Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 10
Etiology, Clinical Features, And Short-Term Outcome Of Seizures In Newborns Admitted To The University Of Gondar Hospital, Ethiopia
Received 22 August 2019
Accepted for publication 27 September 2019
Published 18 October 2019 Volume 2019:10 Pages 107—113
DOI https://doi.org/10.2147/PHMT.S228241
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Hailu Tazebew Amare, Ashenafi Tazebew Amare
Department of Pediatrics and Child Health, University of Gondar, College of Medicine and Health Sciences, Gondar, Ethiopia
Correspondence: Ashenafi Tazebew Amare
Department of Pediatrics and Child Health, P.O. Box 196, Bekafa Street, Gondar, Ethiopia
Tel + 251-913-16-47-22
Email [email protected]
Background: Neonatal seizures are the most common neurological dysfunction in the neonatal period. Neonatal seizure patterns and short-term neurologic outcomes, particularly in the Ethiopian context, have not been adequately studied.
Objective: The main aim of this study is to assess the pattern, probable etiology, short-term outcomes, and determinants of neonatal seizures in the neonatal intensive care unit of Gondar University Specialized Comprehensive Hospital.
Methods: A hospital-based prospective observational cohort study was conducted from October 1, 2016, to September 30, 2018.
Results: Among the 117 neonates enrolled, the most common type of neonatal seizure was subtle (60.6%), followed by tonic (15.4%), and clonic (12.8%) seizures. The most common etiology for the seizure was perinatal asphyxia (PNA) with hypoxic-ischemic encephalopathy (HIE; 74.4%) followed by electrolyte disturbances (12.8%). In the follow-up, 23 (19.7%) died during the acute neonatal illness. The most common cause of death was PNA with HIE, accounting for 73.9% of the deaths. Among the surviving newborns, 10 (10.6%) had neurodevelopmental deficits at discharge. Being a multiparous mother (OR= 0.172; 95% CI: 0.033, 0.880), being female (OR= 0.171; 95% CI: 0.055, 0.538), and having tonic (OR= 0.164; 95% CI: 0.030, 0.885) and myoclonic seizures (OR= 0.040; 95% CI: 0.055, 0.538) were significantly associated with mortality poor short-term outcome.
Conclusion: Subtle seizures were the most common seizure semiology. The most common etiology for seizure was PNA with HIE. Parity, gestational age, neonatal sex, and seizure type were determinants of short-term outcomes.
Keywords: hypoxia-ischemic encephalopathy, neonatal seizures, newborn, etiology, mortality
Introduction
Neonatal seizures are the most common neurological disorder in the neonatal period. Seizures are a paroxysmal alteration in neurological functions like motor, behavior, and/or autonomic function and can occur at any gestational age. Neonatal seizures often indicate an underlying neurologic disturbance. They require an immediate assessment to determine the underlying cause and necessary interventions.1
Seizures are a potentially life-threatening problem with a variety of causes. Thorough and timely evaluations of seizures are necessary to identify and treat the underlying etiology, thereby reducing potential morbidity and mortality.
Studies from different low-income countries showed that perinatal asphyxia with hypoxic-ischemic encephalopathy (HIE) is the most common cause.2–5 Metabolic abnormalities, infection, intracranial hemorrhage, developmental anomalies, and others like inborn errors of metabolism are rare causes of neonatal seizures.6,7 They are important to consider as their detection allows appropriate counseling and may permit specific therapy.8
Factors associated with neonatal seizures include etiology, type of seizure, status epilepticus, early onset of seizures, gestational age, Apgar score, birth weight, need for resuscitation, neurological examination at the onset of seizure, electroencephalogram (EEG), and radiological findings. The reliability of most of these factors is limited because of different reasons.9 However, there are no published studies in Ethiopia regarding neonatal seizure etiology to compare the frequency, probable etiologies, and short-term outcome of neonatal seizures with studies done elsewhere.
The aim of this study is to determine the pattern, probable etiology, and short-term outcome of neonatal seizures in Gondar University Comprehensive specialized hospital neonatal intensive care unit (NICU).
