Back to Journals » Journal of Multidisciplinary Healthcare » Volume 12
Evaluating the effectiveness of the “Germ-Free Hands” intervention for improving the hand hygiene practices of public health students
Authors Kitsanapun A, Yamarat K
Received 2 February 2019
Accepted for publication 23 May 2019
Published 9 July 2019 Volume 2019:12 Pages 533—541
DOI https://doi.org/10.2147/JMDH.S203825
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Apaporn Kitsanapun, Khemika Yamarat
College of Public Health Sciences, Chulalongkorn University, Bangkok, Thailand
Purpose: This quasi-experimental study sought to assess the effectiveness of a multidisciplinary intervention called “Germ-Free Hands” to improve the hand hygiene practices of students attending Thailand’s Sirindhorn College of Public Health (SCPH).
Methods: The intervention was developed and implemented at SCPH and incorporated education, training, a workshop, and performance feedback. The intervention targeted behavioral antecedents specified by the Health Belief Model (HBM) and the Theory of Planned Behavior (TPB). Handwashing determinants (knowledge, beliefs, attitudes, subjective norms, perceived behavioral control, and intentions) and hand hygiene behaviors were assessed at baseline, immediately post-intervention, and 3 months post-intervention for the intervention group at (n=60) at the Suphanburi campus of SCPH and a matched control group (n=60) of students at the Ubonratchathani campus. Data analysis included descriptive statistics, independent samples t-tests, two-way measures of analysis of variance, and a generalized estimating equation to compare handwashing practices by self-reports between two groups.
Results: The “Germ-Free Hands” intervention produced significant improvements in the intervention group’s handwashing knowledge, behavioral and control beliefs, subjective norm scores, intentions, and behaviors, as compared to the control group. However, the intervention had no significant impact on normative beliefs, attitudes, or perceived behavioral control. Reported improvements also decreased 3 months post-intervention, and the number of bacterial colonies on students’ hands increased over the course of the study.
Conclusion: This study adds to the evidence that multidisciplinary interventions can be effective at improving handwashing rates. However, education and training must be continuous, rather than delivered as a one-time program, in order to have sustained results. Participants may also require more in-depth instruction in correct handwashing and drying techniques to remove bacteria effectively and prevent recolonization.
Keywords: handwashing, hand hygiene, public health student, Theory of Planned Behavior, Health Belief Model
Introduction
Good hand hygiene practices reduce the risk of disease transmission,1–5 but rates of compliance with handwashing guidelines are low among healthcare practitioners and students.3,4,6–15 For example, one study among nursing students found that they did not practice handwashing sufficiently frequently, nor did they use correct technique.16 Similarly, other studies have found that while 80% of nursing students reported that they washed their hand before and after contact with patients,21,22 only 3.2% of them were observed to wash their hands between each patient visit.21 Furthermore, only 27% of them washed their hands before and after meals.21 Likewise, a study among dental students found that only 40% washed their hands before beginning a surgical procedure.23 However, research has shown that interventions can be effective at improving hand hygiene practices in healthcare settings.3,4,7–9,11,13–15,17–20
Public health students will typically go on to work in primary care services as public health workers, and students are thus expected to correctly implement practices to reduce infection transmission in healthcare settings. However, comparing to other health science students, public health students are less likely to be trained in infection control methods, including the importance of handwashing, because during their school studies they have less contact with patients in hospitals and with other human specimens. However, there has been a lack of research on this topic to date.
