Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 13
Evaluation of the Effect of an Aqueous Extract of Azadirachta indica (Neem) Leaves and Twigs on Glycemic Control, Endothelial Dysfunction and Systemic Inflammation in Subjects with Type 2 Diabetes Mellitus – A Randomized, Double-Blind, Placebo-Controlled Clinical Study
Authors Pingali U , Ali MA, Gundagani S, Nutalapati C
Received 28 July 2020
Accepted for publication 26 September 2020
Published 17 November 2020 Volume 2020:13 Pages 4401—4412
DOI https://doi.org/10.2147/DMSO.S274378
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Usharani Pingali, Mohammed Abid Ali, Srinivas Gundagani, Chandrasekhar Nutalapati
Department of Pharmacology and Therapeutics, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana 500073, India
Correspondence: Usharani Pingali Email [email protected]
Purpose: Neem tree (Azadirachta indica) offers different bioactives ranging from pesticides to therapeutic molecules, depending on which part of the plant is used and the extraction methodology and the solvent used. This study was aimed at evaluating the safety and efficacy of a standardized aqueous extract of Azadirachta indica leaves and twigs (NEEM) on glycemic control, endothelial dysfunction, and systemic inflammation in patients with type 2 diabetes mellitus (T2DM).
Methods: In this randomized, double-blind, placebo-controlled clinical study (RCT), 80 T2DM subjects, who have already been on standard metformin therapy, received either 125 mg, 250 mg, 500 mg of NEEM or placebo twice daily for 12 weeks. Postprandial blood sugar level (PPBS), fasting blood sugar level (FBS), glycosylated hemoglobin (HbA1c), insulin resistance (IR), endothelial function, oxidative stress, systemic inflammation, IL-6 and TNF-α, platelet aggregation and lipid profile were assessed. Adverse drug reactions, if any, were noted. GraphPad Prism 8 was used to perform statistical analysis.
Results: NEEM at the doses of 125, 250, and 500 mg BID significantly reduced PPBS (from 194.4± 14 to 173.1± 12.8mg/dL, 192.3± 17.1 to 161.8± 9.7mg/dL, and 205.9± 7.2 to 159.3± 7.1mg/dL, respectively), FBS (from 119.2± 5.0 to 109.2± 5.7mg/dL, 115.5± 4.4 to 103.7± 4.2mg/dL, and 120.7± 4.2 to 97.3± 3.7mg/dL, respectively), HbA1c (from 6.87 ± 0.4% to 6.64 ± 0.4%, 7.52 ± 0.4% to 6.86 ± 0.3%, and 7.78 ± 0.2% to 6.26 ± 0.4%, respectively), and IR (from 4.5 ± 1.2 to 3.4 ± 0.9, 3.8 ± 1.1 to 2.5 ± 0.6, and 4.6 ± 1.3 to 2.0 ± 0.6, respectively) compared to placebo. Also, NEEM significantly improved endothelial function, decreased oxidative stress and systemic inflammation compared to placebo. The efficacy was significant with all the doses, but no effect on platelet aggregation or lipid profile was observed.
Conclusion: NEEM may significantly ameliorate hyperglycemia, endothelial dysfunction, and systemic inflammation, on top of what metformin could do, in subjects with T2DM.
Keywords: Azadirachta indica, neem, hyperglycemia, insulin resistance, endothelial dysfunction, type 2 diabetes, metformin
Introduction
Diabetes mellitus (DM) is a critical health problem, affecting the global population. The prevalence and future of diabetes, of which type 2 diabetes (T2DM) comprises the most, the economic burden, the complicating factors and how diabetes impacts cardiovascular disease (CVD) are described in several publications.1–4 Endothelial dysfunction5 (EnD), Insulin resistance6 (IR), oxidative stress7 and hyperglycemia contribute to CVD.
T2DM often exhibits serum elevations of pro-inflammatory mediators, including sialic acid, a-1 acid glycoprotein, amyloid A, interleukin-1β, tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), C-reactive protein, and cortisol, which also exacerbate CVD.9–12
Neem (Azadirachta indica; family: Meliaceae), a tropical evergreen tree, is widely distributed in Asia. Neem leaves13 and seeds14 are used in Ayurveda as a household remedy. Different bioactive compounds have been isolated from neem leaves, such as nimbin, azadirachtin, nimbidiol, quercetin, nimbidin, etc.13 Many in vitro and in vivo studies have reported hypoglycemic activity of neem extracts, made with different solvents.15–20 Azadirachtin,21 Nimbidiol22 and Gedunin and Azadiradione23 also showed anti-hyperglycemic activity, but toxicity is of concern with these bioactives. Aqueous neem leaf and twig extract used in this study does not contain these bioactives, and showed good anti-hyperglycemic activity in our pre-clinical studies.
Thus, the objective of the present study is a controlled clinical study to evaluate an aqueous extract of neem leaves and twigs (NEEM) primarily in hyperglycemia.
