Back to Journals » Journal of Pain Research » Volume 15
Evaluation of Sensory Loss Obtained by Circum-Psoas Blocks in Patients Undergoing Total Hip Replacement: A Descriptive Pilot Study
Authors Li H , Shi R, Shao P, Wang Y
Received 31 December 2021
Accepted for publication 22 March 2022
Published 29 March 2022 Volume 2022:15 Pages 827—835
DOI https://doi.org/10.2147/JPR.S354829
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jinlei Li
Supplementary video of "Sensory loss obtained by circum-psoas blocks" [ID 354829].
Views: 211
Huili Li, Rong Shi, Peiqi Shao, Yun Wang
Department of Anesthesiology, Beijing Chaoyang Hospital, Capital Medical University, Beijing, 100020, People’s Republic of China
Correspondence: Yun Wang, Department of Anesthesiology, Beijing Chaoyang Hospital, Capital Medical University, Beijing, 100020, People’s Republic of China, Tel +86-10-85231330, Email [email protected]
Purpose: The transversalis fascia (TF) encases the quadratus lumborum and psoas major (PM) muscles, respectively, after they split caudalward approximately at the level of the iliac crest. The branches of the lumbar plexus variably exit medially and laterally from the TF-encased PM muscle. We hypothesized that the local anesthetic (LA) injections around the anterolateral edge of PM at the supra-iliac level and into the retro-psoas compartment at the L5/S1 level, which termed as the circum-psoas blocks, could block the lumbar plexus branches. Therefore, here we evaluated the sensory loss caused by the circum-psoas blocks.
Methods: A total of 26 patients scheduled for total hip replacement were recruited for the study. After anesthesia induction, the ultrasound-guided circum-psoas blocks were performed in the lateral position with the affected side upward, in which the 0.3% ropivacaine was injected posterior to the TF and around the anterolateral edge of PM muscle at the supra-iliac level (25 mL), and into the retro-psoas compartment at the L5/S1 level (20 mL). The sensory block dermatomes and the muscle strength of quadriceps femoris were evaluated at 2 h or 6 h after surgery, respectively. The postoperative pain scores and opioid consumption were recorded.
Results: The median (interquartile range) highest and lowest dermatomes of sensory block were T10 (T9–T10) and S2 (S2–S2), respectively. The muscle strength of the quadriceps femoris evaluated at 6 h post-surgery was 4 (4– 5) points. Total postoperative equivalent milligrams of oral morphine consumption in the first 24 h were 11.3 ± 3.6 mg.
Conclusion: The circum-psoas blocks may be a promising approach for postoperative analgesia of hip surgery, since they provide a dermatomal coverage of sensory block from T8– 11 to S1– 3.
Clinical Trial Registration: Chinese Clinical Trial Registry, clinical trial number ChiCTR2100051247.
Keywords: hip surgery, nerve block, lumbar plexus, sacral plexus
Introduction
To provide the complete sensory loss for total hip replacement surgery, the blockade of the branches of both lumbar and sacral plexuses is required, although there remains no single technique that reliably acquires this.1 The transversalis fascia (TF) encases the quadratus lumborum and psoas major (PM) muscles, respectively, after they split caudalward approximately at the level of the iliac crest.2 The main nerve branches of the lumbar plexus, including the femoral nerve, lateral femoral cutaneous nerve (LFCN), and obturator nerve, are located within the PM compartment.3–5 These nerve branches of the lumbar plexus variably exit medially and laterally from the TF-encased PM muscle to the retro-psoas compartment (obturator nerve) and the iliopsoas compartment (femoral nerve and LFCN), respectively.6–9 The sacral plexus originates from the lumbosacral trunk (L4–L5) and the anterior rami of the S1–S3 nerve roots. The obturator nerve arises from the anterior rami of the second, third, and fourth lumbar nerves and descends through the PM muscle. It emerges from the medial border of PM muscle and then runs along the lateral wall of the lesser pelvis. In the retro-psoas compartment, the lumbosacral trunk is found located medially to the obturator nerve.6,9 More caudally, the retro-psoas compartment is anatomically continuous with the compartment between the piriformis and pelvic presacral fascia.