The present study examined the effects of a hand hygiene intervention called “Germ-Free Hands” at Thailand’s Sirindhorn College of Public Health (SCPH). The intervention and assessment measures were based on two theoretical frameworks, the Health Belief Model (HBM) and the Theory of Planned Behavior (TPB). According to the HBM, health-related behaviors are influenced by beliefs about susceptibility to health risks and their potential seriousness, by the anticipated benefits of adopting healthier practices, and by the barriers that could make health-promoting behaviors challenging.24 The TPB, in turn, argues that beliefs contribute to attitudes, subjective norms (ie, social pressure to perform an action), and perceived behavioral control (PBC), which is defined as perception of the ease or challenge of performing an action; together, these three variables directly predict intentions, which in turn predict behaviors.25
Prior research has shown that handwashing knowledge,26 behavioral, normative, and control beliefs,27 and attitudes toward handwashing27–30 all influence handwashing behaviors. The present research therefore proposed the following two hypotheses:
H1: The intervention group’s handwashing knowledge, TPB predictors, handwashing rates, correct handwashing scores, and number of microbial colonies on their hands would improve from baseline at immediate post-intervention and 3 months post-intervention assessments; and H2: The intervention group’s TPB predictor scores and self-reported handwashing rates would differ from those of a matched control group immediately post-intervention and 3 months post-intervention.
Materials and methods
A quasi-experimental study design was used to examine the effects of the “Germ-Free Hands” intervention on the rate and quality of handwashing among public health students attending the SCPH campus at Suphanburi (SCPH-SP). Students from the SCPH campus at Ubonratchathani (SCPH-UB) were recruited for the control group. The study was carried out by the primary author as well as by a laboratory technician and six research assistants from SCPH-SP.
Sample
A randomly selected sample of volunteer participants were stratified by study year level. All participants were students studying at SCPH-SP (n=60) or SCPH-UB (n=60), drawn from total populations of 400 students at SCPH-SP and 487 students at SCPH-UB (see Table 1). The majority of students were female, which reflects the overall demographic composition of the SCPH colleges, and 80% were studying Community Public Health (CPH) or Dental Public Health (DPH); the remaining 20% were pursuing vocational certificates in Technical Pharmacy (TP). The two groups were well matched in terms of study level and other factors that have been found to influence handwashing intentions or behaviors, including gender31–33 and handwashing knowledge.26,34,35
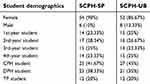 |
Table 1 Demographic characteristics |
Intervention
The “Germ-Free Hands” intervention included a classroom instructional component and a subsequent demonstration session. The instruction consisted of a lecture by the researcher on modes of microbe transmission, handwashing’s effectiveness at preventing the spread of infectious diseases, and the role of public health workers in their communities. The demonstration modeled correct handwashing procedures following World Health Organization (WHO) guidelines.36 Students’ handwashing techniques were then observed and feedback was provided by research assistants. The intervention was conducted over the course of a month, during which students also participated in a 1 hr discussion workshop about the importance of proper handwashing. Posters that reminded students to wash their hands were also hung in prominent places.
Instruments
Hand hygiene questionnaire
A structured seven-part hand hygiene questionnaire was developed for this research based on WHO handwashing guidelines36 and the HBM and TPB theoretical frameworks. The first part collected information about the students’ demographic and educational characteristics; the second part included a 22-question test of handwashing knowledge; and the third through seventh parts consisted of questions on handwashing beliefs, attitudes, subjective norms, PBC, intentions, and behaviors (see Table 2). The questionnaire’s validity was assessed by expert review and its reliability was determined by calculating Cronbach’s alpha scores.37 All items on the final version of the questionnaire had reliability coefficients of >0.7, thereby meeting the threshold for acceptability.38
 |
Table 2 Definitions and sample questions from the hand hygiene questionnaire |
Handwashing observation checklist
Larson and Lusk’s Handwashing Observation Checklist39 was used to score handwashing behaviors and detect errors in technique. This instrument was selected for its high level of inter-rater agreement (95.2%). Observations were performed by three observers; agreement was determined by two of three raters.
Bacterial colonies on hands checklist
Sterile swabs moistened with sterile water were used to swab for bacteria on participants’ hands immediately after a participant finished washing their hands. A Kenner Fecal (KF) Streptococcus agar plate was used to grow fecal streptococci from each participant’s hand. A trained technician then incubated all of the KF agar plates at 35 °C for 48 hrs, after which the researcher and laboratory technician counted the number of colony-forming units growing on each plate. We developed a bacterial colonies on hands checklist to record the number of bacterial colonies on the hands of each SCPH-SP participant at baseline, immediately post-intervention, and 3 months post-intervention.
