Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Evaluation of Short-Term Side Effects Following the First Dose of COVID-19 Vaccines Among Physicians and Dentists: A Cross-Sectional Study from India
Authors Majumder MAA , Singh K, Johnson WMS, Rajasundaram A, Gupta S, Gaur U, Kumar S , Chatterjee M, Fazle Rabbi AM , Sangishetti VP, Rahman S , Campbell MH , Harewood H , Bharatha A , Krishnamurthy K , Kabir R, Parsa AD, Mohammmad S , Haque M , Razzaque MS
Received 19 September 2022
Accepted for publication 10 January 2023
Published 19 January 2023 Volume 2023:16 Pages 161—174
DOI https://doi.org/10.2147/JMDH.S390364
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Md Anwarul Azim Majumder,1,2 Keerti Singh,2 WMS Johnson,3 Archana Rajasundaram,3 Subir Gupta,2 Uma Gaur,2 Santosh Kumar,4 Madhuri Chatterjee,5 Ahbab Mohammad Fazle Rabbi,6 Vijay Prasad Sangishetti,7 Sayeeda Rahman,8 Michael H Campbell,2 Heather Harewood,2 Ambadasu Bharatha,2 Kandamaran Krishnamurthy,2 Russell Kabir,9 Ali Davod Parsa,9 Shegufta Mohammmad,10 Mainul Haque,11 Mohammed S Razzaque12
1Public Health Foundation of Bangladesh, Dhaka, Bangladesh; 2Faculty of Medical Sciences, The University of the West Indies, Bridgetown, Barbados; 3Department of Anatomy, Sree Balaji Medical College and Hospital, Chennai, Tamil Nadu, India; 4Karnavati School of Dentistry, Karnavati University, Ahmedabad, Gujarat, India; 5Department of Pharmacology, Shri Ramkrishna Institute of Medical Science, Durgapur, West Bengal, India; 6Department of Population Sciences, University of Dhaka, Dhaka, Bangladesh; 7Department of Pharmacology, Govt. Medical College, Shivpuri, Madhya Pradesh, India; 8School of Medicine, American University of Integrative Sciences (AUIS), Bridgetown, Barbados; 9Faculty of Health, Education, Medicine and Social Care, Anglia Ruskin University, Chelmsford, Essex, UK; 10BRAC Learning Division, BRAC University, Dhaka, Bangladesh; 11Faculty of Medicine and Defence Health, Universiti Pertahanan Nasional Malaysia (National Defence University of Malaysia), Kuala Lumpur, 57000, Malaysia; 12Lake Erie College of Osteopathic Medicine, Erie, PA, USA
Correspondence: WMS Johnson, Sree Balaji Medical College and Hospital, Chennai, Tamil Nadu, India, Email [email protected]; [email protected] Mainul Haque, Faculty of Medicine and Defence Health, National Defence University of Malaysia, Kuala Lumpur, Malaysia, Email [email protected]; [email protected]
Background: Efficacy and safety are fundamental for the development of successful COVID-19 vaccines. Vaccine-associated side effects influence vaccine hesitancy. This study investigated the prevalence, severity, and onset of side effects following the first dose of COVID-19 vaccines among physicians and dentists working in various healthcare settings across India.
Methods: A cross-sectional survey collected self-report data from April to June 2021 on side effects following the first dose of the vaccine. An online validated questionnaire using the Google Docs® platform was circulated via email and social media platforms.
Results: More than 40% of participants experienced at least one side effect after the first dose of vaccination; the most common were mild and resolved within three days after vaccination. More than 91% of respondents received the Covishield (AstraZeneca) vaccine; the most prevalent adverse effects were soreness of the injected arm (78.9%), tiredness (71.1%), and fever (54.9%). Logistic regression showed that women were almost 60% less likely to report side effects.
Conclusion: Findings supported the safety of the first dose of the COVID-19 vaccine based on relatively few self-limiting side effects, mainly soreness of the injected arm and tiredness. Further research is needed to determine the long-term safety of COVID-19 vaccines, especially after booster doses.
