Back to Journals » Therapeutics and Clinical Risk Management » Volume 16
Estimation of Risk Factors for Head Slippage Using a Head Clamp System. A Retrospective Study
Authors Sakakura K , Fujimoto A , Ichikawa N, Ishikawa E, Matsumura A, Enoki H, Okanishi T
Received 27 January 2020
Accepted for publication 15 March 2020
Published 25 March 2020 Volume 2020:16 Pages 189—194
DOI https://doi.org/10.2147/TCRM.S247402
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Kazuki Sakakura,1,2 Ayataka Fujimoto,1 Naoki Ichikawa,1 Eiichi Ishikawa,2 Akira Matsumura,2 Hideo Enoki,1 Tohru Okanishi1
1Comprehensive Epilepsy Center, Seirei Hamamatsu General Hospital, Hamamatsu, Shizuoka, Japan; 2Department of Neurosurgery, University of Tsukuba, Tsukuba, Ibaraki, Japan
Correspondence: Ayataka Fujimoto
Seirei Hamamatsu General Hospital, 2-12-12 Sumiyoshi, Nakaku, Hamamatsu, Shizuoka 430-8558, Japan
Tel +81-53-474-2222
Fax +81-53-475-7596
Email [email protected]
Background: Although complications have been associated with head clamp systems, few reports have described head slippage. The present study aimed to determine risk factors for head slippage and speculated that the position of head holder pins might be associated.
Patients and Methods: We reviewed medical records and compared the positions of the pinned heads of patients on fused preoperative and postoperative computerized tomography (CT) images. We measured the distance between corresponding head pins to determine head slippage. Age, sex, body weight, body mass index, surgical position, surgical duration, craniotomy volume, and the relationship between head pins and the nasion-inion (NI) line were statistically compared between patients with and without head slippage.
Results: Head slippage in 3 (10%) of 28 patients was significantly associated with the most caudal pin position (p < 0.001) and craniotomy volume (p = 0.036). Receiver operator characteristics curves indicated a cutoff of 4.5 cm from the NI line (sensitivity and specificity, 1.000 and 0.800, respectively).
Conclusion: Clamped heads can slip during surgical procedures. We found that one head pin should be located within 4.5 cm from the NI line to avoid head slippage.
Keywords: head movement, mayfield head clamp, intraoperative computed tomography, nasion-inion line, pinning
Introduction
Holders are used to immobilize the head during many neurosurgical procedures.1 Even if their immobilization ability is not guaranteed, they must be trusted during surgery for various periods. However, slight head movements do occur during surgical procedures. Not all neurosurgeons feel absolutely comfortable with pinned head fixation. In fact, the US Food and Drug Administration in 2016 urged caution with neurosurgical head holders due to slippage, based on reports of 1000 slippages with 700 injuries.2 Some reports have associated skull hematomas,3 fractures,4,5 air embolism,6 and asystole7 as complications of pinned head holders. However, the reasons for slippage have not been addressed and few reports have described head slippage, despite 700 associated injuries. This is probably due to difficulties with comparing pre-and post-operative head holder positions. We postulated that the pin position of the head holder might be associated with slippage. We, therefore, compared preoperative and postoperative computed tomography (CT) images of pinned head positions to determine risk factors associated with slippage.
Patients and Methods
Study Design and Ethics Approval
The Ethics Committee at Seirei Hamamatsu General Hospital approved the protocol of this retrospective, cross-sectional, observational, non-randomized study, which was designed in accordance with the principles of the Declaration of Helsinki (7th revision 2013). Participants were identified via a retrospective electronic chart review of patients treated between October 2015 and March 2019 at the Comprehensive Epilepsy Center, Seirei Hamamatsu General Hospital. Written, informed consent was obtained from all patients to publish their innominate data.
Patients
We reviewed the medical records of patients who underwent preoperative and postoperative CT in an operating room and fulfilled the following criteria: all CT images were acquired with the head clamped using a radiolucent carbon Mayfield three-pin head holder (Infinity XR2 Radiolucent System; Integra LifeSciences Services, Saint-Priest, France); the position of the head holder was not deliberately changed during procedures and the CT slice thickness was <1 mm. The heads of patients who weighed >50 or <50 kg were clamped with 60 and 40 lb of force, respectively.
