Back to Journals » International Journal of General Medicine » Volume 14
Evaluation of Prognosis and Risk of Death by Neutrophil/Lymphocyte Ratio, C-Reactive Protein/Albumin Ratio and Plasma D-Dimer in Patients with Pulmonary Thromboembolism
Authors Shan T, Li X, Yan M , Pan X
Received 6 October 2021
Accepted for publication 16 November 2021
Published 1 December 2021 Volume 2021:14 Pages 9219—9225
DOI https://doi.org/10.2147/IJGM.S343039
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Tiantian Shan,* Xinran Li,* Min Yan, Xiangtao Pan
Department of Hematology, Taicang Hospital Affiliated to Soochow University, Taicang City, Jiangsu Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiangtao Pan Tel +86 18915768003
Email [email protected]
Objective: To investigate the relationship between neutrophil/lymphocyte ratio, C-reactive protein/albumin ratio, plasma D-dimer and prognosis in patients with pulmonary thromboembolism, and to evaluate the risk of death.
Methods: We retrospectively analyzed peripheral hematology and coagulation-related indicators of 362 pulmonary thromboembolism patients and 32 normal people, and the differences between the patients and control group and between good and poor prognosis groups were compared. And we analyzed and compared separate detection and combined detection of neutrophil/lymphocyte ratio, C-reactive protein/albumin ratio and D-dimer on the efficiency of risk of death in patients.
Results: ① Neutrophil/lymphocyte ratio of pulmonary thromboembolism patients was 8.96± 1.94, significantly higher than that of control group 1.76± 0.53 (t=2.4281, P< 0.05). C-reactive protein/albumin ratio was 2.13± 2.08, significantly higher than 0.03± 0.01 in control group (t=20.7736, P< 0.01). D-dimer was 9.69± 8.61mg/L, significantly higher than 0.20± 0.11mg/L in control group (t=3.0066, P< 0.01). ② Hemoglobin, lymphocyte, albumin and lymphocyte/monocyte ratio in patients with good prognosis were significantly lower than those in poor prognosis group, while white blood cell, C-creative protein, neutrophil, C-reactive protein/albumin ratio, neutrophil/lymphocyte ratio and D-dimer were significantly lower than those in poor prognosis group (P all < 0.05). ③ Regression analysis showed that neutrophil/lymphocyte ratio (P=0.007), C-reactive protein/albumin ratio (P=0.010) and D-dimer (P=0.003) were independent prognostic factors for pulmonary thromboembolism. ④ In assessing the risk of death of patients, D-dimer alone had the highest sensitivity (93.1%), and C-reactive protein/albumin ratio alone had the highest specificity (68.8%). The combined detection of these three indicators had higher sensitivity (86.2%) and higher specificity (67.6%) at the same time. ⑤ The area under receiver operating characteristic curve for combined detection of neutrophil/lymphocyte ratio, C-reactive protein/albumin ratio and D-dimer was the largest (up to 0.821).
Conclusion: Patients with pulmonary thromboembolism highly expressed in neutrophil/lymphocyte ratio, C-reactive protein/albumin ratio and D-dimer. The combined detection of these three indicators can improve the assessment efficacy of the risk of death in patients with pulmonary thromboembolism.
Keywords: pulmonary thromboembolism, neutrophil to lymphocyte ratio, C-reactive protein/albumin ratio, plasma D-dimer, risk assessment of death, prognosis
Introduction
Pulmonary thromboembolism (PTE) is a deep venous thrombotic disease that seriously affects the lives of patients. CT pulmonary angiography (CTPA) examination, V/Q scintigraphy and magnetic resonance pulmonary angiography (MRPA) are important clinical diagnostic tools. In addition, PTE may indicate a high level of plasma D-dimer (D-D), but contrarily, a high level of D-D does not equal PTE. In other words, the low level of D-D, to some extent, means that PTE can be excluded.1 Neutrophil/lymphocyte ratio (NLR) is one of the important indicators reflecting the state of inflammation and immune function of the body,2–4 which is manifested in the increase in neutrophil (NE) and/or decrease in lymphocyte (LY) in inflammatory response. Recent studies have confirmed that NLR is closely related to the occurrence and development of thrombotic diseases.5–7 C-reactive protein (CRP) is also an important indicator of inflammatory response. Recently, it has been found that CRP to albumin (ALB) ratio (C-reactive protein/Albumin ratio, CAR) is important in judging the prognosis of malignant tumors,8–11 but research reports on NLR, CAR and D-D for thrombotic disease prognosis are rare. Therefore, this study retrospectively analyzed the characteristics of hematology and coagulation indicators in 362 patients with PTE, and explored the clinical value of combined detection of NLR, CAR and D-D for the evaluation of prognosis and death risk of PTE patients.