Keywords: prevalence, adverse effects, COVID-19 vaccine, physicians, dentists, India
Introduction
In late 2019, patients from Wuhan first experienced pneumonia due to a novel coronavirus subsequently identified as a human beta coronavirus (HβCoV) of zoonotic origin,1 which is predominantly spread directly or indirectly via respiratory droplets and aerosols released when infected persons cough, sneeze, talk, or sing.2–4 In early 2020, the World Health Organization (WHO) designated this fast-spreading virus, with an incubation period ranging from 1–14 days (average of five days), as the 2019 novel coronavirus (2019-nCoV).5 The Coronavirus Study Group of the International Committee on Taxonomy of Viruses designated this virus as the “severe acute respiratory syndrome coronavirus-2” (SARS-CoV-2),6 the seventh known coronavirus to infect humans.7 WHO declared the associated disease, coronavirus disease-2019 (COVID-19), a pandemic in March 2020.8 Until the advent of vaccines in 2021, COVID-19 prevention and control measures in the community relied on a complementary suite of non-pharmaceutical interventions, including hand hygiene, use of personal protective equipment, crowd avoidance, social distancing, community lockdowns, and travel restrictions.9
COVID-19 vaccines provided definitive therapy, reducing illness and hospitalizations from COVID-19 infection, thus potentially ameliorating the course and impact of the COVID-19 pandemic.10 Reports have identified common vaccine-related side effects such as pain at the injection site, fever, myalgia, fatigue, and headache. Less frequently, serious adverse events (SAE) were reported in four vaccine trials: COVID-19 Vaccine AstraZeneca (AZD1222)—168 SAEs with three events shown to be related to the vaccine; Ad26.COV2. S vaccine– four SAEs with none related to the vaccine; Comirnaty (BNT162b1) vaccine – five SAEs reported and; Covaxin (BBV152) vaccine – one SAE was identified.11 Arguably, the low attribution of SAEs speaks to the relative safety of the vaccines. Vaccine uptake depends on public acceptance. Given persistent challenges such as public mistrust and low acceptance even among healthcare workers,12 there remains a need to investigate and document safety data of COVID-19 vaccines in varied settings.
Global efforts to combat COVID-19 primarily depend on preventive measures adopted by individuals to reduce the likelihood of infection transmission.13 Many drugs and therapeutic compounds have been recommended in the fight against COVID-19, but these function only as supportive treatments.14 Vaccination is likely to remain the most effective prophylactic measure for effective public health response.15 Vaccines induce the body’s adaptive immune response via generating protective antibodies against possible future infections. Effective vaccines can reduce disease transmissibility, morbidity, and mortality and, eventually, confer herd immunity.2,4 Knowledge of potential side effects is important for vaccine recipients, clinicians, and caregivers.16
Efficacy and safety are fundamental for the development of a successful vaccine. COVID-19 vaccines have been developed and deployed at an unprecedented pace. These praiseworthy but compressed efforts raised questions about the quality of evidence supporting efficacy and safety.17 At present, eleven COVID-19 vaccines have received Emergency Use Listing (EUL) from the World Health Organization (WHO): Tozinameran (Pfizer/BioNTech), Moderna (Spikevax), Covishield (Oxford/AstraZeneca formulation), Novavax (Covovax), Ad5-nCoV (CanSino), BBV152 (Covaxin –Bharat Biotech), Janssen COVID-19 vaccine, BIBP CorV/BIBP COVID-19 vaccine (Sinopharm), and Sinovac (CoronaVac).18 The different types of COVID-19 vaccination platforms are: a) mRNA vaccines, b) viral vector (adenovirus) vaccines, c) inactivated virus vaccines, and d) protein subunit vaccines. The mechanism of action of these vaccines varies, although the common target is to trigger the immune response against SARS-CoV-2. Accordingly, it is expected that adverse effects associated with vaccines can vary widely.19 Covishield is an adenoviral vector vaccine that does not generate an immune response to the adenovirus but only triggers an immune response to the viral protein encoded in the host DNA.2
The SARS-CoV-2 virus, which is spread via infected respiratory droplets or aerosols, has infected and killed millions globally. As of December 21, 2022, approximately 659.2 million people have been infected, and 6.6 million have died.20 More than 13.7 billion vaccine doses have been administered worldwide, and 68.7% of the world population has received at least one dose of a COVID-19 vaccine.21 India is one of the worst-hit countries by the COVID-19 pandemic. COVID-19 was first reported in India on 30 January 2020 in Kerala state. The total number of COVID-19-infected patients in India is approximately 44.6 million, with at least 530,680 related deaths by December 2022.20 Drug regulators in India granted emergency approval for the first COVID-19 Vaccine, AstraZeneca, on January 1, 2021. As of 21 December 2022, 70% of the Indian population was fully vaccinated.22 Physicians, dentists, nurses, and other healthcare workers (HCWs) have more direct and frequent contact with vulnerable individuals who are at high risk of COVID-19 infection and other health problems.23,24 In India, more than 1700 physicians had died of COVID-19 by February 2022.25
Vaccine awareness programs for HCWs hope to influence behavior and attitudes towards preventive public health measures, thus reducing transmission of COVID-19.26 These attitudes and behaviors are especially important for developing long-term anti-COVID-19 strategies. Studies in India demonstrated that 40% to 90% of physicians, nurses, and dental practitioners were willing to receive a vaccine if available.23,27–29
Notably, most studies on the side effects of the COVID-19 vaccine have been funded by pharmaceutical manufacturers. These studies typically follow guidelines established by drug regulatory authorities and are monitored by third parties.30 However, the (perceived) need for more clearly independent studies on side effects may impact vaccine hesitancy and uptake. Professional and public perceptions of side effects play a primary role in public confidence in vaccine development and uptake.31 Further, unsubstantiated claims regarding side effects spread through mass and social media contribute to vaccine hesitancy among the public and HCWs.24
In an environment where mis- and disinformation threaten public health, accurate reporting of the prevalence and severity of side effects associated with COVID-19 vaccination is essential to inform policy and encourage vaccine uptake.24 Physicians and dentists are a key population in which the study of self-reported side effects following vaccination is necessary for several reasons: they are a priority population for vaccination; their clinical training facilitates greater accuracy in reporting symptoms, and their experiences may shape clinical practice and policy actions.16
This study aims to determine the prevalence, severity, and onset of adverse effects following the first dose of COVID-19 vaccines among physicians and dentists working in public and private healthcare settings across India. During the study, two non-replicating viral vector vaccines, Covishield (AstraZeneca) and Gam-COVID-Vac (Sputnik V), and one inactivated virus vaccine, BBV152/Covaxin (Bharat Biotech), were available in India.