Based on the anatomical analysis, we speculated that if the local anesthetic (LA) was injected posterior to the psoas fascia (TF) and around the anterolateral edge of PM muscle just cranial to the iliac crest under ultrasound guidance, the two main branches of lumbar plexus (femoral nerve and LFCN) would be blocked. Additionally, the cranial spread of LA injected along the TF may lead to the lower thoracic paravertebral block via the medial arcuate ligament.10–12 On the other hand, another branch of lumbar plexus, the obturator nerve, and lumbosacral trunk could be blocked if the LA is injected into the retro-psoas compartment and around the posterior edge of PM muscle at the L5/S1 level.6,9 We termed the simple procedures as the circum-psoas blocks, since the LA was placed around the anterolateral and posterior edges of PM muscle at the supra-iliac and L5/S1 levels, respectively.13 In the current study, we aimed to evaluate the sensory loss obtained by the circum-psoas blocks in patients undergoing total hip replacement.
Methods
Ethical approval for this study (2021-ke-504) was provided by the Ethical Committee of Beijing Chaoyang Hospital, Capital Medical University, China. This clinical trial was registered with the Chinese Clinical Trial Registry, clinical trial number ChiCTR2100051247, date of registration September 16, 2021. Patients scheduled for total hip replacement under general anesthesia at our hospital were enrolled between September 22, 2021, and November 28, 2021. The written informed consents were obtained from all patients. Overall, our study complies with the Declaration of Helsinki.
A total of 26 participants between 50 and 80 years of age with a body mass index (BMI) of 20–30 kg m−2 and an American Society of Anesthesiologists (ASA) physical status of I–III were eligible for inclusion (Figure 1). Patients with a reported history of the use of any analgesic drugs for >3 months, allergy to medications used in our protocol, local or systemic infections, inability to accurately comprehend or take part in pain assessments due to psychiatric disorders, and the narrow distance between L5 transverse process and sacral ala (less than 1 cm in the anteroposterior X-ray film) were excluded. Patient demographic details, including age, sex, height, and weight, were recorded.
 |
Figure 1 A flow chart showing patient progress through the study phases. |
A standardized anesthetic regimen was performed in patients. Briefly, after the patient entered the operating room, the noninvasive blood pressure, electrocardiography, pulse oxygen saturation, and end-tidal carbon dioxide were monitored. Peripheral venous access was established. Next, an invasive radial arterial line was placed. General anesthesia was then induced by administering intravenous propofol 1.5–2 mg kg−1 (Fresenius Kabi AB, Uppsala, Sweden), sufentanil 0.2 μg kg-1 (Yichang Renfu Pharma, Yichang, China), and rocuronium 0.8 mg kg-1 (Xianju Pharma, Xianju, China). Then, the laryngeal mask was inserted, and the mechanical ventilation was initiated. General anesthesia was maintained through a steady infusion of propofol (0.08–0.1 mg kg−1 min−1) and remifentanil (0.1–0.2 μg kg−1 min−1, Yichang Renfu Pharma, Yichang, China).
The patients were placed in the lateral decubitus position with the affected upward after the laryngeal mask insertion. Then, after necessary skin sterilization, we performed the circum-psoas injections just cranial to the iliac crest level, in which the LA was injected posterior to the TF and around the anterolateral edge of PM muscle under ultrasound guidance. In detail, a curved array transducer (KONICA Minolta, Tokyo, Japan) was placed in the transverse position immediately cranial to the iliac crest at the posterior axillary line level. The quadratus lumborum muscle is identified with its attachment to the lateral edge of the transverse process of the lumbar vertebrae and a shamrock sign can be clearly seen in the sonogram.14 Then, a 10 cm puncture needle was then inserted from the lateral transducer edge in the plane of the ultrasound beam in a posterolateral to medial direction until the tip of the needle penetrated the TF of the anterolateral edge of the PM muscle (Figure 2). Proper needle positioning was confirmed by observing the fluid distribution around the PM muscle beneath the TF after injecting a small volume of 0.9% saline (5 mL). Then, 0.3% of ropivacaine (25 mL) was gradually injected into the fascial compartment to form a nearly 1/3 ring around the anterolateral edge of PM muscle after repeated negative aspiration (Supplementary Video).
