Back to Journals » Infection and Drug Resistance » Volume 15
Evaluation of the MeltPro Myco Assay for the Identification of Non-Tuberculous Mycobacteria
Authors Lin J , Zhao Y, Wei S , Dai Z, Lin S
Received 2 April 2022
Accepted for publication 10 June 2022
Published 22 June 2022 Volume 2022:15 Pages 3287—3293
DOI https://doi.org/10.2147/IDR.S369160
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Suresh Antony
Jian Lin,1,2 Yong Zhao,1,2 Shuzhen Wei,1,2 Zhisong Dai,1,2 Shufang Lin1,2
1Institute of Tuberculosis Control and Prevention, Fujian Center for Disease Control and Prevention, Fuzhou, People’s Republic of China; 2Fujian Provincial Key Laboratory of Zoonosis Research, Fujian Center for Disease Control and Prevention, Fuzhou, People’s Republic of China
Correspondence: Shufang Lin; Jian Lin, Institute of Tuberculosis Control and Prevention, Fujian Center for Disease Control and Prevention, No. 386, Chong’an Road, Xindian Town, Jin’an District, Fuzhou, Fujian, 350011, People’s Republic of China, Tel/Fax +86 591 8343 1464, Email [email protected]; [email protected]
Purpose: The purpose of this study was to evaluate a new commercial kit for Mycobacterium species identification and compare its results with that of the commonly used GenoType Mycobacterium CM assay. In addition, we were committed to identifying the main frequent species of nontuberculous mycobacteria (NTM) in Fujian.
Methods: A total of 261 clinical strains, collected at the Center for Disease Control and Prevention of Fujian Province, China, were preliminarily identified as NTM based on p-nitrobenzoic acid (PNB) growth test. The genomic DNA of all 261 strains was extracted and subjected to species identification using MeltPro Myco assay and GenoType Mycobacterium CM assay. The results of the latter were used as a control to calculate the positive agreement, negative agreement, agreement and the total agreement of the former. For samples with inconsistent detection results, sequencing was performed for verification.
Results: Compared to GenoType Mycobacterium CM assay, the total agreement of MeltPro Myco assay was 96.55% (252/261 strains). Both the positive and negative agreement of MeltPro Myco assay in identifying M. intracellulare, M. abscessus, M. kansasii, M. fortuitum, M. avium, M. gordonae, M. scrofulaceum, and mixed infections were higher than 99.00%, but the positive agreement of M. chelonae was relatively low at only 33.33%. In Fujian, the predominant strain of NTM was M. intracellulare (64.36%, 130/202 strains), followed by M. abscessus (19.31%, 39/202 strains), M. kansasii (4.46%, 9/202 strains), and M. fortuitum (3.96%, 8/202 strains).
Conclusion: The reliability of MeltPro Myco assay for identifying mycobacterium species was strongly demonstrated in this study, which greatly supports its usage for the clinical identification of mycobacteria. The present study also showed that the distribution of mycobacteria in Fujian, China, was significantly different from that in other regions and provided important data for future epidemiological study of NTM.
Keywords: evaluation, line probe assay, nontuberculous mycobacteria, species identification
Introduction
Nontuberculous mycobacteria (NTM) are a type of saprophytic bacteria that are naturally found in soil, air, and water.1 More than 200 species or subspecies of NTM have been discovered.2 While some of them are not pathogenic, others can cause infection in people of old age and co-infect people with HIV, or any other immunocompromising disease. Approximately 50 species of NTM act as opportunistic pathogens and are involved in the development of diseases.3–6
NTM cause numerous diseases in humans, and an increasing rate of NTM infections worldwide has unveiled an important challenge.7–11 According to previous reports, the rate of NTM cases in China increased from 4.3% in 1979 to 11.1% in 2000 and finally to 22.9% in 2010.12 The NTM infection rate has also increased because of an increase in HIV infections, as NTM is more likely to be prevalent among immunocompromised populations. Even countries such as the United States, Canada, and regions such as Taiwan with low tuberculosis (TB) incidences have a higher prevalence of NTM than TB.8,13,14
Diseases caused by NTM are easily mistaken for TB infections because both have similar clinical manifestations; however, NTM shows more resistance to anti-TB drugs, with more than 80% of the microbes being resistant against first- and second-line anti-TB drugs.2,15 In addition, different species of NTM show different levels of sensitivity and resistance to different drugs; therefore, the regimen design for each patient is different.16–20
An accurate method for identifying NTM infections also allows for the management and treatment of infected patients along with the implemented epidemiological control methods to reflect the specific mycobacterial species encountered. Although there are documented diagnostic criteria for NTM diseases from the American Thoracic Society, not all species have been tested to ensure that this diagnostic standard is universally suitable for all NTM respiratory pathogens.2 Therefore, further research on the identification of NTM species is required.
