Back to Journals » Patient Preference and Adherence » Volume 15
Evaluation of Patient’s Knowledge of Atorvastatin Information in Patient Information Leaflets: A Pre-Post Intervention Study in Thailand
Authors Pongpunna S, Pratipanawatr T, Wongtaweepkij K , Jarernsiripornkul N
Received 23 August 2021
Accepted for publication 12 October 2021
Published 28 October 2021 Volume 2021:15 Pages 2377—2387
DOI https://doi.org/10.2147/PPA.S334668
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Johnny Chen
Supawinee Pongpunna,1 Thongchai Pratipanawatr,2 Kamonphat Wongtaweepkij,3 Narumol Jarernsiripornkul1
1Division of Clinical Pharmacy, Faculty of Pharmaceutical Sciences, Khon Kaen University, Khon Kaen, Thailand; 2Department of Medicine, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand; 3Division of Clinical Pharmacy, Faculty of Pharmacy, Srinakharinwirot University, Nakhon Nayok, Thailand
Correspondence: Narumol Jarernsiripornkul
Division of Clinical Pharmacy, Faculty of Pharmaceutical Sciences, Khon Kaen University, Khon Kaen, 40002, Thailand
Tel +66-4334-8353
Fax +66-4320-2379
Email [email protected]
Purpose: This study aimed to evaluate the effect of using atorvastatin PIL on patients’ medication knowledge, perceptions of the PIL usefulness, their anxiety about the medication, and factors related to these aspects.
Patients and Methods: A pre-post intervention study was conducted in outpatients at a university hospital. Patients prescribed atorvastatin were enrolled using systematic random sampling. Participants were asked to complete Self-Administered Questionnaire to assess atorvastatin knowledge at baseline. An atorvastatin-PIL produced by the manufacturer was introduced to the participants as the intervention. One month after receiving the PIL, the participants were re-assessed. Ten questions were developed to assess atorvastatin knowledge and visual analog scale (VAS) was used to assess perceived benefits of using the PIL and patient anxiety about the medication. Multiple linear regression was used to assess the related factors.
Results: Of 450 questionnaires distributed, 370 were returned. Atorvastatin knowledge significantly increased with mean score of 5.06± 1.92 at baseline to 8.34± 1.79 at 1-month after intervention. Reading all sections of the PIL (p=0.017) and working for civil service (p=0.006) were associated with higher knowledge scores at baseline and after intervention. Low educational level was associated with lower knowledge scores at baseline (p=0.002), but experience of allergy (p=0.042) was associated with higher knowledge scores after the intervention. Patients had high level of perceived usefulness from the PIL (average scores=8.87± 1.83) and low level of anxiety (average scores=3.69± 3.06). Reading all sections of the PIL (p=0.007) and taking more than 5 medications (p=0.012) were related to perceived usefulness of the PIL. Females (p< 0.001) and herbal supplement users (p=0.048) were related to anxiety about the medication.
Conclusion: PILs could improve medication knowledge in patients. Patients’ perceptions of benefits of PILs were high and anxiety about medication was low. Use of PILs should be encouraged to improve patients’ knowledge and appropriate use of medications.
Keywords: patient information leaflet, medication knowledge, atorvastatin, perceived benefits, anxiety
Introduction
In recent years, it has become increasingly important to improve patient’s knowledge about their diseases and medications to help them to make involved decisions about their treatment. Patients typically need both basic and specific information about their medicines and treatment,1 which includes discussing the adverse effects of their medicines.1,2 Many studies have found that patients lack essential knowledge about their medications such as the correct use of medicines, potential side effects, and how to self-monitor while taking medicines.3–5 Patients report that although they are provided with medicine information by their healthcare providers during consultation, many of them forget that information after the consultation.6,7
Statins are widely prescribed for dyslipidemia and coronary heart disease (CAD) and are normally used long-term. Atorvastatin has been the most extensively used statin worldwide.8 In Thailand, atorvastatin 40 mg is included on the National List of Essential Medicines 2012 (NLEM) and the prescribing volume is high in many hospitals. Although atorvastatin is very effective at lowering cholesterol levels, it sometimes induces adverse drug reactions (ADRs).9–12 The low adherence rate for statins within the first year of use has been reported to be mainly due to patient concerns about statin ADRs.13–15 A lack of knowledge about atorvastatin can reduce patient confidence and lower adherence.
