Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Evaluating the Relationship of Airflow Obstruction in COPD with Severity of OSA Among Patients with Overlap Syndrome
Authors Stewart NH , Brittan M, McElligott M, Summers MO, Samson K, Press VG
Received 15 January 2022
Accepted for publication 4 July 2022
Published 14 July 2022 Volume 2022:17 Pages 1613—1621
DOI https://doi.org/10.2147/COPD.S355897
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Richard Russell
Nancy H Stewart,1 Mollie Brittan,2 Maureen McElligott,2 Michael O Summers,2 Kaeli Samson,3 Valerie G Press4
1Department of Medicine, University of Kansas Medical Center, Kansas City, KS, USA; 2Department of Medicine, University of Nebraska Medical Center, Omaha, NE, USA; 3Department of Biostatistics, University of Nebraska Medical Center, Omaha, NE, USA; 4Department of Medicine, University of Chicago Medical Center, Chicago, IL, USA
Correspondence: Nancy H Stewart, Department of Medicine, University of Kansas Medical Center, 3901 Rainbow Blvd, Kansas City, KS, 66160, USA, Email [email protected]
Background: Chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea (OSA) are common diseases affecting millions worldwide. These two diseases have a complex relationship that is not well understood. Previous small studies suggest an inverse relationship of disease severity of OSA with COPD airflow obstruction.
Objective: The aim of this study was to determine if a relationship exists between severity of airflow obstruction in COPD and severity of OSA via apnea hypopnea index obtained during an in-lab baseline polysomnogram using a large quaternary care center cohort.
Methods: From November 2015 through December 2018, 273 patients with confirmed COPD via spirometry and OSA via in-lab baseline polysomnogram were included.
Conclusion: No associations were noted between severity of airflow obstruction in COPD and disease severity of OSA. Given the heterogeneity of these diseases, further exploration of a relationship within disease subtypes is warranted.
Keywords: airflow obstruction, chronic obstructive pulmonary disease, obstructive sleep apnea
Introduction
Chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea (OSA) are among the most common respiratory disorders worldwide, affecting over 16 million and 28 million US adults, respectively.1–4 The presence of COPD and OSA in the same patient is coined COPD/OSA Overlap Syndrome. The basic understanding of an interaction between these two diseases results from the Sleep Heart Health Study. This study demonstrated persons with both disorders have greater nocturnal oxygen desaturations than those with either disorder alone when utilizing a cohort of patients with mild COPD, as defined by spirometry.5 Patients with both COPD and OSA are at higher risk for hospital admissions and readmissions, and have higher mortality than patients with COPD or OSA alone.6,7 Longitudinal studies of patients with COPD/OSA overlap demonstrate a higher likelihood of recurrent exacerbations and hospitalizations in those patients non-compliant with continuous positive airway pressure therapy.6,7 Characterizing the overall association between COPD and OSA is challenging and studies provide conflicting results.1
In a small sample of the general population, frequency of COPD in patient with OSA was equal to that in the general population, with comorbid COPD and OSA demonstrating a more severe course.8 A large community study utilizing home sleep apnea testing (HSAT) data noted an incremental influence of lung function (by spirometry) on all-cause mortality was less with increasing sleep disordered breathing severity.9 Findings have also varied based on the COPD airflow obstruction severity, by spirometry. In an analysis of the Sleep Heart Health Study patients, those with mild COPD, defined by spirometry of forced expiratory volume in 1 second over forced vital capacity less than 70% (FEV1/FVC <70%) had minimally altered sleep and no association with OSA.5 Sleep disordered breathing was noted to be highly prevalent (65.9% of study participants) in patients with moderate to severe COPD in another small sample.10 A small sample of only veterans with COPD considered present by spirometry and OSA by polysomnography (PSG), no direct relation between COPD and OSA was noted.11
The impact these two diseases have on patients can be profound. Patients with COPD/OSA overlap syndrome are at risk for nocturnal desaturations and complications (pulmonary hypertension, right-sided heart failure, heart rhythm abnormalities, carbon dioxide retention, and death).12–14 Patients with COPD have twice the odds of screening positive for OSA.15 Co-existing cardiovascular conditions are commonly present in overlap syndrome, and are the leading cause of death in these patients.12 Previous research suggests the prevalence of OSA increases with COPD airflow obstruction severity.5,11 All previous studies of the relationship of COPD and OSA have utilized homogenous populations, eg, mild COPD, veterans, or HSAT. A large heterogenous population has yet to be utilized to explore this relationship. The aim of this study was to evaluate the relationship between airflow obstruction severity of COPD based on Global Initiative for Obstructive Lung Disease (GOLD) classification for COPD of FEV1/FVC <70% and forced expiratory volume in 1 second (FEV1) and disease severity of OSA based on apnea hypopnea index (AHI) in a heterogenous population at a quaternary-level academic medical center.