GenoType Mycobacterium CM assay is based on the line probe assay (LPA) and is used to differentiate NTM species within a culture.21–23 This commercial kit is widely utilized in clinical units and laboratories and is highly recognized, as it is recommended by the World Health Organization (WHO). Therefore, in this study, we used the results from this kit as the technical standard.
Recently, a new commercial kit named MeltPro Myco assay was developed to identify NTM species from sputum samples as well as cultures.24 The kit is based on unique multicolor melting curve analysis (MMCA) and can identify 19 clinically relevant Mycobacterium species. It had performed well in a previous study,24 and so we aimed in this study to further evaluate its performance by comparing it to that of GenoType Mycobacterium CM assay.
Materials and Methods
The Source of Strains
In total, 261 strains cultured in the BACTEC MGIT 960 Mycobacterial Detection System (Becton Dickinson, Baltimore, MD, USA) were collected from March 2018 to December 2019 from the Center for Disease Control and Prevention of Fujian Province, China. They were preliminarily identified as NTM by growth test in presence of p-nitrobenzoic acid (PNB).25
Genome DNA Extraction
Genomic DNA was extracted from 261 strains using the Lab-Aid 824S DNA extraction instrument (Zeesan Biotech, Xiamen, China).
GenoType Mycobacterium CM Assay
GenoType Mycobacterium CM assay (Hain Life Science, Nehren, Germany) was performed to identify mycobacteria species, according to the manufacturer’s instructions. The assay was run on a GT-Blot 48 (Hain Life Science, Nehren, Germany). The volume of the PCR mixture was 50 μL, comprised of 35 μL PNM, 5 μL 10x PCR buffer for HotStarTaq DNA Polymerase (Qiagen, Germany), 2 μL 25 mM MgCl2 solution, 1 U HotStarTaq DNA Polymerase, 3 μL deionized water, and 5 μL DNA solution. PCR was performed by denaturation steps at 95℃ for 15 min, 10 cycles of 95℃ for 30s and 58℃ for 2 min, 20 cycles of 95℃ for 25s, 53℃ for 40s, and 70℃ for 40s, followed by an extension at 70℃ for 8 min. After PCR completion, the results were automatically analyzed by the integrated software.
MeltPro Myco Assay
MeltPro Myco assay was run on a Slan-96S real-time PCR system (Zeesan Biotech, Xiamen, China). For sample detection, 25 μL of extracted DNA were added to the reaction tubes prefilled with a lyophilized PCR mixture. The running program involved decontamination at 50℃ for 2 min, denaturation at 95℃ for 10 min, 55 cycles of 95℃ for 15s, 57℃ for 20s and 78℃ for 20s, followed by denaturation at 95℃ for 2 min, and hybridization at 45℃ for 2 min. During hybridization, the temperature was increased from 45℃ to 90℃ at a ramp rate of 0.04℃/s. When the running program had finished, the built-in software (MeltPro Manager version 1.0; Zeesan Biotech) analyzed the results, following the result interpretation guidelines.