Data collection and analysis
Participants from the intervention and control groups completed the hand hygiene questionnaire at baseline, immediately post-intervention, and 3 months post-intervention. Handwashing observations, which occurred prior to lunch breaks over the course of 5 days, as well as swabbing for bacteria on students’ hands, were performed by trained research assistants for the intervention group at each assessment phase. The handwashing rate was the total number of handwashing practices over five days divided by the multiplication of the total number of sample sizes and five days.
Data analysis included descriptive statistics and inferential analysis for hypothesis testing, with the threshold for statistical significance set at p<0.05. Repeated-measures analysis of variance was used to test the intervention effect by comparing the TPB predictors and handwashing intentions of the two groups at the three timepoints since those were continuous. The effect sizes were classified into 3 categories: 0.2 is small, 0.5 is medium, 0.8 is large, and 1.3 is very large. A generalized estimating equation was used to analyze the difference in self-reported handwashing practices at each timepoint between the two groups. The distribution of self-reported handwashing practice was considered a binomial distribution with a restricted upper bound.
Results
The intervention group’s baseline scores for handwashing knowledge, TPB predictors, handwashing rates, correct handwashing scores, and number of microbial colonies on hands were compared to their scores immediately post-intervention and again 3 months post-intervention. The immediate post-intervention scores changed significantly from baseline for handwashing knowledge (p=0.0112) and some of the TPB variables, including behavioral beliefs (p=0.0001), control beliefs (p=0.0006), subjective norms (p=0.0152), and handwashing intensions (p=0.0115). However, the effect size of significant variables were small meaning that the difference was trivial. No significant differences were found for normative beliefs (p=0.0695), attitudes (p=0.1715), or PBC (p=0.2119). We also observed a trend of scores increasing from baseline to post-intervention but then decreasing at 3 months post-intervention. This suggests that gains from the intervention were not maintained (see Table 3).
 |
Table 3 SCPH-SP intervention group mean scores and standard deviations at baseline, immediately post-intervention, and 3 months post-intervention |
Handwashing rates prior to eating lunch over the course of the 5 days of observation increased substantially from baseline (18%) to immediately post-intervention (93%), and although they decreased somewhat at 3 months post-intervention (72%), they remained significantly higher than baseline rates (see Table 4). Correct handwashing scores showed a similar trend, increasing from 33.5% at baseline to 47.1% immediately post-intervention and then falling to 43.0% at 3 months post-intervention. However, the number of bacterial colonies on the students’ hands actually increased over the course of the study, and handwashing quality scores remained below 50% even immediately post-intervention.
 |
Table 4 Observed handwashing behaviors, correct handwashing scores, and bacterial colonies on hands of students in the intervention group before eating lunch (n=60) |
Self-reported handwashing rates per 10 instances in circumstances in which handwashing is required increased significantly from baseline to immediately post-intervention but declined at 3 months post-intervention for the intervention group over the course of the study in all circumstances. As compared to the control group, the statistically changed handwashing rates in the intervention group were after using toilet (p=0.0005), after coughing or sneezing (p=0105), after touching dirty objects (p<0.0001), after playing with pets (p<0.0001), and after visiting patients (p=0.0133) (see Table 5).
 |
Table 5 Comparison in self-reported handwashing practices per 10 incidences for which handwashing is required among the intervention and control groups |
TPB predictors were also compared for the intervention and control groups immediately post-intervention and 3 months post-intervention (see Table 6). Statistically significant group differences were found for attitudes (p=0.0322), subjective norms (p=0.0103), and handwashing intentions (p=0.0049). However, there was no significant difference between the two groups for PBC (p=0.3533).
 |
Table 6 Group differences in TPB predictors and handwashing intentions |
Overall, these findings demonstrate partial support for both H1 and H2. Differences in handwashing determinants and rates were found for the intervention group (SCPH-SP) between baseline and both post-intervention assessments, and between the intervention and control groups post-intervention. However, the intervention group scores did not change significantly from baseline for all the TPB variables. In addition, self-reported handwashing rate changes varied between handwashing situations, and the bacterial colonies found on participants’ hands did not decrease substantially from baseline as expected.
