Back to Journals » Medical Devices: Evidence and Research » Volume 14
Evaluation of Advanced Bimanual Skills in Novices Using the Wrist-Like FlexDex™ Articulating Laparoscopic Needle Holder in 2D and 3D Vision: A Randomised Trial
Authors Motahariasl N, Farzaneh SB, Motahariasl S, Kokotkin I, Sousi S, Zargaran A, Zargaran D, Patel B
Received 13 November 2021
Accepted for publication 13 December 2021
Published 30 December 2021 Volume 2021:14 Pages 469—480
DOI https://doi.org/10.2147/MDER.S344975
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Nima Motahariasl,1 Sayed Borna Farzaneh,1 Sina Motahariasl,2 Ilya Kokotkin,3 Sara Sousi,4,5 Alexander Zargaran,5,6 David Zargaran,7 Bijendra Patel8
1St George’s Hospital NHS Trust, London, SW17 0QT, Greater London, UK; 2Lewisham and Greenwich NHS Trust, London, SE13 6LH, Greater London, UK; 3St George’s University of London, London, SW17 0RE, Greater London, UK; 4Department of Surgery and Cancer, Imperial College London, London, W12 0NN, Greater London, UK; 5King’s College London, London, SE1 1UL, Greater London, UK; 6Chelsea and Westminster Hospital, London, SW10 9NH, Greater London, UK; 7Royal Free Hospital, London, NW3 2QG, Greater London, UK; 8Barts Cancer Institute, Queen Mary University of London, London, EC1M 5PZ, Greater London, UK
Correspondence: Sara Sousi
Department of Surgery and Cancer, Imperial College London, Hammersmith Campus, London, W12 0NN, Greater London, UK
Email [email protected]
Aim: The aim of this study was to evaluate the novice performance of advanced bimanual laparoscopic skills using the articulating FlexDexTM laparoscopic needle holder in two-dimensional (2D) and three-dimensional (3D) visual systems.
Methods: In this prospective randomised trial, novices (n=40) without laparoscopic experience were recruited from a university cohort and randomised into two groups, which used the FlexDexTM and 2D or the FlexDex™ and 3D. Both groups performed 10 repetitions of a validated assessment task. Times taken and error rates were measured, and assessments were made based on completion times, error rates and learning curves.
Results: The intervention group that used FlexDexTM and 3D visual output completed 10 attempts of the standardised laparoscopic task quicker than the control group that used FlexDexTM with standard 2D visual output (268 seconds vs 415 seconds taken for the first three attempts and 176 seconds vs 283 seconds taken for the last three attempts, respectively). Moreover, each attempt was completed faster by the intervention group compared to the control group. The difference in average time for the first three and last three attempts reached statistical significance (P < 0.001).
Conclusion: Combination of 3D visual systems and the FlexDexTM laparoscopic needle holder resulted in superior task performance speed, leading to shorter completion times and quicker learning effect. Although the 3D group demonstrated lower mean error rates, it did not reach statistical significance.
Key Statement: 3D visual systems lead to faster task completion times when combined with an articulating laparoscopic needle holder compared to 2D vision. This effect however is not seen in error rates.