Verification and Confirmation
For strains with inconsistent detection results or the strains identified as Mycobacterium spp. in MeltPro Myco assay and GenoType Mycobacterium CM assay, the ITS region between the 16S rRNA and 23S rRNA genes was used for Sanger sequencing to confirm the strain.24 For the mixed infection strains, Mycobacterium tuberculosis complex (MTBC) was confirmed using the MTBC test kit (Zeesan Biotech, Xiamen, China) that targets the IS6110 gene, M. avium was confirmed with the detection of a specific IS901 gene, and M. intracellulare was confirmed with the detection of a specific DT1 gene.24
Statistical Analysis
Positive agreement, negative agreement, agreement and total agreement of MeltPro Myco assay compared to GenoType Mycobacterium CM assay were calculated. The precision of the estimates was reported using 95% CIs. Agreement between the two methods was assessed using the kappa statistic. All statistical analysis was performed using SPSS 17.0 software (SPSS Inc, Chicago, USA).
Ethics Statement
Ethics approval was obtained from the Ethical Committee of the Fujian Province Center for Disease Control (CDC) for the use of residual specimens received for routine diagnostic testing.
Results
Results of the Detection of 261 Strains by GenoType Mycobacterium CM Assay and MeltPro Myco Assay
In total, 261 strains were subjected to identification using GenoType Mycobacterium CM assay and MeltPro Myco assay (Table 1). Both methods detected eight species of mycobacteria. GenoType Mycobacterium CM assay identified 21 MTBC, 196 NTM, 9 mixed infections, 6 Mycobacterium spp., and 29 negative samples. MeltPro Myco assay identified 26 MTBC, 197 NTM, 9 mixed infections, 6 Mycobacterium spp., and 23 negative samples. Using the results of GenoType Mycobacterium CM assay as the control, both the positive and negative agreement of MeltPro Myco assay in identifying M. intracellulare, M. abscessus, M. kansasii, M. fortuitum, M. avium, M. gordonae, M. scrofulaceum, and mixed infections were found to be higher than 99.00%. The negative agreement of MeltPro Myco assay for identifying M. chelonae was 100.00%, while the positive agreement for this species was relatively low at only 33.33%. The total agreement of MeltPro Myco assay was 96.55% (252/261 strains).
 |
Table 1 Comparison of MeltPro Myco Assay and GenoType Mycobacterium CM Assay |
Results of nine samples were inconsistent after identification by both the assays: one sample was identified as M. intracellulare by GenoType Mycobacterium CM assay, but noted as MTBC in MeltPro Myco assay. Six samples were identified as negative by GenoType Mycobacterium CM assay but identified as M. intracellulare (n=1), M. kansasii (n=1), and MTBC (n=4) by MeltPro Myco assay. Two samples were identified as M. chelonae by GenoType Mycobacterium CM assay but identified as M. abscessus by MeltPro Myco assay.
Verification of Inconsistent Samples and Mixed Infection Samples by Sanger Sequencing
For the nine samples with inconsistent results, Sanger sequencing was performed to verify the results by targeting the ITS region between the 16S rRNA and 23S rRNA genes (Table 2). The verification results of six samples were consistent with MeltPro Myco assay, while the results of three samples were consistent with the results of GenoType Mycobacterium CM assay.
 |
Table 2 List of Discrepant Results and Validation with Sequencing |
For the nine mixed infection samples, the MTBC test kit and the specific gene were used to verify the results (Table 3). The results showed that these nine samples contained MTBC, as identified using an MTBC test kit. Sequencing analysis by targeting a specific IS901 gene showed that sample FZ 052 contained M. avium, while the remaining eight samples contained M. intracellulare as determined by targeting specific DT1 genes. The verification results were consistent with the results of MeltPro Myco assay.
 |
Table 3 List of Mixed Infection Samples and Validation with MTBC Test Kit and Sequencing |
Six samples identified as Mycobacterium spp. by the two kits were verified as M. arupense, M. peregrinum, M. phocaicum, M. sinense, M. vanbaalenii, and M. dioxanotrophicus by Sanger sequencing.
Ratios of Identified Mycobacterium Species
Among the 261 samples, 202 samples were NTM, accounting for 77.39% strains (202/261 strains), 24 samples were MTBC, accounting for 9.20% strains (24/261 strains), 9 samples with mixed infection, accounting for 3.45% strains (9/261 strains), and 26 samples were negative, accounting for 9.96% strains (26/261 strains) (Table 4).