Discussion
Consistent with prior research,3,4,7–9,11,13–15,17–20,40 our results indicate that education and training can improve hand hygiene practices. However, the relative effectiveness of handwashing interventions has varied between studies, likely due to the use of different interventions and outcome measures. Previous interventions have typically included some combination of instruction, problem-based learning, reminders, evaluation, feedback, focus groups, and workshops, and some of these components may be more beneficial than others. Observed handwashing rates for the SCPH-SP intervention group rose from 18% at baseline to 93% immediately post-intervention and were maintained at 72% 3 months after the intervention. These post-intervention gains compare favorably to those seen in other studies, which have had highly variable starting points (ranging from 4% to 50%) and outcomes (ranging from 25% to 84%).6–8,14,19,41,42
There were large differences between self-reported and observed handwashing rates for the intervention group at all three assessments—a problem that has also been noted by other hand hygiene intervention researchers.27,43,4 Our participants had much higher self-reported (61%) than observed (18%) rates of handwashing at baseline and much smaller improvements in self-reported handwashing (7.5% increase) than observed practice (75% increase) at the immediate post-intervention assessment. It is possible that students over-reported their handwashing at baseline due to a social desirability bias effect4,45 or faulty memories. However, it is also possible that their awareness of being observed increased their handwashing rates after the intervention, or that their handwashing rates prior to eating lunch were more susceptible to intervention effects than handwashing practices in other situations.
The findings of this study support the HBM,24 as we found that handwashing practices changed in conjunction with behavioral and control beliefs related to perceived seriousness, susceptibility, barriers, and benefits. Our findings also provide limited support for the TPB,25 since participant behavioral and control beliefs, subjective norms, and intentions changed after the intervention along with actual handwashing behaviors (although no post-intervention changes were seen in normative beliefs, attitudes, or PBC). These findings are consistent with those of other research that has shown that handwashing practices are influenced by beliefs27 and subjective norms.27,28,30 The corresponding increases in handwashing knowledge and practice in this study are also in line with previous findings that knowledge predicts healthcare providers’ hand hygiene behaviors.4,6,34
Overall, the intervention was effective at improving some handwashing determinants and behaviors for the intervention group between the baseline and post-intervention assessments, and the intervention group differed significantly from the control group at post-intervention assessments of attitudes, subjective norms, intentions, and self-reported handwashing rates, providing further evidence for the benefits of hand hygiene education and training. However, the change of determinants between timepoints was negligible. Therefore, the full benefits of the intervention were not maintained, as scores followed a U-shaped curve of significant increase immediately after intervention and a subsequent decline at 3 months post-intervention. This trend has been noted in other handwashing intervention studies as well,4,7,9,15 indicating a need for ongoing rather than time-limited education and training programs.
Another notable finding is that the number of bacterial colonies on the students’ hands increased despite improved handwashing rates. This unexpected result may be attributable to insufficient use of soap or failure to wash hands for the full 40–60 seconds recommended by the WHO.36 However, it is also possible that some of the participants did not dry their hands properly, thereby creating a moist environment conducive to bacterial colonization, or dried their hands on their clothing, thereby adding new bacteria after washing.
Strengths of this study include that it provides information regarding handwashing behaviors among public health students, that results were measured by both self-report and external observation, and that it assessed handwashing determinants based on two theoretical foundations, the HBM and the TPB. However, given the limitations of short-term interventions and assessments, additional research is needed to develop and evaluate long-term interventions that include instruction on hand drying in addition to correct handwashing procedures. Conducting ongoing education and training with longitudinal assessments of program effectiveness would be beneficial for determining what sort of training or follow-ups are required to maintain good hand hygiene practices.
