Back to Journals » Research and Reports in Urology » Volume 12
Evaluation of Preoperative Tamsulosin Role in Facilitating Ureteral Orifice Navigation for School-Age Pediatric Ureteroscopy
Authors Morley C , Hajiran A, Elbakry AA, AL-Qudah HS, AL-Omar O
Received 25 September 2020
Accepted for publication 19 October 2020
Published 16 November 2020 Volume 2020:12 Pages 563—568
DOI https://doi.org/10.2147/RRU.S283126
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jan Colli
Chad Morley,1 Ali Hajiran,1 Amr A Elbakry,1 Hosam S AL-Qudah,2 Osama AL-Omar1
1Department of Urology, West Virginia University, Morgantown, WV, USA; 2Division of Urology, AL Zahra Hospital, Dubai, United Arab Emirates
Correspondence: Osama AL-Omar
Department of Urology, West Virginia University, PO Box 9238, 6300 HSS, Morgantown, WV, PO Box 9238, 6300 HSS, USA
Tel +1 304-293-2706
Fax +1 304-293-2807
Email [email protected]
Purpose: To address whether preoperative tamsulosin increases the rate of successful ureteral orifice navigation for ureteroscopy (URS) without prestenting in school-age pediatric patients.
Methods: We retrospectively reviewed all pediatric patients who had undergone ureteroscopy (URS) at our institution from 2013 to 2020. Patients were divided into two groups: those who had received tamsulosin 0.4 mg daily ≥ 48 hours preoperatively and those who had not. Statistical analysis was done using independent-sample t-tests and Mann–Whitney U tests for continuous variables, and χ2 and Fisher’s exact tests were used for categorical variables. Multivariate analysis was done using binary logistic regression test.
Results: Overall, successful ureteral orifice navigation occurred in 44 of 50 patients (88%) who had received tamsulosin and 17 of 26 (65.4%) who had not (p=0.019). On further subanalysis based on stone location and instrumentation used, successful ureteral orifice navigation had occurred in 21 of 24 patients (87.5%) in the tamsulosin group and one of five (20%) in the no-tamsulosin group for semirigid ureteroscopy for mid–distal ureterolithiasis (p=0.007). For proximal ureteral and renal stones, successful ureteral orifice navigation with a flexible ureteroscope or ureteral access sheath had occurred in 23 of 26 patients (88.5%) in the tamsulosin group and 16 of 21 (76.2%) in the no-tamsulosin group (p=0.437). Multivariate analysis showed no significant difference between success rates in the two groups after controlling for patient weight, height, BMI, and stone location. We did not observe any adverse effects from tamsulosin.
Conclusion: This is the first study to evaluate preoperative tamsulosin on successful ureteral orifice navigation in school-age pediatric patients. Although not reaching statistical significance, further evaluation should be done on larger cohorts. Patient height was found to be an independent predictor of successful ureteral orifice navigation.
Keywords: ureteroscopy, pediatric, tamsulosin, ureteral orifice navigation, α-blockers, renal stone
Introduction
The incidence of pediatric urolithiasis has risen dramatically over the past few decades, with a reported rate of 4% per year.1 This trend has emphasized the need for improved strategies for managing ureteral calculi in this age-group. The 2016 American Urological Association (AUA) guidelines on the surgical management of stones recommend that clinicians offer ureteroscopy (URS) for pediatric patients with ureteral stones who are unlikely to pass the stones or have failed a trial of observation and/or medical expulsive therapy.2 A unique aspect of pediatric URS is the smaller ureteral diameter, which often results in failure to access the ureter during an initial URS attempt.
There is controversy regarding the practice of routine prestenting and balloon dilation to gain ureteral access in children.3 The AUA guidelines recommend against the routine use of prestenting. Balloon dilation of the ureteral orifice carries the risk of ureteral perforation and ureteral stricture, due to tissue ischemia.3 Ureteral orifice navigation is often limited at the level of the ureteral orifice or intramural ureter. α1 adrenergic receptors are densely located at this level, and α-antagonists can reduce the tension of the intramural segment.4 In pediatric patients, studies have demonstrated that off-label use of tamsulosin is associated with an increased rate and decreased time of passage of ureteral calculi.5 The purpose of this study was to evaluate if preoperative treatment with tamsulosin is associated with an increased rate of successful first-time ureteral orifice navigation in a school-age pediatric population, defined as patients 5–18 years old.
