Back to Journals » Infection and Drug Resistance » Volume 15
Evaluation of Antibiotics Use and its Predictors at Pediatrics Ward of Jimma Medical Center: Hospital Based Prospective Cross-sectional Study
Authors Garedow AW , Tesfaye GT
Received 18 July 2022
Accepted for publication 20 August 2022
Published 9 September 2022 Volume 2022:15 Pages 5365—5375
DOI https://doi.org/10.2147/IDR.S381999
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Aster Wakjira Garedow,1 Gorfineh Teshome Tesfaye2
1Jimma University, School of Pharmacy, Jimma, Ethiopia; 2Jimma University Medical Center, Jimma, Ethiopia
Correspondence: Aster Wakjira Garedow, Email [email protected]; [email protected]
Background: One of the biggest emerging public health issues is the alarming increase in the prevelance of antibiotic resistance across the globe, which is linked to significant morbidity and mortality and demands special attention. The most significant risk factor for antimicrobial resistance (AMR), which is increasing considerably in Ethiopia and is responsible for increased adverse effects, treatment failure, and rising health-care costs, is inappropriate antibiotic usage. The purpose of this study was to assess the use of antibiotics in inpatient settings at an Ethiopian teaching hospital providing tertiary care.
Methods: The hospital-based prospective cross-sectional study was undertaken at JMC in southwest Ethiopia. Data were collected by using structured checklist which contains patient’s sociodemographic characteristics and pattern of antimicrobial use. All cards of patients which fulfill the inclusion criteria were selected by using a systematic random sampling technique. Bivariate analysis was done to know the association between independent variable and the outcome variable.
Results: The medical records of 402 pediatric patients who had taken at least one systemic antibiotic were examined. The most frequently prescribed combination antibiotics were ampicillin+gentamycin (43.33%) followed by ceftriaxone+gentamycin (15.23%). Gentamycin 116 (24.11%) was the most frequently used antimicrobial. Overall 19.29% of antibiotic use was improper. A higher percentage of participants 149 (22.41%) experienced inappropriate antibiotic usage as a result of inappropriate frequency. Pediatric patients stay in hospital ≥ 7 days (AOR; 2.45, 95%CI: 2.32– 5.34), prescribed antibiotics ≥ 2 3.12 (AOR: 3.12, 95%CI: 6.32– 13.37) and prescribed empirical treatment types (AOR; 2.65, 95%CI: 4.23– 8.87) were independent predictors of inappropriate antibiotics use.
Conclusion: Antibiotics were generally used inappropriately at high rates. Gentamycin and crystalline penicillin were the most prescribed antibiotics. Longer hospital stay, antibiotics prescription ≥ 2, and empirical treatments were the independent predictors of inappropriate antibiotic use.
Keywords: antibiotics, pediatrics, evaluation, Jimma university
Background
Antimicrobials are medications used to treat diseases caused by microbes (bacteria, viruses, fungi, and parasites).1 Antimicrobial resistance (AMR) occurs when microbes change gradually and become unresponsive to the drugs designed to kill them.1,2 AMR is one of the most serious and urgent global public health problems since it affects the health care, veterinary, and agriculture industries.1–3 AMR is associated with high mortality, frequent health-care visits, prolonged hospital stay, and a huge economic burden on health care.3 For instance, each year in the USA, at least 2.8 million people are infected with antimicrobial-resistant microbes and about 35,000 people die as a result with an overall cost of up to $55 billion annually.2,4 The World Bank indicated that AMR would upraise the rate of poverty and disproportionately affect low-income countries compared to the rest of the world.5
The main driver of AMR is the misuse of antimicrobials both in animal and human medicine globally and antimicrobial misuse is disproportionately higher in low and middle-income countries (LMIC).2,6,7 Worldwide up to 50% of antimicrobials used in the hospital were inappropriate.8,18 Similarly, almost half (49%) of antimicrobials used in Ethiopian hospitals were inappropriate.9,20,21 In addition, the pooled prevalence of multidrug resistant (MDR) strains was about 60% and the majority of bacterial isolates have shown significant resistance to commonly used antibiotics in Ethiopia.10 To increase the appropriate prescription and utilization of antimicrobials the Federal Ministry of Health (FMOH)11 and Ethiopian Food and Drug Administration (EFDA)12 have developed and implemented an antimicrobial stewardship (AMS) program which is crucial for treatment success and prevention of AMR on a broader scale. However, this essential program is not fully implemented in most health care institutions.13,14
In order to prevent multiple drug resistance, treatment failure, nonadherence, adverse medication reactions, drug-drug reactions, and a rise in treatment costs, rational antibiotic prescription is crucial, especially for pediatric patients.15–17 There is now ample global evidence that there is continued irrational use of medications in poorer nations. Fewer than 40% of patients in the public sector and fewer than 30% in the private sector are treated in accordance with existing recommendations, and the situation is not improving in either developing or transitional nations.19 The prevalence of infections caused by resistant bacteria has increased, and certain pathogens are now resistant to several different kinds of antibiotics.20–22
