Back to Journals » Risk Management and Healthcare Policy » Volume 14
Evaluation of the 10 Years’ Association Between DXA Screening and Mortality in Patients Who Received Vertebroplasty in the Taiwan Population
Authors Wu YY, Lin IF , Chen PY, Lin CK, Wu CC , Liang CL, Lee YC, Lin CW, Chin WL, Wang HK
Received 25 January 2021
Accepted for publication 1 July 2021
Published 14 July 2021 Volume 2021:14 Pages 2995—3001
DOI https://doi.org/10.2147/RMHP.S303184
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Kent Rondeau
Yu-Ying Wu,1,2 I-Fan Lin,1,3 Po-Yuan Chen,1,2 Cheng-Kai Lin,1,2 Cheng-Chun Wu,1 Cheng-Loong Liang,1,2 Yi-Che Lee,1,4 Chi-Wei Lin,1,5 Wei-Leng Chin,1,5 Hao Kuang Wang1,2,6
1School of Medicine, College of Medicine, I-Shou University, Kaohsiung, Taiwan; 2Department of Neurosurgery, E-Da Hospital, Kaohsiung, Taiwan; 3Division of Infectious Diseases, Department of Internal Medicine, E-Da Hospital, Kaohsiung, Taiwan; 4Department of Nephrology, E-Da Hospital, Kaohsiung, Taiwan; 5Department of Family Medicine, E-Da Hospital, Kaohsiung, Taiwan; 6Department of Neurosurgery, E-Da Cancer Hospital, Kaohsiung, Taiwan
Correspondence: Hao Kuang Wang
Department of Neurosurgery, E-Da Hospital/ I-Shou University, No. 1, Yida Road, Jiaosu Village, Yanchao District, Kaohsiung City, 82445, Taiwan
Tel +866-975106080
Email [email protected]
Background: Osteoporotic fractures are a significant cause of morbidity and mortality affecting population worldwide. All guidelines recommended vertebral fracture assessment by dual-energy X-ray absorptiometry (DXA). This study aimed at evaluation of any associated benefits of screening with DXA in patients who had received vertebroplasty in Taiwan.
Methods: Data were obtained from the National Health Insurance Research Database (NHIRD) in Taiwan. We retrospectively compared the data of patients, who were admitted for vertebroplasty, whether they received DXA screening or not. The outcomes of interest were recurrence of spinal fracture and mortality during a follow-up period of 10 years.
Results: From this Taiwan national database, the screening rate of osteoporosis in patient who received vertebroplasty was 11.7%. The mean age in the non-DXA screened cohort (n=32,986) was 74.03± 12.21 years (71.98% female). In the DXA screened cohort (n=4361), the mean age was 76.43± 9.19 years (79.91% female). During the 10-year follow-up period, after matching, non-DXA patients had significantly higher mortality rates than their DXA counterparts, which were 42.37% and 37.73% (p-value < 0.0001), respectively. The re-fracture rates between non-DXA and DXA patients were not significantly different at 17.26% and 16.89% (p-value = 0.1766), respectively.
Conclusion: The rate of DXA screening before patients receiving vertebroplasty was extremely low, at 11.7%. Our results showed that DXA screening before vertebroplasty in spinal fractures patients had lower mortality. From this national retrospective cohort study, routine screening of osteoporosis in spinal fracture patients can lead to reduction in mortality.
Keywords: osteoporosis, vertebroplasty, DXA, mortality
Introduction
Osteoporotic fractures are a significant cause of morbidity and mortality affecting population worldwide, particularly in developed countries.1 Symptomatic osteoporotic vertebral compression fractures (VCFs) are very common, especially in the elderly.2 They lead to decreased mobility, morbidities, and age-adjusted mortality.3 In Taiwan, awareness of osteoporosis has significantly improved over the years.4 However, osteoporosis is generally regarded as a metabolic disease too often overlooked by caregivers, who tend to focus solely on pain relief.