Methods
After obtaining institutional research ethics board approval (IRB 1,705,600,370), we retrospectively reviewed all pediatric patients who had undergone URS at our institution from January 2013 to July 2020. All cases had been performed by a single surgeon (senior author) using a standard approach for ureteral navigation based on the location of the stone. A semirigid ureteroscope (Wolf 4.5 Fr) was used for mid–distal ureteral stones, while a flexible ureteroscope (Storz 7.5 Fr) with or without a ureteral access sheath (Cook 9.5 Fr) was used for proximal ureteral and renal stones, but always attempting sheath placement first. Our technique for URS in pediatric patients is as follows. For semirigid URS, we start with cystoscopy and retrograde pyelography, followed by guide-wire insertion up to the renal pelvis. Then, we insert the ureteroscope over the wire under direct vision up to the stone location. No ureteral orifice dilation is attempted or performed prior to URS insertion. In flexible URS, we start with cystoscopy and retrograde pyelography, followed by guide-wire insertion up to the renal pelvis. We attempt to insert a ureteral access sheath (Cook 9.5 Fr) under fluoroscopic guidance, and the ureteroscope is then advanced via the ureteral access sheath. If unable to advance the ureteral access sheath, we advance the ureteroscope over the guide wire under direct vision up to the stone level or renal pelvis. In both situations, if navigation of the ureteral orifice is unsuccessful, then a ureteral JJ stent is placed for 10–14 days before attempting a second URS.
Success in our study was defined as being able to engage the instrument (ureteroscope or ureteral access sheath) in the ureteral orifice to be able to perform the intended procedure. Patients with previously placed ureteral stents and those aged <5 years or >18 were excluded from the study. Patients were divided into two groups: those who had received tamsulosin 0.4 mg daily for at least 48 hours preoperatively (this timing was chosen because tamsulosin was found to have rapid onset of action after 8 hours when used for benign prostatic hyperplasia, so 48 was chosen in our study to allow for sufficient time for distal ureter relaxation) and those who had not received tamsulosin preoperatively. After May 2017, reviewing our data and the observation of a higher success rate for navigating the ureteral orifice with tamsulosin, it became our standard practice to give those patients who had renal stones at least a 2-days cours of tamsulosin prior to undergoing URS. This explains the high number of patients on tamsulosin in this group. Statistical analysis was then performed using independent sample t-tests and Mann–Whitney U tests for continues variables, and χ2 test and Fisher’s exact test for categorical variables. Multivariate analysis was done using binary logistic regression testing. Statistical analysis was done using IBM SPSS version 24.
Results
A total of 103 patients had undergone URS: 27 were excluded, 50 of 76 (65.8%) had received preoperative tamsulosin, and 26 of 76 (34.2%) had not. There were no significant differences in age, sex, BMI, or size of calculi, between the groups, but there were for patient weight, height, and stone location. (Table 1). We included patients who had received tamsulosin for at least 48 hours, with a median of 7 days (range 2–28 days). Those who had received tamsulosin for <48 hours or had not received tamsulosin at all were included in the nontreatment group. Successful first-time ureteral orifice navigation was achieved in 44 of 50 patients (88%) who received preoperative tamsulosin and 17 of 26 patients (65.4%) who did not (p=0.019, Table 2). We further stratified the groups based on stone location. In patients with proximal ureteral and renal stones, successful first-time ureteral orifice navigation was achieved in 23 of 26 (88.5%) in the tamsulosin group and 16 of 21 (76.2%) in those who had not. (p=0.437). For patients with mid–distal ureteral calculi, successful ureteral orifice navigation was achieved in 21 of 24 (87.5%) who had received preoperative tamsulosin and one of five patients (20%) who had not (p=0.007). No adverse effects from the use of tamsulosin were reported. On multivariate analysis, preoperative tamsulosin failed to maintain significance and height was found to be an independent predictor of successful ureteral orifice navigation (Table 3).