Intraoperative CT
An internationally standardized point in the SOMATOM Definition AS64 Open scanner (Siemens AG, Munich, Germany) called the International Organization of Standardization (ISO) center represents the absolute reference point for neuronavigation. The camera of the neuronavigation system also detected the ISO center during CT, as well as a patient reference array, so head positions were automatically determined from CT images. Spatial errors theoretically do not exist between these structures.8 We applied this system without surface matching, using a touchless laser pointer for patient registration, and thus accurately measured head slippage.
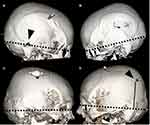
Measurement of Head Slippage as a Primary Outcome
We used the iPlan station of Cranial Surgical Planning software (Brainlab, AG, Munich, Germany) to fuse preoperative and postoperative CT images. We adjusted all angles of CT image slices to the nasion-inion (NI) line on the iPlan station. The thickness of each slice increased from 1 to 2.5 mm using this modification and they were automatically fused using an algorithm.9,10 After fusion, we measured the distance between the corresponding head pins and the height of the pins from the NI-plane. We referred to the maximal distance of pins that had slipped >2.5 mm among the three pins because distances <2.4 mm could not be measured due to the thickness of the CT slices.
Other Factors as Secondary Outcomes
We assessed age, sex, body weight (BW), body mass index (BMI), surgical position, surgical duration, and craniotomy volume, as well as the relationship between each head pin and the NI line of each patient.
Surgical duration was taken as the amount of elapsed time between acquisition of the first preoperative and the first postoperative iCT images with head clamped in the holder. We did not determine the period between skin incision and wound closure. Craniotomy volume was measured using the iPlan station.
Statistical Analysis
Age, sex, BW, BMI, and the craniotomy volume were assessed using univariate regression analyses to determine the influence of variables on slippage rates. Slippage rates and the sample sizes were too small for multivariate logistic regression analysis; therefore, we repeated univariate regression analysis as appropriate. The cutoff value was calculated from receiver operating characteristics (ROC) curves. Statistical significance was taken at p < 0.05. All data were statistically analyzed using Sigma Plot version 14 (Systat Software, San Jose, CA, USA).
Results
Clinical Information
Among 29 patients (male, n = 21; female, n = 8) who fulfilled the inclusion criteria, one was excluded to avoid bias because CT images from this patient could be manually fused, but not be automatically by the iPlan station. Table 1 describes the clinical information.
 |
Table 1 Clinical Information |
Head Slippage: Primary Outcome
Table 2 shows that the primary outcome of head slippage occurred in 3 (10%) patients. The distance between preoperative and postoperative slipped pins ranged from 2.5 to 10 mm. However, no complications were associated with head slippage in these patients.
 |
Table 2 Slippage Cases |
Representative Case 1
A 59-year-old male with a pituitary tumor underwent preoperative iCT for neuronavigation registration after general anesthesia. Complications associated with tumor removal and any other causes were evaluated by postoperative iCT. Preoperative and postoperative iCT images merged using iPlan showed that his head had slipped during the procedure (Figure 1).
Other Factors: Secondary Outcomes
Relationship Between Head Pins and NI Line
The most caudal head pin position was significantly associated with head slippage (p < 0.001; Figure 2) The ROC [Please consider that “ROC has already been defined” in page 7. It does not need to be defined again in the text.] curves indicated a cutoff of 4.5 cm (sensitivity and specificity, 1.000 and 0.800, respectively).
Risk Factors for Slippage
Table 3 shows that craniotomy volume was a significant risk factor for head slippage (p = 0.036), whereas age, sex, BW, BMI, surgical position and surgical duration were not.
 |
Table 3 Risk Factors for Slippage |
The ROC curves indicated a cutoff of 1.54 cm3 (sensitivity and specificity, 0.67 and 0.72, respectively).
Discussion
Head Slippage: Primary Outcome
We found that heads clamped with pins slipped at a frequency of 10% during surgery. We then statistically evaluated risk factors to eliminate such slippage. The most caudal pin above 4.5 cm from NI line was significant (p ≤ 0.001) with 1.000 sensitivity and 0.800 specificity. This means that one of the three pins should be located within 4.5 cm from the NI line to stabilize the clamp. A previous study found that the center of gravity is located at the middle of the NI line.11 This means that the head could slip more easily if the pins are inserted more superiorly, because they would be located further away from the center of gravity of the head.
The positioning of the Mayfield headrest represents the first surgical procedure in the operating room; newer neurosurgeons need to be educated about not only surgical skills,12 but also correct technique and the risks associated with intraoperative slippage.