Methods
Study Design and Data Collection
An observational retrospective chart analysis of adult patients receiving baseline PSG from December 2015 through November 2018 was performed. Patients were identified to have both COPD and OSA with International classification of disease (ICD) 10 codes. Asthma patients were not included in this study unless they had a concurrent diagnosis of COPD, nor inhaler regimen of COPD. We considered COPD to be present with spirometry demonstrating an FEV1/FVC <70%, and severity of COPD based on FEV1% predicted. We did not utilize post-bronchodilator data, only pre-bronchodilator data, as recommended for gold standard diagnosis of COPD. Patients were included in the study if they had a baseline in-lab PSG with apnea-hypopnea index (AHI) ≥5 and spirometry performed within the same calendar year, confirmed by chart review. Only in-lab polysomnography was utilized in this study given it is the gold standard for diagnosis of OSA and is recommended for diagnosis of OSA in patients with COPD. If multiple spirometry tests existed within the calendar year of the baseline PSG used in our study, the spirometry performed closest in date to the baseline PSG was utilized for this study.
Baseline demographics, health status, comorbid health conditions, and health-care system utilization were also collected. COPD severity was classified using GOLD classification: very severe COPD defined as FEV1<30%, severe COPD 50%> FEV1≥ 30%, moderate COPD 80%> FEV1≥ 50%, and mild COPD FEV1≥ 80%. Patients with (FEV1/FVC) ratio of less than <70%, yet FEV1>100 were defined as variant. Sleep medicine clinic notes written during the study dates of interest and documented in the electronic medical record were reviewed to determine continuous positive airway pressure (CPAP) compliance. Patients were noted to meet CPAP compliance if CPAP was worn for greater than 70% of nights and greater than 4 hours each night, as noted on CPAP download documented in the electronic medical record patient chart. Severity of OSA was determined based on American Academy of Sleep Medicine guidelines with severe OSA corresponding with an apnea-hypopnea index (AHI) ≥ 30, Moderate OSA demonstrated by 15≤ AHI <30, and Mild OSA determined by 5 ≤ AHI < 15. The number of hospitalizations, emergency department visits, and clinic visits with pulmonology or sleep medicine within the same calendar year were collected.
Charts were reviewed by three reviewers (M.B., M.E., and N.S.) and adjudicated (by N.S). Informed consent for research from study participants was obtained through health-care system interaction. Guidelines outlined through Declaration of Helsinki were followed. This study was reviewed and approved by the University of Nebraska Medical Center Institutional Review Board, Omaha, Nebraska, USA.