Materials and Methods
Study Design and Participants
A cross-sectional survey was conducted among HCWs in 128 teaching, non-teaching, government, and private hospitals across 16 states of India (Andhra Pradesh, Bihar, Chhattisgarh, Gujarat, Haryana, Himachal Pradesh, Jharkhand, Karnataka, Kerala, Madhya Pradesh, Maharashtra, Pondicherry, Rajasthan, Tamil Nadu, Telangana, Uttar Pradesh, and West Bengal). The inclusion criteria were physicians or dentists who had received at least one dose of a COVID-19 vaccine.
We used the Raosoft software package (Raosoft, Inc., Seattle, WA 98115, USA. http://www.raosoft.com/samplesize.html) to calculate a required sample size of 377 physicians and dentists at a 95% confidence interval with a 5% margin of error. Participation in the survey was voluntary. Inclusion criteria were physicians and dentists working in India’s academic and healthcare institutes. All participants gave consent before participation. No identifiable personal information was collected.
Given the threat of COVID-19 infection, the study employed online convenience and snowball sampling to recruit participants. We distributed the survey link via email to medical and dental schools, professional associations, hospitals, and medical facilities with a request to share it with clinical personnel. We further shared the link using social media (eg, Facebook, Messenger, WhatsApp, and Viber). The survey included a request to share the link with colleagues. Non-respondents received two reminders to complete a questionnaire. Data collection continued from 4 April to 18 June 2021, with a pause for more than one month during the overwhelming second wave of COVID-19 in March 2021. Some members of the research team were infected, and many lost colleagues and family members during the study period.
Study Questionnaire and Data Collection Process
Participants completed a self-administered online questionnaire using the Google Docs® platform (Appendix 1). The questionnaire was validated and used in our previous study, and details are discussed elsewhere.16 The adapted questionnaire was reviewed by a multinational panel of public health specialists from India and other countries (Bangladesh, Barbados, UK, and USA) and amended according to their feedback. Then, a pilot study was conducted with 48 respondents, and the questionnaire was refined based on their inputs. The questionnaire included the following sections: demographic details; vaccination-related information; adverse effects after the 1st dose of vaccine, including onset, severity, and duration of symptoms; and treatment received to alleviate symptoms.
Adverse effects were recorded as follows:
- Time of symptom onset: same day, 1–3 days, and 4–7 days following vaccination.
- Severity: Mild: I was still able to do most daily activities; Moderate: I had to stop my daily activities; and Severe: I had to seek medical attention.
- Duration: 1 day, 2–3 days, 4–7 days, and still present.
Ethical Approval
This study was conducted in accordance with the Declaration of Helsinki, and the ethical approval for the study was granted by the Institutional Review Board (IRB) of Sree Balaji Medical College, Chennai, Tamil Nadu, India (REF:002/SBMCH/IHEC/2021/1178).
Statistical Analysis
After cleaning data and eliminating respondents who did not confirm that they were practicing physicians or dentists, we estimated the prevalence of side effects after vaccination. We conducted univariate and multivariate analyses to explore predictors of side effects following COVID-19 vaccination. Bivariate analyses were performed to examine the relationship between existing comorbidities and demographic characteristics with reported side effects. Multivariate logistic regression was performed to investigate the individual effects of predictor variables on side effects. All statistical analysis was performed using IBM SPSS 22.