Then, we performed the retro-psoas compartment block at the L5/S1 intervertebral level, in which the LA is placed around the posterior edge of the PM muscle.6,9 The transducer was first placed in the lumbosacral region to perform the paramedian sagittal scan on the affected side. After the sacrum and the L5 transverse process were identified, the transducer was rotated to the paramedian transverse plane until the spinal process and laminae of L5 and the iliac bone became visible in the sonogram. The lumbosacral ligament and the intertransverse ligament between the laminae of L5 and iliac bone were seen in the sonogram (Figure 3). The block needle was inserted with a steep out-of-plane approach penetrating the erector spinae muscle, the intertransverse ligament, the osteofibrotic tunnel and the lumbosacral ligament. Proper needle positioning was confirmed by injecting small (2–5 mL) aliquots of 0.9% saline. Ropivacaine (20 mL; 0.3%) was then gradually injected after repeated negative aspiration. A distinct loss-of-resistance during injection and view of the tip when the needle tip penetrated the lumbosacral ligament were considered as the primary endpoint.
All patients received surgery for total hip replacement in the lateral position. Additional intraoperative rocuronium boluses were administered as appropriate. When the surgery was finished, intravenous neostigmine (40 μg kg-1; Shanghai Xinyijinzhu Pharma, Shanghai, China) was administered to reverse the neuromuscular blockade. The total duration of anesthesia from intubation to extubation was recorded. After surgery, patients were transferred to the postanesthesia care room, where they achieved complete anesthetic recovery. A numerical rating scale (NRS) was used to gauge pain severity while at rest and during movement (0 = “no pain,” 10 = “worst pain imaginable”). The patients received the standard postoperative analgesia regimen. Celecoxib 200 mg was given orally every 12 hours. In addition, oral oxycodone 5–10 mg was given every 4 hours to patients with NRS score ≥4.15 The cumulative opioid consumption at 24 h was expressed as equivalent milligrams of oral morphine using a conversion factor of 1.5 for oxycodone. Postoperative pain was evaluated at 2 h, 6 h, 12 h, and 24 h. Possible adverse effects, including nausea and vomiting, dizziness, and pruritus, were recorded.
An investigator assessed sensory block levels using a cool roller at 2 h postoperatively. Normal sensation on the shoulder was used for comparison. The sensory block was identified when the sensation of cold was lost or markedly reduced. Dermatomes of thoracic spinal nerves were tested at the anterior axillary line. Dermatome L1 was tested 2 cm below the midpoint of the inguinal ligament, L2 at the midpoint of the anterior side of the thigh, L3 at the midpoint of the patella, L4 at the midpoint of the medial leg, L5 at the midpoint of the dorsum of the foot, S1 at the lateral side of the fifth toe, S2 at the midpoint of the popliteal crease and S3 at the ischial tuberosity.16
The muscle strength of the quadriceps femoris was assessed at 6 h after surgery. Patients were asked to flex their hips and knees, and their muscle strength was scored as follows: no muscle contraction, 0 points; muscle contraction but no joint movement, 1 point; joint movement but no gravity resistance, 2 points; gravity resistance, 3 points; gravity and partial counterforce resistance, 4 points; and normal joint function, 5 points.17 These scores were independently given by another anesthetist.
Statistical Analysis
The sample size was empirically identified, since this was a pilot study. The previous literature indicated that a sample size of 10–40 is appropriate.18 In the current study, an initial goal of 22 patients was set. After considering a drop-out rate of 20%, the goal sample size was revised to 26 patients. Categorical variables are presented as number and frequency. Continuous variables showing normality are expressed as mean ± standard deviation, whereas those not showing normality are expressed as median values [25th–75th interquartile range (IQR)]. SPSS software (version 22.0, IBM Corporation, Armonk, NY, USA) was used for statistical analysis.
Results
In total, 26 patients were recruited for this study. After excluding one patient who declined to participate, we enrolled 25 (13 men and 12 women) patients who received the circum-psoas blocks. One patient was excluded because he developed the delirium after surgery. The study flow chart is shown in Figure 1.