One of the primary causes of the high incidence of antimicrobial resistance is thought to be the frequent use of antibiotics. Antimicrobials are used more frequently in infants and children than in adults due to the higher frequency of infection;23 in developed countries, these medications are used to treat about 30% of hospitalized patients.24 The effectiveness of many antibiotics may be lost due to their widespread availability and improper usage by patients and health-care professionals in the treatment of diseases with high prevalence.25 The evaluation of medication use among pediatrics is crucial for clinical, educational, and financial reasons.26,28 There is still a lack of information on the usage patterns of antibiotics in the Jimma Medical Center’s (JMC’s) pediatric wards. This study’s goal is to close these knowledge gaps by identifying the hospital’s pattern of antibiotic use.
Methods and Participants
Study Design and Settings
Hospital-based cross-sectional study was conducted from November 1, 2021 to April 30, 2021 at Jimma Medical Centre (JMC). JMC is the only teaching and referral hospital in the southwest of Ethiopia with a bed capacity of 660 and a catchment population of over 20 million. Jimma Medical Center (JMC) is one of the oldest public hospitals in the country. Geographically, it is located about 350 km southwest of Addis Ababa, the capital. It provides services for approximately 15,000 inpatient, 11,000 emergency cases and 4500 deliveries per year. The overall catchment population for the outpatients reaches 160,000 attendants including the pediatrics and those patients on ambulatory follow-up for chronic diseases, human immunodeficiency virus (HIV) and tuberculosis per year. The hospital gives services both for patients from the community presenting directly to the outpatient department and those referred after attending some other health-care facility or primary hospitals. However, as the hospital is the tertiary teaching hospital in the country, more than 75% of inpatient attendants are referred to hospital from lower-level health institution. JMC pediatric ward has 163 beds and around 3670 children are admitted per year.
Study Population
Pediatric patients (aged ≤18 years) who were treated at the inpatient pediatric ward of JMC department were included in the study. The inclusion criteria were patients who were prescribed with at least one systemic antibiotic for suspected or confirmed infections during the study period. Patients who were prescribed with topical antimicrobial, antifungal, antiviral, anthelmintic and antiprotozoal and antituberculosis were excluded. A total of pediatric 610 patients visited the inpatient clinics of the hospital during the study period; from these 402 patients received systemic antibiotics and were included in the study. Dependent variable was patterns of antibiotic Utilization; independent variables include sociodemographic and clinical characteristics (weight, medical condition, mediations, duration of hospital stay, diagnosis, laboratory parameter). World Health Organization Guideline for Pediatric Illness36 and Ethiopia Standard Treatment Guideline for General Hospitals37 were used to assess the rational use and prescribing pattern of antibiotics. Appropriateness was measured according to a recommendation of use in terms of indication, dose, frequency, and duration. Core drug prescribing indicators such as percentage of generic prescription, injection use, and prescription from the National Essential Drug List were assessed using WHO, Food, Medicine, and Healthcare Administration and Control Authority (FMHACA) standards.33,35
Sample Size Determination and Sampling Technique
The required sample size was calculated using simple population proportion formula by considering P=0.499 (P-of study done in other setting33) and d (sampling error) = 5% and using 95% confidence level, the final sample sizes was 402. All cards of patients which fulfill the inclusion criteria were selected by using systematic random sampling technique until the required sampling size was obtained.
Data Collection Procedure
Pharmacists and general practitioners were trained to collect data following predesigned and pretested data collection formats. Antibiotics which were classified as J01 category (antibiotics for systemic use) under the Anatomical Therapeutic Chemical classification (ATC) classification system were included in this study. Medical record of the patient was used to extract data on the antibiotics’ dosage regimen, age of patients, number of antibiotics prescribed per prescription, duration of antibiotics use, and prescriber’s information, the primary diagnosis and comorbid conditions. Data collection was supervised by the investigators frequently in order to monitor the process and to assist in case of queries.