Materials and Methods
Materials
From January 1, 2015 to December 31, 2019, there were 270,983 discharged patients in our hospital, among which 433 patients were confirmed as PTE mainly through CTPA. And there were 362 cases with complete information and clear prognostic record, including 214 males and 148 females, aged 18–93 years with an average age of 71.2 years old. Tumor embolism, amniotic fluid embolism, fat embolism and other non-venous thromboembolism were excluded. The medical record number, name, gender, age, inpatient department, primary disease(s), inducing factor(s), occurrence location(s), preventive measure(s), relevant examination result(s), treatment method(s) and prognosis of all cases were collected. By the way, all patients’ laboratory parameters were measured at the time point of diagnosis. And 32 healthy subjects were selected as the control group, including 19 males and 13 females, aged 29–51 years.
This study was conducted in accordance with the Declaration of Helsinki. It was discussed and approved by the Ethics Committee of Taicang Hospital affiliated with Soochow University, and written informed consent was signed with relevant personnel. And we confirmed that the data was anonymized or maintained with confidentiality.
Research Methods
According to the data of hospitalized venous thrombus embolism (VTE) cases discharged from our hospital from January 1, 2015 to December 31, 2019 provided by the hospital VTE network, all relevant medical records were reviewed through the medical record center of the hospital, and ultrasonography or CTPA, D-D, CRP, prothrombin time (PT), thrombin time (TT), antithrombin III (AT-III, AT), fibrinogen (FB) and international normalized ratio (INR), as well as hemoglobin (Hb), white blood cell (WBC), NE, LY, monocyte (MO) and platelet (PLT) counts.
Grouping Methods
We divided the prognosis into four types based on the patient’s post-treatment survival status, and classified cured and improved patients as good prognosis group (a total of 298 cases, 82.32%), classified deteriorated and dead patients as poor prognosis group (a total of 64 cases, 17.68%) for comparative analysis. As shown in Table 1, hematological, rheumatic and tumor diseases in the poor prognosis group (35 cases, 54.69%) were significantly more than those in the good prognosis group (67 cases, 22.48%) (Χ2=26.99, P=0.000). Other elements such as gender, age, diabetes and hypertension had no significant correlation with the prognosis of PTE patients.
 |
Table 1 General Data of 362 PTE Patients |
Statistical Analysis
SPSS23.0 software was used for statistical analysis. Measurement data were compared between the two groups using t test, counting data were compared using Chi-square test, and Pearson correlation analysis. Binary logistic regression analysis was used to analyze whether and how much the elevation of NLR, CAR, and D-D contribute to the death of PTE patients. Receiver operating characteristic curve (ROC) was used to analyze the diagnostic value of NLR, CAR, and D-D for the risk of death in patients with PTE. P<0.05 was considered as statistically significant difference.
Results
NLR, CAR, and D-D Test results of PTE Patients and Control Group
Results of NLR and other inflammatory indicators in 362 PTE patients compared with the normal control group are shown in Table 2.
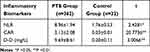 |
Table 2 Comparison of NLR, CAR, and D-D Indicators Between PTE Patients and Control Group |
Table 3 shows the comparative analysis results of specific hematological indexes, inflammatory indexes and coagulation indexes of PTE patients with good prognosis and poor prognosis. It can be seen from Table 3 that Hb, LY, ALB and lymphocyte/monocyte ratio (LMR) levels in the good prognosis group were higher than those in the poor prognosis group. WBC, NE, CAR, CRP, NLR and D-D values were significantly lower than those in the poor prognosis group. For other indexes, including systemic immune inflammation index (SII) and platelet/lymphocyte ratio (PLR), the differences between the two groups had no statistical significance.
 |
Table 3 Comparison of Indicators of PTE Patients Between Good Prognosis Group and Poor Prognosis Group |
Correlation Analysis
Considering that the comparison results of Hb, WBC, NE, LY, CAR, CRP, ALB, NLR, LMR and D-D values were statistically significant between good and poor prognosis groups of PTE patients, and CRP and ALB had constituted a new indicator (CAR); therefore, the correlations between CAR, NLR, D-D and Hb and other indicators were analyzed simultaneously. Specific results are shown in Table 4.
 |
Table 4 Correlation Between CAR and Hb, NLR and Other Indicators |
Logistic Analysis Results of Various Indicators of PTE Patients
We took NLR, CAR, D-D, gender and age as covariates, and death as dependent variable, and then conducted a binary logistic regression analysis. Results showed that high levels of NLR, D-D and CAR could increase the death rate of PTE patients, which also meant NLR, D-D and CAR were independent prognostic factors of PTE death. Specific results are shown in Table 5.