Methods and Materials
We performed this 12-week prospective, randomized, single-center, double-blind, placebo-controlled clinical trial (RCT) between December 2018 to July 2019 at the Department of Clinical Pharmacology and Therapeutics, Nizam’s Institute of Medical Sciences (NIMS), Hyderabad, India.
Enrollment of Study Subjects
Ninety-four subjects, who have already been on a standard therapy of metformin, were screened from the outpatient department of NIMS. The participants received an information package containing an informed consent form, background information of the study, and a description of the intended care as per study protocol. Informed consent was obtained from each patient before study enrollment.
Inclusion Criteria
Patients of either sex, aged between 30 and 65 years with fasting plasma glucose levels of 110–126 mg/dL, glycosylated hemoglobin (HbA1c) levels between 6.5% and 8%, under the antidiabetic treatment (metformin 1500–2500 mg/day) for the past 8 weeks before the screening visit, diagnosed with endothelial dysfunction defined as ≤6% change in reflection index (RI) on post salbutamol challenge test, were included in the study. The patients have been explained the risks and benefits of the study, and they willfully provided written informed consent.
Exclusion Criteria
The patients with severe uncontrolled diabetes (HbA1c > 8% and FBS > 210 mg/dl), uncontrolled hypertension (SBP>180mmHg and DBP>100mmHg), high levels of serum Triglycerides (>500mg/dl), or impaired hepatic or renal function (AST and ALT elevation >3 times upper limit of normal; serum creatinine >1.5 mg/dl), were excluded from this study. The patients with any serious disease requiring active treatment or patients receiving any other herbal supplements were also excluded from the study.
Ethical Consideration
The study was conducted following the Declaration of Helsinki (2013) and ‘Guidelines for Clinical Trials on Pharmaceutical Products in India – GCP Guidelines issued by the Central Drugs Standard Control Organization, Ministry of Health, and Government of India. As required by the ethics committee for a study in patients, subjects enrolled for the study were on standard therapy with metformin. IRB approval was received from NIMS (EC/NIMS/2301/2019 36th ESGS No:798/2018). Ethics committee notifications as per Good Clinical Practice Guidelines, Central Drugs Standard Control Organization and Ethical Guidelines for Biomedical Research on Human Subjects, issued by the Indian Council of Medical Research, were followed. This clinical study has been registered in the clinical trial registry, India -CTRI/2018/12/016666 [registered on: 13/12/2018].
Link: http://ctri.nic.in/Clinicaltrials/showallp.php?mid1=29882&EncHid=&userName=CTRI/2018/12/016666
Investigational Products
Capsules of the standardized aqueous extract of the leaves and twigs of neem (PhytoBGS®), 125 mg and 250 mg strengths, and matching placebo capsules were received from Natreon Inc, New Brunswick, NJ, USA. Placebo capsules contained microcrystalline cellulose, croscarmellose sodium, fumed silicon dioxide and magnesium stearate as excipients.
Bioactive Composition of PhytoBGS®
The bioactives quantified by HPLC-PDA are flavonoids consisting of quercetin-3-O-glucoside, quercetin-3-O-rutinoside, apigenin rutinoside and rutin derivatives. The bioactive quantified by HPLC-ELSD is myo-inositol monophosphate, which appears to be the most predominant bioactive.
Randomization and Blinding
After screening, we randomized the eligible subjects using a computer-based predetermined randomized formation (GraphPad Prism version 8) in a 1:1:1:1 ratio using unstratified blocks of the same length and assigned the subjects to one of the four treatment groups. The randomization and group assignment were concealed both from doctors and subjects.
All the study medications were formulated as hard gelatin capsules having identical size, shape, color, texture, and weight, and they were packed in identical (both appearance and weight) and tamper-proof containers. The bottles containing the test products contained sequentially designated numbers and were dispensed by the pharmacist to the subjects as per the randomly allocated sequence.
During data collection, the research coordinators, the study investigators, and the attending care personnel were prohibited to access the randomization codes and allocations. Unblinding was allowed only after completion of the entire data collection process or in case of serious adverse events.
After the completion of the study period, the allocations were unblinded to tabulate the data, but the identity of the study groups was undisclosed to the data analysts. The data were double entered and blinded to the statisticians.
Study Groups
Group A: Placebo – Two identical capsules of placebo, twice daily administration (BID)
Group B: NEEM125: 1 capsule of neem 125 mg + 1 placebo capsule, BID − (250 mg/day dose of NEEM)
Group C: NEEM250: 1 capsule of neem 250 mg + 1 placebo capsule, BID − (500 mg/day dose of NEEM)
Group D: NEEM500: 2 capsules of neem 250 mg, BID −- (1000 mg/day dose of NEEM)
Subjects took the study products with 250 mL of water after food; they continued their concomitant medication.
Outcome Measures
The primary outcome measure was glycemic control, as assessed by reduction in post-prandial blood glucose (PPBS), fasting blood glucose (FBS), glycosylated hemoglobin (HbA1c) and homeostatic model assessment of insulin resistance (HOMA-IR) from baseline to the end of the study period, and compared to placebo.