Conclusion
Despite the known risks of hand-based transmission of nosocomial infections, rates of handwashing are relatively low among healthcare workers and students. This study assessed the effectiveness of the “Germ-Free Hands” education and training program for improving handwashing rates among students attending a Thai public health college, using the HBM and TPB as theoretical frameworks. The intervention’s effects on handwashing determinants and practices were assessed at baseline, immediately post-intervention, and 3 months post-intervention, and post-intervention scores were compared with baseline scores and with the scores of a matched control group from a similar public health campus.
We found that the intervention improved the intervention group’s handwashing knowledge, behavioral and control beliefs that encourage handwashing, subjective norm perceptions of handwashing as a socially expected practice, handwashing intentions, and both self-reported and observed handwashing practices. However, the intervention had no impact on normative beliefs, attitudes toward handwashing, or PBC. There were also large differences between self-reported and observed rates of handwashing, which may be attributable to social desirability bias or faulty memories affecting self-reported rates, or to an observation effect on actual handwashing behavior. We also found that the benefits of the intervention declined over time, with large gains in handwashing rates immediately post-intervention followed by a decrease in scores at 3 months post-intervention, although observed handwashing rates remained well above the baseline level 3 months post-intervention. However, despite participants’ increased handwashing, the number of bacterial colonies on their hands rose over the course of the study rather than substantially declining.
Studies tend to find major differences in self-reported and observed handwashing rates, and future program assessments should use objective measures, such as covert observation and measurements of the volume of soap used. Moreover, whenever possible these evaluations should be conducted for all situations where handwashing is indicated, since we found that study participants were more inclined to wash their hands in some situations than others. It would also be useful to compare the effects of different intervention components to determine which education and training strategies are likely to have the greatest long-term impacts on hand hygiene practices.
Ethics approval and informed consent
This study’s protocol was approved by the Research Ethics Committee for Research Involving Human Research Participants, Health Sciences Group, Chulalongkorn University, Thailand. Committee approval is in accordance with the International Conference on Harmonization—Good Clinical Practice. Written informed consent were obtained from all participants. The research respected the confidentiality of all information collected from participants.
Acknowledgments
The authors thank all students at SCPH-SP and SCPH-UB who participated in this study.
Disclosure
Miss Apaporn Kitsanapun reports that she is an instructor at Sirindhorn College of Public Health Suphanburi where the study was conducted. The authors report no further conflicts of interest in this work.
References
1. Aiello AE, Coulborn RM, Perez V, Larson EL. Effect of hand hygiene on infectious disease risk in the community setting: a meta-analysis. Am J Public Health. 2008;98(8):1372–1381. doi:10.2105/AJPH.2007.124610
2. Curtis V, Cairncross S. Effect of washing hands with soap on diarrhoea risk in the community: a systematic review. Lancet Infect Dis. 2003;3(5):275–281.
3. Helder OK, Brug J, Looman CW, van Goudoever JB, Kornelisse RF. The impact of an education program on hand hygiene compliance and nosocomial infection incidence in an urban neonatal intensive care unit: an intervention study with before and after comparison. Int J Nurs Stud. 2010;47(10):1245–1252. doi:10.1016/j.ijnurstu.2010.03.005
4. Lam BC, Lee J, Lau Y. Hand hygiene practices in a neonatal intensive care unit: a multimodal intervention and impact on nosocomial infection. Pediatrics. 2004;114(5):e565–e571. doi:10.1542/peds.2004-1107
5. Larson E. A causal link between handwashing and risk of infection? Examination of the evidence. Infect Control Hosp Epidemiol. 1988;9(1):28–36. doi:10.1086/645729
6. Bischoff WE, Reynolds TM, Sessler CN, Edmond MB, Wenzel RP. Handwashing compliance by health care workers: the impact of introducing an accessible, alcohol-based hand antiseptic. Arch Intern Med. 2000;160(7):1017–1021.
