Back to Journals » Risk Management and Healthcare Policy » Volume 13
Estimation of Gestational Age Using Neonatal Anatomical Anthropometric Parameters in Dessie Referral Hospital, Northeast Ethiopia
Authors Tiruneh C
Received 15 September 2020
Accepted for publication 17 November 2020
Published 15 December 2020 Volume 2020:13 Pages 3021—3029
DOI https://doi.org/10.2147/RMHP.S280682
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Chalachew Tiruneh
Department of Anatomy, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
Correspondence: Chalachew Tiruneh Po Box: 1145 Tel +251920245474
Email [email protected]
Introduction: Estimation of gestational age is a key for the identification of a given low birth weight neonate is either preterm or growth retarded.
Objective: To estimate gestational age from neonatal anatomical anthropometric parameters in Dessie Referral Hospital, Ethiopia.
Methods: Institutional-based cross-sectional study design was employed in Dessie Referral Hospital from October 2019 to April 2020, with 424 consecutively live-born of 28– 42 weeks of gestation. After considering the inclusion criteria, neonatal anthropometric parameters were measured within 3 days of birth. Foot length, hand length, mid-upper arm circumference, head circumference, crown-heel length, intermammary distance, umbilical nipple distance, and birth weight were measured and summarized using descriptive statistics, and the power of association was evaluated using correlation analysis. Regression equations of gestational age (GA) in completed weeks with anthropometric parameters were formulated using simple and multiple linear regression analysis.
Results: Except for hand length, all other neonatal anthropometric measurements were positively correlated with GA in completed weeks at p< 0.05. Anthropometric parameters individually, mid-upper arm circumference (MUAC) and BW (birth weight) were correlated well with GA at correlation coefficient (r) of 0.406 and 0.334, respectively. Regression formula was formulated as GA (weeks) = 26.12+ [1.11×MUAC (cm)] and GA (Weeks) = 33.19 + [1.53×BW (kg)]. Multiple regression contributed correlation with GA and used for prediction of GA as GA (weeks) = 28.12 – [0.393×HL (cm)] + [1.07×BW (kg)] + [0.87×MUAC (cm)] (r= 0.458).
Conclusion: The overall relative better correlation for prediction of GA, alone and in combination, is found by combined parameters (HL, MUAC, and BW). The relatively better individual anthropometric parameter for GA assessment is MUAC. Hence, using this neonatal parameter as a prediction of gestational age, the death of neonate due to preterm can be minimized.
Keywords: anatomical parameters, gestational age, neonates, Dessie Referral Hospital
Introduction
Gestational age estimation is vital for medical besides numerous public health functions, including the assessment of intrauterine growth curves and related tricky conditions in populations, such as identifying whether infants of given low birth weight are either preterm or growth-retarded, the adjustment for prematurity when assessing gross motor milestone attainment, and determining at-risk status for potential developmental delay related to target populations in need of follow up and intervention services.1
Indeed, gestational age (GA) denotes the length of time between conception and delivery. Since the timing of conception cannot be easily ascertained, GA is commonly estimated as the difference between the first day of the last normal menstrual period (LNMP) and the delivery date. And also early pregnancy ultrasound is considered as the gold standard for GA assessment. However, in low-resource settings, GA estimation is difficult because of the late for ANC, challenges of LNMP recall because of hormonal contraceptive usage or maternal diseases and low literacy, and unavailability of ultrasonography.2,3
Worldwide, approximately 15 million infants (11%) are born preterm each year.4 Preterm birth is responsible for 28% of all neonatal deaths, and the second leading cause of death in children under 5 years of age.5,6 The burden of preterm birth is higher in low and middle-income countries (LMICs), where more than 90% of the global 15 million preterm deliveries occur each year.7 As stated by the United Nations, mortality estimate in 2013, Ethiopia has 28 per 1000 live births neonatal mortality rate. Even though there is an achievement observed in the reduction of neonatal mortality by 48%, still neonatal mortality is high.8 In 2017 alone, an estimated 6.3 million children and young adolescents died, mostly from preventable causes. Of all the cases, about 2.5 million neonatal deaths occurred before celebrating their 28th days. Among children and young adolescents, the risk of dying was highest in the first month of life with an average rate of 18 deaths per 1000 live births.9
According to the study in Ghana, one of the contributing factor to neonatal mortality is the duration of pregnancy.10 Thus, gestational age estimation at birth and identification and prompt care of premature babies provides us with an opportunity to not only reduce neonatal mortality but also the under-five mortality rate. Gestational age and birth weight as predicted from the last menstrual period have traditionally been used as strong indicators of prematurity and neonatal death.11
A reliable model development to estimate the fetal weight at a given gestational age from maternal and fetus parameters would facilitate intervention plans for health care providers to prevent the risk of low birth weight delivery.12–14 This model development at different gestational ages is crucial for developing countries where there is limited access to ultrasound machines and skilled personnel. However, it is difficult to conduct a study in such countries due to the scarcity of resources.