Keywords: laparoscopic skills, advanced bimanual skills, 2D, 3D, FlexDex™
Introduction
Laparoscopic surgery has been regarded as one of the most significant surgical innovations since the invention of anaesthesia due to its advantages over open surgery.1 These benefits include smaller incision site, decreased post-operative pain, shorter hospital stay and quicker return to daily activity.2,3 In recent years, laparoscopy has become increasingly pervasive throughout various surgical specialities for simple and complex operations.4–6
However, there are certain ergonomic limitations associated with laparoscopic surgery and laparoscopic instruments that remain unfavourable and may be potentially limiting its more widespread adoption. Firstly, the two-dimensional (2D) imaging typically used for guidance during laparoscopic operations results in the loss of depth perception and spatial orientation by the surgeons that operate within a three-dimensional environment.5 Another factor is related to limitations of traditional laparoscopic surgical instruments, which have a rigid linear design and movements at the jaws or the tip of the instruments are limited to just opening and closing of jaws or rotation of the instrument tip that could impact the manoeuvrability and ease of use and could contribute to extended operating time or learning curve. The standard laparoscopic needle holder in its linear form lacks any degree of rotation at the tip, thus making the laparoscopic suturing task difficult to learn or execute during laparoscopic operations. These factors are often perceived as unfavourable barriers to quick and effective learning of laparoscopic skills among junior surgeons in training, ultimately adding to the frustration and fatigue during training and prolonging the learning curve. Several solutions have been developed to address both issues. High-definition passive or active polarising 3D imaging systems could be used to restore depth perception and robotic-like articulating laparoscopic equipment for greater manoeuvrability.7 Research into the latest 3D visual systems showed that these provide close to a “natural view” comparable to a Da Vinci® robot. Multiple systematic reviews of randomised control trials have shown evidence that the latest 3D imaging systems combined with laparoscopic surgery may result in shorter operative times and improved survival outcomes.8–14 Sørensen et al found that 3D increased operative speed and reduced the number of errors compared to 2D laparoscopy.15 Moreover, robot-assisted surgery has greatly improved patient outcomes, especially in urology as robotic surgical instruments offer higher degrees of instrument tip movements due to their human-like wrist movements. However, due to high equipment costs of robotic surgery, its widespread implementation is severely limited by financial funding. Various manufacturers have been developing articulating instruments with the introduction of single port laparoscopic surgery; however, this still lacks the manoeuvrability that is offered with the human wrist like movements of the robotic surgical instruments. A novel type of articulating laparoscopic needle holder with wrist-like movements comparable to robotic instruments has been developed to improve manoeuvrability at a fraction of the cost of robotic ones. The FlexDexTM is an example of such novel articulating needle holder that allows wrist-like movement with seven degrees of motion at a significantly lower price compared to robotic surgery.
This instrument could be used as a needle holder or could substitute the traditional Maryland grasper during laparoscopic surgery therefore combining 3D imaging with greater dexterity of the FlexDex™ could deliver a potential substitute to robot-assisted surgery at a fraction of cost. However, no studies have been conducted to compare the effect of 2D and 3D imaging on the laparoscopic task performance while using the FlexDex™. Thus, this study will assess the effect of visual imaging modality utilising the FlexDex™ instrument and assess its bimanual skill usability. Moreover, this is the first study this wrist-like manual articulating instrument would be used as a needle holder and a Maryland grasper for grasping and dissecting in 2D and 3D.
Aims
This study evaluates novice performance of advanced bimanual laparoscopic skills using the articulating FlexDex™ laparoscopic needle holder in 2D versus 3D visual systems.
Materials and Methods
Ethics
Ethical clearance was granted by King’s College London Research Ethics Committee (MRA-21/22-26329).
Recruitment
A convenience sample of medical students was taken. Advertisements were circulated via Surgical Society events. Participants applied to join via a Google Form. There was no financial incentive for participants to join the study.
Randomisation
Participants were randomised to either trial arm using a sealed envelope method.
Inclusion and Exclusion Criteria
To qualify for participation in the trial, strict inclusion and exclusion criteria were applied to reduce bias. The inclusion criteria were as follows: Novices to laparoscopy with no previous laparoscopic training or exposure beyond camera handling, full commitment to the completion of the study, and no uncorrected sight issues. The exclusion criteria included: Laparoscopic experience beyond camera manipulation, lack of commitment, absence during the trial and inability to adapt to 3D vision.
Materials and Equipment
Laparoscopic box trainer by Zhejiang Shendasiao Medical Instruments Co., Ltd was used containing six skin-like access ports for the introduction of laparoscopic instruments. Finlux 42S7080 monitors were used (Display Size: 42 Inch (42”), Display Type: LED Full HD 1080p 3D and 2D monitor). The camera was a Sony camcorder (HDR-TD10 Handycam, (10X Zoom in 2D)) capable of recording both in 2D and 3D. In the 3-dimensional group, participants wore passive polarized Finlux 3D glasses (weight: 21 grams). Articulating laparoscopic grasper was the FlexDexTM laparoscopic needle holder provided by FlexDex Surgical→ and the laparoscopic grasper used was a 3mm laparoscopic grasper (Maryland) by LaproSurge™.