Data Analysis
Descriptive statistics were used to describe patient-level characteristics. Due to positive skew of the data, AHI was log transformed. Due logs transform of AHI, Pearson correlation was used to assess for an association between FEV1 severity and log AHI. Linear regression was used to assess the association between FEV1 and log AHI, while adjusting for relevant variables: sex, age, race, BMI, coronary artery disease (CAD), congestive heart failure (CHF), and atrial fibrillation (A fib). Separate logistic regressions were used to assess associations between FEV1 or log AHI and the outcomes of at least one readmission within one year of sleep study (versus none), at least one emergency department visit (versus none), and PAP compliance as documented in the electronic medical record (yes versus no), while adjusting for sex, age, race, and BMI. All analyses were performed using SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Between December 2015 and November 2018, 316 patients underwent PSG and were identified with ICD codes to have concomitant COPD with FEV1/FVC ≤70%. Of the patients identified with concomitant COPD and OSA, 273 patients had FEV1/FVC compatible with COPD. Many patients were female (n = 157, 58%), Caucasian (n = 215, 79.0%), with a mean age of 65.2 years (SD: 10.7) (Table 1). Within a year after their sleep study, over a third of patients had at least one hospitalization (n = 105, 38.5%), and over half had at least one emergency department visit (n = 139, 50.9%).
 |
Table 1 Sample Demographics and Clinical Characteristics |
Over half had moderate COPD (n = 138, 50.6%), while one-fifth had mild or severe COPD (n = 55, 20.2%; n = 47, 17.2%, respectively (Table 2)). Few had either very severe COPD (n = 7, 2.6%) or an FEV1 > 100 (n = 26, 9.5%). OSA severity was nearly represented equally across all three severity groups: mild (n = 96, 35.2%), moderate (n = 74, 27.1%), and severe (n = 103, 37.7%) (Table 2).
 |
Table 2 COPD Degree of Airflow Obstruction (Severity) and OSA Severity |
No significant correlation between severities of COPD (ie, FEV1) and OSA (ie, log of AHI) (r = −0.04, p = 0.51) was noted; this corresponds to a non-significant decrease of 0.002 (95% CI: −0.006, 0.003) in log AHI for every one unit increase in FEV1 (unadjusted model). This is lack of relationship between FEV1 and log AHI in the unadjusted model is seen in Figure 1. Even after adjusting for potential confounders age, sex, race, BMI, CAD, CHF, and atrial fibrillation, the association between FEV1 and log AHI remained not statistically significant (model adjusted coefficient for FEV1 where log AHI is the outcome: 0.000, 95% CI: −0.004, 0.005, p = 0.84), which indicates an estimated change of 0.000 in log AHI for every one unit increase in FEV1, see Table 3. CPAP compliance with compliance as a binary variable was assessed. Fewer than half of patients were on continuous oxygen, while oxygen burden via oxygen disturbance index was not reported.
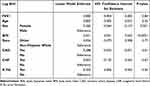 |
Table 3 Regression Model |
 |
Figure 1 Unadjusted model with log AHI as outcome. |
Discussion
In this study, we sought to evaluate the relationship of airflow obstruction seen in COPD and severity of OSA using via AHI in patients who have both documented COPD airflow obstruction on PFTs and documented OSA on in-lab polysomnography in the largest heterogenous cohort published to date. In addition, we utilized a heterogenous cohort of patients from a quaternary care academic medical center who had both documented OSA via baseline in-lab polysomnography and COPD with airflow obstruction via spirometry. Although our sample was heterogenous across airflow obstruction severities, over two-thirds of patients had mild or moderate obstruction, which is unusual in most large samples of patients with COPD, which trend towards moderate to severe. The prevalence of COPD and OSA was higher in women than in men in our cohort, which could be due to regional gender differences. We did not find a significant relationship between severity of airflow obstruction in COPD and severity of obstructive sleep apnea. Since fewer than half of patients were on continuous oxygen, it is challenging to make associations regarding oxygen burden. In addition, oxygen disturbance index was not available nor reported. Moreover, our cohort had an increased prevalence of HTN, however fewer than half had diabetes, coronary heart disease, congestive heart failure, or chronic kidney disease, all of which are unusual in a cohort of patients with comorbid COPD/OSA.