So, the above problems specify that there are needs for another model development at delivery which is a new simple, cost-effective, reliable, easy to use and uniform method for estimation of gestational age that can be used in developing countries for immediate identification of preterm neonate and referral of preterm neonates, as well as the delivery of potentially life-saving management. Thus, alternative measurements of neonates at the time of delivery may have a good correlation with gestational age in new-born. Neonatal foot length, hand length, mid-upper arm circumference, umbilical nipple distance, intermammary distance, crown-heel length, and birth weight have been studied for their correlation with gestational age. All of these neonatal parameters can be measured with simple and easily available equipment “measuring tape” and does not require any special training for use. Therefore, the study was aimed 1) to investigate the relationship between gestational age and the above neonatal anatomical parameters after delivery, 2) to find the better parameter for gestational age assessment from this neonatal anatomical anthropometric parameter alone or in combination, 3) to develop regression models to predict gestational age from these neonatal anatomical anthropometric parameters.
Materials and Methods
Study Area and Period
This institutional-based prospective cross-sectional study was carried out from October 2019 to April 2020 at Dessie Referral Hospital in the gynecology and obstetrics department. The hospital is found in Dessie town, located 401 km from Addis Ababa, the capital city of Ethiopia, and 478 km far from Bahir Dar, the capital city of Amhara regional state. The hospital serves about 2.4 million peoples of South Wollo and neighboring zones. It has more than five wards including the obstetrics and gynecology ward. The hospital’s monthly delivery report is above 500 mothers.
Source and Study Population
The source population for this study was all neonates who were delivered at Dessie Referral Hospital from October 2019 to April 2020, whereas all alive delivered neonates who fulfill inclusive criteria were the study population.
Sample Size Determination and Sampling Procedure
To date, there are no such published reports on the estimation of gestational age from neonatal anatomical parameters. Therefore, the minimum required sample size for this study was determined using the single population proportion formula by taking into consideration a prevalence 50% (p=0.5%), level of significance 5% (α = 0.05), Zα/2 =1.96, and margin of error 5% (d = 0.05). Finally, a 10% non-response rate was added, then, the total sample size required for this study was set at 424.
After checking the medical card of cases and taking informed consent from the parents, based on the inclusive and exclusive criteria of the study, a purposive sampling technique was employed until the required sample size was achieved.
Eligibility Criterion
Inclusion Criteria
Four hundred twenty-four (424) consecutively alive delivered neonates within 3 days of life and the calculated gestational age ranged from 28 to 42 weeks were included in the study.
Exclusion Criteria
Exclusion criteria consisted of mothers not knowing LMP exactly (i.e. women having irregular menstrual cycle before pregnancy), twin neonates, newborn with gross congenital anomalies, severe perinatal asphyxia, chronic maternal disease – hypertension, diabetes mellitus, cardiac disease and severe anemia, TORCH infections positive mothers, obstetrical complications known to compromise fetal growth – eclampsia, smoking history, alcohol consumption or drug abuse.
Anthropometry Equipment
- Weight scale and
- Flexible, non-elastic measuring tape meter
Data Collection Tools and Procedures
A properly designed checklist was used to collect relevant information. The tool was adapted from different peer-reviewed literatures. It contains written consents, socio-demographic variables, gestational age of the mother just at delivery, and neonatal anatomical parameters which include head circumference (HC), crown-heel length (CHL), mid-upper arm circumference (MUAC), foot length (FL), hand length (HL), intermammary distance (IMD), umbilical nipple distance (UND), and birth weight (BW).
The medical records were reviewed for early findings and the neonates were checked by physical examination for their normal appearance. Following confirmation of the normal appearance of a newborn by physical examination, the study subjects were recruited to the study. The neonates were placed in a supine position. Neonatal anatomical parameters were measured by using a non-elastic measuring tape meter to the nearest of 0.1 cm. Birth weight was measured by a balanced neonatal weight scale in kilograms (kg). The GA of the study participant was calculated from the history sheets by the use of “Naegele’s formula” (i.e. count back 3 months from the first day of the LNMP, add 1 year plus 7 days).