Laparoscopic Task
The assessment was task 1 (Grasping and manipulation) of the LapPass® examination created by the Association of Laparoscopic Surgeons of Great Britain and Ireland (ALSGBI). This is an advanced bimanual skill training task divided into 4 steps of bimanual manipulation of an object (polo or a hollow ring) as described in Appendix 1.
Duration of Training
Individuals were asked to perform 10-repetitions with both time and number of errors being recorded for all 10 tries.
Assessment and Error Measurement
1. Completion times were measured for all 10 repetitions.
2. Learning curve assessment comparing completion time of first 3 and last 3 attempts.
3. Error scores were defined as dropping the rings outside the model surface or losing a ring outside the field of view at any point during the 4 steps of the bimanual manipulation. Each drop outside the model surface or loss outside the field of view was given a score of 1 and the accumulated error score was measured for each of the 10 attempts. No drop or loss of a ring during an attempt was given an error score of 0.
Study Pathway
All individuals were required to attend 2 mandatory sessions, where absence in any of the two would result in exclusion from the study. Session 1 was an introductory lecture about the study, where participants were given a full explanation of the task to be performed alongside watching a video demonstration of the validated assessment task. This validated assessment task was task number 1, “grasping and manipulation” of the LapPass® examination.17 The sequence of actions required to be performed by the participants is detailed in Appendix 1 of the Supplementary Material. It consisted of 4 steps that all needed to be done for 1 completed attempt.
After the first session, individuals were randomised into two groups (study arms) where they would be using one of the following combinations of instrumentation: A) FlexDex™ needle holder and 2-dimensional vision B) FlexDex™ needle holder and 3-dimensional vision.
After successful randomisation of individuals, participants of the same experimental arm were grouped into groups of three and were scheduled to attend the second session, which happened 2 weeks after session 1. During session 2, participants in both groups were given a 45-minute familiarisation period where they were given a set of 6 exercises to perform acquaint themselves with the equipment they would be using. A description of these familiarisation tasks is detailed in Appendix 2 of the Supplementary Material. Furthermore, participants in the FlexDex™ and 3-dimensional vision group partook in a two-minute visual adaptation exercise where they were asked to look at a 3D image for ten seconds and away for ten seconds.
In order to compare the performance of individuals in each group, participants were required to perform 10 repetitions of task 1 (Grasping and manipulation) of the LapPass® examination. Completion times and the number of errors were recorded for all ten attempts. To evaluate any difference in task completion times between the two study arms, an inter-cohort comparison was made between the average times of the first and last three attempts, as well as the individual times of each attempt. Furthermore, a comparison was made between the average total number of errors between the 2 groups.
Familiarisation Period
Participants had a 45-minute time slot dedicated to familiarisation with the FlexDex™ instrument by performing a set of six training exercises designed according to videos provided by FlexDex™ Surgical™ (Appendix 2 of the Supplementary Material). Participants were shown 2-minute videos of the six exercises and were given 5–6 minutes to carry them out ultimately, allowing them to become more acquainted with the FlexDex™. Moreover, participants in the FlexDex™ and 2D groups were required to perform these familiarisation tasks in a 2D environment and the FlexDex™ and 3D group in a 3D environment. Appendix 3 of the Supplementary Material demonstrates the FlexDexTM needle holder as well as images from the experiment environment and the participants utilising the needle holder.
Consent
Participants gave written consent during the recruitment process, before the commencement of the trial.
Consort Diagram
The consort diagram is illustrated in Figure 1.
 |
Figure 1 Consort diagram demonstrating the flow of participants through the trial. |
Data Collection and Statistical Analysis
Score sheets were made using Microsoft® Word version 16.21 for each participant to record completion times and the number of errors per attempt. Moreover, data was collected through spreadsheets using Microsoft® Excel version 16.21. Evaluation of task completion speed between the two groups was through inter-cohort comparison of completion times between the first and last three repetitions. Additionally, the average error throughout all 10 repetitions was used to compare error rates between the two trial arms. This data was analysed for normality of spread, and therefore a Kruskal–Wallis One-Way analysis was performed to assess for any significant differences. Error rates were also analysed for normality of spread using Kolmogorov–Smirnov and Shapiro–Wilk test of data distribution. The Shapiro–Wilk test was used to assess the normality of the variables (Appendix 4 of the Supplementary Material) as the sample size is small (n=20), and the F-test to assess whether two variables had equal variance. Based on the p-values generated by those tests, the Two Sample t-test, the Welch Two Sample t-test, or the Wilcoxon rank-sum test was implemented to compare the differences between the two groups based on the assumptions of each test. This was done both for the errors and completion times. The significance level was set at 0.05 (a = 0.05) for this study. The statistical analysis was carried out using International Business Machines (IBM) SPSS version 25 analytic software and R version 4.0.3.
