761. | ||
Gussekloo J, van Exel E, de Craen AJ, Meinders AE, Frölich M, Westendorp RG. Thyroid status, disability and cognitive function, and survival in old age. JAMA. 2004;292:2591–2599. | ||
Howlett SE, Rockwood MR, Mitnitski A, Rockwood K. Standard laboratory tests to identify older adults at increased risk of death. BMC Med. 2014;12:171. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.