Crown-heel length of the neonate was measured from the highest point on the head in the mid-sagittal plane (vertex) of the skull to the heel of the foot (supine position).15
Head circumference was measured by non-elastic measuring tape meter which encircles the head just above the superciliary arch on the anterior aspect, just above the auricle on the lateral aspect and, at the level of external occipital protuberance on the posterior aspect.16
Foot length was measured with a non-elastic measuring tape meter as the maximum length between the most prominent posterior point of heel and the tip of hallux and the tip of the second toe if it was larger than the hallux.18 Hand length was measured from the distance between the heel of the hand and the tip of the middle finger.17 Both foot length and hand length were measured from the right side of the body.
Umbilical nipple distance was measured between the 12 o’clock positions of the rim of the umbilicus to the right nipple.17 Intermammary distance was measured between the distances of the nipples at the end of expiration.
Mid-upper arm circumference: it was measured at midpoint circumference of humerus between the acromion end of clavicle and olecranon process of the ulna. The right side of the arm was measured.
Data Quality Control
The data were collected by three Bachelor of Science in Midwifery profession who works in the delivery room. To maintain data quality, training on neonatal anatomical anthropometry measurements and measurement errors was given for the data collectors. The data collection was carried out within 3 days of the postpartum period. All measurements were taken by the trained tester/measurer. A properly designed data collection material was prepared. Anatomical parameters were measured by non-stretchable tape and recorded to the nearest 0.1 cm. To maintain reproducibility, each measurement was repeated 2 times and the average was recorded. The principal investigator had carried out day-to-day supervision during the data collection period, and the collected data were checked for its completeness and consistency.
Data Processing and Analysis
The collected data were checked for completeness, accuracy, and clarity before analysis. The data were entered in EPI data version 3.1 and exported to statistical package for social sciences (SPSS) version 23 for analysis. Data were cleaned and edited before analysis. The normality test was carried out to determine the normality of the samples and it was normally distributed. The correlation among different neonatal anatomical anthropometric measurements with gestational age was tested. A P-value of less than 0.05 was considered statistically significant. Simple and multiple linear regression analyses were done. To determine what combination gives the most accurate predictions of GA, multiple regression analysis was carried out using backward elimination procedures. Linear regression equations were derived as a predictive model for gestational age from neonatal anatomical parametric measurements. The multicollinearity between the independent variable was assessed using variance inflation factor (VIF) and it was less than 10. The fitness of regression models was assessed using coefficients of determination (r2) and residual plots. The predictive accuracy of the regression models was also evaluated using the mean absolute error (MAE) and mean average percentage error (MAPE). Finally, the data were presented by using statements, tables, charts, and graphs.
Ethical Considerations
Ethical clearance was obtained from the institutional research review board of Wollo University. A supporting letter was sent to Dessie Referral Hospital and permission was obtained from the hospital manager to implement the study. The aim and objectives of the study were clarified to each study participant’s parent/legal guardians. The verbal informed consent was obtained for participant’s parents/legal guardians who could not able to read and write, and the verbally informed consent process was approved by the DRERC of Wollo University. Written informed consent was obtained from each participant’s parent/guardians who could able to read and write. Privacy was kept by taking the data anonymously and also the participant’s parent/guardians had the right to be excluded from the study if they were not voluntary to participate.
Results
Descriptive Statistics of Sociodemographic Variables
A total of 424 women who gave alive birth had participated in this study. About 262 (61.8%) and 162 (38.2%) study participants’ parents came from urban and rural, respectively. The age of them was in the range of 16–38 with a mean of 26.8 (±5.2). The majority of the newborns were delivered at term 360 (84.9%) followed by preterm 64 (15.1%), of which 216 (50.9%) of them were males and 208 (49.1%) were females. The gestational age of newborns was in the range of 31–42 weeks with a mean of 38.1 (±1.8). The proportions of cases in each gestational week were not evenly divided. The largest proportions of delivery occurred at 38 weeks followed by 39 weeks, which accounted for 134 (31.6%) and 98 (23.1%) respectively. Conversely, the smallest proportions of delivery occurred at 42 weeks 1 (0.2%). The status of the newborn was term 360 (84.9%) followed by preterm 64 (15.1%) (Table 1 and Figures 1 and 2).