Data Processing and Analysis
The collected data was checked for completeness and consistency, coded, cleaned compiled, and entered into EpiData 4.6, and exported to the SPSS version 21.0 for analysis. Sociodemogrphic characteristics of patients, clinical characteristics, and treatment-related information were described in terms of frequency and proportions using descriptive statistics. Univariate and multivariate logistic regression analyses were employed to come up with factors associated with inappropriate use of antibiotics. Bivariate analysis was done to know the association between independent variable and the outcome variable. The multivariate logistic regression model was used to identify the independent determinants of appropriateness of antibiotic prescribing after selecting variables that meet crude odds ratio significance value, ie, P <0.25 in bivariate analysis. Finally, based on adjusted odds ratios at 95% confidence interval and P-value <0.05, the variables with significant predictors were identified.
Data Quality Control and Assurance
The questionnaires were prepared in English and translated into Amharic and local language Afan Oromo, and back-translated into English by an independent person to assure its consistency. A pretest was conducted on 8 (5%) study participants by randomly selected patients before the actual data collection to check the consistency and validity of the structured data collection format. Data were compiled, cleared, coded, and checked for consistency. All steps in data collection and recording were closely monitored by the supervisor and any gaps identified were immediately communicated with the data collectors.
Ethical Consideration
The study was conducted in accordance with the principles of the Declaration of Helsinki and the International Council on Harmonization Guidelines for Good Clinical Practice. The Jimma University Institution Review Board (IRB) granted ethical clearance and approval, and the JMC clinical director office was given a letter of authorization. The pediatric unit received a letter from the JUMC clinical director office. By employing identification numbers rather than patient names, confidentiality was guaranteed. A patient’s parent or legal guardian gave their consent.
Operational Definitions and Definitions of Terms
Antibiotics
Are substances produced by microorganisms and used to treat bacterial infections by killing or inhibiting their growth.
Drug Use Evaluation
Is a performance improvement method that focuses on evaluating and improving drug use processes to achieve optimal patient outcomes.
Rational Use of Drugs
Is the process of prescribing right drug for right patient at right time, frequency and for right duration of time as well as correct dispensing and correct use of the drug by the patient.
Empirical Treatment
Is an administration of drugs without an identification of causative agent.
Prophylactic Treatment
Administration of drugs to prevent possible infection before its occurrence.
Neonate
New born especially less than one month of age.
Pediatrics
The branch of medicine concerned with the care and development of children and with the prevention and treatment of children’s diseases.
Antibiotics Utilization
Is using of the antimicrobial for treatment of bacterial infections.
Results
Baseline and Clinical Characteristics of Study Participants
From a total of 6100 pediatric patients visited the pediatric ward of JUM during study period, 402 patients received systemic antibiotics and included to the final analysis. The average antibiotics prescribed per patient was 1.62±0.45. Most 132 (32.83%) of them were in the age range of 1–5 years. Most (72.33%) of patients’ were prescribed with monotherapy antibiotics. Majority 285 (70.89%) of patients stays in hospital for greater than seven days, 288 (71.64%) patients were from rural areas. In more than two thirds of the cases, antibiotic prescriptions were ordered by medical interns (Table 1).
 |
Table 1 Study Participants’ Baseline Characteristics and Other Related Information at the JUMC Pediatric Ward from November 1, 2021 to April 30, 2021 |
Primary Infectious Condition and Comorbidities
From a total of 485 primary infectious conditions for which an antibiotic were prescribed, 162 (33.4%) accounted for meningitis and 137 (28.24%) for lower respiratory tract infection. About 3.3% of study participants used antibiotics for unknown infections (Table 2).
 |
Table 2 Primary Infectious Conditions for which Antibiotics were Prescribed at Pediatric Ward of JUMC from November 1, 2021 to April 30, 2021 (N=485) |
Antibiotics Consumption
Among all pediatrics medical records containing antimicrobials, gentamycin 116 (24.11%), was the most commonly used antimicrobial followed by pencillin G 87 (18.1%), ampicillin 82 (17%), ceftriaxone 73 (15.17%) (Table 3). From the 184 combination antibiotic prescriptions, ampicillin with gentamicin 66 (43.3%) and ceftriaxone with gentamycin 33 (17.93%) was more widely prescribed antibiotics, while ceftriaxone with ampicillin 3 (1.63%) and ceftriaxone with gentamycin with cloxacillin 3 (1.63%) was the least commonly used antibiotics combination in the study area (Table 4).