Results
Respondents’ Characteristics
The demographic characteristics of participants are shown in Table 1. A total of 509 participants responded to the questionnaire. 64% were dentists, and 36% were physicians. Most were female (53.1%) and employed in the public healthcare sector (74.1%). More than 41% were between 31 and 40 years old, and 22.4% of the respondents had comorbidities. Approximately one-quarter of respondents (23.2%) had tested positive for COVID-19 by RT-PCR test, and more than three-quarters (78%) had received both the first and second doses of COVID-19 vaccination at the time of the survey. Among the COVID-19-positive cases, approximately half of respondents (47.4%) contracted the virus before the 1st dose of vaccination and 35.6% after the 2nd dose. The majority (91%) received Covishield (AstraZeneca) vaccine, followed by Covaxin (India) (8.4%), Moderna (0.4%), and Sputnik V (0.2%).
 |
Table 1 Demographic and Background Characteristics of Respondents |
Adverse Effects Following the 1st Dose of COVID-19 Vaccination
The prevalence of vaccine-related adverse effects among respondents is shown in Figure 1. More than 40% (n=204) of the respondents reported one or more side effects. The six most reported side effects were: soreness of the injected arm (78.9%), tiredness (71.1%), fever (54.9%), headache (49.8%), generalized soreness of muscles (46.6%), and longer-than-usual sleeping period (43.1%). Most respondents (55.5%) characterized the severity of symptoms as mild. However, some respondents (6.6%) did rate their experience of symptoms as severe. The two most common severe symptoms were tiredness (5.9%) and longer-than-usual sleep (4.9%). The actions taken to alleviate vaccine-related sickness included: paracetamol (86.7%), sleep (75.2%), and drinking copious amounts of water (67.5%). Only 10.8% of the respondents had suffered similar side effects from previous vaccinations for other diseases (eg, BCG, HPV). The respondents were aware of the risk of thromboembolic events (70.1%) and thrombocytopenia (47.5%), which may occur as rare but serious complications.
 |
Figure 1 Reported adverse effects of COVID-19 vaccination following the first dose of COVID-19 vaccines (n = 204). |
The details of the five most reported side effects, including onset and duration, are summarized in Table 2. For most respondents, these side effects appeared on the day of vaccination. Approximately half of the participants reported soreness in the arm (48.4%), and nearly one-third reported fever (31.9%) and headache (31.9%) on the day they were vaccinated. However, most respondents reported that these frequently observed side effects lasted 1 to 3 days. For 47.1% of participants, soreness in the arm lasted for 1 to 3 days, followed by fever (37.7%) and tiredness (31.4%). Soreness in the arm persisted for 7 days or more for 19.1% of participants, and tiredness persisted for more than 7 days for 4.4%. There was no significant association between vaccine type and observed side effects.
 |
Table 2 Summary of the Five Most Reported Side Effects Following the First Dose of COVID-19 Vaccines (n = 204) |
The prevalence of side effects among physicians stratified by gender, age, and occupation is shown in Table 3. Only soreness of muscles showed a significant relationship with the gender of participants. We examined differences in the level of reported events by two age groups (≤ 45 years and >45 years). Soreness of muscles, tiredness, and sleeping more than usual differed significantly by age group. No adverse effects were significantly associated with the participants’ occupation except for diarrhea, nausea, and vomiting.
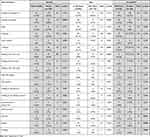 |
Table 3 Prevalence of Side Effects Among Physicians and Dentists Following First Dose of COVID-19 Vaccines Stratified by Gender and Age |
Determinants of Side Effects
Findings from the binary logistic regression model are summarized in Table 4. We considered six explanatory variables for the regression analysis. However, except for the gender of the physicians and dentists, no variables were associated with the presence of side effects. Female physicians and dentists were almost 60% less likely to report side effects than their male counterparts.
 |
Table 4 Logistic Regression Coefficients and Odds Ratios (95% CI) for Determinants of Side Effects Following the First Dose of COVID-19 Vaccines |
Discussion
The unprecedented and devastating challenges and consequences of the COVID-19 pandemic precipitated record-pace efforts to develop and deploy vaccines and global interest in the effective, rapid development of safe vaccines.24 Vaccines are designed to trigger the body’s immune response (reactogenicity). These processes typically are associated with transient post-vaccination effects such as pain at the injection site, fever, and malaise occurring within a few days after vaccination.32 However, occasional severe side effects may also occur.30 Several factors, including host and vaccine characteristics and a mode of vaccine administration, modulate the perception and extent of reactogenicity.33
Ensuring that all sections of society sufficiently accept COVID-19 vaccines is a major challenge for public health agencies. Negative perceptions of short- and long-term side effects and uncertainty regarding safety and efficacy are common barriers to the acceptance of vaccines.26,27 In the case of COVID-19, these barriers have been exacerbated by the unprecedented pace of development and deployment of novel vaccines under emergency authorization. Historically, vaccines have required 8 to 10 years of research and development before approval for use in humans. In contrast, the first COVID-19 vaccines were authorized within 8 to 10 months. Enormous investment of resources by pharmaceutical companies and governments drove this record-breaking effort.19 Availability of data on the structural and genomic characteristics of previously identified coronaviruses and global scientific collaborations with relevant safety, efficacy, and effectiveness trials were also important factors in the accelerated release of COVID-19 vaccines.34 However, these investments and scientific achievements have been frustrated by persistent barriers to vaccine acceptance. In addition to doubts raised by the rapid development of vaccines, misinformation, false beliefs, lack of confidence among stakeholders, and conspiracy theories have posed major obstacles to COVID-19 vaccination programs.26,27
In the global fight against the COVID-19 pandemic, vaccines seem to have played a critical role in reducing hospitalization, controlling disease spread, and preventing deaths.32 However, evidence related to the safety and efficacy of the COVID-19 vaccines in real-world settings is still emerging, especially as reformulated vaccines are deployed to combat newer viral strains.