Methods And Subjects
Study Setting And Period
This was a hospital-based, prospective observational cohort study involving the clinical and laboratory data collection conducted in the neonatal intensive care unit of Gondar University hospital from October 1, 2016, to September 30, 2018.
This study was conducted at the University of Gondar Hospital (UoGH), which is one of the largest referral hospitals with access to about 5 million people and also one of the oldest academic institutions in Ethiopia. UoGH is located at the heart of Gondar city in the northwestern part of the country. The NICU was established 20 years ago and serves as a tertiary and a referral unit for the region. It receives high-risk babies delivered within the institution, referrals from other health facilities, and referrals from home deliveries. The number of admitted neonates varies from time to time, with an average of 1500 admissions every year.
Data Collection And Processing
Inclusion Criteria
Any neonates with reported or observed seizure and unequivocal description of seizure by the parents or clinicians were included in the study.
Exclusion Criteria
Neonates with uncertain clinical manifestations like jitteriness, tetanic spasms, and newborns with complex malformations and syndromic presentations were excluded.
After enrolment, baseline characteristics of convulsive neonate, including gender, gestational age, and weight were recorded at admission. A detailed antenatal history, which included history of maternal illness during pregnancy, prenatal history, labor records for evidence of fetal distress, Apgar score, and type of delivery were recorded in a pretested case recording format. Discharge, duration of stay, condition at discharge, and seizure control were recorded.
Operational Definitions
The diagnosis of neonatal seizures is based on clinical observation and an accurate description of the type of seizures. We classified seizures according to the International League Against Epilepsy: subtle, tonic, clonic, myoclonic, and mixed.10 A complete clinical examination of neonates, blood glucose, total serum calcium, and magnesium levels were done immediately after neonate had seizures and before starting any specific treatment. The seizure etiology diagnosis was based on clinical data, laboratory findings, and/or brain imaging studies. Various criteria for diagnosing metabolic abnormalities were defined as hypoglycemia; blood sugar <40 mg/dL (2.2 mmol/L), hypocalcemia; total serum calcium <7.0 mg/dL (1.7 mmol/L), hypomagnesemia; serum magnesium <1.5 mg/dL, hyponatremia; serum sodium <125 mEq/L, and hypernatremia when it is >150 mEq/L.
The diagnosis of HIE was based on history, physical examination, Apgar score, arterial blood gas, and neuroimaging. The diagnosis of neonatal infection was based on the clinical manifestation, sepsis workup, and positive blood, urine, and/or urine culture. Bacterial meningitis was confirmed by positive CSF cell count or culture. Acute bilirubin encephalopathy was diagnosed by high total serum bilirubin plus clinical manifestations. At the time of discharge, duration of stay, condition at discharge, and seizure control will be recorded. Short-term outcome in this study was defined as an outcome at the time of discharge which is death and neurologic status.
Data Entry, Analyses, And Processing
The extracted data were analyzed using SPSS software package version 21. Frequencies, cross-tabulation, and Chi-square test were used for data analysis. Binary logistic regression was fitted to identify factors associated with treatment outcome. Variables with p-value <0.25 were fitted to multivariate logistic regression analysis. Odds ratio with the corresponding 95% confidence interval was calculated to show the strength of association. In multivariate analysis, variables with p-value <0.05 were considered statistically significant. Descriptive statistics like percentage, mean, and standard deviation were presented.
Ethical Approval
Ethical clearance was obtained from the Ethical review board of University of Gondar, School of Medicine. All data were collected after the management of the neonate is complete. A written consent was obtained from the mother/father before collecting data and that the study was conducted in accordance with the Declaration of Helsinki.
Results
Socio-Demographic Characteristics Of Patients
A total of 117 patients were included in the study. The demographic data revealed that the number of male and female patients was 86 (73.5%) and 31 (26.5%), respectively. The mean (± SD) of age at admission was 55.79 ± 133.36 hrs (2.3 ± 5.6 days). The minimum and maximum age of patients involved was 0.25 hrs and 648 hrs (27 days), respectively (Table 1). The majority of study participants are delivered to mothers in the age range of 25–35 years (53.8%) (Table 2).
 |
Table 1 Sociodemographic Characteristics Of Study Participants At The University Of Gondar Hospital, NICU, In Northwest Ethiopia, 2016–2018 (n=117) |
 |
Table 2 Socio-Demographic And Other Characteristics Of Mothers Of Babies With Neonatal Seizures In University Of Gondar Hospital, NICU, In Northwest Ethiopia, 2016–2018 (n=117) |
Classification Of Neonatal Seizures
Of the 117 study participants, subtle seizures were the most common seizure type (60.6%) followed by tonic seizure (15.4%) and clonic (12.8%) seizure (Table 3).