These findings increase the questions surrounding the comorbid relationship between COPD and OSA. Although previous work evaluating whether a relationship exists between the severity of airflow obstruction in COPD and apnea hypopnea index has suggested an inverse relationship, our study is in opposition to this, warranting further research in this area. Given the heterogeneity of COPD across subtypes as well as the heterogeneity across obstructive sleep apnea subtypes, it may prove challenging to collectively address this question utilizing small homogenous cohorts. Within small homogenous cohorts’ conclusions such as an inverse relationship with disease severity may be plausible. For instance, within COPD there are several different subtypes (eg, emphysematous, bronchitic, combined pulmonary fibrosis and emphysema), with varying management options and these phenotypes may ultimately behave differently when it comes to airflow obstruction seen in patients with OSA. In addition, Krachman et al demonstrated amongst 51 smokers with moderately severe COPD (average FEV1 58% predicted) that an increase in emphysema by chest tomography correlated with a decrease in AHI on polysomnography.16
This lack of association found between severity of OSA and severity of airflow obstruction in COPD stands in opposition to the previously proposed positive association of these disease severities.9–11 Small studies evaluating airway collapsibility during sleep in patients with COPD suggest these patients have a less collapsible airway and increased expiratory time, increasing the risk of dynamic hyperinflation,17 however in this study, severity of airflow obstruction is averaged across participants. The large cohort utilized in this study also varies from typical cohort studies in COPD which generally are male prevalence predominate.
The question of the directionality and degree of relationship between severity of airflow obstruction in COPD and severity of obstructive sleep apnea remains. This uncertainty regarding directionality of the relationship of severity does not change current practice, however, should influence future research in this area, and whether certain phenotypes of COPD and OSA patients could have a directional relationship. Clinically, hospitalized patients with COPD are at twice the risk of screening positive for OSA.15 Early detection and treatment of OSA in hospitalized COPD patients can decrease hospital readmissions.18 Furthermore, increased severity of COPD with undiagnosed OSA has demonstrated increased odds for hospital readmission.19 The implications of our findings of a lack of association with disease severity warrant further exploration due to the potential impact this would have on overlap syndrome disease screening, treatment, and health system management.
While it is known that comorbid COPD/OSA overlap disease leads to increased morbidity, mortality, and health-care use, we did not directly evaluate co-morbid COPD/OSA since the aim of our study was to evaluate the severity of airflow obstruction and severity of OSA on each other. Many of the patients in this study had mild or moderate COPD, which may have influenced the lack of association with OSA severity. In addition, the use of ICD codes to screen for eligibility is imperfect as administrative data commonly under and over-diagnose,20,21 however we utilized ICD for screening only, and confirmed with spirometry and polysomnogram. We used broad definitions of COPD without delineating subtypes (eg, emphysematous versus chronic bronchitic).22,23 Subtypes of OSA also exist, such as the “excessively sleepy” subtype, and those with co-morbid insomnia, however these subtypes were outside the scope of this study. Fewer than half of patients were on continuous oxygen, while oxygen burden via oxygen disturbance index was not reported, nor was oxygen burden assessed otherwise. In addition, slightly more than half of patients in our population were compliant with CPAP, which could potentially impact the results.24,25 A significant number of patients in this cohort had heart failure (32%), atrial fibrillation (22%), or coronary artery disease (33%), which are strongly associated with sleep disordered breathing, and could be viewed as limiting generalizability, however, adds to the understanding of the association of heart disease and sleep apnea.
While this is the largest study to date exploring the association of airflow obstruction in COPD and severity of OSA in a heterogenous population, the heterogeneity across these two disease spectrums may make associations difficult.
It is possible amongst subtypes of COPD and severity of COPD there is an association with OSA. Likewise, there is no disputing patients with COPD/OSA overlap are at an increased risk for morbidity and mortality, however the underlying causal mechanism and subtype analyses are lacking in this area. Heterogeneity of OSA management can depend on apnea-hypopnea severity, increased sleep fragmentation, or presence of comorbid insomnia, and management of each can vary.