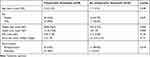 |
Table 1 Characteristics of Patients and Associated Stone Burden |
 |
Table 2 Rates of Successful First-Time Ureteral Orifice Navigation in Pediatric Patients Who had Received Preoperative Tamsulosin Compared to those who had not |
 |
Table 3 Multivariate Analysis of Predictors of Successful Ureteral Orifice Navigation without Prestenting in Pediatric Patients |
Discussion
The prevalence of urolithiasis in children has been increasing dramatically. One tertiary-care center reported a fivefold increase in incidence of pediatric urolithiasis over 10 years, with a recurrence rate of approximately 40%.6 Most urinary calculi in the kidneys or ureters are comprised of either calcium oxalate or calcium phosphate and associated with an identifiable metabolic abnormality.7 Adolescents with ureterolithiasis may present similarly to adult patients; however, younger children can present a diagnostic challenge, due to aspecific pain localized to the abdomen or pelvis. As per the 2016 AUA guidelines, an initial trial of observation with or without medical expulsion therapy is appropriate in children with uncomplicated ureteral stones ≤10 mm, because many children will pass their stones spontaneously.2
Although spontaneous passage of ureteral calculi is more likely in children than adults, many children may still require surgical intervention. In a review of 7,921 children with urolithiasis, 22% eventually required stone-related surgery.8 Of those children, 25% required two to three procedures.8 It is recommended that clinicians offer URS for pediatric patients with ureteral stones who are unlikely to pass the stones or who have failed a 4- to 6-week trial of observation and/or medical expulsive therapy.2 There are some similarities in performing URS in the adult and pediatric populations; however, there are also some important differences: a pediatric patient has different anesthetic requirements and risks, a higher risk of lifelong recurrent urological interventions, and smaller anatomy, which requires smaller instruments and technical expertise.9 A unique aspect of pediatric URS is the smaller ureteral diameter, which often results in failure to access the ureter during an initial URS attempt. In a review of 251 pediatric URS cases, 76.6% of prestented patients required stent placement, due to unsuccessful instrumentation of the ureteral orifice.10 There is controversy regarding the practice of routine prestenting and balloon dilation to gain ureteral access in children.3 Although some studies have reported higher URS success rates with prestenting, many clinicians question whether the benefits outweigh the disadvantages of an additional procedure. Additionally, this practice will commit all patients to two or more procedures under anesthesia, which is another burden on both patients and health systems. The most recent AUA guidelines recommend against the routine use of prestenting.2 In children, balloon dilation of the ureteral orifice is avoided by many clinicians, due to the risk of ureteral perforation and ureteral stricture due to tissue ischemia.3
During pediatric URS, ureteral access is often limited at the level of the intramural ureter or ureteral orifice. α-adrenergic receptors have been shown to be present along the entire length of the human ureter, including subtypes α1a, α1b, and α1d.11 The distal ureter has the highest concentration of α receptors, particularly the α1d subtype.11 α-receptor stimulation increases the force of ureteral contraction and frequency of ureteral peristalsis.12 In adults, the use of α-receptor antagonists has been shown to increase the spontaneous passage rates of ureteral stones, reduce analgesic requirements, and decrease time to stone passage.13–15 The likely mechanism of α-antagonists in this setting involves reduction of ureteral spasms, increasing pressure proximal to the stone, relaxing the ureter in the region of and distal to the calculus, and decreasing the tone and frequency of contractions.12,16 Tamsulosin is the most widely studied α1 antagonist in the treatment of ureteral calculi. Sato et al demonstrated that tamsulosin has high affinity for α1a and α1d receptors.17 Tamsulosin demonstrates a rapid onset of action (4– 8 hours) based on Qmax after the first dose, which is why 48 hours was chosen in our study as sufficient time to expect intramural ureteral relaxation.18 A multi-institutional cohort study in children found that the odds of passage of ureteral stones were greater in children prescribed tamsulosin versus analgesics alone.5 In this study, no adverse effects of tamsulosin were noted in 99 children who received treatment.5 Mokhless et al similarly demonstrated no clinically significant adverse effects in children treated with tamsulosin at doses of 0.4 mg daily for children aged >4 years and 0.2 mg daily for children aged <4 years.19 Recent literature has demonstrated that the use of medical expulsion therapy in children is now increasing nationwide.20
To our knowledge, there have been no studies assessing the use of preoperative α-adrenergic antagonists for pediatric navigation of thye ureteral orifice, whether for the purpose of semirigid/flexible URS or passing a ureteral access sheath. In theliterature on adults, Abdelaziz et al reported a prospective randomized trial to assess if preoperative α-adrenergic blockers increased the rate of successful ureteral access.21 In this study, 98 patients (>18 years old) were randomized to receive tamsulosin for 1 week prior to URS versus no treatment. They found that the treatment group had a higher success rate (94.1% versus 87.2%) and lower complication rate (11.7% versus 19.1%) than the control group.21
In our study, successful first-time ureteral orifice navigation was achieved in 44 of 50 patients (88%) in the treatment group and only 17 of 26 patients (65.4%) in the nontreatment group, which was statistically significant (p=0.019) on univariate analysis. Further stratification of the data showed that in the mid–distal ureteral group, there was statistical significance (p=0.007). However, in the proximal/renal group, there was a significantly higher success rate in the tamsulosin group (88.5%) vs 76.2% in the nontreatment group, but it did not reach statistical significance (p=0.437). We suspect that the higher success rate in ureteral orifice navigation in patients that had received preoperative tamsulosin was associated with relaxation of distal ureteral tone, which facilitates advancement of the ureteroscope or ureteral access sheath. However, these findings were not statistically significant after controlling for weight, height, and stone location on multivariate analysis, which may be due to the small sample and lack of randomization. Assessing the effect of duration of tamsulosin on relaxation of the ureteral orifice or intramural part of the ureter is beyond the scope of this study. However, with the observation of higher successful navigation of the ureteral orifice with at least 48 hours (median 7 days), it will not be a surprise for us if we obtain similar results with longer-duration tamsulosin use.