 |
Table 3 Most Commonly Prescribed Individual Antibiotics at the Pediatric Ward of JUMC from November 1, 2021 to April 30, 2021 (N=481) |
 |
Table 4 Most Commonly Prescribed Combination Antibiotics at the Pediatric Ward of JUMC from November 1, 2021 to April 30, 2021 (N=184) |
Considering the route of drug administration, out of the 665 total number of antimicrobial drugs, the parenteral route contributed the highest, 523 (78.65%) followed by oral (PO) 142 (21.35%) (Table 5). A higher proportion of participants 149 (22.41%) encountered inappropriate use of antibiotics due to inappropriate frequency followed by inappropriate dose 130 (19.55%) and indication 129 (19.4%). The overall inappropriate use of antibiotics was 19.29% (Table 6).
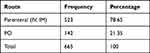 |
Table 5 Route of Drug Administration Among Pediatric Patient of JUMC Pediatric Ward from November 1, 2021 to April 30, 2021 (N=665) |
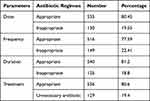 |
Table 6 Appropriateness of Dosage Regimen of Overall Antibiotics Prescribed at the Pediatric Ward of JUMC from November 1, 2021 to April 30, 2021 (N=665) |
Predictors of Inappropriate Use of Antibiotics
In crude analysis using binary logistic regression: duration of hospital stay >7 days, antibiotic treatment duration >7 days, number of antibiotics prescribed ≥2, empirical treatment and prophylactic treatment types were found to predispose a pediatric for inappropriate antibiotic use with statistically significant association. Independent predictors for encountered inappropriate use of antibiotics were identified using multivariate logistic regression, Duration of hospital stay (day) >7 days (AOR; 2.45, 95%CI: 2.32–5.34, P=0.03), antibiotic treatment duration >7 days (AOR; 2.54, 95%CI: 4.34–6.54, P=0.02), number of antibiotics prescribed ≥2 (AOR: 3.12, 95%CI: 6.32–13.37, P=0.01), empirical treatment types (AOR; 2.65, 95%CI: 4.23–8.87, P=0.02) were found to be independent predictors of inappropriate antibiotic use.
According to our finding pediatric patients who stay in hospital >7 days are 2.45 (AOR; 2.45, 95%CI: 2.32–5.34) times at risk for inappropriate antibiotic use than those stay in hospital <7 days, pediatric patients prescribed antibiotics ≥2 are 3.12 (AOR: 3.12, 95%CI: 6.32–13.37) times likely to encounter inappropriate antibiotic use than those with monotherapy. Pediatric patients prescribed empirical treatment types were 2.65 (AOR; 2.65, 95%CI: 4.23–8.87, P=0.02) times likely to encounter inappropriate antibiotic use than those prescribed kinetic/definitive treatment (Table 7).
 |
Table 7 Factors Associated with Inappropriate Use of Antibiotics Using Binary Logistic Regression at the Pediatric Ward of JUMC from November 1, 2021 to April 30, 2021 |
Discussion
Monitoring antibiotic usage is crucial for enhancing the efficacy of antibiotic use. It is crucial in establishing the justification for using antibiotics. The highest incidences of AMR are found in nations with the highest per capita antibiotic use.31 Drug consumption studies have always been helpful in highlighting the issue and the risks of frequently prescription antimicrobial drugs. This problem is prevalent throughout the world. To better understand the connection between the use of antibacterial medications and the emergence of bacterial resistance, numerous groups have urged that antibacterial drug use at the institutional and governmental levels be tracked.32
Antibiotics are strong and effective medicines which are used to treat most different bacterial infections and are among the most commonly prescribed drugs in the pediatric department. According to this study, the average antibiotics prescribed per patient was 1.62±0.45, which is nearly approachable with a study done in Saudi Arabia, which showed 2.12 antibiotics prescribed per patient,27 lower than that reported from Nigeria where antibiotics prescribed per patient were 4.54±1.71,18 but higher than a report from Turkey (1.54).21 This difference might be due to study setting, study design, the sample size, type, and geographical location of the hospital, different infection prevention strategy, and antibiotic use policy between our country and the aforementioned countries.