Future evaluation of the degree of heterogeneity within COPD as it relates to OSA is recommended, as the significance of a COPD subtype in relation to OSA severity is unknown. COPD exacerbations and the role they play in hospital admissions were not explored in this cohort, however, would be an important next step to consider. COPD and OSA are common conditions with a complex relationship that is not well understood. Treatment of each should include reciprocal screening for the other. Further exploration of the relationship severity is warranted which may guide targeted therapeutics.
Conclusions
There is significant heterogeneity amongst patients with COPD as well as within OSA. We performed the largest to date evaluation of the association between COPD airflow obstruction and OSA severity in patients with comorbid disease and no significant association was found, even after adjusting for demographic and clinical characteristics. Further evaluation should delve into these associations within each disease subtype.
Abbreviations
COPD, chronic obstructive pulmonary disease; OSA, obstructive sleep apnea; PSG, polysomnography; FEV1/FVC, forced expiratory volume in one second/ forced vital capacity; AHI, apnea hypopnea index; GOLD, Global Initiative for Chronic Obstructive Lung Disease; FEV1, forced expiratory volume in one second; CPAP, continuous positive airway pressure; BMI, body mass index; ED, emergency department; PAP, positive airway pressure; A fib, atrial fibrillation.
Acknowledgments
We appreciate the support of the Graduate Medical Education Office of Research at the University of Nebraska College of Medicine. This study was performed at the University of Nebraska Medical Center.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
Nancy H Stewart reports funding from the CHEST Foundation. Valerie G Press has consulted for Humana, Vizient, and Roundglass. She reports funding from the NIH, AHRQ, the American Medical Association, and the American Lung Association. The authors report no other conflicts of interest in this work.
References
1. Owens RL, Macrea MM, Teodorescu M. The overlaps of asthma or COPD with OSA: a focused review. Respirol Carlton Vic. 2017;22(6):1073–1083. doi:10.1111/resp.13107
2. CDC. Basics about COPD - Chronic Obstructive Pulmonary Disease (COPD); 2019. Available from: https://www.cdc.gov/copd/basics-about.html.
3. CDC. Disease of the week - COPD. Centers for disease control and prevention; 2019. Available from: http://www.cdc.gov/dotw/copd/index.html.
4. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–1014. doi:10.1093/aje/kws342
5. Sanders MH, Newman AB, Haggerty CL, et al. Sleep and sleep-disordered breathing in adults with predominantly mild obstructive airway disease. Am J Respir Crit Care Med. 2003;167(1):7–14. doi:10.1164/rccm.2203046
6. Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med. 2010;182(3):325–331. doi:10.1164/rccm.200912-1869OC
7. Ioachimescu OC, Janocko NJ, Ciavatta MM, Howard M, Warnock MV. Obstructive Lung Disease and Obstructive Sleep Apnea (OLDOSA) cohort study: 10-year assessment. J Clin Sleep Med. 2020;16(2):267–277. doi:10.5664/jcsm.8180
8. Bednarek M, Plywaczewski R, Jonczak L, Zielinski J. There is no relationship between chronic obstructive pulmonary disease and obstructive sleep apnea syndrome: a population study. Respir Int Rev Thorac Dis. 2005;72(2):142–149. doi:10.1159/000084044
9. Putcha N, Crainiceanu C, Norato G, et al. Influence of lung function and sleep-disordered breathing on all-cause mortality. A community-based study. Am J Respir Crit Care Med. 2016;194(8):1007–1014. doi:10.1164/rccm.201511-2178OC