Results
63 participants were recruited in the trial. After the application of the inclusion and exclusion criteria, 13 participants were removed due to previous experience with laparoscopic training. From the remaining 50 participants, all were invited to attend the first session with a further 10 individuals excluded due to absence from the first session. The final number of participants in the study was 40 individuals, with no further participant exclusion or drop-out for the remaining duration of the trial. The 40 participants were randomised into each arm of the study with 20 allocated to each group; FlexDex™ in 2D (n=20) and FlexDex™ in 3D (n=20). Table 1 illustrates the demographic information of participants in either group.
 |
Table 1 Table Demonstrating Demographic Information of Participants in Both the FlexDex™ and 2D Group and the FlexDex™ and 3D Group |
To demonstrate any pre-eminence of instrumentation, task completion time and accuracy were compared between the study arms. With regards to completion time, an inter-cohort comparison was conducted for the initial 3 attempts and the final 3 attempts. This method was chosen as it revealed an average for completion times at the beginning and towards the end of the assessments, therefore reducing the probability of comparison with single anomalous times. Moreover, using average times at the beginning and at the end would demonstrate differences in the learning curves for each set of instruments and illustrate how readily participants can adapt to them.
Completion Times
Table 2 demonstrates the average completion time per attempt between the 20 participants in each of the cohorts. As shown in Table 3, analysis of results demonstrates an average of 415 seconds for the first 3 attempts and 283 seconds for the last 3 attempts in the FlexDex™ in 2D group. The FlexDex™ in 3D group had an average of 268 seconds for the first 3 attempts and 176 seconds for the last 3 attempts. Furthermore, the P-values from the Wilcoxon rank test in Table 4 indicate that there is a difference in means (P < 0.001). Figure 2 illustrates the average completion time per attempt between FlexDex™ in 2D and FlexDex™ in 3D.
 |
Table 2 Table Demonstrating the Average Time per Attempt Between All Individuals Within the FlexDex™ and 2D Group and the FlexDex™ and 3D Group |
 |
Table 3 Table Demonstrating the Average Time, Standard Deviation, and Range of the First and Final 3 Attempts Between All Individuals Within the FlexDex™ and 2D Group and the FlexDex™ and 3D Group |
 |
Table 4 Table Demonstrating the Average Completion Time in Seconds and the Standard Deviation per Attempt Between All Individuals Within the FlexDex™ and 2D Group and the FlexDex™ and 3D Group |
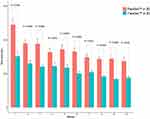 |
Figure 2 Bar plot of the average completion time (in seconds) in all 10 attempts of the assessment task in participants allocated to the FlexDex™ in 3D and FlexDex™ in 2D groups. The standard deviation is also indicated on the plot, in addition to the p-value of the Wilcoxon signed rank test (the exact p-values may be seen in Table 4). |
Error Rates
Review of data regarding error rates demonstrates an average error rate of 7.3 errors between all participants throughout all 10 attempts in the FlexDex™ and 3D group (Table 5). Moreover, analysis demonstrated an average of 9.3 errors between all participants throughout all 10 attempts in the FlexDex™ and 2D group (Table 5). Figure 3 demonstrates the average overall error rate in each of the two groups, and the results of the Two Sample t-test are presented on the plot. The Two Sample t-test was chosen as the data is normally distributed (Shapiro–Wilk P > 0.05, Table 6) and of equal variance (F-test: F = 1.65, df = 19, P = 0.2811, 95% CI: (0.66, 4.18), ratio of variance: 1.65).