7. Erasmus V, Kuperus M, Richardus JH, Vos M, Oenema A, Van Beeck E. Improving hand hygiene behaviour of nurses using action planning: a pilot study in the intensive care unit and surgical ward. J Hosp Infect. 2010;76(2):161–164. doi:10.1016/j.jhin.2010.04.024
8. Higgins A, Hannan M. Improved hand hygiene technique and compliance in healthcare workers using gaming technology. J Hosp Infect. 2013;84(1):32–37. doi:10.1016/j.jhin.2013.02.004
9. KuKanich KS, Kaur R, Freeman LC, Powell DA. Original research: evaluation of a hand hygiene campaign in outpatient health care clinics. Am J Nurs. 2013;113(3):36–42. doi:10.1097/01.NAJ.0000427878.80053.f7
10. Martín-Madrazo C, Soto-Díaz S, Salinero-Fort MA, et al. Cluster randomized trial to evaluate the effect of a multimodal hand hygiene improvement strategy in primary care. Infect Control Hosp Epidemiol. 2012;33(07):681–688. doi:10.1086/666343
11. Pittet D. Improving compliance with hand hygiene in hospitals. Infect Control Hosp Epidemiol. 2000;21(06):381–386. doi:10.1086/501777
12. Pittet D. Hand hygiene: it’s all about when and how. Infect Control Hosp Epidemiol. 2008;29(10):957–959. doi:10.1086/592218
13. Scheithauer S, Rosarius A, Rex S, et al. Improving hand hygiene compliance in the anesthesia working room work area: more than just more hand rubs. Am J Infect Control. 2013;41(11):1001–1006. doi:10.1016/j.ajic.2013.02.004
14. Song X, Stockwell DC, Floyd T, Short BL, Singh N. Improving hand hygiene compliance in health care workers: strategies and impact on patient outcomes. Am J Infect Control. 2013;41(10):e101–e105. doi:10.1016/j.ajic.2013.01.031
15. Tromp M, Huis A, de Guchteneire I, et al. The short-term and long-term effectiveness of a multidisciplinary hand hygiene improvement program. Am J Infect Control. 2012;40(8):732–736. doi:10.1016/j.ajic.2011.09.009
16. Doron SI, Kifuji K, Hynes BT, et al. Infection prevention and control a multifaceted approach to education, observation, and feedback in a successful hand hygiene campaign. Jt Comm J Qual Patient Saf. 2011;37(1):3–3AP.
17. Gould DJ, Moralejo D, Drey N, Chudleigh JH. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst Rev. 2010;9:1–50.
18. Pessoa-Silva CL, Hugonnet S, Pfister R, et al. Reduction of health care–associated infection risk in neonates by successful hand hygiene promotion. Pediatrics. 2007;120(2):e382–e390. doi:10.1542/peds.2007-2361
19. Whitby M, McLaws ML, Slater K, Tong E, Johnson B. Three successful interventions in health care workers that improve compliance with hand hygiene: is sustained replication possible? Am J Infect Control. 2008;36(5):349–355. doi:10.1016/j.ajic.2007.07.016
20. Hochbaum G, Rosenstock I, Kegels S. Health Belief Model. United States Public Health Service; 1952:W432W8784.
21. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi:10.1016/0749-5978(91)90020-T
22. Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med. 2004;141(1):1–8.
23. O’Boyle CA, Henly SJ, Larson E. Understanding adherence to hand hygiene recommendations: the theory of planned behavior. Am J Infect Control. 2001;29(6):352–360. doi:10.1067/mic.2001.18405
24. Jenner E, Watson P, Miller L, Jones F, Scott G. Explaining hand hygiene practice: an extended application of the Theory of Planned Behaviour. Psychol Health Med. 2002;7(3):311–326. doi:10.1080/13548500220139412
25. De Wandel D, Maes L, Labeau S, Vereecken C, Blot S. Behavioral determinants of hand hygiene compliance in intensive care units. Am J Crit Care. 2010;19(3):230–239. doi:10.4037/ajcc2010892
26. Whitby M, McLaws ML, Ross MW. Why healthcare workers don’t wash their hands: a behavioral explanation. Infect Control. 2006;27(05):484–492.
