Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 10
Ethiopian health care professionals’ knowledge, attitude, and interests toward pharmacogenomics
Authors Abdela OA , Bhagavathula AS , Gebreyohannes EA , Tegegn HG
Received 1 July 2017
Accepted for publication 31 October 2017
Published 5 December 2017 Volume 2017:10 Pages 279—285
DOI https://doi.org/10.2147/PGPM.S145336
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Martin Bluth
Ousman Abubeker Abdela, Akshaya Srikanth Bhagavathula, Eyob Alemayehu Gebreyohannes, Henok Getachew Tegegn
Department of Clinical Pharmacy, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Pharmacogenomics is a field of science which studies the impact of inheritance on individual variation in medication therapy response.
Aim: We assessed healthcare professionals’ knowledge, attitude, and interest toward pharmacogenomics.
Methods: A cross-sectional survey was conducted using a 32-item questionnaire among physicians, nurses, and pharmacists who were working at the University of Gondar Referral and Teaching Hospital in northwest Ethiopia. Descriptive statistics was applied, and the categorical variables were summarized as frequency and percentages. An analysis of variance (ANOVA) test was performed to compare mean scores among health professionals. A p-value of <0.05 was considered as statistically significant.
Results: Of 292 health professionals who responded, the majority were male (60%) and the mean age of study participants was 27.00 (±4.85 SD) years. The mean knowledge scores of all participants, pharmacists, physicians, and nurses were 2.343±1.109, 2.671±1.059, 2.375±1.093, and 2.173±1.110, respectively. Based on the ANOVA test, a statistically significant difference was noted in mean knowledge score between pharmacists and nurses (p=0.002). More than two-thirds (67.33%) of nurses, 42.86% of pharmacists, and 40.27% of physicians who participated did not know that genetic variations can account for as much as 95% of the variability in drug disposition and effects. The ability to accurately apply their knowledge to drug therapy selection, dosing, or monitoring parameter was reported by 35.3% of the participants. More than two-thirds (69.2%) of participants thought that pharmacogenomic testing will allow the identification of the right drug with less side effects. Most of the participants (83.2%) also requested to have training on pharmacogenomics.
Conclusion: Participants showed limited knowledge, but they had positive attitude toward pharmacogenomics. Educational programs focusing on pharmacogenomic testing and its clinical application need to be emphasized.
Keywords: pharmacogenomics, genetics, personalized medicine, Gondar University Referral and Teaching Hospital, Gondar
Introduction
Differences in response to medication therapy among individuals have been explained largely in terms of variations in weight, renal function, and age among patients or due to drug–drug interaction. In addition to these factors, pharmacogenetics is also one of the determinants of medication therapy variability.1 In other words, one particular medication therapy can be effective but cause severe side effect in a group of patients while resulting in no response in terms of either toxicity or the intended therapeutic effect in others. Differences in individuals’ genetic makeup are found to be the major reason for this discrepancy and account for an estimated 20–95% of variations in medication disposition and effect.2 Pharmacogenomics is a field of science which studies the impact of inheritance on individual variation in medication therapy response.3,4 Currently, more than 100 medications are identified by the US FDA to have variable responses among individuals with certain genetic variations and hence are made to be labeled with pharmacogenomic information.4 This information can aid the prescribers about the potential events and also helps to utilize genetic information during the therapeutic decision-making process.5
Many health professionals are not competent enough in the field of pharmacogenomics, even though results from different studies promote pharmacogenomic practice and education. They continue to lack confidence and education in this field.4 If the concept of pharmacogenomic science is to be translated into clinical practice, all those involved in health care service including physicians, nurses, and pharmacists need to be educated well about pharmacogenomics.3
Despite the fact that pharmacogenomic testing and application of the information will have positive impact on the treatment of diseases, gaps are documented with respect to knowledge and attitude toward pharmacogenomics among health care providers even in developed countries.4 In Ethiopia, studies addressing such issues were not done at all. This research aimed at disclosing the knowledge, attitude, and interest of health care providers at the University of Gondar (UOG) Referral and Teaching Hospital toward pharmacogenomics.