Craniotomy Volume
A larger craniotomy volume was a risk factor for head slippage. A larger craniotomy often does not achieve satisfactory cosmetic results due to shifting.13 However, this outcome might be statistically paradoxical due to lower sensitivity and specificity than the cutoff of the NI-line. Nonetheless, this factor should be considered before patients with larger craniotomies are scheduled to undergo procedures that require immobilizing the head.
Study Limitations
The number of participants in this preliminary retrospective study at a single facility was small. The thickness of the axial image slices had to be increased from 1 to 2.5 mm to measure distances between the head pins. We should be able to show more details with thinner slices A prospective, multicenter trial with more participants and thinner slices is needed to confirm the present findings.
Conclusions
Clamped heads can slip during surgery. One head pin should be located within 4.5 cm of the NI line to avoid head slippage.
Highlights
- Measurement of head slippage with head clamp system
- Frequency of head slippage is 10%
- Head pin position is a risk factor for head slippage
Abbreviations
BMI, body mass index; BW, body weight; CT, computed tomography; ISO, International Organization of Standardization; NI, nasion-inion; ROC, receiver operating characteristics.
Acknowledgments
We are grateful to Dr. C. Inenaga and Dr. T. Tanaka for help with surgical procedures.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
No funding was received for this investigation.
Disclosure
None of the authors has any conflicts of interest to declare.
References
1. Goel A, Muzumdar DP, Phalke U. Head holder for microsurgical dissection. J Clin Neurosci. 2004;11(3):300–301. doi:10.1016/j.jocn.2003.09.009
2. Atteya MME, Raslan S, Elkallaf M, Soliman MS, AlQalla MA. A novel method for safe and accurate placement of the rocker pins of head immobilization devices utilizing a digital caliber phantom: technical note. Childs Nerv Syst. 2019;35(9):1599–1602. doi:10.1007/s00381-019-04216-x
3. Baerts WD, de Lange JJ, Booij LH, Broere G. Complications of the mayfield skull clamp. Anesthesiology. 1984;61(4):460–461. doi:10.1097/00000542-198410000-00017
4. Matouk CC, Ellis MJ, Kalia SK, Ginsberg HJ. Skull fracture secondary to application of a mayfield skull clamp in an adult patient: case report and review of the literature. Clin Neurol Neurosurg. 2012;114(6):776–778. doi:10.1016/j.clineuro.2011.12.036
5. Zaazoue MA, Bedewy M, Goumnerova LC. Complications of head immobilization devices in children: contact mechanics, and analysis of a single institutional experience. Neurosurgery. 2018;82(5):678–685. doi:10.1093/neuros/nyx315
6. Grinberg F, Slaughter TF, McGrath BJ. Probable venous air embolism associated with removal of the mayfield skull clamp. Anesth Analg. 1995;80(5):1049–1050. doi:10.1097/00000539-199505000-00036
7. Miyoshi H, Nakamura R, Hamada H. Asystole following skull clamp to Chiari malformation. J Anesth. 2015;29(2):317. doi:10.1007/s00540-014-1890-y
8. Fujimoto A, Okanishi T, Kanai S, Sato K, Nishimura M, Enoki H. Neuronavigation-guided Frameless Stereoelectroencephalography (SEEG). Neurol Med Chir (Tokyo). 2017;57(9):496–502. doi:10.2176/nmc.tn.2017-0110
9. Riva M, Hiepe P, Frommert M, et al. Intraoperative computed tomography and finite element modelling for multimodal image fusion in brain surgery. Oper Neurosurg (Hagerstown). 2019. doi:10.1093/ons/opz196
10. Jin JY, Yin FF, Tenn SE, Medin PM, Solberg TD. Use of the BrainLAB ExacTrac X-ray 6D system in image-guided radiotherapy. Med Dosim. 2008;33(2):124–134. doi:10.1016/j.meddos.2008.02.005
11. Vital JM, Senegas J. Anatomical bases of the study of the constraints to which the cervical spine is subject in the sagittal plane. A study of the center of gravity of the head. Surg Radiol Anat. 1986;8(3):169–173. doi:10.1007/BF02427845
12. Lemole GM
13. Unterhofer C, Wipplinger C, Verius M, Recheis W, Thome C, Ortler M. Reconstruction of large cranial defects with poly-methyl-methacrylate (PMMA) using a rapid prototyping model and a new technique for intraoperative implant modeling. Neurol Neurochir Pol. 2017;51(3):214–220. doi:10.1016/j.pjnns.2017.02.007
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.