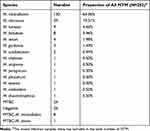 |
Table 4 Summary of Mycobacterium Species Identification of 261 Strains |
Among the 202 NTMs, M. intracellulare was the most abundant, accounting for 64.36% of the strains (130/202 strains), followed by M. abscessus (19.31%, 39/202 strains), M. kansasii (4.46%, 9/202 strains), and M. fortuitum (3.96%, 8/202 strains). Comparatively, there were fewer M. avium (1.98%, 4/203 strains), M. gordonae (1.49%, 3/202 strains), and M. scrofulaceum (0.99%, 2/202 strains) identified. In addition, the other seven species were rare with only one of M. chelonae, M. arupense, M. peregrinum, M. phocaicum, M. sinense, M. vanbaalenii, and M. dioxanotrophicus each identified.
Discussion
Recently, the overall prevalence of NTM diseases has increased globally and is becoming an emerging health issue. The incidence of pulmonary disease caused by NTM is on the rise,2,26 and that of HIV co-infection has also seen a sudden increase.4,5 However, it is difficult to differentiate NTM-caused diseases from MTBC-caused diseases.27 Furthermore, most NTMs are difficult to treat because of their resistance to the drugs used to treat TB infection in all healthcare systems including public, private, and TB-specific hospitals.2,15,28
In this study, we comparatively evaluated the clinical performance of MeltPro Myco assay, using GenoType Mycobacterium CM assay as a control. Herein, 261 samples were identified as NTM positive using the conventional PNB growth tests, then were subjected to strain evaluation using these two methods. Compared with GenoType Mycobacterium CM assay, the positive and negative agreement of MeltPro Myco assay to identify Mycobacterium species were confident (≥98%), except for M. chelonae with identification confidence of only 33.3% due to the only three samples enrolled.
Nine samples were inconsistently identified by the two assays. One sample (FZ 174) was identified as M. intracellulare by GenoType Mycobacterium CM assay, but as MTBC by MeltPro Myco assay and sequencing. A possible reason for this observation is that the sample may have been contaminated during the processing for GenoType Mycobacterium CM assay, or there was a cross-reaction with MTBC in the specific probe to detect M. intracellulare in GenoType Mycobacterium CM assay. Furthermore, two samples (FZ 160 and FZ 190) were identified as M. chelonae by GenoType Mycobacterium CM assay, but as M. abscessus by MeltPro Myco assay and sequencing. A possible explanation for this observation is that there may have been a cross-reaction in the specific probe used to detect M. chelonae in GenoType Mycobacterium CM assay. It is important to distinguish between M. abscessus and M. chelonae because their treatment regimens are different. However, many of the current commercial kits, including GenoType Mycobacterium CM assay, do not distinguish between the two species or differentiate them poorly. In this study, MeltPro Myco assay showed excellent ability to distinguish between the two species. Six samples were identified as negative by GenoType Mycobacterium CM assay, while MeltPro Myco assay identified four MTBC, one M. kansasii, and one M. intracellulare. Sequencing results proved that three of these samples were negative, while the remaining three matched with the results of the latter. A possible reason for this observation is that the DNA concentration of these samples was relatively low, so they were not detected by GenoType Mycobacterium CM assay or Sanger sequencing; however, MeltPro Myco assay, with its relatively high sensitivity, could detect these six samples as positive. All six samples were identified as gram-positive bacteria by GenoType Mycobacterium CM assay. In summary, nine inconsistent samples were verified by sequencing, which proved that the detection results of six samples by MeltPro Myco assay were correct, and the detection results of the other three samples by GenoType Mycobacterium CM assay were accurate.
Moreover, six samples were identified as Mycobacterium spp. using the two test kits, but no specific Mycobacterium species were identified. After sequencing, they were found to be uncommon pathogens, thereby explaining why neither of the kits could identify them as specific strains of Mycobacterium.