In our study, the common reasons for antibiotic prescription were, meningitis followed by lower respiratory tract infection, and severe pneumonia which were in line with studies done in northern and North East Ethiopia where the most common diagnosis was pneumonia and severe pneumonia, respectively.6,30 This is in contrast to a study from Saudi Arabia which explored that gastroenteritis was the most common reason for antibiotic prescriptions.27 This discrepancy might be due to the difference in the study design, study area, and time period during which these studies were conducted.
The most frequently prescribed individual antimicrobial agents were gentamycin followed by crystalline pencillin and ampicillin which is similar to a study done in northern Ethiopia.38 This was different from a study done in Indonesia,23 which showed that cefotaxime, amoxicillin, and ampicillin were the most frequently prescribed antibiotics, and a study in India20 indicated that the most frequently prescribed individual antimicrobial drugs were cefotaxim, ceftriaxone, cefpodoxime, cefaclor. This difference might be due to availability of that drug in the facility, the difference in the indications, differences in the types of infections that are prevalent, antibiotics selection based on the sensitivity of the responsible pathogens unlike our case in which most of them were selected empirically.
The most frequently prescribed combined antimicrobials were ampicillin+gentamycin followed by ceftriaxone+gentamycin, which is similar with study done in another part of Ethiopia, which explored that the most commonly prescribed multiple drugs were ampicillin+gentamicin followed by ceftriaxone+gentamicin.29 This was different from Study done in Indonesia which indicated that the most frequently prescribed multiple antimicrobials were ampicillin+chloramphenicol followed by cefotaxime+amikacin and cefotaxime+cotrimoxazole.24 This difference might be due to the availability of drug within study area. The majority of antimicrobials were prescribed by parenteral 523 (78.65%). This was similar with study done in northern Ethiopia which showed most of (71.8%) the drugs were administered through parenteral route.38 This result was higher than WHO standards (13.4–24.1).33 A report from the University of Gondar indicated that the proportion of drugs given by injections was 6.3%.34 The discrepancy could be due to a focus of the study to outpatient pharmacy, while the result of our study represents inpatient pediatric wards.
The overall inappropriate use of antibiotics was 19.29%. A higher proportion of participants 149 (22.41%) encountered inappropriate use of antibiotics due to inappropriate frequency, followed by inappropriate dose 130 (19.55%), and indication 129 (19.4%). This was in line with study done in Nekemte which showed inappropriate dose, frequency, and duration was the commonly observed inappropriate antibiotic use.16 In contrast to this, a study done in Turkey showed that the rate of inappropriate antibiotic use was 33.8%, Unnecessary antibiotic prescription was the most common cause for inappropriate antibiotic use (51.9%), followed by unnecessary multiple antibiotic use (29.6%), inaccurate dosing (11.1%), use of broader spectrum than required (7.4%), and use of antibiotics with narrower spectrum than needed (3.7%).30 This difference might be due to the professional knowledge, skills, integrity to their works, and also unavailability of first-line drugs.
According to our finding pediatric patients stay in hospital >7 days are 2.45 (AOR; 2.45, 95%CI: 2.32–5.34) times at risk for Inappropriate antibiotics use than those stay in hospital <7 days. Pediatric patients prescribed antibiotics ≥2 are 3.12 (AOR: 3.12, 95%CI: 6.32–13.37) times likely to encounter Inappropriate antibiotics use than those with monotherapy. It is in line with earlier findings done in Nigeria.18 This study also revealed that Pediatric patients prescribed empirical treatment types were 2.65 (AOR; 2.65, 95%CI: 4.23–8.87, P=0.02) times likely to encounter inappropriate antibiotics use than those prescribed definitive treatment. This finding was different from study done in North Ethiopia, which showed that advanced age was the independent predictors of inappropriate drug use.
Conclusion
Inappropriateness of antibiotics use was high in our setting. Longer hospital stay, antibiotics prescription ≥2, empirical treatment types was the independent determinant of inappropriate drug use.
Abbreviations
ADRs, adverse drug reactions; AGE, acute gastroenteritis; AMA, antimicrobial agent; EDL, essential drug list; JUMC, Jimma University Medical Center; SPSS, Statistical Packages for Social Sciences.
Data Sharing Statement
Readers who require data and materials of the current study can communicate and get from the corresponding author with a reasonable request.