Secondary outcome measures included change in endothelial function (Reflection Index, RI), oxidative stress biomarkers – nitric oxide (NO), glutathione (GSH), malondialdehyde (MDA), inflammatory biomarker – high sensitivity C-reactive protein (hsCRP), platelet aggregation, lipid profile, and pro-inflammatory cytokines (IL-6 and TNF-α) from baseline to the end of the study period.
Assessment of Endothelial Function
Endothelial function was assessed using the salbutamol challenge test employing digital volume plethysmography, following the methods of Chowienczyk et al24 and Naidu et al.25 The patients were inspected in the supine position after resting for 5 minutes. A digital volume pulse (DVP) was recorded using a photo-plethysmograph (Pulse Trace PCA2, PT200, Micro Medical, Kent, UK) transmitting infra-red light at 940 nm, placed on the index finger of the right hand. The signal from the plethysmograph was digitized using a 12-bit analog to a digital converter with a sampling frequency of 100 Hz. DVP waveforms were recorded over 20 second period, and the height of the late systolic/early diastolic portion of the DVP was expressed as a percentage of the amplitude of the DVP to yield the RI, following the procedure of Millasseau et al.26 After the DVP recording, three measurements of RI were calculated, and the mean value was determined. The patients were then administered with 400 µg of salbutamol by inhalation. After 15 minutes, three more measurements of RI were recorded, and the difference in mean RI before and after administration of salbutamol was used for assessing endothelial function. A change in ≤6% of RI postsalbutamol administration was considered as endothelial dysfunction.
Biomarker Evaluation
MDA,27 NO 28 and GSH29 levels were estimated spectrophotometrically, and hsCRP by ELISA method. After overnight fasting of 12hr, the samples were collected after the last dose of medication for determining HbA1c and lipid profile, including total cholesterol (TC), high-density lipoprotein-cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C), triglyceride (TG), and very low-density lipoprotein-cholesterol (VLDL-C) by appropriate standard techniques.
Platelet aggregation tests with ADP and collagen were performed using a platelet aggregometry test, ie, (Chronologlight transmittance aggregometry). TNF-α and IL-6 were estimated using commercially available ELISA kits. The HOMA-IR is an approximating equation for insulin resistance. It is estimated using the formula: fasting insulin (mIU/L) x fasting glucose (mg/dL)/405. HOMA-IR value less than 3 indicates normal insulin resistance; values between 3 and 5 indicate moderate insulin resistance, whereas values above 5 indicate severe insulin resistance.
Follow-Up Visits
The subjects were recalled for follow-up visits at 4 weeks, 8 and 12 weeks of therapy for evaluating the efficacy and safety of the interventions. FBS, PPBS, MDA, NO, GSH, hsCRP, and RI were estimated at baseline, 4 weeks, 8 and 12 weeks. HOMA-IR, IL-6, and TNF-α were evaluated at baseline, 4, and 12 weeks. HbA1c, lipid profiles, and platelet aggregation were estimated at baseline and 12 weeks of treatment (Figure 1).
 |
Figure 1 Treatment protocol. |
Safety Evaluation
The patients underwent a complete physical examination and laboratory investigations for safety parameters, including hematological, hepatic, and renal biochemical parameters at baseline and after 12 weeks by appropriate standard techniques. At each visit, the subjects were asked to report any adverse drug reactions for records in the case report form.
Compliance Verification
The compliance with study medications was verified by the pill-count method. Compliance was considered good, fair or poor, if a patient received >80%, between 60% and 80%, or <60% of the dispensed medication.
Sample Size Determination
To detect a reduction of 10mg/dL of PPBS with a 5% margin of alpha error, power of 80% and assuming a dropout rate of 10% and a screen failure of 5% a total of 94 patients were screened.
Statistical Analysis
Data are expressed as mean ± SD. The within-group statistical analysis was done using paired “t” test. The between-group analysis was performed using ANOVA. Post-hoc analysis between the groups was done with Tukey’s test. A p-value <0.05 was considered statistically significant. The statistical analysis was done using the software GraphPad Prism 8.