 |
Table 5 Table Demonstrating the Average Error Rate per Attempt Between All Individuals Within the FlexDexTM and 2D Group and the FlexDexTM and 3D Group |
Learning Curve Assessment
Inter-cohort comparison of the first three attempts revealed statistically significant (Wilcoxon Rank Sum test p < 0.001) quicker completion time in the FlexDexTM in 3D group with a mean difference of 147.1 seconds (Table 7). Analysis of the final three attempts also demonstrated statistically significant (Welch Two sample t-test p < 0.001) shorter completion times in favour of the FlexDex™ in 3D combination with a mean difference of 107.5 seconds (Table 7). Figures 4, and 5, demonstrate the boxplots of attempts 1, 2, 3 and attempts 8, 9, 10, respectively, between FlexDex™ in 2D and FlexDex™ in 3D. The statistics of the tests are displayed on the plot. Both results have reached statistical significance (p < 0.001), indicating that there is a difference between the means of completion times between the groups.
 |
Table 6 This Table Demonstrates the Difference Between FlexDex™ in 2D and FlexDex™ in 3D in Terms of Average Error Rate Over Their 10 Attempts of the Standardised Assessment Task |
 |
Table 7 This Table Demonstrates the Difference Between FlexDex™ in 2D and FlexDex™ in 3D in the First 3 Attempts and Last 3 Attempts |
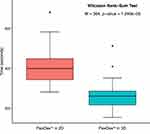 |
Figure 4 Box plot of total average completion times in attempts 1, 2, 3 between the FlexDex™ in 3D and FlexDex™ in 2D groups. The Wilcoxon Rank-Sum test results are displayed on the plot. |
 |
Figure 5 Box plot of total average completion times in attempts 8, 9, 10 between the FlexDex™ in 3D and FlexDex™ in 2D groups. The Welch Two Sample t-test results are displayed on the plot. |
Discussion
This study is the first to explore the effect of 3D vision on task performance speed and accuracy utilising the wrist-like articulating laparoscopic instrument FlexDex™ by surgical novices. Previously conducted studies aimed at assessing the performance of FlexDex™ demonstrated that this mechanical instrument may have an advantage over non-articulating laparoscopic needle holder in terms of manoeuvrability and performance speed. However, no study has been conducted evaluating possible effects of 3D vision on accuracy and speed while performing laparoscopic tasks with FlexDex™.
Completion Times
The results of this study suggest that 3D visual output may have a positive effect on reducing the time taken to complete a standardised task. This was expected as available literature evidence indicates that 3D tends to increase the speed of task completion.9,16 Shorter completion times in this study could be explained by improved depth perception and spatial awareness offered by this visual technology.12 Considering that articulation of FlexDex™ tries to imitate natural wrist movements, integration of the 3D video equipment that restores natural depth perception may facilitate user’s spatial orientation and offer visual and motion similarity of open surgery. As there were statistically significant differences in completion times in both the first and final 3 attempts, this illustrates the continuously added benefit of 3-dimensional visualisation in terms of task completion times. However, there is no previously published evidence comparing articulating mechanical laparoscopic instruments combined with 2D and 3D visual systems, therefore the results of this study were critically appraised according to previous studies on non-articulating instruments and 3D. A prospective randomised control trial carried out by Bhayani et al on performance effects of 3D in 24 novices utilising non- articulating instruments demonstrated quicker operating times. However, the difference in performance precision between the intervention and the control groups did not reach statistical significance. This can be attributed to the inherent difficulties of 3-dimensional visualisation such as blurred vision, double vision, nausea, and eye fatigue.
Error Rates
This study did not find a statistically significant difference in the number of errors that occurred during task attempts between the intervention group and the control group. Given that participants in both trial arms were recruited from the same cohort of novice medical students, the only variable between these two groups was the type of video visualisation (2D versus 3D). This was an unexpected result, as multiple previously published randomised control trials demonstrated reduced error rates in the groups utilising 3D imaging equipment to perform laparoscopic tasks.15 Negative features of the 3D that affect its users such as fatigue and headache could be one of the reasons explaining no statistically significant difference in the error rates between the intervention and the control groups. Novices who are not accustomed to 3D video output could be overwhelmed, particularly at the end of their trials, with visual exhaustion, thus more prone to mistakes. Another explanation could be that the assessment itself might not have elicited the full effect of the 3D on the performance accuracy. The laparoscopic tasks used in this study may have been chosen incorrectly for the objective of assessing the difference in performance accuracy when used with 2D and 3D.