Written drug information is provided to patients to help increase the amount of drug information that they retain.16 Patient information leaflets (PILs) have an important role to play during counseling by including patients in decision making about their medications.17,18 A number of studies have investigated the effect of PILs on patients’ knowledge19,20 and medication anxiety, as well as their potential to influence patients to discontinue therapy due to fear of possible ADRs.16 However, most of these studies are short-term studies, focused on PILs produced by the researchers, or conducted in small populations. Few studies have investigated any association of improvement in patients’ knowledge with the usefulness and emotions involved in the use of PILs in large populations.
In Thailand, the pharmaceutical manufacturers of atorvastatin produce a PIL for all packages, but there have been no studies to test the benefits and the effect of PILs on patients’ knowledge, as well as effects on patients’ anxiety. The Thai-PILs produced by manufacturers have not been evaluated by health authorities or consumers to explore how much understanding and knowledge is received from PILs. This study used PILs produced by manufacturers, which is different from other studies that have used PILs produced by the researchers.19–21 Thus, this study was conducted to assess patients’ knowledge about atorvastatin at baseline and after reading the PILs, and to determine the factors affecting their knowledge. In addition, patients’ opinions about the benefits of using PILs and their anxiety after using the PILs were investigated.
Methods
Study Design and Setting
This was a pre-post interventional study conducted in outpatient clinics at Queen Sirikit Heart Center, a university hospital in the Northeastern Thailand between February to October 2017.
Participants
Patients aged 18 years and older who had taken atorvastatin and were able to complete the questionnaire were selected using a systematic random sampling method. Patients who were prescribed atorvastatin were identified by their prescriptions. These prescriptions were reviewed by the hospital pharmacists. Every second patient waiting for pharmacy service that had atorvastatin-containing prescriptions were selected and invited to take part in the study by the researcher. The sample size for the pretest-posttest study was calculated by using an alpha error at 0.05, a power of 0.90 (beta = 0.1), and an effect size of 0.20. The approximate sample size was 263. To achieve adequate response from calculated sample size, we distributed a total of 450 questionnaires at the Queen Sirikit Heart Center.
Study Instruments
Questionnaire Development and Testing
The pre-test questionnaire consisted of two sections: (1) participants’ demographic data including age, gender, education level, occupation, health care program status and past medical history and (2) atorvastatin knowledge test consisting of 10 multiple choice questions about the name of the medicine, indication, contraindication, precaution, dosage regimen, administration, ADRs and ADR monitoring, and storage.
The post-test questionnaire consisted of two sections: (1) the atorvastatin knowledge test and (2) patients’ behavior survey on the use of PILs and their opinions on potential benefits and anxiety after reading the PILs. A visual analog scale from 0 (least) to 10 (most) was used to assess patients’ perception of benefits and anxiety score.21,22
The questionnaire was tested for content validity by three pharmacists who had experience in medicine information. The index of consistency was 0.97 indicating good content validity. The questionnaire was then piloted with 15 patients to ensure its readability and ease of understanding.23 After piloting, the questionnaire was modified to be used for the actual study.
Atorvastatin PILs
The atorvastatin PIL used in this study was produced by the originator manufacturer and was available inside medicine boxes or packages. The PIL, printed on 2-sided paper, contained 6 main topics as follows: what is the medicine and what is it used for; precautions before using the medicine; how to take the medicine; possible side effects; how to store the medicine, and information about the manufacturer. The PIL was written in Thai with simple language for lay people’s understanding, and was not available online.
Data Collection
The pre-test questionnaire and a cover letter explaining the aims of the study were distributed to participants at outpatient clinics in the hospital by a researcher. Informed consent was obtained from each participant. The pre-test questionnaire was returned to the researcher directly after completion. The researcher then provided participants with a PIL of atorvastatin and suggested they read it at home. The post-test was performed after one month. The post-test questionnaire was sent to the participants by mail one week before deadline with an enclosed atorvastatin PIL. The participants were instructed to read the PIL again, complete the post-test questionnaire and return the questionnaire by mail. If the questionnaires were not returned within one-week, non-responders received a personal contact by phone and a reminder letter.