Methods
An institutional-based cross-sectional study was conducted among health professionals including nurses, pharmacists, and physicians together with graduating students from nursing, pharmacy, and medicine department who were at their final-year clinical attachment at the UOG Referral and Teaching Hospital from April 1 to May 30, 2016. The hospital is a 550-bedded teaching hospital located in northwest Ethiopia 750 km away from the capital city, Addis Ababa. According to data from human resources office of the institution, more than 820 health professionals composed of physicians, nurses, pharmacists, laboratory technologists anesthetists, and radiographers were actively engaged in health care service. In addition, graduating class students of the respected departments were also actively involved in the process of health care provision. The hospital has 14 wards in 5 inpatient departments together with 14 different units for outpatient services.
Source and study population
All pharmacists, nurses, medical doctors, and graduating class students from nursing, pharmacy, and medicine departments at the UOG Referral and Teaching Hospital were our source population, whereas those pharmacists, nurses, medical doctors, and graduating class students from nursing, pharmacy, and medicine departments at the UOG Referral and Teaching Hospital who were available during the study period were our study population.
Inclusion and exclusion criteria
All Ethiopian nurses, medical doctors, pharmacists, and graduating class students from these disciplines of both genders working at the UOG Referral and Teaching Hospital were included, whereas those who were unwilling to return the questionnaire on time were excluded.
Survey questionnaire
We used a survey questionnaire employed by a previous research done among Jordanian pharmacists after securing permission to reuse it with little modification from the corresponding author.6 The obtained questionnaire was pretested among 20 randomly selected health care providers for reliability and validity. No language problems and corrections were encountered. The survey questionnaire was then distributed during a face-to-face interview, and participants were allowed to fill the survey questionnaire during their leisure time.
The survey questionnaire consisted of a total of 32 questions in 5 sections. Section 1 included questions related to the sociodemographic information (9 items). Section 2 had questions about their general pharmacogenomic knowledge (5 items; true, false, or I don’t know), and self-assessed knowledge (4 items). Section 3 involved questions on attitude toward pharmacogenomic testing (6 items) which was assessed using a 5-point Likert scale (strongly agree to strongly disagree). Section 4 had questions regarding future expectations about pharmacogenomic testing (4 items; strongly agree to strongly disagree). The final section included 4 questions concerned regarding pharmacogenomic education (the questionnaire is available on request to the corresponding author).
Ethical considerations
The study protocol was approved by the institutional ethical committee from the School of Pharmacy, UOG. Verbal consent of willingness to fill the questionnaires was obtained from the participants, and contact information of the researchers was provided. Participation in the survey was voluntary, and no compensation was provided. Confidentiality of the data was maintained by not disclosing any personal details of the study participants.
Statistical analysis
The obtained data were checked for accuracy of the information provided, and then the data were entered into Statistical Package of Social Sciences program version 22.0 for analysis. Descriptive statistics was applied, and the categorical variables were summarized as frequencies and percentages. The continuous variables were expressed as means and SD. Knowledge score was calculated for the 5 questions by giving 1 point for correct answers and no point for wrong or “I don’t know” answer. Analysis-of-variance (ANOVA) test was performed to compare mean scores among health professionals. A p-value of less than 0.05 was considered as statistically significant.
Results
Sociodemographic characteristics of study group
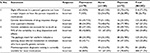
The characteristics of 292 survey participants are summarized in Table 1. Of the respondents, approximately 60% were male with a mean (SD) age of 27.00 (±4.85) years and were single (67.1%), from orthodox Christian religion (65.1%), and with an average monthly income of 2100–5077 Ethiopian Birr. More than half of the health professionals were nurses (51.3%), with BSc qualification (30.5%), and having an average of 0–3 years of work experience (42.5%).