We acknowledge the many limitations of this study. First, all surgeries were performed by a single surgeon at a single center, although this may give a strength in standardization of the comparison. Second, although all patients in the treatment group were reported to have received at least 48 hours of tamsulosin prior to surgery, some patients received longer courses of therapy, given the different durations of trials of passage and operative scheduling limitations. Third, there were statistically differences in weight, height, and stone location between the groups. As a retrospective study, there is a risk of selection bias, and our sample size for mid–distal ureteral stones was small, as there were few patients with distal ureteral stones who had been referred without prior medical expulsive therapy. This is mainly related to the widely published literature and AUA guidelines on the positive effect of α-blockers to facilitate passing ureteral stones, and it has become general practice to place those patients on tamsulosin by urologists, pediatricians, and ER physicians before referring patients to pediatric urology services. Therefore, only five patients had had distal URS without tamsulosin. Finally, our observations should be validated using a prospective randomized multi-institutional trial.
Conclusion
This study is the first to assess the effect of preoperative tamsulosin on navigating the ureteral orifice in school-age pediatric patients. Although preoperative treatment with tamsulosin failed to show a statistically significant difference for successful ureteral orifice navigation, the trend for higher success rate following preoperative tamsulosin warrants further evaluation using a larger sample in a randomized controlled trial. Patient height was found to be an independent predictor of successful ureteral orifice navigation in this age-group.
Data-Sharing Statement
Our data set is available from the correspondending author upon reasonable request. Code availability: IBM SPSS version 24.
Ethics Approval
This was a retrospective study that included subjects data that already existed, and IRB approval was obtained from the West Virginia University ethical board (IRB 1,705,600,370). No consent was obtained from patients, as this was a retrospective study with very minimal risk of harm to participants. Therefore, the IRB at our institution granted us a waiver from obtaining consent. Data were collected from electronic medical records and kept as deidentified data in Excel. The key codes to reidentify the data are kept only on a secure institutional computer that can be accessed only by the PI. Patients and their data were managed according to the Declaration of Helsinki.
Consent to Participate
Consent was waived, as this was a retrospective study involving retrospective data collection.
Consent for Publication
This was not obtained.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data, took part in drafting the article or revising it critically for important intellectual content, agreed to submit to the current journal, gave final approval to the version to be published, and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors have no conflicts of interest or financial disclosure.
References
1. Dwyer ME, Krambeck AE, Bergstralh EJ, Milliner DS, Lieske JC, Rule AD. Temporal trends in incidence of kidney stones among children: a 25-year population based study. J Urol. 2012;188(1):247–252. doi:10.1016/j.juro.2012.03.021
2. Assimos D, Amy Krambeck NL, Miller MM, et al. Surgical management of stones: American urological association/endourological society guideline, Part I. J Urol. 2016;196(4):1153–1160. doi:10.1016/j.juro.2016.05.090
3. Schneck FX, Ost MC. Surgical management of pediatric stone disease. In: Wein AJ, Kavoussi LR, Partin AW, Peters CA, editors. Campbell-Walsh Urology. Vol. Chapt 135.