This may warrant further research into the extent of the effect of restored depth perception on the performance accuracy in novel surgeons whilst operating articulating mechanical laparoscopic instruments. A systematic review by Sørensen et al of 19 randomised control trials showed that only 12 of them (63%) showed a statistically significant reduction in the error rates. Furthermore, studies included in the review emphasised multiple side effects of the 3D imaging, such as increased fatigue, headache, and longer adaptation period as possible causes for this result.7
Learning Curve Assessment
Overall, subsequent attempts resulted in reduced completion times in both intervention and study groups. However, the results indicate that the participants in the 2D group had a faster learning curve compared to the 3D group (line gradient 13.2 versus 9.2 respectively). In the 2D group, the difference in completion times between the first and last three attempts is 132 seconds, compared to 92 seconds in the 3D group. This may indicate that although the participants in the control group had a more drastic difference in the performance times between the first and the last attempts, thus quicker learning curve, the participants in the FlexDex™ and 3D group were faster throughout all 10 attempts compared to the 2D group. One of the possible explanations could be that the introduction of the 3D video output could help overcome certain learning barriers such as lack of depth perception, thus allowing for faster performance times from the first attempts.
Limitations
There are several potential limitations to this study. Firstly, FlexDex™ is a suturing device that for the purpose of this study was being used as a grasper. Furthermore, the participants were medical students with no prior experience or knowledge of laparoscopic surgery. Considering this novel articulating device has been designed to be used by experienced surgeons, medical students may not have been an appropriate cohort to recruit from for this study. Furthermore, the advantages of the 3D video output compared to 2D could have had a more drastic effect on laparoscopic task performance among participants consisting solely of experienced surgeons. Another limitation of the study is the grip of FlexDex™. This is a novel tool with a unique manoeuvring mechanism unlike any other laparoscopic instrument in the world. Users who will be holding the FlexDex™ in one hand and a standard laparoscopic tool in the other might find this discrepancy in tool handling physically and mentally demanding. Moreover, due to the complexity of the wrist-like movement mechanism, the FlexDex™ handle and interface was reported to be non-user-friendly, and the majority of participants complained of arm ache and finger fatigue. Moreover, no power calculations were performed to set the minimum number of participants required for each trial arm; hence the sample size of the study may be another limitation for providing valid results. Finally, due to the lack of any validated training program for FlexDex™ instrument, a training routine had to be developed by the authors of this study, which may constitute another limitation of this study.
Conclusion
The FlexDex™ laparoscopic needle driver is an FDA-approved surgical device that allows the surgeon to perform laparoscopic surgery with the same seven degrees of motion afforded by a robotic arm. The results of this study represent the first- ever assessment of task performance speed and accuracy of a novel laparoscopic needle holder FlexDex™ in combination with the 3D visual imaging as well as comparing to the commonly utilised 2D imaging. This study showed that the introduction of the 3D vision led to reduced time taken to complete laparoscopic tasks compared to 2D. The results of this study are in line with some of the previously published evidence. Additional randomised controlled trials will be necessary to assess the generalisability of these initial results.
Further Research
In order to consolidate the findings of this study, further trials with higher participant numbers would be required to compare the differences between 2D and 3D vision on the use of articulating laparoscopic instruments. Furthermore, robotic equipment such as the Da Vinci surgical system™ by Intuitive Surgical Inc has allowed for the production of fully articulating instruments mimicking movements that of the human hand.18 Such tools are very intuitive and have improved ergonomic designs with great dexterity and improved visualisation. However, a major limitation impeding their widespread use is their cost and financial burden on health care organisations.19 Henceforth, it would be valuable to compare the FlexDex™ in 3D against the Da Vinci robot™ to see if there is any significant difference in terms of task completion speeds, error rates and user satisfaction and to evaluate for the cost- effectiveness and possibility of the widespread incorporation of these devices in medical institutes.
Acknowledgments
We gratefully thank Dr Alpa Jekishandas Morawala for her kind help with the methodology and review of this article.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Subido EDC, Pacis DMM, Bugtai NT. Recent technological advancements in laparoscopic surgical instruments. Bali, Indonesia; 2018:040007.