  | Table 1 Sociodemographic characteristics of study participants at the University of Gondar, April 1–May 30, 2016 (N=292) Note: 1 US$=23 ETB. Abbreviations: ETB, Ethiopian Birr. |
Assessment of general knowledge of pharmacogenomics
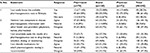
Using ANOVA, the mean knowledge score of all participants was found to be relatively low (2.343±1.109). The mean knowledge scores of pharmacists, physicians, and nurses were 2.671±1.059, 2.375±1.093, and 2.173±1.110, respectively. There was statistically significant difference in knowledge between pharmacists and nurses (p=0.002). Homogeneity of variances was checked using Levene’s test (p=0.699). While almost three-fourth of study participants (73.29%) knew that slight difference in a person’s genome can have a major impact on how the person responds to medications, 71.3% of participants did not know that pharmacogenomic diagnostic testing is currently available for most medications.
A significant knowledge gap between the health professionals was noticed. For instance, 90% of the pharmacists correctly answered for the statement “slight differences in genome can have a major impact on medication outcomes” compared to 73.6% of the physicians and 65.3% of the nurses. Similarly, 67.33% of the nurses, 42.86% of the pharmacists, and 40.27% of the physicians participated did not know that genetic variations can account for as much as 95% of the variability in drug disposition and effects (Table 2).
  | Table 2 General pharmacogenomic knowledge of health professionals at the University of Gondar referral hospital, April 1–May 30, 2016 (N=292) |
Self-assessed knowledge of pharmacogenomics
Less than half of the respondents (43.1%) thought that they were capable of discussing pharmacogenomic information with other health care providers. The ability to accurately apply their knowledge to drug therapy selection, dosing, or monitoring parameter was reported by 35.3% of the participants, whereas 39.4% claimed that they can identify which medications require pharmacogenetic testing (Table 3).
  | Table 3 Self-assessed knowledge about pharmacogenetic testing at the University of Gondar referral hospital, April 1–May 30, 2016 |
Attitude toward pharmacogenomic testing
The majority of participants agreed that pharmacogenomic testing would be associated with benefits such as decreased adverse events, optimized drug dosing, and improved efficacy. More than two-third (67.1%) of the pharmacists agreed that pharmacogenomics is suitable for their practice setting compared to 48% of the nurses and 47.2% of the physicians (Table 4).
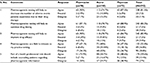  | Table 4 Attitude of health professionals toward pharmacogenomic testing at the University of Gondar referral hospital, April 1–May 30, 2016 |
Future expectations about pharmacogenomics testing
The majority of health professionals were hopeful about the future of pharmacogenomic testing. Around 66.8% thought that pharmacogenomic testing will prevent prescribing the wrong type of medicine or the wrong dose, and 69.2% thought that pharmacogenomic testing will allow identifying the right drug with less side effects (Figure 1).
  | Figure 1 Percentage of responses of health professionals regarding future expectations about pharmacogenomic testing. |
Pharmacogenomic education
Regarding pharmacogenomic education in Ethiopia, one-third (34.2%) of the participants disagreed and 38 (13.0%) strongly disagreed that pharmacogenomics was a fundamental part of college curriculum and/or training. In addition, majority of the participants either agreed (38.0%) or strongly agreed (22.3%) that health professionals should be required to have some knowledge of pharmacogenomics. Further, participants were also asked regarding access to pharmacogenomic information; 45% of the participants believed that all professionals should have access to pharmacogenomic information. Most of the participants (83.2%) also requested to have training on pharmacogenomics.
Discussion
Pharmacogenomics offers a great promise to better understand the patients’ genetic risk and drug response to improve therapeutic outcomes. It has also generated important additional clinical information related to the disease and drugs in the past 50 years. However, integrating the pharmacogenomic knowledge in clinical practice is still a challenge. It is important for all health professionals (doctors, nurses, and pharmacists) to use pharmacogenomic information for optimal medication use.