We found that 40% of the participants experienced at least one side effect after the first dose of the COVID-19 vaccination. More than 91% of the respondents received the Covishield (AstraZeneca) vaccine, and the most common adverse effects reported were pain at the site of vaccination, followed by soreness of the injected arm (78.9%), tiredness (71.1%), fever (54.9%), and headache (49.8%). Symptoms were mainly mild and resolved within the first three days of immunization. The prevalence of side effects among HCWs reported in recent Indian studies ranged from 40% to 70%.35–39 Further studies in India37,40 and other Asian countries16,41,42 have demonstrated that common adverse effects of the COVID-19 vaccine are fever, fatigue, muscle pain, joint pain, and headache. A Phase 2/3 study of the Covishield vaccine reported local and systemic side effects as primarily mild to moderate in severity.43 Another Phase 1/2 study reported similar local and systemic reactions, which were reduced by the use of prophylactic paracetamol.44
A study conducted in India investigated side effects following the first immunization dose with Covishield and Covaxin among oral health care personnel. Consistent with the current findings, pain at the injection site was the most frequently reported adverse event. The majority reported that side effects were mild and self-limiting (ie, resolved within two days of vaccination).45 The available clinical trial data for various COVID-19 vaccines support our findings that reported side effects were mild/moderate, self-limiting, and did not require any further treatment.44,46–52 As in other studies of HCWs in India,37–40,53 Nepal,41,42 and Bangladesh,16 most of our respondents experienced mild to moderate symptoms (93.4%), which were self-limiting and resolved within a few days.
We found that females were more likely to report generalized soreness of muscles (p=0.003), and younger participants reported more intense symptoms related to the soreness of muscles (p=0.027), tiredness (p=0.001), and sleeping more than usual (p=0.027). These findings are consistent with other studies reporting a significantly higher prevalence of side effects among females16,54,55 and greater severity among younger people.16 However, our findings showed that female respondents were almost 60% less likely to develop side effects in aggregate compared to males, controlling for other variables in multivariate analysis.
Many unsubstantiated claims regarding purported side effects have circulated on social media.17 Public and social media have announced numerous cases of death after vaccination, even though evidence for a causal connection is lacking.56 Based on reports of rare but life-threatening side effects (eg, thromboembolic events), some vaccines were temporarily paused or withdrawn from the market.57 Evidence for currently available COVID-19 vaccines indicates no immediate serious side effect concerns, although some vaccines have been linked to deaths in rare cases. In our earlier study, we found a few serious (eg, acute myocardial infarction) and rare (eg, meningismus, severe eye pain, menstrual irregularities, excessive menstrual bleeding, hematuria) side effects among physicians in Bangladesh who received the 1st dose of Covishield (AstraZeneca) vaccine.16 Clinical trials of Covishield vaccines conducted in Brazil, South Africa, and the UK reported serious adverse events (SAEs) among 168 participants (n = 11,636). Only 3 of 172 events were shown to be related to vaccination.48 Similarly, a UK-based phase 2/3 trial identified 13 SEAs, none related to vaccination.43 These and similar claims should be carefully reported and documented, requiring further longitudinal studies.
Limitations of This Study
Convenience sampling and associated response biases do not permit the generalizability of findings. For example, lack of internet access or fluency in English is potential source of under-coverage bias. Further, the presence of side effects may have influenced potential participants’ motivation or ability to respond to the survey. Future studies using probability sampling would be useful. Finally, we caution that the absence of major side effects immediately post-vaccination does not imply long-term vaccine safety. A strength of this study is the accuracy and reliability of trained medical professionals to self-reported side effects.16
Conclusion
Our study elucidates the clinical presentation of short-term side effects associated with the Covishield vaccine among clinicians in India. First-dose administration was mainly associated with mild and self-resolving side effects. The most common side effects following the first dose were soreness of muscles and tiredness, and 40% of the respondents experienced at least one side effect. No life-threatening vaccine-related events were reported in this survey. More robust studies are needed to determine the true prevalence of side effects and examine the potential long-term side effects of COVID-19 vaccines, especially after booster doses.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
The authors thank the physicians who consented to participate in this study and completed the questionnaire. MAA Majumder, AMF Rabbi, A Rajasundaram, and WMS Johnson have full access to all the data and take responsibility for the integrity of the data.