In Fujian Province, the most frequent NTM species was M. intracellulare (64.36%), followed by M. abscessus (19.31%), M. kansasii (4.46%), M. fortuitum (3.96%), M. avium (1.98%), M. gordonae (1.49%), and M. scrofulaceum (0.99%). Compared to other areas of China, these frequencies of NTM showed obvious differences,12,16–20 demonstrating that the distribution rate of different NTM species varied geographically and had obvious regional features, even within the same country.
One limitation of this study is that some species covered by the MeltPro Myco assay were not detected among the clinical samples. This is mainly due to the limited sample size and sample types, which were relatively uncommon or restricted to respiratory samples. Further study is needed on larger sample size and those nonrespiratory sample types, such as tissues or pus, so that a comprehensive coverage of NTM species might be achieved.
In summary, MeltPro Myco assay is a molecular method that can rapidly and accurately identify NTM species. It has a lower limit of detection than GenoType Mycobacterium CM assay and Sanger sequencing. We expect that MeltPro Myco assay will become a useful tool of routine use in the clinical setting.
Acknowledgments
We thank all of the persons involved in this study for their essential work and support. We also wish to thank Xiamen Zeesan Biotech Co. Limited for their technical support for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Falkinham JO
2. Forbes BA, Hall GS, Miller MB, et al. Practical guidance for clinical microbiology laboratories: mycobacteria. Clin Microbiol Rev. 2018;31(2):e00038–17. doi:10.1128/CMR.00038-17
3. Larsson LO, Polverino E, Hoefsloot W, et al. Pulmonary disease by non-tuberculous mycobacteria - clinical management, unmet needs and future perspectives. Expert Rev Respir Med. 2017;11(12):977–989. doi:10.1080/17476348.2017.1386563
4. Kobayashi T, Nishijima T, Teruya K, et al. High mortality of disseminated non-tuberculous mycobacterial infection in HIV-infected patients in the antiretroviral therapy era. PLoS One. 2016;11(3):e0151682. doi:10.1371/journal.pone.0151682
5. Varley CD, Ku JH, Henkle E, Schafer SD, Winthrop KL. Disseminated nontuberculous mycobacteria in HIV-infected patients, Oregon, USA, 2007–2012. Emerg Infect Dis. 2017;23(3):533–535. doi:10.3201/eid2303.161708
6. Zhang ZX, Cherng BPZ, Sng LH, Tan YE. Clinical and microbiological characteristics of non-tuberculous mycobacteria diseases in Singapore with a focus on pulmonary disease, 2012–2016. BMC Infect Dis. 2019;19(1):436. doi:10.1186/s12879-019-3909-3
7. Marras TK, Chedore P, Ying AM, Jamieson F. Isolation prevalence of pulmonary non-tuberculous mycobacteria in Ontario, 1997–2003. Thorax. 2007;62(8):661–666.
8. Billinger ME, Olivier KN, Viboud C, et al. Nontuberculous mycobacteria-associated lung disease in hospitalized persons, United States, 1998–2005. Emerg Infect Dis. 2009;15(10):1562–1569. doi:10.3201/eid1510.090196
9. Sood G, Parrish N. Outbreaks of nontuberculous mycobacteria. Curr Opin Infect Dis. 2017;30(4):404–409. doi:10.1097/QCO.0000000000000386
10. Prevots DR, Marras TK. Epidemiology of human pulmonary infection with nontuberculous mycobacteria: a review. Clin Chest Med. 2015;36(1):13–34. doi:10.1016/j.ccm.2014.10.002
11. Donohue MJ, Wymer L. Increasing prevalence rate of nontuberculous mycobacteria infections in five states, 2008–2013. Ann Am Thorac Soc. 2016;13(12):2143–2150. doi:10.1513/AnnalsATS.201605-353OC
12. Yu X, Liu P, Liu G, et al. The prevalence of non-tuberculous mycobacterial infections in mainland China: systematic review and meta-analysis. J Infect. 2016;73(6):558–567. doi:10.1016/j.jinf.2016.08.020