To the best of our knowledge, however, this is the first survey from sub-Saharan Africa which investigated the health professionals’ knowledge, attitude, and their interest regarding pharmacogenomics. We identified a study from Ghana that investigated the knowledge of pharmacogenomics among health professionals7 and another study from Nigeria that assessed the knowledge and perception of pharmacogenomics among health professionals.8 Our survey data showed that majority of participants were aware about pharmacogenomics and its importance in various areas of clinical practice. These findings were consistent with results from other surveys assessing the pharmacogenomic knowledge among health professionals.7–16 Forty-four (61%) physicians, however, did not think that they are competent enough to discuss the patients’ pharmacogenomic information with other health professionals. This might be due to lack of integration of pharmacogenomics in their medical curriculum and also information gained might be self-directed learning from their colleagues or through internet that may lead to an unequal standard of practice.
When we looked at the attitude toward the pharmacogenomics, all the participants showed a positive attitude. For instance, all the health professionals opinioned that the pharmacogenomic testing might help to decrease the adverse events that occur due to drug therapy and also agreed that the testing will help to optimize the drug dosing and improve drug efficacy. However, there were little discrepancies with respect to the attitude of physicians and nurses toward admitting pharmacogenomics as a field of their practice setting. Similar findings were noticed in other studies where health care students and professionals considered pharmacogenomics as an important area of clinical practice; however, they expressed that it has not been considered an important part in their curriculum.4,17,18 This emphasizes the need of integrating pharmacogenomics into the curriculum and providing them with sufficient training in this area for the readiness of our future medical professionals to practice. The discrepancies can also be explained in terms of the large number of nurse responders (almost twice) compared to physicians in our study which can alter the result noticeably.
The overall rate of future expectations to order any pharmacogenomic testing was moderate; it was reported in our study that more than 50% of the health professionals like to order pharmacogenomic testing to provide drug with less side effects. Previous studies revealed that doctors had low interest to practice and poor adoption.4,10–19 For instance, a study from the US reported that only 12.9% of the physicians ordered the pharmacogenomic test while 70% reported that they never order any pharmacogenomic testing.9 Contradictorily, 2 studies reported around 30.2–79.6% had ordered pharmacogenomic testing at least once a year.10,20 Our results point to the need for resources that can assist health professionals to make them aware of the genetic variations that could result in a patient’s suboptimal response to a drug.
The availability of pharmacogenomic technologies is also an important consideration for ordering a pharmacogenomic test in Ethiopia. Currently, pharmacogenomic technologies are not available in Ethiopia, and hence, pharmacogenetic tests are not being practiced. However, more than half of the participants were ready to order pharmacogenetic tests if necessary when the technology is available. With pharmacogenomic testing expected to come into picture in the country in the near future, this study provided baseline data on the health professionals’ knowledge and attitude toward pharmacogenomic testing.
Despite the outstanding amount of evidence promoting the pharmacogenomic education in several developing countries, pharmacogenomic or genomic education or training is not considered in their universities. This was already highlighted by our study participants as yet pharmacogenomics subject is not included in their curriculum and no training is provided. In our study, majority of health professionals were hopeful about the future of pharmacogenomic education and practice in Ethiopia. Providing solid understanding of pharmacogenomics to all health professionals can prepare these competent practitioners for the concept of personalized medicine. Further, emphasis is needed to provide continuous medical education courses on pharmacogenomics for a better understanding of the importance and practice of pharmacogenomics in Ethiopia.
Limitations
We conducted this survey from a single center which may not be generalized to whole Ethiopia, and the health professionals included may not be a representative sample of all health professionals in Ethiopia. We relied on participants’ trust to evaluate their knowledge and attitude; some of the participants may have overestimated or underestimated their abilities while answering the survey questions which may lead to recall bias. In spite of these limitations, this is the first study to investigate the knowledge, attitude, and future expectations of health professionals about pharmacogenomics in Ethiopia.
Conclusion
Our findings provided baseline information on the knowledge, attitude, and interest toward pharmacogenomics among health professionals in the UOG College of Medicine and Health Sciences. The participants showed limited knowledge, but they had positive attitude toward pharmacogenomics. Educational programs focusing on pharmacogenomic testing and its clinical application are needed.