Funding
This research received no external funding.
Disclosure
Dr. Md Anwarul Azim Majumder is the Editor-in-Chief of Advances in Medical Education and Practice (Dove Press). The other authors report no conflicts of interest in this work.
References
1. Chan JF, Kok KH, Zhu Z, et al. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg Microbes Infect. 2020;9(1):221–236. doi:10.1080/22221751.2020.1719902
2. Rahman S, Montero MTV, Rowe K, Kirton R, Kunik F. Epidemiology, pathogenesis, clinical presentations, diagnosis and treatment of COVID-19: a review of current evidence. Expert Rev Clin Pharmacol. 2021;14(5):601–621. doi:10.1080/17512433.2021.1902303
3. Priyanka COP, Singh I, Patra G, Patra G. Aerosol transmission of SARS-CoV-2: the unresolved paradox. Travel Med Infect Dis. 2020;37:101869. doi:10.1016/j.tmaid.2020.101869
4. Habas K, Nganwuchu C, Shahzad F, et al. Resolution of coronavirus disease 2019 (COVID-19). Expert Rev Anti Infect Ther. 2020;18(12):1201–1211. doi:10.1080/14787210.2020.1797487
5. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi:10.1038/s41586-020-2012-7
6. Gorbalenya AE, Baker SC, Baric RS; Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5(4):536–544. doi:10.1038/s41564-020-0695-z
7. Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF. The proximal origin of SARS-CoV-2. Nat Med. 2020;26(4):450–452. doi:10.1038/s41591-020-0820-9
8. World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19-11 March 2020. World Health Organization. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-The-media-briefing-on-covid-19---11-march-2020.
9. Güner R, Hasanoğlu I, Aktaş F. COVID-19: prevention and control measures in community. Turk J Med Sci. 2020;50(Si–1):571–577. doi:10.3906/sag-2004-146
10. Stokel-Walker C. What do we know about covid vaccines and preventing transmission? BMJ. 2022;376:o298. doi:10.1136/bmj.o298
11. Kaur RJ, Dutta S, Bhardwaj P, et al. Adverse events reported from COVID-19 vaccine trials: a systematic review. Indian J Clin Biochem. 2021;36(4):427–439. doi:10.1007/s12291-021-00968-z
12. Krishnamurthy K, Sobers N, Kumar A, et al. COVID-19 vaccine intent among health care professionals of Queen Elizabeth Hospital, Barbados. J Multidiscip Healthc. 2021;14:3309–3319. doi:10.2147/jmdh.s336952
13. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973–1987. doi:10.1016/s0140-6736(20)31142-9
14. Al-Hatamleh MAI, Hatmal MM, Alshaer W, et al. COVID-19 infection and nanomedicine applications for development of vaccines and therapeutics: an overview and future perspectives based on polymersomes. Eur J Pharmacol. 2021;896:173930. doi:10.1016/j.ejphar.2021.173930
15. Azim Majumder MA, Razzaque MS. Repeated vaccination and ‘vaccine exhaustion’: relevance to the COVID-19 crisis. Expert Rev Vaccines. 2022;1–4. doi:10.1080/14760584.2022.2071705
16. Majumder MAA, Lutfor AB, Rabbi AMF, et al. Prevalence of COVID-19 vaccine reactogenicity among Bangladeshi physicians. FASEB Bioadv. 2022;4(6):379–390. doi:10.1096/fba.2021-00158
17. Hatmal MM, Al-Hatamleh MAI, Olaimat AN, et al. Side effects and perceptions following COVID-19 vaccination in Jordan: a randomized, cross-sectional study implementing machine learning for predicting severity of side effects. Vaccines. 2021;9(6). doi:10.3390/vaccines9060556
18. COVID19 Vaccine Tracker. World Health Organization. 11 vaccines granted Emergency Use Listing (EUL) by WHO. VIPER Group COVID19 Vaccine Tracker Team. Available from: https://covid19.trackvaccines.org/agency/who/.
19. Mascellino MT, Di Timoteo F, De Angelis M, Oliva A. Overview of the main anti-SARS-CoV-2 vaccines: mechanism of action, efficacy and safety. Infect Drug Resist. 2021;14:3459–3476. doi:10.2147/idr.s315727
20. Worldometer. COVID-19 Coronavirus Pandemic. Worldometer. Available from: https://www.worldometers.info/coronavirus/.
21. Our World in Data. Coronavirus (COVID-19) vaccinations. our world in data. Available from: https://ourworldindata.org/covid-vaccinations.