Acknowledgments
Jimma University is greatly acknowledged for the financial support of the study. The authors are grateful to the study participants for taking their time to provide information. Data collectors are also appreciated for their immense contributions.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was funded by Jimma University Institute of Health. The funding body had no role in the design of the study, data collection, and analysis, interpretation of data and in writing the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World health organization (WHO). Fact sheets, antimicrobial resistance; 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance.
2. CDC. Antibiotic/antimicrobial resistance (AR/AMR); 2020. Available from: https://www.cdc.gov/drugresistance/about.html.
3. Michael CA, Dominey-Howes D, Labbate M. The antimicrobial resistance crisis: causes, consequences, and management. Front Public Heal. 2014;2:1–8. doi:10.3389/fpubh.2014.00145
4. Dadgostar P. Antimicrobial resistance: implications and costs. Infect Drug Resist. 2019;12:3903–3910. doi:10.2147/IDR.S234610
5. Wang W, Arshad MI, Khurshid M, et al. Antibiotic resistance: a rundown of a global crisis. Infect Drug Resist. 2018;11:1645–1658. doi:10.2147/IDR.S173867
6. Klein EY, Van Boeckel TP, Martinez EM, et al. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci U S A. 2018;115(15):E3463–E3470. doi:10.1073/pnas.1717295115
7. Pokharel S, Raut S, Adhikari B. Tackling antimicrobial resistance in low-income and middle-income countries. BMJ Glob Heal. 2019;4(6):4–6. doi:10.1136/bmjgh-2019-002104
8. CDC. Antibiotic Resistance Threats in the United States, 2019. Washington, DC: US Department of Health and Human Services; 2019.
9. Muhie OA. Antibiotic use and resistance pattern in Ethiopia: systematic review and meta-analysis. Int J Microbiol. 2019;2019. doi:10.1155/2019/2489063
10. Tsegaye A, Mulubrahan A, Enkosilassie M, Mengistu H. The burden of antimicrobial resistance at tertiary care hospital, southern Ethiopia: a three years ’ retrospective study. BMC Infect Dis. 2019;1:6–13.
11. Ethiopia. Strategy for the prevention and containment of antimicrobial resistance for Ethiopia. World Health Organization (WHO). https://www.who.int/publications/m/item/ethiopia.
12. Gerba H. Ethiopian food, medicine and healthcare administration and control authority; 2018. Available from: http://www.nifds.go.kr/brd/m_95/down.do?brd_id=board_mfds_411&seq=30934&data_tp=A&file_seq=4.
13. FMHACA. A practical guide to antimicrobial stewardship program in Ethiopian hospitals; 2018. Available from: https://www.ghsupplychain.org/sites/default/files/2019-03.
14. Gebretekle GB, Mariam DH, Abebe W, et al. Opportunities and barriers to implementing antibiotic stewardship in low and middle-income countries: lessons from a mixed-methods study in a tertiary care hospital in Ethiopia. PLoS One. 2018;13(12):1–15. doi:10.1371/journal.pone.0208447
15. Narayan DS, Mangesh MMA. Study of prescription pattern of antibiotics in paediatric in patients at a tertiary care hospital in central India. Int J Pharmacol Res. 2016;6(8):2277–3312.
16. Asefa L, Bayissa G, Abera Z. Antibiotics use evaluation for pediatrics at nekemte referral hospital East Wollega Zone, Oromia Region, West Ethiopia. World J Med Sci. 2016;13(1):17–26.
17. Choudhury DK, Bezbaruah BK. Antibiotic prescriptions pattern in pediatrics in-patient department Gauhati medical college and hospital, Guwahati. J Appl Pharm Sci. 2013;3(8):144–148.
18. Shivaleela J, Revankar S, Vedavathi H, et al. A study of prescription pattern of antibiotics in pediatric in-patients of mc-gann teaching hospital Shivamogga Institute of Medical Sciences (SIMS), Shivamogga, Karnataka. Age. 2014;4(1):32–33.
19. Bonniface M, Nambatya W, Rajab K. An evaluation of antibiotic prescribing practices in a rural refugee settlement district in Uganda. Antibiotics. 2021;10(2):172. doi:10.3390/antibiotics10020172
20. Shamshy K, Mufida Begum I, Perumal P. Drug utilization of antimicrobial drug in pediatrics population in a tertiary care hospital in Erode, Tamilnadu, India. Int J Pharmtech Res. 2011;3(3):1530–1536.