The patients’ demographics and operation details are presented in Table 1. The patients had a mean age of 70.5 (6.5) yr, weight 59.2 (5.7) kg, height 162.1 (6.7) cm, and BMI 26.4 (3.1). The average anesthesia and operation duration were 123 ±19 min, and 94 ± 11 min, respectively.
 |
Table 1 Demographics and Operation Details |
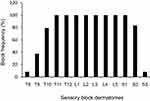
The dermatomal coverage of the sensory block was tested at 2 h after surgery. The median (IQR) highest and lowest sensory levels were T10 (T9–T10) and S2 (S2–S2), respectively. The mean number of blocked dermatomes was 10.2 ± 0.8. The sensory blockade range from T11 – S1 was obtained in every patient (Figure 4). Two patients achieved coverage as cephalad as T8 and 2 patients achieved coverage as caudal as S3.
The muscle strength of the quadriceps femoris evaluated at 6 h post-surgery was 4 (4–5) [median (IQR)]. 41.7% patients acquired the 5 points in muscle strength scoring. The 3 points was given in 12.7% patients. No patients had the points less than 3 (Table 2).
 |
Table 2 The Postoperative Data |
The postoperative pain scores were shown in (Table 2). Total postoperative equivalent milligrams of oral morphine consumption in the first 24 h were 11.3 ± 3.6 mg (Table 2). No patients required additional rescue analgesics in the first 24 h after surgery.
Two patients suffered from the nausea, 1 patient had vomiting and 1 patient developed pruritus during the first 24 h after surgery.
Discussion
In this prospective observational study, the circum-psoas injections at the two different levels could acquire the dermatomal coverage of sensory block from T8–11 to S1–3, which was detected at 2 h after surgery. Moreover, the NRS pain scores at rest and on movement, and postoperative opioid consumption were kept at the relatively lower levels during the first 24 postoperative hours, while the muscle strength of quadriceps femoris was little affected by the blocks.
Three mechanisms may be involved in the blocking actions of the circum-psoas blocks. First, the sub-endothoracic compartment (thoracic paravertebral space) communicates with the compartment between the TF and PM muscles.10–12 It indicates that the LA injected into the compartment around the PM muscle at the supra-iliac level may spread cranially into the lower thoracic paravertebral space. Second, the main branches of lumbar plexus, such as LFCN, femoral and obturator nerves, anatomically emerge lateral and medial to PM muscle encased by the TF at variable levels.4,13,19 Therefore, the LA injected into the compartment around the anterolateral border of PM muscle at the supra-iliac level may spread caudally and laterally to block the LFCN and the femoral nerves. Finally, the LA injected into the compartment around and posterior to the PM muscle at the L5/S1 level can block the lumbosacral trunk and obturator nerve, since these nerves are located in the same compartment.6,7,9 Additionally, the LA may also spread caudally to block the more sacral nerves, if the volume given is high enough.
Postoperative analgesia of total hip replacement surgery involves a wide range of nerves, including the obturator nerve and the femoral nerve in front of the hip joint, the superior gluteal nerve and the sciatic nerve behind the hip joint, the iliohypogastric nerve, the subcostal nerve, and the LFCN around the incision as well as the dorsal branch of L1/2/3 and S1/2/3 spinal nerves. In this observational study, we found that the LA injected around the PM muscle at two different levels could acquire the dermatomal coverage of sensory block from T8–11 to S1–3, which was detected at 2 h after surgery. The wider dermatomal coverage of circum-psoas block can almost provide the complete analgesia for hip surgery. The average anesthesia and operation duration were 123 ±19 min, and 94 ± 11 min, respectively. In order to ensure the complete recovery of cognitive function from the general anesthesia in patients, we chose to evaluate the sensory loss coverage at 2 h after blocks. As a result, the reported sensory block in patients was reliable.
Previous study has shown that the patients undergoing total hip replacement had moderate pain on movement (NRS > 4) at 6 h after surgery, even if receiving local infiltration analgesia, which may delay the hip exercise and enhanced recovery.15,17 Our data demonstrated that the circum-psoas blocks can provide better postoperative pain relief at rest or during movement and are associated with the lower demand for postoperative opioid in the first 24 h after surgery.
The muscle strength was measured during the first active motion at 6 h after surgery. In the current study, the circum-psoas blocks did not cause serious quadriceps femoris muscle weakness. 87.5% of patients had more than 3 points, and only 12.5% of patients acquired the 3 points. Ropivacaine at the low concentration could present the sensory block, but has no or a limited effect on motor nerves, thus preserving the ability to muscle strength. The lower concentration of ropivacaine (0.3%) we used for the circum-psoas blocks may explain why a sensory, but not motor block occurred.