Results
A total of 94 subjects were screened, and 80 eligible subjects were enrolled in the study. A total of 78 subjects completed 12 weeks of treatment. Two subjects from the NEEM 250 group dropped out of the study before the first follow-up- one subject dropped out as he got transferred to another city and the other subject dropped out citing logistical reasons as he had relocated to a far-off location in the same city. Figure 2 shows the CONSORT diagram. Table 1 shows the demographic data of the subjects, who completed the study. No significant differences were observed between the treatment groups in baseline characteristics, including age, and body mass index (BMI).
 |
Table 1 Demographic Data of the Randomized Subjects |
 |
Figure 2 CONSORT diagram. |
The results are presented in Tables 2–12 and discussed below.
 |
Table 2 Effect on Post-Prandial Blood Sugar (PPBS in mg/dL) |
 |
Table 3 Effect on Fasting Blood Sugar (FBS, Mg/dL) |
 |
Table 4 Effect on HOMA-IR (Homeostatic Model Assessment for Insulin Resistance) |
 |
Table 5 Effect on HbA1c |
 |
Table 6 Effect on Reflection Index (RI%) |
 |
Table 7 Effect on NO (µM/L) |
 |
Table 8 Effect on MDA (µM/L) |
 |
Table 9 Effect on GSH (µmol/L) |
 |
Table 10 Effect on hsCRP (mg/L) |
 |
Table 11 Effect on IL-6 (pg/ml) |
 |
Table 12 Effect on TNF-α (pg/ml) |
Post-Prandial Blood Sugar Level
The within-group analysis shows that the PPBS level decreased significantly (p ≤ 0.0001) at all-time points of treatment, while the placebo has shown no improvement (Table 2). The between-group analysis shows that none of the groups is statistically better than the placebo at 4 weeks, while at 8 and 12 weeks, the neem extract is significantly (p ≤ 0.0001) better than the placebo. There is no significant difference between the doses at 4 and 8 weeks. However, at 12 weeks, there is a significant difference between 250 mg and 125 mg BID doses (p ≤ 0.05) and 500 mg and 125 mg BID doses (p ≤ 0.01), but not between 500 mg and 250 mg BID doses. A 22.6% decrease in PPBS at 12 weeks with the 500 mg BID dose is remarkable.
Fasting Blood Sugar Level
The within-group analysis shows that there is a significant improvement in FBS values at 4, 8, and 12 weeks of treatment with NEEM125, NEEM250 and NEEM500 (p ≤ 0.01 - p ≤ 0.0001), compared to baseline, while Placebo has not shown any improvement (Table 3). The response is dose dependent. The between-group analysis shows that NEEM125, NEEM250 and NEEM500 are significantly better than the placebo group at all the treatment time points (p ≤ 0.05 - p ≤ 0.0001), with the significance of improvement getting better with both the duration of treatment as well as the increasing dose. With 500 mg BID dose, a decrease of 19% in FBS in 12 weeks is again remarkable.
HOMA-IR
The within-group analysis shows that HOMA-IR values reduced significantly (p ≤ 0.0001) in all groups (including placebo) at 4 and 12 weeks compared to baseline, although the magnitude of change is much less with the placebo group, compared to the other groups (Table 4). The between-group analysis shows that NEEM250 (p ≤ 0.01) and NEEM500 (p ≤ 0.001) significantly improved HOMA-IR values than the placebo at 4 weeks, while at 12 weeks, all doses of neem extract are significantly (p ≤ 0.001-p ≤ 0.0001) better than the placebo. Also, at 12 weeks, significant differences exist between 250 mg and 125 mg BID doses (p ≤ 0.01) and 500 mg and 125 mg BID doses (p ≤ 0.0001), but not between 500 mg and 250 mg BID doses. HOMA-IR values show a 57.4% decrease at 12 weeks with the 500 mg BID dose.
HbA1c
Within the group analysis: HbA1c values reduced significantly for placebo (p ≤ 0.05) and all doses of neem extract (p ≤ 0.0001) at 12 weeks compared to baseline (Table 5). HbA1c values show a 19.6% decrease at 12 weeks with the 500 mg BID dose.
Between the group analysis: HbA1c values reduced significantly NEEM125 (p ≤ 0.0001), NEEM250 (p ≤ 0.0001) and NEEM500 (p ≤ 0.0001) groups, compared to placebo at 12 weeks. Also, significant differences exist between 250 mg and 500 mg BID doses (p ≤ 0.0001), and 500 mg and 125 mg BID doses (p ≤ 0.0001), but not between 125 mg and 250 mg BID doses.
Endothelial Function-Reflection Index
Within the group analysis: %RI values reduced significantly after 4, 8, and 12 weeks of treatment with NEEM125, NEEM250 and NEEM500 (p ≤ 0.01- p ≤ 0.0001) compared to baseline, while Placebo has not shown any improvement (Table 6).
Between the group analysis: %RI values reduced significantly with NEEM250 and NEEM500 groups, compared to placebo at 8 weeks (p ≤ 0.001; p ≤ 0.0001) and 12 weeks (p ≤ 0.0001; p ≤ 0.0001).
Nitric Oxide
Within the group analysis: NEEM125, NEEM250 and NEEM500 treatments significantly increased NO levels after 4, 8, and 12 weeks of treatment (p ≤ 0.0001) compared to baseline, while Placebo has not shown any improvement (Table 7).
Between the group analysis: all doses of NEEM failed to produce any significant effect on NO levels compared to placebo.
Malondialdehyde
Within the group analysis: all doses of NEEM significantly reduced MDA levels after 4, 8, and 12 weeks of treatment (p ≤ 0.0001) compared to baseline (Table 8). Placebo failed to show any changes.