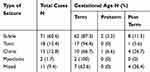 |
Table 3 Types Of Clinical Seizure In Babies With Neonatal Seizure In Gondar University Comprehensive Specialized Hospital, NICU, 2016–2018 (n=117) |
Possible Etiology Of Seizure
The most common etiology for seizure was PNA with HIE (74.4%) followed by transient metabolic disturbances (hypocalcemia, hyponatremia, hypernatremia) (12.8%) (Table 4). Of all the newborns with seizures, 72.6% of them had a seizure during the first 24 hrs of life (Table 5).
 |
Table 4 Etiologic Profile In Neonates With Seizure In Gondar University Comprehensive Specialized Hospital, NICU, 2016–2018 (n=117) |
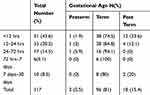 |
Table 5 Onset Of Seizure In Neonates With Seizure In Gondar University Comprehensive Specialized Hospital, NICU, 2016–2018 (n=117) |
Management Of Neonatal Seizure
Among 27 (23.1%) patients, seizures were controlled with monotherapy (either calcium gluconate or phenobarbital). Dual (calcium gluconate and phenobarbital) and triple (calcium gluconate, phenobarbital, and phenytoin) therapies were used in 50 (42.7%) and 40 (34.2%) patients, respectively. About six (5.1%) need intermittent diazepam to control seizures. Four out of six neonates had subtle seizures.
Duration Of Stay In The Ward
The length of stay in the ward with mean ± SD was 209.64 ± 134.01 hrs (8.7 ± 5.6 days) with a minimum and maximum of 0.5 days and 25 days, respectively
Outcome
In the follow-up, 23 (19.7%) died during the acute neonatal illness and 10.6% of surviving newborns had neurologic sequelae like motor deficits, spasticity and decreased the level of consciousness at the time of discharge (Table 6). The most common cause of death was PNA with HIE accounting for 73.9% of the deaths. Death is common among babies with the onset of seizure between 24 and 72 hrs of age.
 |
Table 6 Short-Term Outcome In Neonates With Seizure In Gondar University Comprehensive Specialized Hospital, NICU, 2016–2018 (n=117) |
Determinants Of Short-Term Outcome
Multivariate logistic regression output indicated that parity, gestational age, sex of newborn, and type of seizure were significantly associated with mortality as shown in Table 7.
 |
Table 7 A Bivariate And Multivariate Logistic Regression Output Showing Factors Associated With Short-Term Outcomes In Neonates With Seizure GUH, Northwest Ethiopia, 2016–2018 (n=117) |
The likelihood of death from neonates having seizures was decreased by 82.8% in multiparous mothers (AOR= 0.172; 95% CI: 0.033, 0.880) as compared with primiparous mothers.
The likelihood of survival in neonates with seizure was 42 times higher in terms than preterm (OR= 42.334; 95th CI: 1.326, 1351.3). The odds of death in male neonates with seizure were 5.84 lower than female neonates with seizure (OR= 0.171; 95% CI: 0.055, 0.538).
As compared with neonates with subtle seizure, those with tonic and myoclonic seizures have a higher mortality rates about 83.6% (OR= 0.164; 95% CI: 0.030, 0.885) and 96% (AOR= 0.040; 95% CI: 0.055, 0.538) respectively.