The posterior approach for psoas compartment block has been used to provide pain management for the hip surgery. However, the risk of inadvertent neuraxial block or injury to vital vascular structures and organs, and the need for neurostimulation and ultrasound guidance have decreased popularity.3,8,15,19 The circum-psoas block has some advantages over the other blocks used for the hip surgery. First, it belongs to the interfascial plane block and can be performed under ultrasound guidance alone and without using neurostimulation. Second, the blocks have wider dermatomal coverage of sensory block and provide almost complete analgesia for hip surgery. Third, unlike the psoas compartment block, the circum-psoas blocks have reliable efficacy for obturator nerve blockade.4,6,7 On the other hand, the sacral plexus block is often used for the hip surgery together with the lumbar plexus block. Variations in the relationship between the sciatic nerve and piriformis muscle can influence the efficacy of sacral plexus block.20–22 Additionally, the LA deposit compartment for sacral plexus block is adjacent to the surgical area. A part of LA is possibly drained away during the surgical dissection, thus affecting the acting duration of the block. In contrast, the injection target with the circum-psoas block (retro-psoas compartment) is far away from the surgical area. Moreover, in the current study, the circum-psoas blocks present the 100% of block probability for the L4, L5, and S1 spinal nerves and 83.3% of block probability for the S2 spinal nerve. It provides most of the dermatomal coverage of sacral plexus block.
This study has several limitations. Sensory areas were assessed postoperatively, and a previous study demonstrated sensory ranges regressing over time.23 Hence, our results may be less than the maximum height and range. Due to incisions and dressings, we could not evaluate the blocked area as a plane, but only on the representative longitudinal lines. We only included the patients with BMI < 30 kg/m2. Future studies should evaluate the utility of the technique we described above in the obese patients. Additionally, this study is descriptive but not a randomized trial. The comparisons between this technique and the other blocks should be implemented in the future.
Conclusion
In summary, we have demonstrated the successful use of the circum-psoas blocks at the supra-iliac and the L5/S1 intervertebral levels. The circum-psoas blocks are characterized by wider dermatomal coverage of sensory blockade, ease of performance and little-affected muscle strength of quadriceps femoris. Further, randomized trials are needed to compare the circum-psoas blocks with other blocks to improve the surgical outcomes.
Data Sharing Statement
We all agree to share all the data for this article. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Bugada D, Bellini V, Lorini LF, Mariano ER. Update on selective regional analgesia for hip surgery patients. Anesthesiol Clin. 2018;36:403–415. doi:10.1016/j.anclin.2018.04.001
2. Li H, Shi R, Wang Y. A dynamic test to identify the potential recess between the psoas major and quadratus lumborum muscles at the supra-iliac level. J Pain Res. 2021;14:3235–3238. doi:10.2147/JPR.S329736
3. Capdevila X, Macaire P, Dadure C, et al. Continuous psoas compartment block for postoperative analgesia after total hip arthroplasty: new landmarks, technical guidelines, and clinical evaluation. Anesth Analg. 2002;94:1606–13, table of contents. doi:10.1097/00000539-200206000-00045
4. Farny J, Drolet P, Girard M. Anatomy of the posterior approach to the lumbar plexus block. Can J Anaesth. 1994;41:480–485. doi:10.1007/BF03011541
5. Mannion S, Barrett J, Kelly D, Murphy DB, Shorten GD. A description of the spread of injectate after psoas compartment block using magnetic resonance imaging. Reg Anesth Pain Med. 2005;30:567–571. doi:10.1016/j.rapm.2005.08.004
6. Bendtsen TF, Pedersen EM, Haroutounian S, et al. The suprasacral parallel shift vs lumbar plexus blockade with ultrasound guidance in healthy volunteers–a randomised controlled trial. Anaesthesia. 2014;69:1227–1240. doi:10.1111/anae.12753