Data Analysis
For the atorvastatin knowledge test, each correct answer was worth one point (total score=10). The scores were divided into pass (total score ≥ 8 points) and not pass (total score < 8 points) categories based on Bloom’s cut-off point about knowledge/attitude/practice assessment and a previous study of knowledge assessment in Thai patients.21,24 Descriptive statistics are used to describe the demographic data. The atorvastatin knowledge scores and the scores of the perceived benefits and anxiety about medication after reading the PIL are presented as mean ± standard deviation (S.D.). Pre-test and post-test atorvastatin knowledge scores were compared by using Paired sample t-test. Chi-square test was used to compare sub-groups for categorical data, and Mc Nemar’s test was used for comparison of pre-test and post-test within groups. Kolmogorov–Smirnov test was used to assess normal distribution of the data. For factors associated with pre-test and post-test knowledge scores (univariate analysis), independent t-test and one-way ANOVA or Mann Whitney U-test and Kruskal–Wallis test, where appropriate, were used to compare the knowledge scores between groups. Multivariate linear regression analysis was used to evaluate the factors that might affect pre-test and post-test knowledge scores, and factors related to benefit and anxiety scores after reading the PIL. P-value less than 0.05 indicated statistical significance. All data were analyzed using IBM SPSS for Windows version 19.0.
Ethical Approval
The study protocol was approved by the Khon Kaen University Ethics Committee for Human Research (HE591091) and conducted in accordance with the Declaration of Helsinki.
Results
Demographic Data
A total of 450 participants completed pre-test questionnaires and 370 of them returned completed post-test questionnaires; hence the response rate was 82.2%. Most of the respondents were male (n=231, 62.4%), with a mean age of 58.35 ± 7.62 years old (range = 32–83). The majority of respondents had a bachelor’s degree or higher (n=154, 41.7%) and most of them worked as civil servants (n=169, 45.8%). The majority of respondents had more than one underlying disease (n=156, 42.2%), received more than five concomitant drugs (n=162, 44.4%), and had used atorvastatin for more than one year (n=257, 70.6%).
Comparison of Atorvastatin Knowledge Between Pre-Test and Post-Test
The average score on the knowledge pre-test (baseline) was 5.06±1.92, and the post-test was 8.34±1.79. There was a significant difference in the total score before and after reading PILs (p<0.001). In the pre-test, respondents gave correct answers about atorvastatin including the name of the medicine (n=143, 38.6%), serious ADRs (n=139, 37.6%), contraindications (n=122, 33.0%), ADR monitoring (n=86, 23.2%), and the effect of the medicine on glucose level (n=36, 9.7%). The percentage of correct answers for each question was less than 80%, of which the highest percentage was 79.7% (n=295). The question that had the lowest percentage of correct answers was “how does this medicine affect sugar level” (n=36, 9.7%).
After reading the PIL, more than 70% of respondents gave correct answers for almost all questions, except for information of serious ADRs (n=137, 37.0%). The number of respondents who gave correct answers about the effect of the medicine on glucose level increased to 277 (74.9%). The questions that showed the most improvement in the proportion of correct responses from the pre-test to the post-test were “What does this medicine affect the sugar levels?” (9.7% at baseline vs 74.9% at 1 month), “What organ that you should check after receiving this medication 6 and 12 weeks and every 6 months” (23.2% at baseline vs 73.5% at 1 month), and “What is the contraindication of this drug?” (33.0% at baseline vs 85.1% at 1 month). However, the number of respondents answering the question “What is the symptom that you should stop taking and going to the doctor?” correctly was slightly reduced from 139 pre-test (37.6%) to 137 post-test (37.0%) (Table 1).
 |
Table 1 Percentage of Respondents Giving Correct Answers to Atorvastatin Knowledge at Baseline and at 1-Month |
Figure 1 shows the results for atorvastatin knowledge categorized by a passing score at ≥ 8 points. At baseline, the number of atorvastatin users with a passing score was 34 (9.2%), which was significantly less than the 296 respondents (80.0%) who achieved a passing score 1 month after receiving the PIL (p<0.001).