13. Damaraju D, Jamieson F, Chedore P, Marras TK. Isolation of non-tuberculous mycobacteria among patients with pulmonary tuberculosis in Ontario, Canada. Int J Tuberc Lung Dis. 2013;17(5):676–681. doi:10.5588/ijtld.12.0684
14. Chien JY, Lai CC, Sheng WH, Yu CJ, Hsueh PR. Pulmonary infection and colonization with nontuberculous mycobacteria, Taiwan, 2000–2012. Emerg Infect Dis. 2014;20(8):1382–1385. doi:10.3201/eid2008.131673
15. Griffith DE, Aksamit T, Brown-Elliott BA, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175(4):367–416. doi:10.1164/rccm.200604-571ST
16. Nie W, Duan H, Huang H, Lu Y, Chu N. Species identification and clarithromycin susceptibility testing of 278 clinical nontuberculosis mycobacteria isolates. Biomed Res Int. 2015;2015:506598. doi:10.1155/2015/506598
17. Wang X, Li H, Jiang G, et al. Prevalence and drug resistance of nontuberculous mycobacteria, northern China, 2008–2011. Emerg Infect Dis. 2014;20(7):1252–1253. doi:10.3201/eid2007.131801
18. Pang Y, Tan Y, Chen J, et al. Diversity of nontuberculous mycobacteria in eastern and southern China: a cross-sectional study. Eur Respir J. 2017;49(3):1601429. doi:10.1183/13993003.01429-2016
19. Liu H, Lian L, Jiang Y, et al. Identification of species of nontuberculous mycobacteria clinical isolates from 8 provinces of China. Biomed Res Int. 2016;2016:2153910. doi:10.1155/2016/2153910
20. Tan Y, Su B, Shu W, et al. Epidemiology of pulmonary disease due to nontuberculous mycobacteria in Southern China, 2013–2016. BMC Pulm Med. 2018;18(1):168. doi:10.1186/s12890-018-0728-z
21. Russo C, Tortoli E, Menichella D. Evaluation of the new Genotype Mycobacterium assay for identification of mycobacterial species. J Clin Microbiol. 2006;44(2):334–339. doi:10.1128/JCM.44.2.334-339.2006
22. Mäkinen J, Marjamäki M, Marttila H, Soini H. Evaluation of a novel strip test, Genotype Mycobacterium CM/AS, for species identification of mycobacterial cultures. Clin Microbiol Infect. 2006;12(5):481–483. doi:10.1111/j.1469-0691.2006.01380.x
23. Gitti Z, Neonakis I, Fanti G, Kontos F, Maraki S, Tselentis Y. Use of the GenoType Mycobacterium CM and AS assays to analyze 76 nontuberculous mycobacterial isolates from Greece. J Clin Microbiol. 2006;44(6):2244–2246. doi:10.1128/JCM.02088-05
24. Xu Y, Liang B, Du C, et al. Rapid identification of clinically relevant mycobacterium species by multicolor melting curve analysis. J Clin Microbiol. 2019;57(1):e01096–18. doi:10.1128/JCM.01096-18
25. Singh AK, Maurya AK, Umrao J, et al. Role of GenoType(®) Mycobacterium common mycobacteria/additional species assay for rapid differentiation between mycobacterium tuberculosis complex and different species of non-tuberculous mycobacteria. J Lab Physicians. 2013;5(2):83–89. doi:10.4103/0974-2727.119847
26. Dastranj M, Farahani A, Hashemi Shahraki A, et al. Molecular identification and distribution of non-tuberculous mycobacteria isolated from clinical specimens by PCR-sequencing method in West of Iran. Clin Respir J. 2018;12(3):996–1002. doi:10.1111/crj.12617
27. Mohajeri P, Yazdani L, Shahraki AH, et al. Verification of frequency in species of nontuberculous mycobacteria in Kermanshah drinking water supplies using the PCR-sequencing method. Microb Drug Resist. 2017;23(3):359–364. doi:10.1089/mdr.2016.0064
28. Khosravi AD, Mirsaeidi M, Farahani A, et al. Prevalence of nontuberculous mycobacteria and high efficacy of d-cycloserine and its synergistic effect with clarithromycin against mycobacterium fortuitum and mycobacterium abscessus. Infect Drug Resist. 2018;11:2521–2532. doi:10.2147/IDR.S187554
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