Discussion
Seizures are the most important clinical manifestation of neurological disorders in the neonatal period. Even though seizures are usually reported to occur more frequently in premature infants,11 in the present study, we observed a predominance of seizures in term newborns with birth weight appropriate to gestational age. These results agree with another studies done by Gacias da Silva et al12 and Holand M et al.13 This finding might be related to regional peculiarities of maternal and birth care or perhaps due to the high incidence of perinatal asphyxia in our cohort, which is a more common cause of seizure in term newborns rather than preterms in whom interventricular hemorrhage and infections are the most frequent causes.14
In this study, seizure was more common in male neonates as other studies. This could be due to prominent occurrence of opening of the chloride channels, which are excitatory in immature brains, in male brain than females’ results in depolarizing the cell perhaps explaining their greater predisposition to seizures.15–17
Perinatal asphyxia, in this study, in agreement with other series, was the most frequent etiology related to neonatal seizures. It is comparable to studies which have shown the incidence from 73.9% to 44%.2,15,16,17, 18, 1917–21 neonates with HIE followed by of neonates with metabolic abnormalities and intracranial hemorrhage while the main diagnosis in another study was sepsis in 85 (60%) then neonatal encephalopathy in 30 (21%).20 Metabolic abnormalities were found in 42 (47.7%) neonates followed by birth asphyxia representing the second most common cause in his study 14 (15.9%) neonates.7 Despite being most common, percentage difference could be because of lack of complete investigation in the study setting due to financial constraints and the high number of term newborns in the study.
In the present study, subtle seizure was found to be the most common type of neonatal seizure accounting for 60.7%, similar results were described in other studies conducted in different settings.6,7,21,22 However, these were different from studies in which clonic seizures were the most common.20,21 In a study conducted by Soni et al, the commonest type of seizures in term group was tonic seizures which were seen in 15 (37.5%) neonates and subtle seizures in 10 (25%) neonates.22
The outcome of neonates with seizure in our study, where the mortality rate was 19.6%, is comparable with findings reported by Sahana et al15 study in which 49.54% of the neonates had recovered completely, 32.11% of the neonates had neurological sequelae, and 18.35% of the neonates died. However, it was higher than that (14.7%) reported in the study of Sabzehei et al.6 The difference in the mortality rates from different settings is primarily dependent on the level of the neonatal care and the etiologic factors.
Multivariate logistic regression output indicated that sex of newborn and type of seizure was significantly associated with short-term outcomes. As compared with neonates with subtle seizure, those with tonic and myoclonic seizures have higher death rates about 83.6% (OR= 0.164; 95% CI: 0.030, 0.885) and 96% (OR= 0.040; 95% CI: 0.055, 0.538), respectively. This could be associated with the fact that it was associated with meningitis and delayed onset of seizure in HIE which suggests a structural abnormality rather than common metabolic causes.
The main strength of this study is that it is a prospective observational study which is done for the first time in Ethiopia as far as the author’s knowledge is concerned. However, it has its limitations. The inclusion of newborns with seizures was based on clinical criteria without synchronized video EEG recording might have resulted in the inclusion of newborns with seizure mimics which have different causes and outcomes. The fact that advanced neuroimaging studies were not done in the majority of cases due to financial constraints is another major limitation. This study includes short-term follow-up only; further, follow-up is required to evaluate long-term neurological follow-up.
The study revealed subtle seizure was the most common type of neonatal seizure which is common among neonates with asphyxia and metabolic abnormalities. HIE was the commonest etiology of neonatal seizures and in most of the seizures had an onset in the first 72 hrs. Parity, gestational age, neonatal sex, and seizure type were determinants of short-term outcome.
Conclusion
The study revealed subtle seizure was the most common type of neonatal seizure, which is common among neonates with asphyxia and metabolic abnormalities. HIE was the most common etiology of neonatal seizures, which had an onset within the first 72 hrs of what birth. Parity, gestational age, neonatal sex, and seizure type were determinants of mortality of short-term outcome.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors are grateful for the authors, editors, and publishers of the articles that are cited and included in the references for this manuscript. We would also like to express our deep gratitude to Dr. Rishi Mediratta for English editing and Mr. Tiruneh Ayele for his comments and suggestions.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mosley M. Neonatal seizures. Pediatr Rev. 2010;31:127–128. doi:10.1542/pir.31-3-127
2. Aziz A, Gattoo I, Aziz M, Rasool G. Clinical and etiological profile of neonatal seizures: a tertiary care hospital-based study. Int J Res Med Sci. 2015;3(9):2198–2203. doi:10.18203/2320-6012.ijrms20150601
3. Najeeb S, Qureshi AM, Rehman A, et al. Aetiology and types of neonatal seizures presenting at Ayub Teaching Hospital Abbottabad. J Ayub Med Coll Abbottabad. 2012;24(1):33–37.