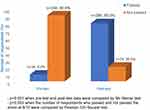 |
Figure 1 Atorvastatin knowledge between pre-test and post-test categorized by a passing score at ≥ 8 points. |
Factors Associated with Atorvastatin Knowledge
At both baseline and for the post-test, the mean score of respondents with bachelor’s degree or higher was significantly higher than other educational levels (p<0.001) and there was no statistical difference between post-test and pre-test scores. Civil servants also had significantly higher mean scores than other careers in the pre-test and post-test (p<0.001) with no significant difference between post-test and pre-test scores.
For the post-test, respondents who were taking less than 3 medications were more likely to have a higher mean score than others (p=0.006). Respondents who had received atorvastatin for more than one year or respondents who used herbal supplements had significantly higher scores (p=0.009, p=0.015 respectively). For both the pre-test and post-test, respondents who read all the content of the PIL were found to have greater mean scores compared to those who read some parts of the PIL (p=0.002 and p=0.001, respectively) (Table 2).
 |
Table 2 Comparison of Factors Affecting Pre-Test, Post-Test and Mean Difference of Atorvastatin Knowledge Score |
Multiple linear regression analysis found that, at baseline, respondents who had educational levels of primary school and high school had lower pre-test scores than those of bachelor’s degree or higher (β= −0.395, p<0.001 and β= −0.175, p=0.002, respectively). Agriculturists had higher pre-test scores than unemployed or students (β=0.142, p=0.031). Respondents who indicated reading all contents of the PILs had a greater pre-test score than those who read only some parts of the PIL (β=0.121, p=0.017). After 1 month of receiving the PIL, civil servants had a greater post-test score than unemployed and students (β=0.280, p<0.001). Likewise, respondents who indicated they read all contents of the PILs (β=0.141, p=0.006) and who had an allergic history (β= −0.101, p=0.042) had higher post-test scores. Respondents who had been taking the medicine for at least one year had a higher mean difference than those who had been taking the medicine less than one year (β=0.130, p=0.012) (Table 3).
 |
Table 3 Adjusted Linear Regression for Atorvastatin Knowledge at Pre-Test, Post-Test, and Change in Knowledge Score |
Benefit Scores and Anxiety Scores After Using the PILs
A visual analog scale (VAS) was used to determine patients’ perceptions of the benefits of PILs and their anxiety after reading the PIL. The mean±sd PIL benefit score was 8.87±1.83 and the anxiety score was 3.69±3.06 (score range=0–10). Patients who read all content of the PIL rated the benefits of the PIL with a higher score than those who read some parts of the PIL (p=0.007). Patients who had more than 5 concomitant medications rated the PIL benefit score significantly lower than those who had less than 3 concomitant drugs (p=0.012). For patients’ anxiety scores about atorvastatin after reading the PIL, females had significantly more anxiety than males (p<0.001). In addition, patients who used herbal medicines were more likely to be anxious than those who had never used them. (p=0.048) (Table 4).
 |
Table 4 Factors Associated with PIL Benefit Scores and Patients’ Anxious Scores (Multiple Linear Regression) |
Discussion
Atorvastatin Knowledge
Our study was conducted to assess patients’ knowledge of atorvastatin after PIL reading. The atorvastatin knowledge score at 1 month after receiving the PIL had a statistically significant increase when compared to the baseline. Several previous studies have reported similar results that reading PILs increased patients’ knowledge.20,25–27 Patients’ knowledge 1-month after receiving the PIL was tested. Patients had been encouraged to open the post-test envelope and they could read while they answered the test. In the pre-test, information about indication, missed-dose management, and how to take the medication was basic knowledge that most patients knew (more than 70%). Patients had perceived their illness and treatment information and these issues were frequently provided by the healthcare professionals.28,29 However, the information about risks of medications and ADRs is not generally provided to patients.30
Only one-third of patients in our study knew about the name of the medicine, serious ADRs, and contraindications. Hence, patients should be informed about these topics. A high number of patients answered incorrectly on the effect of atorvastatin on blood sugar level. This question examined respondents’ willingness to read all of the PIL because this information was only provided in a sub-topic in the PIL. After receiving the PIL, the number of patients who answered correctly significantly increased in all questions, except ADR monitoring and management. The most common and correct response in the pre-test was “fever and pain/sore muscles that is not caused by physical work” while respondents answered, “diarrhea and indigestion” for the post-test. It is possible that the patients were confused about the side effect information on the PIL since a previous study suggested that patients might confuse conflicting information between consultation from physicians, pharmacists, and written medication information, or information overload.31 A few studies found that using different ways of presenting side effect information: natural frequencies, percentages, and positive framing could lead to consumers’ misunderstanding and affect risk appraisal processes.32,33 Therefore, healthcare professionals should focus on this issue before providing the information to patients.