Between the group analysis: the 12-week treatment with NEEM500 significantly reduced MDA levels compared to placebo (p ≤ 0.05). All other doses of NEEM failed to produce any significant effect on MDA levels compared to placebo.
Glutathione
Within the group analysis: all doses of NEEM significantly increased GSH levels after 4, 8, and 12 weeks of treatment (p ≤ 0.0001) compared to baseline (Table 9). Placebo failed to show any changes.
Between the group analysis: NEEM500 significantly increased GSH levels after 4 weeks (p ≤ 0.05), 8 weeks (p ≤ 0.0001) and 12 weeks (p ≤ 0.0001) compared to placebo. NEEM250 significantly increased GSH levels after 12 weeks (p ≤ 0.0001) compared to placebo. NEEM125 failed to produce any significant effect on GSH levels compared to placebo.
hsCRP
Within the group analysis: all doses of NEEM significantly reduced hsCRP levels after 4, 8, and 12 weeks of treatment (p ≤ 0.0001) compared to baseline (Table 10). Placebo failed to show any changes.
Between the group analysis: NEEM500 significantly reduced hsCRP levels after 4 weeks (p ≤ 0.05), 8 weeks (p ≤ 0.001) and 12 weeks (p ≤ 0.0001) compared to placebo. NEEM125 and NEEM250 significantly reduced hsCRP levels after 12 weeks (p ≤ 0.05; p ≤ 0.05) compared to placebo.
IL-6
Within the group analysis: all doses of NEEM significantly reduced IL-6 levels after 4 and 12 weeks of treatment (p ≤ 0.01 - p ≤ 0.0001) compared to baseline (Table 11). Placebo failed to show any changes.
Between the group analysis: all doses of NEEM significantly reduced IL-6 levels after 4 and 12 weeks of treatment (p ≤ 0.0001) compared to placebo.
TNF-α
Within the group analysis: all doses of NEEM significantly reduced TNF-α levels after 4 and 12 weeks of treatment (p ≤ 0.01 - p ≤ 0.0001) compared to baseline (Table 12). Placebo failed to show any changes.
Between the group analysis: all doses of NEEM failed to produce any significant effect on TNF-α levels compared to placebo.
Platelet Aggregation Using ADP and Collagen
NEEM did not have any significant effect on platelet aggregation induced by either ADP or collagen (Tables 13 and 14).
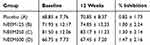 |
Table 13 Effect on Platelet Aggregation Using ADP |
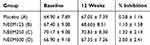 |
Table 14 Effect on Platelet Aggregation Using Collagen |
Lipid Profile (Tables 15–19)
NEEM did not have any significant effect on the lipid profile (TC, HDL-C, LDL-C, and TG) (Tables 15– 19).
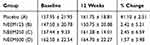 |
Table 15 Effect on TC (mg/dL) |
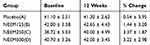 |
Table 16 Effect on HDL-C (mg/dL) |
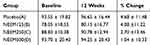 |
Table 17 Effect on LDL-C (mg/dL) |
 |
Table 18 Effect on VLDL-C (mg/dL) |
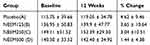 |
Table 19 Effect on TG (mg/dL) |
Safety Evaluation
No significant changes were observed in vital, hematological, renal, and hepatic functions in all groups (Tables S1–S3). All subjects tolerated the therapy well. One patient in NEEM125 and one in NEEM500 reported mild gastrointestinal disturbances, which subsided with symptomatic treatment. None of the subjects in either group discontinued the study due to adverse events. No incidence of hypoglycemia was reported by any of the subjects.
Discussion
Twelve-week treatment with NEEM, at all dosages studied, has significantly decreased the PPBS levels compared to placebo. Some pre-clinical studies support this finding. A combination of A. indica and G. procumbens ethanolic extracts has significantly reduced the postprandial blood glucose levels in alloxan-induced diabetic rats compared to the control group.30 Meliacinolin, isolated from A. indica leaves, significantly reduced the postprandial blood glucose levels in streptozotocin-induced diabetic rats.20 No RCTs have been found in the literature for evaluating the antidiabetic effects of neem leaf extract.
Similarly, NEEM treatment, at all the doses, significantly reduced the FBS levels compared to placebo and supported by in-vivo studies with experimentally diabetes-induced laboratory animals.17,31–33
NEEM significantly reduced insulin resistance, compared to the placebo group. This result is supported by a report that a polyherbal formulation containing neem leaves significantly reduced HOMA-IR values in the high fat diet-fed, low dose streptozocin-induced experimental type 2 diabetes in rats.34
NEEM significantly reduced the HbA1c levels, confirming an improved glycemic control compared to the placebo group. This finding is supported by Shailey et al and Gutierrez et al, who reported that A. indica leaf extract showed significantly lower HbA1c levels in experimentally induced diabetic rats compared to the control group.18,35
In addition to its anti-hyperglycemic effect, NEEM significantly improved endothelial function in T2DM subjects, compared to the placebo group. No such findings were available in the literature.