27. Hiller J, Schatz K, Drexler H. Gender influence on health and risk behavior in primary prevention: a systematic review. J Public Health (Bangkok). 2017;25(4):339–349. doi:10.1007/s10389-017-0798-z
28. Korniewicz DM, El-Masri M. Exploring the factors associated with hand hygiene compliance of nurses during routine clinical practice. Appl Nurs Res. 2010;23(2):86–90. doi:10.1016/j.apnr.2008.06.002
29. Sax H, Uçkay I, Richet H, Allegranzi B, Pittet D. Determinants of good adherence to hand hygiene among healthcare workers who have extensive exposure to hand hygiene campaigns. Infect Control Hosp Epidemiol. 2007;28(11):1267–1274. doi:10.1086/521663
30. Al-Khawaldeh OA, Al-Hussami M, Darawad M. Influence of nursing students handwashing knowledge, beliefs, and attitudes on their handwashing compliance. Health. 2015;7(5):572. doi:10.4236/health.2015.75068
31. Zil-E-Ali A, Cheema MA, Ullah MW, Ghulam H, Tariq M. A survey of handwashing knowledge and attitudes among the healthcare professionals in Lahore, Pakistan. Cureus. 2017;9(3):e1089.
32. World Health Organization. WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge. Clean Care Is Safer Care. Geneva, Switzerland: World Health Organization; 2009.
33. Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. doi:10.1007/BF02310555
34. Cortina JM. What is coefficient alpha? An examination of theory and applications. J Appl Psychol. 1993;78(1):98. doi:10.1037/0021-9010.78.1.98
35. Larson E, Lusk E. Evaluating handwashing technique. J Adv Nurs. 2006;53(1):46–50. doi:10.1111/j.1365-2648.2006.03666.x
36. O’Donoghue M, Ng S-H, Suen LK, Boost M. A quasi-experimental study to determine the effects of a multifaceted educational intervention on hand hygiene compliance in a radiography unit. Antimicrob Resist Infect Control. 2016;5(1):36. doi:10.1186/s13756-016-0133-4
37. Doronina O, Jones D, Martello M, Biron A, Lavoie‐Tremblay M. A systematic review on the effectiveness of interventions to improve hand hygiene compliance of nurses in the hospital setting. J Nurs Scholarsh. 2017;49(2):143–152. doi:10.1111/jnu.12274
38. Kingston L, O’Connell N, Dunne C. Hand hygiene-related clinical trials reported since 2010: a systematic review. J Hosp Infect. 2016;92(4):309–320. doi:10.1016/j.jhin.2015.11.012
39. Nematian SSS, Palenik CJ, Mirmasoudi SK, Hatam N, Askarian M. Comparing knowledge and self-reported hand hygiene practices with direct observation among Iranian hospital nurses. Am J Infect Control. 2017;45(6):e65–e67. doi:10.1016/j.ajic.2017.03.007
40. Jenner EA, Fletcher BC, Watson P, Jones F, Miller L, Scott G. Discrepancy between self-reported and observed hand hygiene behaviour in healthcare professionals. J Hosp Infect. 2006;63(4):418–422. doi:10.1016/j.jhin.2006.03.012
41. Contzen N, De Pasquale S, Mosler H-J. Over-reporting in handwashing self-reports: potential explanatory factors and alternative measurements. PLoS One. 2015;10(8):e0136445. doi:10.1371/journal.pone.0136445
42. Korhonen A, Vuori A, Lukkari A, et al. Increasing nursing students’ knowledge of evidence-based hand-hygiene: a quasi-experimental study. Nurse Educ Pract. 2019;35:104–110. doi:10.1016/j.nepr.2018.12.009
43. Neo JRJ, Sagha-Zadeh R, Vielemeyer O, Franklin E. Evidence-based practices to increase hand hygiene compliance in health care facilities: an integrated review. Am J Infect Control. 2016;44(6):691–704. doi:10.1016/j.ajic.2015.11.034
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