Studies about improved medication knowledge have been conducted with different study designs, types of interventions, and post-intervention periods. Although verbal information is considered as the primary source of medical knowledge,28,29 results of some comparative studies have found that written information combined with verbal information is more effective than verbal information alone in knowledge improvement.20,34 In contrast, other studies have found no difference between combined written and verbal information and written information alone.25 The results from the current study are consistent with a previous study conducted in Thailand that showed knowledge about non-steroidal anti-inflammatory drugs was increased 1-month after receiving PILs. Moreover, other studies have found that this increased knowledge could be sustained at 2–3 month follow-ups.35,36
Factors Related to Atorvastatin Knowledge
Factors related to atorvastatin knowledge score at baseline showed an association of higher education level and higher knowledge score. Occupation was also related to atorvastatin knowledge score. After reading the PIL, education level and occupation maintained their association with the atorvastatin knowledge score and there was no difference between pre-test and post-test scores. Previous studies confirm that the level of education influences patients’ knowledge.37,38 A previous study found that patients with a higher level of education preferred to read PILs.26 After reading the PIL, patients who were taking 3 concomitant drugs or less had a higher mean knowledge score. Patients receiving multiple medications are more likely to be confused about their medications,39 which could lead those patients being unable to remember the details for all of their medications. Surprisingly, patients who had previous experience with allergy had lower post-test scores than those who had not. This finding was not consistent with a previous qualitative study that found previous experiences of allergies and side effects were factors that contributed to consumers reading written drug information.40 The possible reason for the difference in our study was that patients who had experienced allergies might only pay attention to ADRs or allergic issues, rather than all the details contained in the PILs. We found that patient reading behavior was a factor influencing the knowledge score both at baseline and after receiving the PIL, with particularly high knowledge scores in those who read all of the contents of the PIL. Good medication knowledge was also associated with longer duration of medication use. It is possible that patients who had received more than one year of medication treatment were familiar with the details of their medicines provided by their healthcare professionals such as the drug name, how to take, and any possible side effects.
Perceived Benefits of Using the PILs and Patient’s Anxiety About Medications
PILs are useful for educating patients regarding medications.41 Our study showed a high level of positive attitude regarding PIL benefits. A previous study showed 42.3% of respondents stated that the information in the patient package inserts was useful.42 A study in Thailand also found high usefulness scores and low anxiety scores among patients after reading the developed PIL. Higher educational level was found as a significant factor for higher usefulness scores, and type of medicines was associated with lower anxiety score.21 Whilst the current study found that patients who read all sections of the PIL had a better opinion about benefit of the PILs than those who read some sections of the PIL. Our findings show that patients who had polypharmacy (more than 5 concomitant items) gave lower PIL benefit scores. This may be because the provision of more than 5 PILs might overload patients’ and affect their reading behavior, thus they might not be interested in the usefulness of PILs. Our study also found low levels of anxiety in patients after reading PILs so that information about possible risks of medications did not reduce or influence patients’ anxiety about their treatment.43–45
Implication of the Study
As PILs can improve patients’ knowledge on taking medicines accurately, PILs produced by manufacturers should be supported and approved by health authorities before distribution to consumers. User testing, as a method of consumer assessment of PILs, should be used to test for comprehension to ensure that consumers can easily understand the whole PIL. Future research could assess the impact of PILs on patients’ behavior, such as medication adherence and safety awareness about taking medicines.