Acknowledgments
The authors would like to acknowledge Mr Asresaw Ebabu and Mr Nejb Sefa for their cooperation in collecting data. They are also thankful to health practitioners working at the University of Gondar for participation in the study.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Zembles T. An inservice program on pharmacogenetics to individualize drug therapy. Am J Pharm Educ. 2010;74(1):10. | ||
Crews KR, Hicks JK, Pui CH, Relling MV, Evans WE. Pharmacogenomics and individualized medicine: translating science into practice. Clin Pharmacol Ther. 2012;92(4):467–475. | ||
Wang L. Pharmacogenomics: a systems approach. Wiley Interdiscip Rev Syst Biol Med. 2010;2(1):3–22. | ||
Moen M, Lamba J. Assessment of healthcare students’ views on pharmacogenomics at the University of Minnesota. Pharmacogenomics. 2012;13(13):1537–1545. | ||
Owusu-Obeng A, Weitzel KW, Hatton RC, et al. Emerging roles for pharmacists in clinical implementation of pharmacogenomics. Pharmacotherapy. 2014;34(10):1102–1112. | ||
AlEjielat R, Ejielat Z, Andrawes S, Mhaidat NM. An evaluation of the knowledge, opinions, expectations and concerns toward pharmacogenomics among Jordanian pharmacists. Pers Med. 2016;13(2):143–154. | ||
Kudzi W, Addy BS, Dzudzor B. Knowledge of pharmacogenomics among healthcare professionals and faculty members of health training institutions in Ghana. Ghana Med J. 2015;49(1):50–56. | ||
Madadi P, Enato EFO, Babatunde EO. Perceptions of health care professionals towards pharmacogenomics in Nigeria: preliminary results. West Afr J Pharm. 2011;22(1):97–101. | ||
Stanek EJ, Sanders CL, Taber KA, et al. Adoption of pharmacogenomic testing by US physicians: results of a nationwide survey. Clin Pharmacol Ther. 2012;91(3):450–458. | ||
Haga SB, Burke W, Ginsburg GS, Mills R, Agans R. Primary care physicians’ knowledge of and experience with pharmacogenetic testing. Clin Gen. 2012;82(4):388–394. | ||
Dodson C. Knowledge and attitudes concerning pharmacogenomics among healthcare professionals. Pers Med. 2011;8(4):421–428. | ||
Taber KA, Dickinson BD. Pharmacogenomic knowledge gaps and educational resource needs among physicians in selected specialties. Pharmacogenomics Pers Med. 2014;7:145. | ||
Mai Y, Mitropoulou C, Papadopoulou XE, et al. Critical appraisal of the views of healthcare professionals with respect to pharmacogenomics and personalized medicine in Greece. Pers Med. 2014;11(1):15–26. | ||
Yau A, Aziz AB, Haque M. Knowledge, attitude and practice concerning pharmacogenomics among pharmacists: a systematic review. J Young Pharm. 2015;7(3):145. | ||
Selkirk CG, Weissman SM, Anderson A, Hulick PJ. Physicians’ preparedness for integration of genomic and pharmacogenetic testing into practice within a major healthcare system. Genet Test Mol Biomarkers. 2013;17(3):219–225. | ||
Bartlett MJ, Shephard EA. The integration and interpretation of pharmacogenomics – a comparative study between the United States of America and Europe: towards better health care. Drug Metab Pers Ther. 2016;31(2):91–96. | ||
Squassina A, Manchia M, Manolopoulos VG, et al. Realities and expectations of pharmacogenomics and personalized medicine: impact of translating genetic knowledge into clinical practice. Pharmacogenomics. 2010;11(8):1149–1167. | ||
Peterson JF, Field JR, Shi Y, et al. Attitudes of clinicians following large-scale pharmacogenomics implementation. Pharmacogenomics J. 2015;12(4):339–347. | ||
Klitzman R, Chung W, Marder K, et al. Attitudes and practices among internists concerning genetic testing. J Genet Couns. 2014;22(1):90–100. | ||
Shields AE, Blumenthal D, Weiss KB, Comstock CB, Currivan D, Lerman C. Barriers to translating emerging genetic research on smoking into clinical practice. Perspectives of primary care physicians. J Gen Intern Med. 2005;20(2):131–138. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