4. Troxel SA, Jones AW, Magliola L, et al. Physiologic effect of nifedipine and tamsulosin on contractility of distal ureter. J Endourol. 2006;20(8):565–568. doi:10.1089/end.2006.20.565
5. Tasian GE, Cost NG, Granberg CF, et al. Tamsulosin and spontaneous passage of ureteral stones in children: a Multi-Institutional Cohort Study. J Urol. 2014;192(2):506–511. doi:10.1016/j.juro.2014.01.091
6. VanDeroot K, Wiesen J, Frank R, Vento S, Chandra M, Trachtman H. Urolithiasis in pediatric patients: a single center study of incidence, clinical presentation and outcome. J Urol. 2007;177(6):23000–23005.
7. Copelovitch L. Urolithiasis in children: medical approach. Pediatr Clin North Am. 2012;59(4):881–896. doi:10.1016/j.pcl.2012.05.009
8. Routh JC, Graham DA, Nelson CP. Trends in imaging and surgical management of pediatric urolithiasis at American pediatric hospitals. J Urol. 2010;184:1816–1822.
9. Guven S, Basiri A, Varshney AK, et al. Examining pediatric cases from the CROES Ureteroscopy Global Study. Urology. 2017;101:31–37. doi:10.1016/j.urology.2016.11.020
10. Gocke MI, Telli O, Akinci A, et al. Effect of presenting on complication rates of ureteroscopy in pediatric population. J Endourol. 2016;30(8):850–855. doi:10.1089/end.2016.0201
11. Itoh Y, Kojima Y, Yasui T, Tozawa K, Sasaki S, Kohri K. Examination of alpha 1 adrenoreceptor subtypes in the human ureter. Int J Urol. 2000;14(8):749–753. doi:10.1111/j.1442-2042.2007.01812.x
12. Lipkin M, Shah O. The use of alpha blockers for the treatment of nephrolithiasis. Rev Urol. 2006;8(Suppl 4):S35–S42.
13. Pedro RN, Hinck B, Hendlin K, et al. Alfuzosin stone expulsion therapy for distal ureteral calculi: a double-blind, placebo controlled study. J Urol. 2008;179(6):2244. doi:10.1016/j.juro.2008.01.141
14. Hollingsworth JM, Rogers MA, Kaufman SR, et al. Medical therapy to facilitate urinary stone passage: a meta-analysis. Lancet. 2006;368(9542):1171. doi:10.1016/S0140-6736(06)69474-9
15. Hermanns T, Sauermann P, Rufibach K, et al. Is there a role for tamsulosin in the treatment of distal ureteral stones of 7mm or less? Results of a randomised, double-blind, placebo-controlled trial. Eur Urol. 2009;56(3):407. doi:10.1016/j.eururo.2009.03.076
16. Weiss RM. Physiology and pharmacology of the renal pelvis and ureter. In: Wein AJ, Kavoussi LR, Partin AW, Peters CA, editors. Campbell’s Urology. Vol. Chap 43, 2.
17. Sato S, Hatanka T, Yuyama H, et al. Tamsulosin potently and selectively antagonizes human recombinant α(1A/1D)-adrenoceptors: slow dissociation from the α(1A)-adrenoceptor may account for selectivity for α(1A)-adrenoceptor over α(1B)-adrenoceptor subtype. Biol Pharm Bull. 2012;35(1):72–77. doi:10.1248/bpb.35.72
18. Lepor H. Phase III multicenter placebo-controlled study of tamsulosin in benign prostatic hyperplasia. Tamsulosin Investigator Group. Urology. 1998;51(6):892–900. doi:10.1016/S0090-4295(98)00126-5
19. Mokhless I, Zahran A-R, Youssif M, et al. Tamsulosin for the management of distal ureteral stones in children: a prospective randomized study. J Pediatr Urol. 2012;8(5):544. doi:10.1016/j.jpurol.2011.09.008
20. Ellison JS, Merguerian PA, Fu BC, et al. Use of medical expulsive therapy in children: an assessment of nationwide practice patterns and outcomes. J Pediatr Urol. 2017;13(5):509 e7. doi:10.1016/j.jpurol.2017.04.019
21. Abdelaziz AS, Kidder AM. Tamsulosin therapy improved the outcome of ureterorenoscopy for lower ureteral stones: a prospective, randomized, controlled, clinical trial. Afr J Urol. 2017;23:148–153. doi:10.1016/j.afju.2015.12.003
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