When reviewing clinical guidelines for the management of VCFs, the diagnostic and therapeutic recommendations were generally inconsistent. However, all guidelines recommended vertebral fracture assessment by dual-energy X-ray absorptiometry (DXA).5,6
It is indisputable that screening for osteoporosis using DXA in VCF patients is an indispensable part of disease management. However, DXA is not performed routinely in VCF patients in Taiwan. Under Taiwan’s National Health Insurance (NHI), Taiwan Diagnosis Related Groups (Tw-DRGs) were implemented to provide standardized payment rates for each diagnosis. This served as a disincentive to perform additional tests, such as DXA. Physicians in Taiwan tend to perform vertebroplasty for pain relief solely based on image evidence such as serial X-rays and magnetic resonance imaging (MRI), omitting DXA scan to screen for osteoporosis in the high-risk population.
The primary aim of this study was to investigate the screening rates of DXA in patients who had received vertebroplasty in Taiwan. The secondary aim of this study was to point out any identifiable benefits of routine DXA screening.
Methods
Materials and Methods
This study was approved by the Ethical Medicine Committee of E-Da hospital (EMRP-108-061) and supported by the Clinical Monitoring Research Program of E-Da hospital (EDAD2005). The study protocol was also reviewed by the National Health Research Institute (NHRI), who consented to the planned analysis of the National Health Insurance Research Database (NHIRD) data.
Database
This population-based cohort study was performed using computerized records from the Taiwan NHIRD, a large encrypted secondary organized collection of data maintained by the Taiwan national healthcare system, covering more than 99% of the population in Taiwan. The NHIRD contains comprehensive medical records of the entire population of Taiwan since its implementation in 1995. Surgical case codes were used to identify and classify diseases. This study was performed in accordance with the Declaration of Helsinki guidelines.
Study Sample
The vertebroplasty cohort in this study included all patients with surgical codes 33126B (percutaneous vertebroplasty) and 64160B (open reduction for fracture of spine) in 1996–2013 and aged 20 years or older from the database. To maximize case ascertainment, the analysis was limited to patients receiving vertebroplasty exclusively. Thus, concomitant appearance of surgical codes 83044B (spinal fusion-anterior spinal fusion with spinal instrumentation≦4 motion segments) and 83046B (spinal fusion-posterior spinal fusion with spinal instrumentation≦6 motion segments) were excluded from this cohort study. Then, this vertebroplasty cohort was divided DXA group and non-DXA group, depending on whether the patients received DXA screening or not, respectively. Figure 1 shows a flow chart of the study procedure.
 |
Figure 1 Flow chart showing selection of the study subjects. Abbreviation: NHIRD, National Health Insurance Record Database. |
Using matched propensity scoring, the DXA to non-DXA ratio was set at 1:1 since enough vertebroplasty cases were available to enhance the power of statistical tests to be used in stratified analyses. Every single patient in the DXA group was matched by gender, age and comorbidities with one patient in the non-DXA group obtained in the same period to the maximal capacity.
Both the DXA and non-DXA groups were followed up until the end of 2018. Baseline comorbidities which were ascertained from ICD-9-CM codes in claims records included diabetes mellitus (ICD-9-CM code 250), hypertension and its complications (ICD-9-CM code 401–405), peripheral vascular disease (ICD-9-CM code 440–447) Cerebrovascular disease (ICD-9-CM code 430–437), respiratory disease (ICD-9-CM code 491–493), peptic ulcer disease (ICD-9-CM code 531–534), chronic liver disease (ICD-9-CM code 571–573), chronic kidney disease (ICD-9-CM code 580–588), rheumatologic disease (ICD-9-CM code 710, 714, 725), cardiac disease (ICD-9-CM code 410–414), pneumonia (ICD-9-CM code 480–486), urinary tract infection (ICD-9-CM code 599) and cancer (ICD-9-CM code 140–199, 200, 202–207).
The clinical characteristics and categorical demographics of the study cases were analyzed by Student’s t-test to compare between the non-DXA and DXA groups, for the unmatched and matched cohorts, in Tables 1 and 2, respectively. Patient survival was calculated until the study endpoint (31 December 2018). The main event of interest was patient death. All statistical tests were performed using Statistical Analysis Software V9.4 (SAS Institute), reported using 95% confidence intervals (CI) and adopted a two-tailed significance of 0.05.
 |
Table 1 Baseline Characteristics of the Study Population (UNMATCHED) |
 |
Table 2 Baseline Characteristics of the Study Population (MATCHED) |
Patient and Public Involvement
The patients and the public were not involved in the research.