Limitations of the Study
Our study was conducted in only one university hospital. Thus, we cannot generalize the results to the wider Thai population. The study design did not compare between a control group and intervention group. The effect of the PILs was evaluated in patients 1-month after receiving the PILs, which is similar to previous studies of short-term knowledge assessment.21,46 Thus, the long-term effects of PILs on patients’ knowledge are not known. Patients reading the PIL or accessing additional sources of medicine information while completing the post-test questionnaire could not be controlled. Using a VAS to assess perceptions about the benefits of PILs and medication anxiety has a limitation caused by variation in judgment among individuals, and patients might have experienced some difficulty in finding a point on the line of a VAS that best represented their perception.47
Conclusion
Reading PILs could increase patients’ medicine knowledge. The factors that were associated with this increased knowledge were higher education level, reading the entire PIL, and prior experience of an allergic response. Moreover, longer duration of medication use was an important factor in improving patient’s knowledge. Patients had a good perception about PIL benefits and had less anxiety after reading the PIL. The availability of qualified PILs in Thailand should be promoted by the health authorities and pharmaceutical manufacturers to support the appropriate use of medicines. Moreover, healthcare professionals could provide PILs in counseling practice to ensure that patients understand the information without causing excessive anxiety about taking medicines.
Acknowledgments
We would like to express our thanks to all participants in this study and the staff at Queen Sirikit Heart Center who assisted in data collection. The authors thank Dr. Glenn Borlace for English language assistance through the Khon Kaen University publication clinic.
Funding
This study received financial support from Graduate School, Khon Kaen University (Grant Number 59121110). The funding organization had no role in the design or conducting of the study.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Nair K, Dolovich L, Cassels A, et al. What patients want to know about their medications. Focus group study of patient and clinician perspectives. Can Fam Physician. 2002;48:104–110.
2. Tarn DM, Wenger A, Good JS, Hoffing M, Scherger JE, Wenger NS. Do physicians communicate the adverse effects of medications that older patients want to hear? Drugs Ther Perspect. 2015;31(2):68–76. doi:10.1007/s40267-014-0176-7
3. Fosnocht D, Taylor JR, Caravati EM. Emergency department patient knowledge concerning Acetaminophen (paracetamol) in over-the-counter and prescription analgesics. Emerg Med J. 2008;25(4):213–216. doi:10.1136/emj.2007.053850
4. Cullen G, Kelly E, Murray FE. Patients’ knowledge of adverse reactions to current medications. Br J Clin Pharmacol. 2006;62(2):232–236. doi:10.1111/j.1365-2125.2006.02642.x
5. Yilmaz H, Gürel S, Özdemir O. Turkish patients with osteoarthritis: their awareness of the side effects of NSAIDs. Turkish J Gastroenterol. 2005;16(2):89–92.
6. Jarernsiripornkul N, Phueanpinit P, Pongwecharak J, Krska J. Experiences of and attitudes towards receiving information about non-steroidal anti-inflammatory drugs: a cross-sectional survey of patients in Thailand. Expert Opin Drug Saf. 2016;15(4):417–426. doi:10.1517/14740338.2016.1139571
7. Kandula NR, Malli T, Zei CP, Larsen E, Baker DW. Literacy and retention of information after a multimedia diabetes education program and teach-back. J Health Commun. 2011;16:89–102. doi:10.1080/10810730.2011.604382
8. Alnouri F, Wood D, Kotseva K, Ibrahim MEA. Which statin worked best to achieve lipid level targets in a European registry? A post-hoc analysis of the EUROASPIRE III for coronary heart disease patients. J Saudi Heart Assoc. 2014;26:183–191. doi:10.1016/j.jsha.2014.04.005
9. Liu Y, Cheng Z, Ding L, et al. Atorvastatin-induced acute elevation of hepatic enzymes and the absence of cross-toxicity of pravastatin. Int J Clin Pharmacol Ther. 2010;48(12):798–802. doi:10.5414/cpp48798
10. Collins R, Reith C, Emberson J, et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet. 2016;388(10059):2532–2561. doi:10.1016/S0140-6736(16)31357-5
11. Jones PH, McKenney JM, Karalis DG, Downey J. Comparison of the efficacy and safety of atorvastatin initiated at different starting doses in patients with dyslipidemia. Am Heart J. 2005;149(1):e1. doi:10.1016/j.ahj.2004.07.025