10. Soler X, Gaio E, Powell FL, et al. High prevalence of obstructive sleep apnea in patients with moderate to severe COPD. Ann Am Thorac Soc. 2015:150414075541005. doi:10.1513/AnnalsATS.201407-336OC
11. López-Acevedo MN, Torres-Palacios A, Elena Ocasio-Tascón M, Campos-Santiago Z, Rodríguez-Cintrón W. Overlap syndrome: an indication for sleep studies?: A pilot study. Sleep Breath Schlaf Atm. 2009;13(4):409–413. doi:10.1007/s11325-009-0263-5
12. Mieczkowski B, Ezzie ME. Update on obstructive sleep apnea and its relation to COPD. Int J Chron Obstruct Pulmon Dis. 2014;9:349–362. doi:10.2147/COPD.S42394
13. Shawon MSR, Perret JL, Senaratna CV, Lodge C, Hamilton GS, Dharmage SC. Current evidence on prevalence and clinical outcomes of co-morbid obstructive sleep apnea and chronic obstructive pulmonary disease: a systematic review. Sleep Med Rev. 2017;32:58–68. doi:10.1016/j.smrv.2016.02.007
14. Bradley TD, Rutherford R, Grossman RF, et al. Role of daytime hypoxemia in the pathogenesis of right heart failure in the obstructive sleep apnea syndrome. Am Rev Respir Dis. 1985;131(6):835–839. doi:10.1164/arrd.1985.131.6.835
15. Stewart NH, Walters RW, Mokhlesi B, Lauderdale DS, Arora VM. Sleep in hospitalized patients with chronic obstructive pulmonary disease: an observational study. J Clin Sleep Med. 2020;16(10):1693–1699. doi:10.5664/jcsm.8646
16. Krachman SL, Tiwari R, Vega ME, et al. Effect of emphysema severity on the apnea-hypopnea index in smokers with obstructive sleep apnea. Ann Am Thorac Soc. 2016;13(7):1129–1135. doi:10.1513/AnnalsATS.201511-765OC
17. Biselli P, Grossman PR, Kirkness JP, et al. The effect of increased lung volume in chronic obstructive pulmonary disease on upper airway obstruction during sleep. J Appl Physiol Bethesda Md. 2015;119(3):266–271. doi:10.1152/japplphysiol.00455.2014
18. Konikkara J, Tavella R, Willes L, Kavuru M, Sharma S. Early recognition of obstructive sleep apnea in patients hospitalized with COPD exacerbation is associated with reduced readmission. Hosp Pract. 2016;44(1):41–47. doi:10.1080/21548331.2016.1134268
19. Naranjo M, Willes L, Prillaman BA, Quan SF, Sharma S. Undiagnosed OSA may significantly affect outcomes in adults admitted for COPD in an Inner-City Hospital. Chest. 2020;158(3):1198–1207. doi:10.1016/j.chest.2020.03.036
20. Diab N, Gershon AS, Sin DD, et al. Underdiagnosis and overdiagnosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198(9):1130–1139. doi:10.1164/rccm.201804-0621CI
21. Stein BD, Bautista A, Schumock GT, et al. The validity of international classification of diseases, ninth revision, clinical modification diagnosis codes for identifying patients hospitalized for COPD exacerbations. Chest. 2012;141(1):87–93. doi:10.1378/chest.11-0024
22. Mohamed Hoesein FAA, Zanen P, Lammers JWJ. Lower limit of normal or FEV1/FVC < 0.70 in diagnosing COPD: an evidence-based review. Respir Med. 2011;105(6):907–915. doi:10.1016/j.rmed.2011.01.008
23. Mannino DM, Diaz-Guzman E. Interpreting lung function data using 80% predicted and fixed thresholds identifies patients at increased risk of mortality. Chest. 2012;141(1):73–80. doi:10.1378/chest.11-0797
24. Berry RB, Brooks R, Gamaldo C, et al. AASM Scoring Manual Updates for 2017 (Version 2.4). J Clin Sleep Med. 2017;13(5):665–666. doi:10.5664/jcsm.6576
25. Kennedy B, Lasserson TJ, Wozniak DR, Smith I. Pressure modification or humidification for improving usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev. 2019;12:CD003531. doi:10.1002/14651858.CD003531.pub4
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