4. Malik AR, Quddusi AI N. Neonatal seizures, experience at Children Hospital and Institute of Child Health Multan. Pak J Med Sci. 2013;29(5):1128–1131. doi:10.12669/pjms.295.3847
5. Talebian A, Jahangiri M, Rabiee M, Masoudi Alavi N, Akbari H, Sadat Z. The etiology and clinical evaluations of neonatal seizures in Kashan, IRAN. Iran J Child Neurol. 2015;9(2):29–35.
6. Sabzehei M, Basiri B, Bazmamoun H. The etiology, clinical type, and short outcome of seizures in Newborns Hospitalized in Besat Hospital/Hamadan/Iran. Iran J Child Neurol. 2014;8(2):24–28.
7. Marzoki JMA. Clinco- biochemical profile of neonatal seizures. QMJ. 2010;6(10):163–164.
8. Chan DWS, Cleary MA. Neonatal seizures: when to consider and how to investigate for an inborn error of metabolism. Proc Singapore Healthcare. 2010;19(2):112–113. doi:10.1177/201010581001900206
9. Pisani F, Sisti L, Seri S. A scoring system for early prognostic assessment after neonatal seizures. Pediatrics. 2009;124:e580–7. doi:10.1542/peds.2008-2087
10. Report of ILAE task Force on Neonatal Seziures. Available from: https://www.ilae.org/guidelines/definition-and-classification/neonatal-seizure-classification.
11. Lahorgue Nunes M, Costa da Costa J. Outcome of newborns with neonatal seizures: risk factors and predictors. Curr Pediatr Rev. 2006;2:315–321. doi:10.2174/157339606778699662
12. Da Silva LFG, Nunes ML, Da Costa JC. Risk factors for developing epilepsy after neonatal seizures. Pediatr Neurol. 2004;30:271–277. doi:10.1016/j.pediatrneurol.2003.09.015
13. Holanda MRR, Melo AN. Comparative clinical study of preterm and full-term newborn neonatal seizures. Arq Neuropsiquiatr. 2006;64:45–50. doi:10.1590/s0004-282x2006000100010
14. Vasudevan C, Levene M. Epidemiology and aetiology of neonatal seizure. Semin Fetal Neonatal Med. 2013;18(4):185–191. doi:10.1016/j.siny.2013.05.008
15. Sahana G, Anjaiah B. Clinical profile of neonatal seizures. Int J Med Appl Sci. 2014;3(1):21–27.
16. Kumar A, Gupta A, Talukdar B. Clinico-etiological and EEG profile of neonatal seizures. Indian J Pediatr. 2007;74(1):33–37. doi:10.1007/s12098-007-0023-0
17. Hallberg B, Blennow M. Investigations for neonatal seizures. Semin Fetal Neonatal Med. 2013;18(4):196–201. doi:10.1016/j.siny.2013.03.001
18. Rastogi S, Rai PL, Prasad PL. Clinicoetiological profile of neonatal seizures in a tertiary care hospital. Indian J Child Health. 2017;4(4):587–590.
19. Lim SJ, Jun JK, Youn YA, et al. Follow up of full term neonatal seizures: prognostic factors for neuro developmental sequelae. Neonatal Med. 2013;20(1):97–105. doi:10.5385/nm.2013.20.1.97
20. Moayedi AR, Zakeri S, Moayedi F. Neonatal seizure: etiology and type. Iran J Child Neurol. 2007;1:23–26.
21. Iype M, Prasad M, Nair PM, Geetha S, Kailas L. The newborn with a seizures-a follow-up study. Indian Pediatr. 2008;45(9):749–752.
22. Soni A, Sabarawal RK, Amita K. Clinical profile of seizures in neonatal intensive care unit.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