 |
Table 5 Logistic Regression Analysis Results of NLR, D-D and CAR |
Death Risk Assessment of PTE Patients by NLR, CAR and D-D Respectively and in Combination
When assessing the death risk of pulmonary thromboembolism patients, D-dimer alone had the highest sensitivity (93.1%), but the lowest specificity (39.6%), and CAR alone had the highest specificity (68.8%), but lower sensitivity (72.4%). The combined detection of NLR, CAR and D-D significantly improved the diagnostic efficacy of PTE death risk, with the higher sensitivity (86.2%) and specificity (67.6%) at the same time. Specific results are shown in Table 6 and Figure 1.
 |
Table 6 Risk Assessment of Death in Patients with PTE by NLR, CAR and D-D, Respectively, and in Combination |
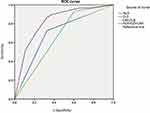 |
Figure 1 Risk assessment results of NLR, CAR and D-D tests separately and in combination for PTE patients. |
Discussion
The study found that the inflammatory indicators of NLR, CAR and D-D in PTE patients were significantly higher than those in the control group, and the NLR, CAR and D-D of PTE patients in the poor prognosis group were also significantly higher than those in the good prognosis group, indicating that PTE patients did have significant inflammatory responses and hypercoagulability trend during the occurrence and development of PTE. Considering that PLR and SII were not statistically significant between the good and poor prognosis groups, that CRP and albumin constituted a new indicator (CAR), and that LMR and NLR had duplicated parameters, we selected NLR, CAR and D-D without repeated parameters to study the prognosis and death risk of PTE.
The importance of D-D in thrombotic diseases has been widely recognized, and it is associated with pulmonary thromboembolism, acute myocardial infarction, cerebral infarction and other thrombotic diseases.12 In this study, the D-D level of poor prognosis PTE patients’ group was significantly higher than that of the control group and good prognosis group, which was consistent with the above literature results.12 Based on Halaby R and other research results,1 our study also showed that D-D was an independent prognostic indicator of PTE (P=0.010). ROC curve showed that the sensitivity of D-D alone in the death risk assessment of PTE was the highest (93.1%), but its specificity was very low (39.6%), which was consistent with the results of Bounds and Kok.13 Therefore, it is necessary to explore new prognostic indicators for PTE or combine several indicators to improve the specificity of risk assessment of death.
The Hb level of PTE patients was lower than that of the control group, which was consistent with our previous research results.14 Inflammation can cause the high expression of Hepcidin, which leads to the failure of the body to use iron and causes anemia in patients. The levels of WBC and NE in the poor prognosis group were significantly higher than those in good prognosis group, while LY was significantly lower than those in good prognosis group, which also indicated that PTE patients had abnormal inflammatory response and immune function. And that may explain why both NLR and CAR in patients were significantly higher than those in the control group, which was consistent with the results reported in the literature.2–4 NE releases inflammasome, a small molecule that participates in the formation of extracellular bactericidal substances of NE, releases protease and interacts with platelets to promote thrombosis,5 indicating a close relationship between inflammation and thrombosis.15 Kapoor6 and Manfredi et al7 all confirmed that NLR is closely related to thrombotic diseases. In this study, NLR alone was also an independent prognostic factor for PTE (P=0.007), and the sensitivity to assess the risk of death was 72.4%, slightly lower than D-D, but the specificity was significantly higher than D-D (67.3%). This result is basically consistent with that of Cavuş et al.16 Therefore, it is of certain value for the evaluation of prognosis of PTE to a certain extent.
CRP is also an important indicator of inflammatory response, and recent studies8–11 have found that CRP is associated with the prognosis of solid tumors, especially CAR combined with nutritional indicator ALB has stronger specificity. However, no study has been reported on the prognosis of PTE, and this study showed that CAR alone was also an independent prognostic factor of PTE (P=0.03). The sensitivity was 72.4%, slightly lower than D-D but consistent with NLR, and the specificity of CAR was the highest (68.8%).
ROC curve results showed that combined detection of NLR, D-D and CAR significantly improved the diagnostic efficacy of PTE death risk, with the higher sensitivity (86.2%) and specificity (67.6%) at the same time. And it showed the largest area under the AUC curve (0.821) and the highest Youden (0.528), which represents the highest diagnostic value. It is suggested that the combined test of these three indicators can make up for the deficiency of a single indicator in the assessment of the death risk of PTE patients, and reflect the occurrence, development and progression degree from different aspects. Therefore, it has a good prediction significance for the risk of death, which is conducive to better clinical guidance.
However, this study was a retrospective and single-center study, and only analyzed the relationship between hematology and coagulation indicators and prognosis, without including the underlying diseases and primary diseases of PTE as well as other influencing factors. Besides, the control group was much smaller and younger than the PTE group. Therefore, this result may have limitations and bias. We will further conduct necessary prospective validation, or expand the number of cases and control group, unify the diagnostic criteria and parameter indicators, and strictly apply the inclusion and exclusion criteria of patients in our further study, in order to clarify the relationship between NLR, D-D and CAR and the prognosis of PTE, as well as its true significance for the risk assessment of death.