 |
Table 1 Socio-Demographic Characteristics of the Study Participants in Dessie Referral Hospital, Northeast Ethiopia |
 |
Figure 1 Distribution of the study samples for each age of the woman in Dessie Referral Hospital, Northeast Ethiopia. |
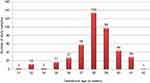 |
Figure 2 Break-up of the study sample for each gestational age in Dessie Referral Hospital, Northeast Ethiopia. |
Descriptive Statistics of Gestational Age and Anatomical Anthropometric Parameters of Neonates
Descriptive statistics of neonatal anatomical measurements of study participants were presented in Table 2. It was observed that the different neonatal anatomical parameters had different measurement quantities. Additionally, the birth weight of the study subjects ranged from 2.2 kg to 4.5 kg with a mean birth weight of 3.2 (±0.4 kg).
 |
Table 2 Descriptive Statistics of the Gestational Age of the Woman and Anatomical Anthropometric Parameters of the Neonate in Dessie Referral Hospital, Northeast Ethiopia |
Correlation Between Gestational Age and Neonatal Anatomical Anthropometric Measurements
Pearson’s correlation coefficient (r) between gestational age and neonatal anatomical anthropometric measurements are provided in Table 3. The r-value between gestational age and neonatal anatomical anthropometric parameters ranged from −0.018 to 0.406. Except for the hand length, all other neonatal anatomical anthropometric parameters had a positive statistically significant correlation with gestational age (p < 0.05). The highest correlation was observed on mid-upper arm circumference (r=0.406). On the other hand, the lowest correlation was detected on hand length (r= −0.018) and this parameter was not significantly correlated (p > 0.05). It also explained that birth weight had a positive significant correlation (r=0.334, p<0.05) (Table 3).
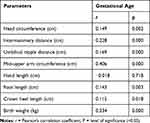 |
Table 3 Correlation Between Gestational Age and Neonatal Anthropometric Parameters in Dessie Referral Hospital, Northeast Ethiopia |
Gestational Age Estimation from Neonatal Anatomical Anthropometric Measurements
Simple and multiple linear regression analyses were conducted to estimate GA from neonatal anatomical measurements. It was evident that the relative maximum significant correlation coefficient was obtained when all anthropometric parameters were entered in a multiple linear regression analysis. To determine what combination gives the most accurate predictions of GA, a backward elimination procedure was conducted. In this method of analysis, the birth weight, hand length, and MUAC had p<0.1 and they were the best predictor variables, whereas the HC, IMD, UND, CHL, and FL were eliminated (p> 0.1). As a result, a relatively better significant correlation coefficient was obtained on (MUAC, BW, and HL) (r=0.458) followed by a simple linear regression model entry, MUAC (r=0.406). Hence, a relative better predictor regression equation for gestational age was formulated as GA (in weeks) = 28.12 – [0.393×HL (cm)] + [1.07×BW (kg)] + [0.87×MUAC (cm)] and GA (in weeks) = 26.12+ [1.11×MUAC (cm)] (Table 4).
 |
Table 4 Gestational Age Estimation from Neonatal Anthropometric Parameters in Dessie Referral Hospital, Northeast Ethiopia |
Predictive Accuracy Measurements of the Formulated Regression Models
The predictive capacity of the formulated regression models was measured using mean absolute error (MAE) and mean average percentage error (MAPE). These predictive accuracy measurements revealed that all of the proposed models had the potential to estimate the gestational age. Based on MAE, model (8) which was formulated using a combination of MUAC, BW, and HL had a better predictive accuracy (MAE= 1.21) followed by MUAC parameter model (4) (MAE=1.23). Furthermore, the models’ predictive accuracy using MAPE, indicated that the error of using the model (8) was (MAPE=3.27%) followed by the model (4) (MAPE=3.31%) (Table 5).
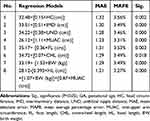 |
Table 5 Assessment of the Prediction Accuracy of the Formulated Regression Models in Dessie Referral Hospital, Northeast Ethiopia |
Discussion
This study was intended to estimate gestational age from neonatal anatomical anthropometric measurements including HC, CHL, MUAC, HL, FL, IMD, UND, and BW in 424 consecutively delivered neonates of Dessie Referral Hospital. The study was conducted in the gynecology and obstetrics department of the postpartum ward within 72 hours of delivery.