21. Anong DN, Akoachere J-FK. Prescribing patterns and associated factors of antibiotic prescription in primary health care facilities of Kumbo East and Kumbo West Health Districts, North West Cameroon. PLoS One. 2018;13:e0196861.
22. Frieden T. Antibiotic resistance threats in the United States. Centers Dis Control Prev. 2013;12(1):136–141.
23. Amin H, Abdoerrachman H, Akib A. Antibiotic profile in pediatric wards, department of child health, ciptomangunkusumo hospital. PaediatricaIndonesiana. 2014;44:3–4.
24. Nebyu Daniel A, Berhe YH, Kaushik A. Assessment of inpatient antibiotic use in halibet national referral hospital using WHO indicators: a retrospective study. BMC Res Notes. 2018;11:904. doi:10.1186/s13104-018-4000-7
25. Mezgebe HB, Tadesse B, Legesse B. Antibiotics prescribing pattern in pediatric unit of Ayder referral hospital Tigray Region, Northern Ethiopia. J Sci Innov Res. 2015;4(2):57–60. doi:10.31254/jsir.2015.4202
26. Venkateswaramurthy N, Murali R, Sampathkumar R. the study of drug utilization pattern in pediatric patients. Int J Pharm Pharm Sci. 2012;5(3):140–144.
27. Alakhali K, Shaik Mohammad A. Prescribing pattern of antibiotics in pediatric patients in the Jazan Region, Kingdom of Saudi Arabia. RGUHS J Pharm Sci. 2014;4(3):120–124. doi:10.5530/rjps.2014.3.6
28. Chaitanya Kumar T, Pappachan B, John A, et al. study on prescribing pattern and utilization of antibiotics in inpatients of the medicine department of a tertiary care teaching hospital, davangere, Karnataka, Indo. Am J Pharmacol Res. 2015;5:12.
29. Alemnew G, Asared S. assessment of the pattern of antibiotics use in pediatrics ward of dessie referral hospital, north east Ethiopia. Int J Med Medical Sci. 2015;7(11):1–7. doi:10.5897/IJMMS2014.1101
30. Ergül B, Gökçek İ, Çelik T, Altuner Torun Y. Assessment of inappropriate antibiotic use in pediatric patients: point-prevalence study. Turk Pediatri Ars. 2018;53:17–23. doi:10.5152/TurkPediatriArs.2018.5644
31. Patel S, Shah A, Shah R, et al. Evaluation of drug utilization pattern of antimicrobials using ATC/DDD system in intensive care unit of a tertiary-care teaching hospital. Int J Med Sci Public Health. 2016;5(1):2–6. doi:10.5455/ijmsph.2016.08112015189
32. Azizi H, Kabir K, Farrokhi B, et al. Pattern and determinants of antibiotic mal-prescribing among family physicians in the primary health care facilities in Iran; 2019.
33. World Health Organization. How to investigate drug use in health facilities: selected drug use indicators. World Health Organization; 1993, https://apps.who.int/iris/bitstream/handle/10665/60519/WHO_DAP_93.1.pdf.
34. Gebretsadik Z, Gebrehans M, Getnet D, Gebrie D, Alema T, Belay YB. Assessment of drug-drug interaction in ayder comprehensive specialized hospital, Mekelle, Northern Ethiopia: a retrospective study,”. Biomed Res Int. 2017;2017:6. doi:10.1155/2017/9792363
35. World Health Organization. Food, medicine and healthcare administration and control authority of Ethiopia, national essential medicine list fifth edition. https://www.who.int/selection_medicines/country_lists/EML_5th_edition_2015.pdf?ua.
36. World Health Organization. Pocket book of hospital care for children; guidelines for the management of common childhood illness- 2nd ed. https://www.who.int/maternal_child_adolescent/documents/child_hospital_care/en/.
37. Standard treatment guideline for general hospitals in Ethiopia-4th edition. http://www.fmhaca.gov.et/wp-content/uploads/2014/03/STGGeneral-Hospital.pdf.
38. Adane Y, Chernet T, Abere TB, Desalegn GD. Appropriateness and pattern of antibiotic prescription in pediatric patients at Adigart General Hospital, Tigray, Ethiopia. Biomed Res Int. 2021;6640892:7. doi:10.1155/2021/6640892
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