NEEM also significantly reduced the oxidative stress as evidenced by significant reduction in MDA levels and increase in GSH level, compared to baseline. These results are substantiated by several animal studies.35–38
NEEM also significantly reduced the systemic inflammatory markers in T2DM subjects, compared to baseline. Though no studies have investigated the effect of neem extract on systemic inflammatory markers in diabetic humans, several studies have reported that neem extract can reduce the levels of pro-inflammatory cytokines (IL-6 and TNF-α) in experimentally-inflammation-induced laboratory animals, which supports our findings.39–43
It is promising to note that most of the outcome measures in the present study are also significant at 8 weeks as well as 4 weeks of treatment with NEEM, compared to the placebo.
It is very interesting to note that the observed NEEM’s significant effects on glycemic control, endothelial function and systemic inflammation are in addition to the effects of metformin treatment the subjects have been receiving. It is also important to note that animal study results may not always hold true in controlled human clinical trials, as NEEM in this study showed no effect on lipid profile, while some animal studies have shown improvement.
Α-glucosidase and α-amylase inhibitory activities of meliacinolin, a bioactive in the leaves of neem, were suggested to be the mechanisms of action for antihyperglycemic effect.20 The blood sugar lowering activity of neem leaf extract may be due to its insulin release effect via preventing the glucose load induced inhibitory effect of serotonin on insulin release.44 Actual mechanism of action studies on NEEM are in progress.
The major limitations of the present study design are the relatively small sample size, relatively short duration of the study and lack of monitoring food intake and exercise, although the subjects were instructed to continue their routine food intake and exercise. Studies with a larger population and longer duration, involving a wider cross-section of the subjects with regard to age groups, occupation, and socioeconomic background, are planned.
Conclusion
The present study has established that a proprietary standardized aqueous extract of the leaves and twigs of Azadirachta indica has the potential to significantly help blood sugar management, improve vascular health and reduce systemic inflammation in subjects with type 2 diabetes mellitus. And, the beneficial effects observed with this extract were in addition to the benefits provided by the metformin treatment. Although, some neem extracts, especially of the seeds and possibly of the alcoholic extracts of the leaves, the aqueous extract used in this study seemed to have no safety concerns. However, additional large-scale studies are planned to confirm safety and efficacy of this product.
Data Sharing Statement
The data will be handled on a case-by-case basis as per institutional policy. The authors Usharani Pingali and Chandrasekhar Nutalapati can be contacted for the same.
Acknowledgments
The authors thank Natreon Inc., New Brunswick, NJ, USA for providing capsules of the test products and the placebo used in this study, kits for biomarker estimation and relevant literature.
We are grateful to Dr Y.S.N. Raju, Professor of General Medicine, NIMS, for his clinical support.
Disclosure
The authors declare no competing interests.
References
1. Cho NH, Shaw JE, Karuranga S, et al. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi:10.1016/j.diabres.2018.02.023
2. Kolb H, Martin S. Environmental/lifestyle factors in the pathogenesis and prevention of type 2 diabetes. BMC Med. 2017;15(1). doi:10.1186/s12916-017-0901-x
3. Aguiree F, Brown A, Cho NH, et al. IDF Diabetes Atlas. 2013.
4. Rivellese AA, Riccardi G, Vaccaro O. Cardiovascular risk in women with diabetes. Nutr Metab Cardiovasc Dis. 2010;20(6):474–480. doi:10.1016/j.numecd.2010.01.008
5. Tan KCB, Chow WS, Tam SCF, Ai VHG, Lam CHL, Lam KSL. Atorvastatin lowers C-reactive protein and improves endothelium-dependent vasodilation in type 2 diabetes mellitus. J Clin Endocrinol Metab. 2002;87(2):563–568. doi:10.1210/jcem.87.2.8249
6. Dhananjayan R, Koundinya KSS, Malati T, Kutala VK. Endothelial dysfunction in Type 2 diabetes mellitus. Indian J Clin Biochem. 2016;31(4):372–379. doi:10.1007/s12291-015-0516-y
7. Folli F, Corradi D, Fanti P, et al. The role of oxidative stress in the pathogenesis of Type 2 diabetes mellitus micro- and macrovascular complications: avenues for a mechanistic-based therapeutic approach. Curr Diabetes Rev. 2012. doi:10.2174/157339911797415585
8. De Vriese AS, Verbeuren TJ, Van De Voorde J, Lameire NH, Vanhoutte PM. Endothelial dysfunction in diabetes. Br J Pharmacol. 2000;130(5):963–974. doi:10.1038/sj.bjp.0703393
9. Guest CB, Park MJ, Johnson DR, Freund GG. The implication of proinflammatory cytokines in type 2 diabetes. Front Biosci. 2008;Volume(13):5187. doi:10.2741/3074
10. Uysal KT, Wiesbrock SM, Marino MW, Hotamisligil GS. Protection from obesity-induced insulin resistance in mice lacking TNF-α function. Nature. 1997;389(6651):610–614. doi:10.1038/39335
11. Cai D, Yuan M, Frantz DF, et al. Local and systemic insulin resistance resulting from hepatic activation of IKK-β and NF-κB. Nat Med. 2005;11(2):183–190. doi:10.1038/nm1166
12. Guest CB, Hartman ME, O’Connor JC, Chakour KS, Sovari AA, Freund GG. Phagocytosis of cholesteryl ester is amplified in diabetic mouse macrophages and is largely mediated by CD36 and SR-A. PLoS One. 2007. doi:10.1371/journal.pone.0000511
13. Paul R, Prasad M, Sah NK. Anticancer biology of Azadirachta indica L (neem): a mini review. Cancer Biol Ther. 2011;12(6):467–476. doi:10.4161/cbt.12.6.16850
14. Maithani A, Parcha V, Pant G, Dhulia I, Kumar D. Azadirachta indica (neem) leaf: a review. J Pharm Res. 2011;4(6):1824–1827.