7. Bendtsen TF, Pedersen EM, Moriggl B, et al. Anatomical considerations for obturator nerve block with fascia iliaca compartment block. Reg Anesth Pain Med. 2021;46:806–812. doi:10.1136/rapm-2021-102553
8. Dong J, Zhang Y, Chen X, et al. Ultrasound-guided anterior iliopsoas muscle space block versus posterior lumbar plexus block in hip surgery in the elderly: a randomised controlled trial. Eur J Anaesthesiol. 2021;38:366–373. doi:10.1097/EJA.0000000000001452
9. Strid JM, Pedersen EM, Al-Karradi SN, et al. Real-time ultrasound/MRI fusion for suprasacral parallel shift approach to lumbosacral plexus blockade and analysis of injectate spread: an exploratory randomized controlled trial. Biomed Res Int. 2017;2017:1873209. doi:10.1155/2017/1873209
10. Li H, Shi R, Shi D, Wang R, Liu Y, Wang Y. Anterior quadratus lumborum block at the lateral supra-arcuate ligament versus transmuscular quadratus lumborum block for postoperative analgesia in patients undergoing laparoscopic nephrectomy: a randomized controlled trial. J Clin Anesth. 2021;75:110561. doi:10.1016/j.jclinane.2021.110561
11. Li H, Shi R, Wang Y. A modified approach below the lateral arcuate ligament to facilitate the subcostal anterior quadratus lumborum block. J Pain Res. 2021;14:961–967. doi:10.2147/JPR.S306696
12. Shi R, Li H, Wang Y. Dermatomal coverage of single-injection ultrasound-guided parasagittal approach to anterior quadratus lumborum block at the lateral supra-arcuate ligament. J Anesth. 2021;35:307–310. doi:10.1007/s00540-021-02903-1
13. Diwan S, Nair A, Gawai N, Shah D, Sancheti P. Circumpsoas block - an anterior myofascial plane block for lumbar plexus elements: case report. Braz J Anesthesiol. 2021. doi:10.1016/j.bjane.2021.04.015
14. Sauter AR, Ullensvang K, Niemi G, et al. The Shamrock lumbar plexus block: a dose-finding study. Eur J Anaesthesiol. 2015;32:764–770. doi:10.1097/EJA.0000000000000265
15. Polania Gutierrez JJ, Ben-David B, Rest C, Grajales MT, Khetarpal SK. Quadratus lumborum block type 3 versus lumbar plexus block in hip replacement surgery: a randomized, prospective, non-inferiority study. Reg Anesth Pain Med. 2021;46:111–117. doi:10.1136/rapm-2020-101915
16. Aikawa K, Yokota I, Maeda Y, Morimoto Y. Evaluation of sensory loss obtained by modified-thoracoabdominal nerves block through perichondrial approach in patients undergoing gynecological laparoscopic surgery: a prospective observational study. Reg Anesth Pain Med. 2021;47:134–135. doi:10.1136/rapm-2021-102870
17. Hu J, Wang Q, Zeng Y, Xu M, Gong J, Yang J. The impact of ultrasound-guided transmuscular quadratus lumborum block combined with local infiltration analgesia for arthroplasty on postoperative pain relief. J Clin Anesth. 2021;73:110372. doi:10.1016/j.jclinane.2021.110372
18. Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health. 2008;31:180–191. doi:10.1002/nur.20247
19. Cappelleri G, Aldegheri G, Ruggieri F, Carnelli F, Fanelli A, Casati A. Effects of using the posterior or anterior approaches to the lumbar plexus on the minimum effective anesthetic concentration (MEAC) of mepivacaine required to block the femoral nerve: a prospective, randomized, up-and-down study. Reg Anesth Pain Med. 2008;33:10–16. doi:10.1016/j.rapm.2007.07.008
20. Babinski MA, Machado FA, Costa WS. A rare variation in the high division of the sciatic nerve surrounding the superior gemellus muscle. Eur J Morphol. 2003;41:41–42. doi:10.1076/ejom.41.1.41.28099
21. Butz JJ, Raman DV, Viswanath S. A unique case of bilateral sciatic nerve variation within the gluteal compartment and associated clinical ramifications. Australas Med J. 2015;8:24–27. doi:10.21767/AMJ.2015.2266
22. Carare RO, Goodwin M. A unique variation of the sciatic nerve. Clin Anat. 2008;21:800–801. doi:10.1002/ca.20696
23. Lee TH, Barrington MJ, Tran TM, Wong D, Hebbard PD. Comparison of extent of sensory block following posterior and subcostal approaches to ultrasound-guided transversus abdominis plane block. Anaesth Intensive Care. 2010;38:452–460. doi:10.1177/0310057X1003800307
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.