Results
In Tables 1 and 3, the baseline demographics characteristics and comorbidities of the study cohorts are shown. We observed that 4361 patients who received DXA screening and 32,986 patients who did not receive DXA screening were eligible for analysis. From this Taiwan national database, the screening rate of osteoporosis in patient who received vertebroplasty for VCF was 11.7%.
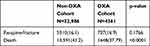 |
Table 3 Outcome of the Study Population (UNMATCHED) |
Table 1 showed the baseline characteristics of the study population. In the non-DXA cohort, the mean age was 74.03±12.21 years, which was significantly younger than the DXA cohort, with mean age at 76.43±9.19 years (p-value < 0.0001). The proportion of female patients were lower in the non-DXA cohort than the DXA cohort, at 71.68% and 79.91% (p-value < 0.0001), respectively. Table 3 showed the repeated spinal fracture rates in both cohorts and their mortality rates at 10 years follow-up. The spinal re-fracture rates were similar in both cohorts, 16.1% in non-DXA and 16.9% in DXA (p-value = 0.1766). The mortality rate was lower in DXA cohort, at 37.79%, when compared to non-DXA cohort, at 41.20% (p-value < 0.0001).
After propensity score matching, the present study consisted of 4333 screened with DXA and 4333 matched non-DXA patients, shown in Tables 2 and 4. All baseline characteristics were well balanced between the cohorts. No statistically significant inter-cohort differences were observed in age, genders, and baseline comorbidities. Non-DXA patients had higher mortality rates, which was 42.37%, than their DXA counterparts, which was 37.73% (p-value < 0.0001). Non-DXA patients had higher repeated spinal fracture rates, at 17.26%, than DXA patients, at 16.89%, even though it was not statistically significant (p = 0.679).
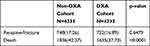 |
Table 4 Outcome of the Study Population (MATCHED) |
Discussions
Osteoporosis-related fractures are a major health concern, affecting a growing number of individuals worldwide.1 It is associated with age-related fractures, rheumatic diseases, and chronic pulmonary diseases.2 Epidemiological studies have consistently shown that osteoporosis is associated with high mortality and adverse outcomes in the elderly population.3 However, most studies focused on hip fractures,7,8 with fewer literature reporting on the outcomes of other fracture types, such as spinal fracture. In limited studies, hip fracture is associated with significantly increased mortality than VCF, reaching 32.1% compared to 10%, respectively; however, the latter is associated with more morbidity.9 It is proven in multiple studies that osteoporosis treatment in vertebral and nonvertebral fracture can reduce mortality in older, frailer individuals who are at high risk of fracture. In the meta-analysis, osteoporosis treatment was associated with an 11% reduction in mortality.10
Vertebroplasty is a time-proven management for VCF that can improve pain score, disability, and quality of life. It is considered as an effective procedure for the treatment of painful acute vertebral fracture in patients who have failed to respond to a 4- to 6-week course of appropriate medical therapy.11 In this observational cohort study, we evaluated the rates and potential benefits of DXA screening in patients treated for VCF with vertebroplasty using electronic record from Taiwan NHIRD.
This is the first nationwide study to evaluate the effect of DXA screening on mortality rate in patients who received vertebroplasty. There were two main findings in this study. Firstly, the rate of DXA screening before patients receiving vertebroplasty was extremely low, at 11.7%. Secondly, our results showed that compared to no DXA screening, DXA screening before vertebroplasty in spinal fractures patients had lower mortality, 37.73% compared to 42.37% (p-value < 0.0001).
In Taiwan, the DXA screening rate of less than 12% in vertebroplasty patients was strikingly low. This is understandable under Taiwan’s National Health Insurance payment system which implement the same Standardized Payment Rate of a particular Diagnosis Related Group. This served as a disincentive since it became unprofitable to perform DXA examination for patients admitted for spinal fractures. Caregivers tend to focus solely on pain relief provided by vertebroplasty, foregoing the importance to screen for osteoporosis using DXA, which was clearly stated in management guidelines.5,6 Caregivers were more likely to issue DXA screening in patients having comorbidities. In other words, osteoporosis awareness is higher in these patients. After matching in Table 2, patients not screened with DXA evaluation had significantly higher mortality.