22. Holder J. Tracking coronavirus vaccinations around the world. The New York Times. Available from: https://www.nytimes.com/interactive/2021/world/covid-vaccinations-tracker.html.
23. Gopakumar R, Mahesh J, Alexander B, Arya KS, John S, Kumbla S. Acceptance of COVID-19 vaccine among dental professionals: a cross-sectional study among practitioners, residents, and students. J Pharm Bioallied Sci. 2021;13(Suppl2):S985–s988. doi:10.4103/jpbs.jpbs_342_21
24. World Health Organization. Statement for healthcare professionals: how COVID-19 vaccines are regulated for safety and effectiveness (Revised March 2022). Joint statement from the International Coalition of Medicines Regulatory Authorities and World Health Organization. World Health Organization. Available from: https://www.who.int/news/item/17-05-2022-statement-for-healthcare-professionals-how-covid-19-vaccines-are-regulated-for-safety-and-effectiveness.
25. Varsha Torgalkar PD. COVID killed droves of Indian health workers. Their families must fight for recompense. Los Angeles Times. Available from: https://www.latimes.com/world-nation/story/2022-01-18/india-covid-health-workers-compensation.
26. Alam A, Majumder MAA, Haque M, et al. Disproportionate COVID-19 vaccine acceptance rate among healthcare professionals on the eve of nationwide vaccine distribution in Bangladesh. Expert Rev Vaccines. 2021;20:1167–1175. doi:10.1080/14760584.2021.1951248
27. Ashok N, Krishnamurthy K, Singh K, Rahman S, Majumder MAA. High COVID-19 vaccine hesitancy among healthcare workers: should such a trend require closer attention by policymakers? Cureus. 2021;13(9):e17990. doi:10.7759/cureus.17990
28. Kumar R, Beniwal K, Bahurupi Y, Kant R, Bairwa M. Determinants of COVID-19 vaccination willingness among health care workers: a quick online survey in India. Korean J Fam Med. 2021;42(6):445–452. doi:10.4082/kjfm.21.0071
29. Dara S, Sharma SK, Kumar A, et al. Awareness, attitude, and acceptability of healthcare workers about COVID-19 vaccination in Western India. Cureus. 2021;13(9):e18400. doi:10.7759/cureus.18400
30. Centres for Diseases Control and Prevention (CDC). Understanding adverse events and side effects. Centres for Diseases Control and Prevention (CDC). Available from: https://www.cdc.gov/vaccinesafety/ensuringsafety/sideeffects/index.html.
31. Riad A, Pokorná A, Attia S, Klugarová J, Koščík M, Klugar M. Prevalence of COVID-19 vaccine side effects among healthcare workers in the Czech Republic. J Clin Med. 2021;10(7):1428. doi:10.3390/jcm10071428
32. World Health Organization. Side Effects of COVID-19 Vaccines. World Health Organization. Available from: https://www.who.int/news-room/feature-stories/detail/side-effects-of-covid-19-vaccines.
33. Hervé C, Laupèze B, Del Giudice G, Didierlaurent AM, Tavares Da Silva F. The how’s and what’s of vaccine reactogenicity. NPJ Vaccines. 2019;4:39. doi:10.1038/s41541-019-0132-6
34. Centres for Diseases Control and Prevention (CDC). Understanding how COVID-19 vaccines work. Centres for Diseases Control and Prevention (CDC). Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/how-they-work.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fvaccines%2Fdistributing%2Fsteps-ensure-safety.html.