15. Sanni O, Erukainure OL, Chukwuma CI, Koorbanally NA, Ibeji CU, Islam MS. Azadirachta indica inhibits key enzyme linked to type 2 diabetes in vitro, abates oxidative hepatic injury and enhances muscle glucose uptake ex vivo. Biomed Pharmacother. 2019;109:734–743. doi:10.1016/j.biopha.2018.10.171
16. Gautam MK, Gangwar M, Singh SK, Goel RK. Effects of Azadirachta indica on vascular endothelial growth factor and cytokines in diabetic deep wound. Planta Med. 2015. doi:10.1055/s-0035-1545917
17. Satyanarayana K, Sravanthi K, Shaker I, Ponnulakshmi R. Molecular approach to identify antidiabetic potential of Azadirachta indica. J Ayurveda Integr Med. 2015;6(3):165. doi:10.4103/0975-9476.157950
18. Perez Gutierrez RM, De Jesus Martinez Ortiz M. Beneficial effect of Azadirachta indica on advanced glycation end-product in streptozotocin-diabetic rat. Pharm Biol. 2014;52(11):1435–1444. doi:10.3109/13880209.2014.895389
19. Saidu Y, Muhammad SA, Abbas AY, Onu A, Tsado IM, Muhammad L. In vitro screening for protein tyrosine phosphatase 1B and dipeptidyl peptidase IV inhibitors from selected nigerian medicinal plants. J Intercult Ethnopharmacol. 2017. doi:10.5455/jice.20161219011346
20. Perez-Gutierrez RM, Damian-Guzman M. Meliacinolin: a potent α-glucosidase and α-amylase inhibitor isolated from Azadirachta indica Leaves and in vivo antidiabetic property in streptozotocin-nicotinamide-induced Type 2 diabetes in mice. Biol Pharm Bull. 2012;35(9):1516–1524. doi:10.1248/bpb.b12-00246
21. Dubey R, Patil K, Dantu SC, et al. Azadirachtin inhibits amyloid formation, disaggregates pre-formed fibrils and protects pancreatic β-cells from human islet amyloid polypeptide/amylin-induced cytotoxicity. Biochem J. 2019;476(5):889–907. doi:10.1042/BCJ20180820
22. Mukherjee A, Sengupta S. Characterization of nimbidiol as a potent intestinal disaccharidase and glucoamylase inhibitor present in Azadirachta indica (neem) useful for the treatment of diabetes. J Enzyme Inhib Med Chem. 2013. doi:10.3109/14756366.2012.694877
23. Ponnusamy S, Haldar S, Mulani F, Zinjarde S, Thulasiram H, RaviKumar A. Gedunin and azadiradione: human pancreatic alpha-amylase inhibiting limonoids from neem (Azadirachta indica) as anti-diabetic agents. PLoS One. 2015;10(10):e0140113. doi:10.1371/journal.pone.0140113
24. Chowienczyk PJ, Kelly RP, MacCallum H, et al. Photoplethysmographic assessment of pulse wave reflection: blunted response to endothelium-dependent beta2-adrenergic vasodilation in type II diabetes mellitus. J Am Coll Cardiol. 1999;34(7):2007–2014. doi:10.1016/S0735-1097(99)00441-6
25. Naidu MUR, Sridhar Y, Rani PU, Mateen AA. Comparison of two β2 adrenoceptor agonists by different routes of administration to assess human endothelial function [1]. Indian J Pharmacol. 2007. doi:10.4103/0253-7613.33439
26. Millasseau SC, Kelly RP, Ritter JM, Chowienczyk PJ. Determination of age-related increases in large artery stiffness by digital pulse contour analysis. Clin Sci. 2002;103(4):371–377. doi:10.1042/cs1030371
27. Vidyasagar J, Karunakar N, Reddy MS, Rajnaranyana K, Surender T, Krishna DR. Oxidative stress and antioxidant status in acute organophosphorous insecticide poisoning. Indian J Pharmacol. 2004.