12. Bin Abdulhak AA, Vaughan-Sarrzin M, Kaboli P, et al. Temporal trends of high-intensity statin therapy among veterans treated with percutaneous coronary intervention. J Am Heart Assoc. 2018;7(5):e007370. doi:10.1161/JAHA.117.007370
13. Mann DM, Woodward M, Muntner P, Falzon L, Kronish I. Predictors of nonadherence to statins: a systematic review and meta-analysis. Ann Pharmacother. 2010;44(9):1410–1421. doi:10.1345/aph.1P150
14. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. doi:10.1161/circ.106.25.3143
15. Travis Gossey J, Whitney SN, Crouch MA, Jibaja-Weiss ML, Zhang H, Volk RJ. Promoting knowledge of statins in patients with low health literacy using an audio booklet. Patient Prefer Adherence. 2011;5:397–403. doi:10.2147/PPA.S19995
16. Koo MM, Krass I, Aslani P, Guzmàn WM, Le Duff M. Factors influencing consumer use of written drug information. Ann Pharmacother. 2003;37(2):259–267. doi:10.1177/106002800303700218
17. Grime J, Blenkinsopp A, Raynor DK, Pollock K, Knapp P. The role and value of written information for patients about individual medicines: a systematic review. Heal Expect. 2007;10(3):286–298. doi:10.1111/j.1369-7625.2007.00454.x
18. Gibson Smith K, Booth JL, Stewart D, Pfleger S, McIver L, Maclure K. Supporting shared decision-making and people’s understanding of medicines: an exploration of the acceptability and comprehensibility of patient information. Pharm Pract (Granada). 2017;15(4):1–7. doi:10.18549/PharmPract.2017.04.1082
19. Morrow DG, Weiner M, Young J, Steinley D, Deer M, Murray MD. Improving medication knowledge among older adults with heart failure: a patient-centered approach to instruction design. Gerontologist. 2005;45(4):545–552. doi:10.1093/geront/45.4.545
20. Mai A, Aslani P. Impact of Vietnamese written and verbal medicine information on Vietnamese-speaking Australians’ knowledge and satisfaction. Br J Clin Pharmacol. 2007;64(4):527–535. doi:10.1111/j.1365-2125.2007.02968.x
21. Jarernsiripornkul N, Phueanpinit P, Pongwecharak J, Krska J. Development and evaluation of user-tested Thai patient information leaflets for non-steroidal anti-inflammatory drugs: effect on patients’ knowledge. PLoS One. 2019;14(1):1–15. doi:10.1371/journal.pone.0210395
22. Williams VS, Morlock RJ, Feltner D. Psychometric evaluation of a visual analog scale for the assessment of anxiety. Health Qual Life Outcomes. 2010;8:57. doi:10.1186/1477-7525-8-57
23. Ruel E, Edward Wagner W, Gillespie BJ. Pretesting and pilot testing. In: The Practice of Survey Research: Theory and Applications. SAGE Publications; 2016.
24. Bloom BS. Learning for mastery. instruction and curriculum. regional education laboratory for the Carolinas and Virginia. Eval Comment. 1968;1:1–12.
25. Hill J, Bird H. The development and evaluation of a drug information leaflet for patients with rheumatoid arthritis. Rheumatology. 2003;42(1):66–70. doi:10.1093/rheumatology/keg032
26. Mansoor L, Dowse R. Written medicines information for South African HIV/AIDS patients: does it enhance understanding of co-trimoxazole therapy? Health Educ Res. 2006;22(1):37–48. doi:10.1093/her/cyl039
27. Curtis LM, Mullen RJ, Russell A, et al. An efficacy trial of an electronic health record-based strategy to inform patients on safe medication use: the role of written and spoken communication. Patient Educ Couns. 2016;99(9):1489–1495. doi:10.1016/j.pec.2016.07.004
28. Puspitasari HP, Aslani P, Krass I. Pharmacists’ and consumers’ viewpoints on counselling on prescription medicines in Australian community pharmacies. Int J Pharm Pract. 2010;18(4):202–208. doi:10.1111/j.2042-7174.2010.00041.x
29. Phueanpinit P, Jarernsiripornkul N, Pongwecharak J, Krska J. Hospital pharmacists’ roles and attitudes in providing information on the safety of non-steroidal anti-inflammatory drugs in Thailand. Int J Clin Pharm. 2014;36(6):1205–1212. doi:10.1007/s11096-014-0018-7
30. Schmitt MR, Miller MJ, Harrison DL, et al. Communicating non-steroidal anti-inflammatory drug risks: verbal counseling, written medicine information, and patients’ risk awareness. Patient Educ Couns. 2010;83:391–397. doi:10.1016/j.pec.2010.10.032
31. Vander Stichele RH. Impact of Written Drug Information in Patient Package Inserts: Acceptance and Impact on Benefit/Risk Perception [Thesis for the Degree of Doctor in Medical Sciences]. Gent, Belgium: Ghent University; 2004.