Though prematurity is a major determinant of neonatal survival, there was no study finding entitled on gestational age estimation from neonatal anatomical anthropometry in developing country including Ethiopia. These countries rely on LNMP for the determination of gestational age to assess the delivered neonate whether they were term or preterm. However, LNMP may not be recalled due to irregularity, hormonal contraceptive usage, and low literacy in low-income countries. As a result, this study might have significance for the early management of prematurity and then reducing under-five mortality rates.
In the current study, head circumference, crown-heel length, mid-upper arm circumference, foot length, intermammary distance, umbilical nipple distance, and birth weight had a positive significant correlation with gestational age. This finding was in agreement with a study conducted in India by Thawani et al.17 Furthermore, hand length had an insignificant correlation in the current study with gestational age as compared to the study conducted by Thawani et al. This discrepancy may be due to differences in sample size used. Moreover, this study had in agreement with a study conducted by Yadav et al in India,19 which explained that birth weight, foot length, head circumference, and crown-heel length had a positive correlation with gestational age.
Concerning the strength of association in the current study, mid-upper arm circumference (r=0.406) had a relatively strong correlation with gestational age on complete weeks followed by birth weight (r=0.334). This finding was inconsistent with a study conducted by Yadav et al,19 where foot length (r=0.878, p<0.0001) had a maximum correlation followed by birth weight (r=0.799). These contradictions might be due to the demographic profile and sample size differences. Another study conducted by Das, et al,20 HC had a strong association (r=0.863) followed by CHL (r= 0.859). This explains that the inconsistency was demonstrated to the use of only two variables for estimation of the gestational age as compared to the current study.
Contemporarily, this study discussed the regression equation was formulated in complete weeks and found that a relatively strong association was obtained in combination of (MUAC, BW, HL) (r=0.458), and formulated as GA in weeks= 28.12 - [0.393×HL (cm)] + [1.07×BW (kg)] + [0.87×MUAC (cm)], followed by a simple linear regression equation on mid-upper arm circumference (r=0.406), GA in weeks = 26.12+ [1.11×MUAC (cm)]. This finding was consistent with a study carried out by Yadav et al,19 as revealed using a combination of neonatal parameters would determine a better prediction for gestational age as compared to individual parameters.
Conclusion
Except for hand length, all other neonatal anatomical parameters had a positive correlation with gestational age. The overall relative better correlation for estimation of gestational age, alone and in combination, is found by combined MUA, HL, and BW. The relatively better individual neonatal parameter for GA prediction is MUAC.
The relatively better regression model is obtained by combined parameters of MUAC, HL, and BW. These simple and multiple linear regression models are simple and quick. As a result, it can be used at any primary health care by health care providers with the help of ordinary measuring tape. Hence, basic health care personnel can identify preterm cases easily and quickly refer for further management.
Recommendations
Clinicians should carry out routine GA assessment and neonatal anatomical parametric measurement during the postpartum period. Hence, this will provide better evidence for clinical decisions. A similar large scale and multi-center study should be conducted. It would also be ideal to carry out a study on other neonatal anatomical parameters. Furthermore, studies should be conducted on bilateral neonatal anatomical parameters to detect the difference for the prediction of gestational age.
Abbreviations
BW, birth weight; CHL, crown-heel length; CM, centimeter; FL, foot length; GA, gestational age; HC, head circumference; HL, hand length; IMD, intermammary distance; LNMP, last normal menstrual period; MAE, mean absolute error; MAPE, mean average percentage error; MUAC, mid-upper arm circumference; UND, umbilical nipple distance.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval and Consent to Participate
Before data collection, ethical clearance was obtained from the Department of Research Ethics Review Committee (DRERC) of Wollo University. A supporting letter was sent to Dessie Referral Hospital and permission was obtained from the hospital manager to implement the study. The aim and objectives of the study were clearly explained to the manager of Dessie Referral Hospital and midwifery staff. Additionally, all participants’ parents/legal guardians were informed about the purpose and confidentiality issues related to the study. Participation was voluntary. Verbal informed consent was obtained from the participant’s parent/legal guardians who could not able to read and write, and the verbally informed consent process was approved by the DRERC of Wollo University. Written informed consent was obtained from each participant’s parent/guardians who could able to read and write. Finally, data were collected and Confidentiality of patient information was maintained by taking the data anonymously. Lastly, the author confirms that this study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
I thanked Wollo University for providing ethical clearance and a supporting letter for this research preparation. My most sincere gratitude goes to Dessie Referral Hospital health workers for their kind unbroken support throughout the study period. Also, I would like to thank the data collectors for their cooperation during data collection. Finally, I would like to express my great thanks to Dr. Caridad Sanchez for editing the English language.