Conclusion
Patients with pulmonary thromboembolism highly expressed of neutrophil/lymphocyte ratio, C-reactive protein/albumin ratio and D-dimer. The increase in NLR, D-D, and CAR were independent prognostic factors of PTE death. The combined detection of these three indicators can improve the assessment efficacy of the risk of death in patients with pulmonary thromboembolism.
Data Statement
No further data will be shared.
Ethics Approval and Consent to Participant
This study was conducted in accordance with the Declaration of Helsinki. It was discussed and approved by the Ethics Committee of Taicang Hospital affiliated with Soochow University, and written informed consent was signed with relevant personnel. And we confirmed that the data was anonymized or maintained with confidentiality.
Acknowledgments
All authors read and approved the final manuscript. Tiantian Shan and Xinran Li are co-first authors for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Halaby R, Popma CJ, Cohen A, et al. D-Dimer elevation and adverse outcomes. J Thromb Thrombolysis. 2015;39(1):55–59. doi:10.1007/s11239-014-1101-6
2. Wiwanitkit V. Neutrophil to lymphocyte ratio in allergic rhinitis. Eur Arch Otorhinolaryngol. 2016;273(10):3443. doi:10.1007/s00405-015-3886-0
3. Lee H, Um SJ, Kim YS, et al. Association of the neutrophil-to-lymphocyte ratio with lung function and exacerbations in patients with chronic obstructive pulmonary disease. PLoS One. 2016;11(6):e0156511. doi:10.1371/journal.pone.0156511
4. Kolber W, Kuśnierz-Cabala B, Maraj M, et al. Neutrophil to lymphocyte ratio at the early phase of acute pancreatitis correlates with serum urokinase-type plasminogen activator receptor and interleukin 6 and predicts organ failure. Folia Med Cracov. 2018;58(4):57–74.
5. Petersen E, Wågberg F, Angquist KA. Proteolysis of the abdominal aortic aneurysm wall and the association with rupture. Eur J Vasc Endovasc Surg. 2002;23(2):153–157. doi:10.1053/ejvs.2001.1572
6. Kapoor S, Opneja A, Nayak L. The role of neutrophils in thrombosis. Thromb Res. 2018;170:87–96. doi:10.1016/j.thromres.2018.08.005
7. Manfredi AA, Ramirez GA, Rovere-Querini P, et al. The neutrophil’s choice: phagocytose vs make neutrophil extracellular traps. Front Immunol. 2018;9:288. doi:10.3389/fimmu.2018.00288
8. Joffe L, Dwyer S, Glade Bender JL, et al. Nutritional status and clinical outcomes in pediatric patients with solid tumors: a systematic review of the literature. Semin Oncol. 2019;46(1):48–56. doi:10.1053/j.seminoncol.2018.11.005
9. Bairey O, Shacham-Abulafia A, Shpilberg O, et al. Serum albumin level at diagnosis of diffuse large B- cell lymphoma: an important simple prognostic factor. Hematol Oncol. 2016;34(4):184–192. doi:10.1002/hon.2233
10. Kinoshita A, Onoda H, Imai N, et al. The C-reactive protein/albumin ratio, a novel inflammation- based prognostic score, predicts outcomes in patients with hepatocellular carcinoma. Ann Surg Oncol. 2015;22(3):803–810. doi:10.1245/s10434-014-4048-0
11. Zhou T, Zhan J, Hong S, et al. Ratio of C-reactive protein/albumin is an inflammatory prognostic score for predicting overall survival of patients with small-cell lung cancer. Sci Rep. 2015;5:10481. doi:10.1038/srep10481
12. Li WJ, Sha M, Ma W, et al. Efficacy evaluation of D-dimer and modified criteria in overt and nonovert disseminated intravascular coagulation diagnosis. Int J Lab Hematol. 2016;38(2):151–159. doi:10.1111/ijlh.12467
13. Bounds EJ, Kok SJ. D Dimer. In: StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2021, StatPearls Publishing LLC.; 2021.
14. Cheng Z, Yan M, Lu Y, et al. Expression of serum BMP6 and hepcidin in cancer-related anemia. Hematology. 2020;25(1):134–138. doi:10.1080/16078454.2020.1738098
15. Gupta N, Sahu A, Prabhakar A, et al. Activation of NLRP3 inflammasome complex potentiates venous thrombosis in response to hypoxia. Proc Natl Acad Sci USA. 2017;114(18):4763–4768. doi:10.1073/pnas.1620458114
16. Cavuş UY, Yildirim S, Sönmez E, et al. Prognostic value of neutrophil/lymphocyte ratio in patients with pulmonary embolism. Turk J Med Sci. 2014;44(1):50–55. doi:10.3906/sag-1302-47
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