2. Casarin J, Multinu F, Ubl D, et al. Adoption of minimally invasive surgery and decrease in surgical morbidity for endometrial cancer treatment in the United States. Obstet Gynecol. 2018;131(2):304–311. doi:10.1097/AOG.0000000000002428
3. Mason M, Tran Cao H, Awad S, Farjah F, Chang G, Massarweh N. Hospital minimally invasive surgery utilization for gastrointestinal cancer. Ann Surg. 2018;268(2):303–310. doi:10.1097/SLA.0000000000002302
4. Davis C, Shirkey B, Moore L, et al. Trends in laparoscopic colorectal surgery over time from 2005–2014 using the NSQIP database. J Surg Res. 2018;223:16–21. doi:10.1016/j.jss.2017.09.046
5. Athanasiou C, Lockwood S, Markides G. Systematic review and meta-analysis of laparoscopic versus open appendicectomy in adults with complicated appendicitis: an update of the literature. World J Surg. 2017;41(12):3083–3099. doi:10.1007/s00268-017-4123-3
6. Izquierdo L, Peri L, García-Cruz E, et al. 3D advances in laparoscopic vision. Eur Urol Rev. 2012;7:137–139.
7. Jaschinski T, Mosch C, Eikermann M, Neugebauer E, Sauerland S. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2018;2018(11). doi:10.1002/14651858.CD001546.pub4
8. Pantalos G, Patsouras D, Spartalis E, Dimitroulis D, Tsourouflis G, Nikiteas N. Three- dimensional versus two-dimensional laparoscopic surgery for colorectal cancer: systematic review and meta-analysis. In Vivo. 2019;34(1):11–21. doi:10.21873/invivo.11740
9. Cicione A, Autorino R, Breda A, et al. Three-dimensional vs standard laparoscopy: comparative assessment using a validated program for laparoscopic urologic skills. Urology. 2013;82(6):1444–1450. doi:10.1016/j.urology.2013.07.047
10. Cicione A, Autorino R, Laguna MP, et al. Three-dimensional technology facilitates surgical performance of novice laparoscopy surgeons: a quantitative assessment on a porcine kidney model. Urology. 2015;85(6):1252–1256. doi:10.1016/j.urology.2015.03.009
11. He B, Mou L, De Roo R, Musk GC, Hamdorf JM. Evaluation of three-dimensional versus conventional laparoscopy for kidney transplant procedures in a human cadaveric model. Exp Clin Transplant. 2017;15(5):497–503. doi:10.6002/ect.2016.0177
12. Leon P, Rivellini R, Giudici F, Sciuto A, Pirozzi F, Cor-cione F. 3D vision provides shorter operative time and more accurate intraoperative surgical performance in laparoscopic hiatal hernia repair compared with 2D vision. Surg Innov. 2017;24(2):155–161. doi:10.1177/1553350616687434
13. Komaei I, Navarra G, Curro G. Three-dimensional versus two-dimensional laparoscopic cholecystectomy: a systematic review. J Laparoendosc Adv Surg Tech A. 2017;27(8):790–794. doi:10.1089/lap.2017.0155
14. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols(PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi:10.1186/2046-4053-4-1
15. Sørensen S, Savran M, Konge L, Bjerrum F. Three-dimensional versus two-dimensional vision in laparoscopy: a systematic review. Surg Endosc. 2015;30(1):11–23. doi:10.1007/s00464-015-4189-7
16. Storz P, Buess GF, Kunert W, Kirschniak A. 3D HD versus 2D HD: surgical task efficiency in standardised phantom tasks. Surg Endosc. 2012;26(5):1454–1460. doi:10.1007/s00464-011-2055-9
17. LapPass ® [Internet]. ALSGBI; [cited May 25, 2019]. Available from: https://www.alsgbi.org/lappass/.
18. Anderson PL, Lathrop RA, Webster III RJ. Robot-like dexterity without computers and motors: a review of hand-held laparoscopic instruments with wrist-like tip articulation. Expert Rev Med Devices. 2016;13(7):661–672. doi:10.1586/17434440.2016.1146585
19. Kã¶ckerling F. Robotic vs. standard laparoscopic technique–What is better? Front Surg. 2014;1:15. doi:10.3389/fsurg.2014.00015
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