These data reflected that DXA screening was too often overlooked in vertebroplasty patients, especially if they do not have chronic diseases. Furthermore, this neglect to screen for osteoporosis in patients receiving vertebroplasty is a missed opportunity to initiate osteoporosis treatments, which is proposed to be associated with decreased mortality.
As the great English social reformer William Wilberforce once famously declared, “You may choose to look the other way, but you can never say that you did not know.” The under-recognition and under-appreciation of osteoporosis in symptomatic VCF patients in Taiwan was alarming, although osteoporosis was already declared as a government mandated national health priority (NHP) in Taiwan in 2005.4 A similar trend was observed in the Perspective database, which analyzed 51,346 patients hospitalized for osteoporotic hip fracture and showed only 1023 patients (2%) were prescribed ideal therapy for osteoporosis, although bone mineral testing information was unavailable in that study.12 Based on our study, we suggest that DXA should be routinely screened for patients with any type of fracture. Ultimately, detection of osteoporosis in vertebroplasty patients was associated with decreased mortality.
The main strength of this study was the large number of patients who received vertebroplasty collected using procedure codes from NHIRD. Therefore, the problems of insufficient power and the potential for selection biases were minimized.
Our study had some limitations. First, the most glaring missing link in the data presented in this study was that diagnosing osteoporosis do not necessary signify initiation of osteoporosis treatment. However, refusal of treatment after an osteoporosis diagnosis is a rarity in Taiwan since osteoporotic drugs are reimbursed due to their roles as secondary prevention for osteoporotic fracture under Taiwan’s NHI system. Future studies on the osteoporosis treatment rate after a diagnosis made with DXA scan would shed more light on this matter. Second, the NHIRD did not include important parameters such as lifestyle variables, such as smoking and drinking. Lifestyle modifications were shown to impact osteoporosis outcome and mortality.13 Third, studies have shown that the cause, locations, and extent of vertebral fractures were reportedly associated with the risk of refracture and long-term functional outcome,14,15 but the imaging information was unavailable in the claims database. Four, no comparison of treatment options, such as alendronate and denosumab, that might have affected the patient outcomes were carried out.10,16 Last, no comparison between short-term and long-term survival was carried out. No evaluation of quality of life and disability levels was carried as well.
Despite these limitations, our study encompassed a large cohort of patients with VCFs treated with vertebroplasty in all demographic segments who were matched with corresponding controls. Although we have demonstrated the positive impact of DXA screening on survival, this does not imply a causal relationship. Future studies are needed to include a comparison of different treatment strategies and preventive regimens for osteoporosis in fracture patients. This study proved that recognition of osteoporosis using DXA screening is the first step in the right direction for caregivers to provide effective managements, ultimately decreasing the mortality rate of vertebral fracture patients.
Conclusions
In conclusion, we found in this national database of Taiwan that the rates of in-hospital screening for osteoporosis with dual energy x-ray absorptiometry (DXA) was very low. Our findings suggest that despite proven therapies and established guidelines for osteoporosis, DXA screening remained severely under-utilized in patients undergoing vertebroplasty, presenting as a massive missed opportunity to initiate osteoporosis treatment in this high-risk population. Evidence have shown that treating osteoporosis is associated with better outcome and lower mortality.
Data Sharing Statement
This retrospective, population-based cohorts were selected from among patients registered in the National Health Research Institute (NHRI) Database, which was released for research purposes in 2008. The details of database generation, monitoring, and maintenance are published online by the Taiwan NHRI (http://nhird.nhri.org.tw/).
Ethics Approval and Consent to Participate
We analyzed administrative claims data obtained from Taiwan’s National Health Insurance Research Database (NHIRD). The details of database generation, monitoring, and maintenance are published online by the Taiwan NHRI (http://nhird.nhri.org.tw/). Because the National Health Insurance (NHI) program is the sole payer in Taiwan, the data represents the original medical claims for all islanders covered by the NHI program, and are distributed by sex, age, or amount of average payroll-related insurance payments. The subjects of this study were recruited by reviewing monthly patient discharge data released by NHIRD, and data in the NHIRD that could be used to identify patients is scrambled before being sent to the NHRI for database construction. Because the analysis was limited to aggregate secondary data that could not be used to identify the patients, the study was approved by the NHRI Ethics Review Committee, Taiwan. However, the study protocol conformed to the ethical standards established by the Declaration of Helsinki (1964), which do not require written or verbal consent for data-linkage studies.