32. Tong V, Raynor DK, Blalock SJ, Aslani P. Exploring consumer opinions on the presentation of side effects information in-Australian Consumer Medicine Information leaflets. Health Expect. 2016;19(3):543–556. doi:10.1111/hex.12215
33. Knapp P, Raynor DK, Berry DC. Comparison of two methods of presenting risk information to patients about the side effects of medicines. Qual Saf Heal Care. 2004;13(3):176–180. doi:10.1136/qshc.2003.009076
34. Savaş S, Evcik D. Do undereducated patients read and understand written education materials? A pilot study in Isparta, Turkey. Scand J Rheumatol. 2001;30(2):99–102. doi:10.1080/03009740151095385
35. Akour A, Bardaweel S, Awwad O, Al-Muhaissen S, Hussein R. Impact of a pharmacist-provided information booklet on knowledge and attitudes towards oral contraception among Jordanian women: an interventional study. Eur J Contracept Reprod Health Care. 2017;22:459–464. doi:10.1080/13625187.2017.1412425
36. Adepu R, Swamy M. Development and evaluation of patient information leaflets (PIL) usefulness. Indian J Pharm Sci. 2012;74:174. doi:10.4103/0250-474X.103857
37. Ndwiga JM, Kikuvi G, Omolo JO. Factors influencing knowledge on completion of treatment among tb patients under directly observed treatment strategy, in selected health facilities in embu county, Kenya. Pan Afr Med J. 2016;25:234. doi:10.11604/pamj.2016.25.234.8761
38. Hanprasertpong T, Rattanaprueksachart R, Janwadee S, et al. Comparison of the effectiveness of different counseling methods before second trimester genetic amniocentesis in Thailand. Prenat Diagn. 2013;33(12):1189–1193. doi:10.1002/pd.4222
39. Pérez-Jover V, Mira JJ, Carratala-Munuera C, et al. Inappropriate use of medication by elderly, polymedicated, or multipathological patients with chronic diseases. Int J Environ Res Public Health. 2018;15(2):310. doi:10.3390/ijerph15020310
40. Koo M, Krass I, Aslani P. Consumer opinions on medicines information and factors affecting its use - an Australian experience. Int J Pharm Pract. 2002;10(2):107–114. doi:10.1111/j.2042-7174.2002.tb00595.x
41. Nicolson D, Knapp P, Raynor DK, Spoor P. Written information about individual medicines for consumers. Cochrane Database Syst Rev. 2009;15(2):CD002104. doi:10.1002/14651858.CD002104.pub3
42. Al-Ramahi R, Zaid AN, Kettana N, Sweileh W, Al-Jabi D. Attitudes of consumers and healthcare professionals towards the patient package inserts-a study in Palestine. Pharm Pract. 2012;10(1):57–63. doi:10.4321/S1886-36552012000100010
43. Oldman M, Moore D, Collins S. Drug patient information leaflets in anaesthesia: effect on anxiety and patient satisfaction. Br J Anaesth. 2004;92(6):854–858. doi:10.1093/bja/aeh162
44. Vinker S, Eliyahu V, Yaphe J. The effect of drug information leaflets on patient behavior. Med Assoc J. 2007;9(5):383–386.
45. Garrud P, Wood M, Stainsby L. Impact of risk information in a patient education leaflet. Patient Educ Couns. 2001;43(3):301–304. doi:10.1016/s0738-3991(00)00168-3
46. Ghimirey A, Sapkota B, Shrestha S, Basnet N, Shankar PR, Sapkota S. Evaluation of pharmacist counseling in improving knowledge, attitude, and practice in chronic kidney disease patients. SAGE Open Med. 2013;1:2050312113516111. doi:10.1177/2050312113516111
47. Klimek L, Bergmann KC, Biedermann T, et al. Visual analogue scales (VAS): measuring instruments for the documentation of symptoms and therapy monitoring in case of allergic rhinitis in everyday health care. Allergo J Int. 2017;26(1):16–24. doi:10.1007/s40629-016-0006-7
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