35. Kamal D, Thakur V, Nath N, Malhotra T, Gupta A, Batlish R. Adverse events following ChAdOx1 nCoV-19 vaccine (COVISHIELD) amongst health care workers: a prospective observational study. Med J Armed Forces India. 2021;77(Suppl2):S283–s288. doi:10.1016/j.mjafi.2021.06.014
36. Kaur U, Ojha B, Pathak BK, et al. A prospective observational safety study on ChAdOx1 nCoV-19 Corona virus vaccine (recombinant) use in healthcare workers- first results from India. EClinicalMedicine. 2021;38:101038. doi:10.1016/j.eclinm.2021.101038
37. Jayadevan R, Shenoy R, Ts A. Survey of symptoms following COVID-19 vaccination in India. medRxiv. 2021. doi:10.1101/2021.02.08.21251366
38. Inbaraj LR, George CE, Franklyn NN. How safe is Covishield (ChAdOx1nCoV-19) vaccine? Experience from a tertiary care hospital in South India. medRxiv. 2021. doi:10.1101/2021.03.16.21253744
39. Kaur S, Singh A, Saini S, et al. Reporting adverse events of ChAdOx1 nCoV-19 coronavirus vaccine (Recombinant) among the vaccinated healthcare professionals: a cross-sectional survey. Indian J Med Res. 2022. doi:10.4103/ijmr.ijmr_1221_21
40. Mahapatra S, Nagpal R, Marya CM, Taneja P, Kataria S. Adverse events occurring post-covid-19 vaccination among healthcare professionals - A mixed method study. Int Immunopharmacol. 2021;100:108136. doi:10.1016/j.intimp.2021.108136
41. Shrestha S, Devbhandari RP, Shrestha A, et al. Adverse events following the first dose of ChAdOx1 nCoV-19 (COVISHIELD) vaccine in the first phase of vaccine roll out in Nepal. J Patan Acad Health Sci. 2021;8(1):9–17. doi:10.3126/jpahs.v8i1.36242
42. Gautam A, Dangol N, Bhattarai U, et al. ChAdOx1 nCoV-19 vaccine and its self-reported adverse events: a cross-sectional study from Western Nepal. J Glob Health Rep. 2021;5:e2021069. doi:10.29392/001c.25471
43. Ramasamy MN, Minassian AM, Ewer KJ, et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet. 2021;396(10267):1979–1993. doi:10.1016/s0140-6736(20)32466-1
44. Folegatti PM, Ewer KJ, Aley PK, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet. 2020;396(10249):467–478. doi:10.1016/s0140-6736(20)31604-4
45. Sachdev SS, Chettiankandy TJ, Adhane YB, Sardar MA, Yaduwanshi K. Survey on individual experiences after first dose of COVID-19 vaccination amongst Indian oral health care personnel. J Commun Health Manag. 2021;8(3):119–123. doi:10.18231/j.jchm.2021.027
46. Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA covid-19 vaccine. N Engl J Med. 2020;383(27):2603–2615. doi:10.1056/NEJMoa2034577
47. Baden LR, El Sahly HM, Essink B, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403–416. doi:10.1056/NEJMoa2035389
48. Voysey M, Clemens SAC, Madhi SA, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397(10269):99–111. doi:10.1016/s0140-6736(20)32661-1
49. Sadoff J, Gray G, Vandebosch A, et al. Safety and efficacy of single-dose Ad26.COV2.s vaccine against covid-19. N Engl J Med. 2021;384(23):2187–2201. doi:10.1056/NEJMoa2101544
50. Xia S, Duan K, Zhang Y, et al. Effect of an inactivated vaccine against SARS-CoV-2 on safety and immunogenicity outcomes: interim analysis of 2 randomized clinical trials. JAMA. 2020;324(10):951–960. doi:10.1001/jama.2020.15543
51. Mulligan MJ, Lyke KE, Kitchin N, et al. Phase I/II study of COVID-19 RNA vaccine BNT162b1 in adults. Nature. 2020;586(7830):589–593. doi:10.1038/s41586-020-2639-4
52. Logunov DY, Dolzhikova IV, Zubkova OV, et al. Safety and immunogenicity of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine in two formulations: two open, non-randomised phase 1/2 studies from Russia. Lancet. 2020;396(10255):887–897. doi:10.1016/s0140-6736(20)31866-3
53. Kamble B, Bashar MA, Mishra CP. Incidence, pattern and severity of adverse events following immunization (AEFIs) associated with Chadox1 nCOV-19 corona virus vaccine (recombinant) among the healthcare workers of a tertiary care institute of Eastern Uttar Pradesh, India. Cureus. 2022;14(2):e21848. doi:10.7759/cureus.21848
54. Menni C, Klaser K, May A, et al. Vaccine side-effects and SARS-CoV-2 infection after vaccination in users of the COVID Symptom Study app in the UK: a prospective observational study. Lancet Infect Dis. 2021;21(7):939–949. doi:10.1016/s1473-3099(21)00224-3
55. Omeish H, Najadat A, Al-Azzam S, et al. Reported COVID-19 vaccines side effects among Jordanian population: a cross sectional study. Hum Vaccin Immunother. 2022;18(1):1981086. doi:10.1080/21645515.2021.1981086
56. Kounis NG, Koniari I, de Gregorio C, et al. Allergic reactions to current available COVID-19 vaccinations: pathophysiology, causality, and therapeutic considerations. Vaccines. 2021;9(3):221. doi:10.3390/vaccines9030221
57. European Medicines Agency. Signal Assessment Report on Embolic and Thrombotic Events (SMQ) with COVID-19 Vaccine (ChAdOx1-S [Recombinant])—Vaxzevria (Previously COVID-19 Vaccine AstraZeneca) (Other Viral Vaccines). European Medicines Agency; 2021.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