Acknowledgments
This study was supported by Center for Database Research, E-DA HEALTHCARE GROUP. We are also grateful to Health Data Science Center, National Cheng Kung University Hospital for providing administrative and technical support.
Funding
This study was supported in part by grants from the E-da hospital, Kaohsiung, Taiwan (EDAD2005).
Disclosure
The authors confirm that this article content has no conflicts of interest.
References
1. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12):1726–1733. doi:10.1007/s00198-006-0172-4
2. Melton LJ
3. Nazrun AS, Tzar MN, Mokhtar SA, Mohamed IN. A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Ther Clin Risk Manag. 2014;10:937–948. doi:10.2147/TCRM.S72456
4. Chen FP, Huang TS, Fu TS, Sun CC, Chao AS, Tsai TL. Secular trends in incidence of osteoporosis in Taiwan: a Nationwide Population-Based Study. Biomed J. 2018;41(5):314–320. doi:10.1016/j.bj.2018.08.001
5. Musculoskeletal I, Shah LM, Jennings JW, et al.; Expert Panels on Neurological Imaging IR. ACR appropriateness criteria((R)) management of vertebral compression fractures. J Am Coll Radiol. 2018;15(11S):S347–S364.
6. Lentle B, Cheung AM, Hanley DA, et al. Osteoporosis Canada 2010 guidelines for the assessment of fracture risk. Can Assoc Radiol J. 2011;62(4):243–250. doi:10.1016/j.carj.2011.05.001
7. Harvey NC, McCloskey EV, Mitchell PJ, et al. Mind the (treatment) gap: a global perspective on current and future strategies for prevention of fragility fractures. Osteoporos Int. 2017;28(5):1507–1529. doi:10.1007/s00198-016-3894-y
8. Ballane G, Cauley JA, Luckey MM, Fuleihan Gel H. Secular trends in hip fractures worldwide: opposing trends east versus west. J Bone Miner Res. 2014;29(8):1745–1755. doi:10.1002/jbmr.2218
9. Rizkallah M, Bachour F, Khoury ME, et al. Comparison of morbidity and mortality of hip and vertebral fragility fractures: which one has the highest burden? Osteoporos Sarcopenia. 2020;6(3):146–150. doi:10.1016/j.afos.2020.07.002
10. Bolland MJ, Grey AB, Gamble GD, Reid IR. Effect of osteoporosis treatment on mortality: a meta-analysis. J Clin Endocrinol Metab. 2010;95(3):1174–1181. doi:10.1210/jc.2009-0852
11. Jay B, Ahn SH. Vertebroplasty. Semin Intervent Radiol. 2013;30(3):297–306. doi:10.1055/s-0033-1353483
12. Jennings LA, Auerbach AD, Maselli J, Pekow PS, Lindenauer PK, Lee SJ. Missed opportunities for osteoporosis treatment in patients hospitalized for hip fracture. J Am Geriatr Soc. 2010;58(4):650–657. doi:10.1111/j.1532-5415.2010.02769.x
13. Pinheiro MM, Castro C, Frisoli Júnior A, Szejnfeld VL. Lifestyle changes after osteoporotic fractures in elderly women. Rev Bras Reumatol. 2003;43:279–286. doi:10.1590/S0482-50042003000500004
14. Ikeda Y, Sudo A, Yamada T, Uchida A. Mortality after vertebral fractures in a Japanese population. J Orthop Surg (Hong Kong). 2010;18(2):148–152. doi:10.1177/230949901001800204
15. Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR; Study of Osteoporotic Fractures Research Group. Vertebral fractures and mortality in older women: a prospective study. Arch Intern Med. 1999;159(11):1215–1220. doi:10.1001/archinte.159.11.1215
16. Winkler EA, Yue JK, Birk H, et al. Perioperative morbidity and mortality after lumbar trauma in the elderly. Neurosurg Focus. 2015;39(4):E2. doi:10.3171/2015.7.FOCUS15270
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