Disclosure
The author declares that there is no conflicts of interest regarding the publication of this paper.
References
1. Alexander GR, Tompkins ME, Petersen DJ, Hulsey TC, Mor J. Discordance between LMP-based and clinically estimated gestational age: implications for research, programs, and policy. Public Health Rep. 1995;110(4):395–402.
2. Moller AB, Petzold M, Chou D, Say L. Early antenatal care visit: a systematic analysis of regional and global levels and trends of coverage from 1990 to 2013. Lancet Glob Health. 2017;5(10):977–983. doi:10.1016/S2214-109X(17)30325-X
3. Alexander GR, Allen MC. Conceptualization, measurement, and use of gestational age. Clinical and public health practice. J Perinatol. 1996;16(1):53–59.
4. Blencowe H, Cousens S, Oestergaard MZ, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379(9832):2162–2172. doi:10.1016/S0140-6736(12)60820-4
5. Althabe F, Belizán JM, Mazzoni A, et al. Antenatal corticosteroids trial in preterm births to increase neonatal survival in developing countries: study protocol. Reprod Health. 2012;9(1):22. doi:10.1186/1742-4755-9-22
6. Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet. 2015;385(9966):430–440. doi:10.1016/S0140-6736(14)61698-6
7. Lawn JE, Davidge R, Paul VK, et al. Born too soon: care for the preterm baby. Reprod Health. 2013;10(Suppl 1):S5. doi:10.1186/1742-4755-10-S1-S5
8. The Federal Democratic Republic of Ethiopia Ministry of Health Sector Transformation Plan 2015/16–2019/20 (2008-2012 EFY); 2015.
9. UNICEF, Organization WH. Levels & trends in child mortality estimates developed by the UN inter-agency group for child mortality estimation report; 2018.
10. Annan GN, Asiedu Y. Predictors of neonatal deaths in Ashanti Region of Ghana: a cross-sectional study. Adv Public Health. 2018;2018. doi:10.1155/2018/9020914.
11. Gupta A, Mehrotra GK, Mulye S. Study of correlation between gestational age and new-born foot length and chest circumference. Int J Contemp Pediatr. 2018;5(5):1875–1882. doi:10.18203/2349-3291.ijcp20183523
12. Anggraini D, Abdollahian M, Marion K. Foetal weight prediction models at a given gestational age in the absence of ultrasound facilities: application in Indonesia. BMC Pregnancy Childbirth. 2018;18(1):436. doi:10.1186/s12884-018-2047-z
13. Anggraini D, Abdollahian M, Marion K. Accuracy assessment on prediction models for fetal weight based on maternal fundal height. information technology: new generations. Adv Intell Syst Comput. 2016;448. doi:10.1007/978-3-319-32467-8_74.
14. Anggraini D, Abdollahian M, Marion K. Review of low birth weight prediction models in Indonesia. Int J Adv Sci Eng Technol. 2015;3(4):105–111.
15. Nemade P, Ambiye M, Nemade A. Regression analysis on stature estimation from cephalic dimensions. Int J Appl Basic Med Res. 2015;4:298–312.
16. Mansur DI, Haque MK, Sharma K, Mehta DK, Shakya R. Use of head circumference as a predictor of height of individual. Kathmandu Univ Med J. 2014;12(2):89–92. doi:10.3126/kumj.v12i2.13651
17. Thawani R, Dewan P, Faridi M, Arora SK, Kumar R. Estimation of gestational age, using neonatal anthropometry: a cross-sectional study in India. J Health Popul Nutr. 2013;31(4):523–530. doi:10.3329/jhpn.v31i4.20051
18. Khanapurkar S, Radke A. Estimation of stature from the measurement of foot length, hand length and head length in Maharashtra region. Indian J Basic Appl Med Res. 2012;1(2):77–85.
19. Yadav R, Bhatnagar P, Gunjan, et al. Gestational age assessment in newborns using regression equation of anthropometric parameters singly or in combination. Int J Biomed Res. 2016;7(8):600–605. doi:10.7439/ijbr
20. Das NK, Nandy S, Mondal R, Ray S, Hazra A. Gestational age assessment with anthropometric parameters in newborns. Oman Med J. 2018;33(3):229–234. doi:10.5001/omj.2018.42
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