28. Miranda KM, Espey MG, Wink DA. A rapid, simple spectrophotometric method for simultaneous detection of nitrate and nitrite. Nitric Oxide Biol Chem. 2001. doi:10.1006/niox.2000.0319
29. Ellman GL. Tissue sulfhydryl groups. Arch Biochem Biophys. 1959;82(1):70–77. doi:10.1016/0003-9861(59)90090-6
30. Sunarwidhi AL, Sudarsono S, Nugroho AE. Hypoglycemic effect of combination of Azadirachta indica A. Juss. and Gynura procumbens (Lour.) Merr. ethanolic extracts standardized by rutin and quercetin in alloxan-induced hyperglycemic rats. Adv Pharm Bull. 2014. doi:10.5681/apb.2014.090
31. Khosla P, Bhanwra S, Singh J, Seth S, Srivastava RK. A study of hypoglycamic effects of Azadirachta indica (Neem) in normal and alloxan diabetic rabbits. Indian J Physiol Pharmacol. 2000.
32. Bisht S, Sisodia SS. Anti-hyperglycemic and antidyslipidemic potential of azadirachta indica leaf extract in STZ- induced diabetes mellitus. J Pharm Sci Res. 2010.
33. Halim ME. Lowering of blood sugar by water extract of Azadirachta indica and Abroma augusta in diabetes rats. Indian J Exp Biol. 2003.
34. Sathyanarayan S, Pillai KS. Antidiabetic and antidyslipidemic properties of goa-111, a mixture of gymnemasylvestrae, ocimum sanctum and azadirachta indica extract in the ratio of 1:1:1 studied in high fat diet fed- low dose streptozotocin induced experimental type 2 diabetes in rat. J Drug DelivTher. 2019. doi:10.22270/jddt.v9i4-a.3394
35. Shailey S, Basir SF. Strengthening of antioxidant defense by Azadirachta indica in alloxan-diabetic rat tissues. J Ayurveda Integr Med. 2012. doi:10.4103/0975-9476.100174
36. Akinola OB, Omotoso GO, Akinola OS, Dosumu OO, Adewoye ET. Effects of combined leaf extract of vernoniaamygdalitis and azadirachta indica on hepatic morphology and hepatotoxicity markers in streptozotocin-induced diabetic rats. J Chinese Integr Med. 2011;9(12):1373–1379. doi:10.3736/jcim20111215
37. Gutierrez RMP, Gómez YGY, Guzman MD. Attenuation of nonenzymatic glycation, hyperglycemia, and hyperlipidemia in streptozotocin-induced diabetic rats by chloroform leaf extract of Azadirachta indica. Pharmacogn Mag. 2011;7(27):254. doi:10.4103/0973-1296.84243
38. Shrivastava A, Chaturvedi U, Sonkar R, Khanna AK, Saxena JK, Bhatia G. Antioxidant effect of Azadirachta indica on high fat diet induced diabetic charles foster rats. Appl Biochem Biotechnol. 2012. doi:10.1007/s12010-012-9681-0
39. Koul A, Bharrhan S, Singh B, Rishi P. Potential of Azadirachta indica against Salmonella typhimurium-induced inflammation in BALB/c mice. Inflammopharmacology. 2009;17(1):29–36. doi:10.1007/s10787-008-8032-9
40. Lee JW, Ryu HW, Park SY, et al. Protective effects of neem (Azadirachta indica A. Juss.) leaf extract against cigarette smoke- and lipopolysaccharide-induced pulmonary inflammation. Int J Mol Med. 2017. doi:10.3892/ijmm.2017.3178
41. Morris J, Gonzales CB, De La Chapa JJ, et al. The highly pure neem leaf extract, SCNE, inhibits tumorigenesis in oral squamous cell carcinoma via disruption of pro-tumor inflammatory cytokines and cell signaling. Front Oncol. 2019;9. doi:10.3389/fonc.2019.00890
42. Patel MJ, Tripathy S, Mukhopadhyay KD, et al. A supercritical CO2 extract of neem leaf (A. indica) and its bioactive liminoid, nimbolide, suppresses colon cancer in preclinical models by modulating pro-inflammatory pathways. Mol Carcinog. 2018;57(9):1156–1165. doi:10.1002/mc.22832
43. Bharitkar YP, Bathini S, Ojha D, et al. Antibacterial and antiviral evaluation of sulfonoquinovosyldiacylglyceride: a glycolipid isolated from Azadirachta indica leaves. Lett Appl Microbiol. 2014;58(2):184–189. doi:10.1111/lam.12174
44. Chattopadhyay RR. Possible mechanism of antihyperglycemic effect of Azadirachta indica leaf extract: part V. J Ethnopharmacol. 1999;67(3):373–376. doi:10.1016/S0378-8741(99)00094-X
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
