Back to Journals » Neuropsychiatric Disease and Treatment » Volume 14
Estimated prevalence and incidence of diagnosed ADHD and health care utilization in adults in Sweden – a longitudinal population-based register study
Authors Polyzoi M, Ahnemark E , Medin E, Ginsberg Y
Received 1 November 2017
Accepted for publication 30 January 2018
Published 7 May 2018 Volume 2018:14 Pages 1149—1161
DOI https://doi.org/10.2147/NDT.S155838
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Maria Polyzoi,1 Ewa Ahnemark,2 Emma Medin,1,3 Ylva Ginsberg4,5
1PAREXEL International, Stockholm, Sweden; 2Medical Affairs Department, Shire Sweden AB, Stockholm, Sweden; 3Department of Learning, Informatics, Management and Ethics, Karolinska Institutet, Stockholm, Sweden; 4Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden; 5Department of Clinical Neuroscience, Centre for Psychiatric Research, Karolinska Institutet, Stockholm, Sweden
Background: Although the worldwide prevalence of attention-deficit/hyperactivity disorder (ADHD) in adults is estimated to be between 2% and 5%, it is considered to be underdiagnosed. This register study explored the prevalence of diagnosed ADHD and incidence of newly diagnosed ADHD in Swedish adults over time, and assessed comorbidities and pharmacologic treatment.
Methods: National Patient Register data were used to estimate the overall prevalence of adults (≥18 years) with a registered ADHD diagnosis from 2006 to 2011, and the incidence of newly registered diagnoses from 2007 to 2011. Data from the Prescribed Drug Register were used to estimate the mean dose of the most frequently prescribed ADHD medication.
Results: The estimated annual prevalence (N=44,364) of diagnosed ADHD increased from 0.58 per 1,000 persons in 2006 to 3.54 per 1,000 persons in 2011. The estimated annual incidence of newly diagnosed ADHD (N=24,921) increased from 0.39 per 1,000 persons to 0.90 per 1,000 persons between 2007 and 2011. At least one comorbidity was diagnosed in 52.6% of adults with ADHD (54.0% of newly diagnosed adults), with anxiety, substance use disorders, and depression being the most common. Among all adults with ADHD, 78.9% (65.7% of newly diagnosed adults) were prescribed ADHD medication and one-third were prescribed more than one add-on medication. Osmotic release oral system methylphenidate was the most commonly used medication. The mean daily dose was 51.5 mg, and was significantly higher in males, patients with substance use disorders, patients with drug holidays, and patients with at least one add-on medication. The most frequent concomitant medications were anxiolytics and hypnotics.
Conclusion: In Sweden, the number of adults diagnosed with ADHD increased between 2006 and 2011, and the majority of patients were prescribed ADHD-specific medication. Over one-half of patients had psychiatric comorbidities; one-third were prescribed more than one add-on medication. Consumption of pharmacologic ADHD medication was high in specific patient subpopulations.
Keywords: prevalence, attention-deficit/hyperactivity disorder, adult, register analysis, daily dose, methylphenidate, comorbidity, concomitant medication, treatment dosing
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a heterogeneous neurodevelopmental disorder characterized by core symptoms of inattention, hyperactivity, and impulsivity, with childhood onset and at least partial persistence into adulthood in the majority of cases.1–3 The worldwide prevalence of ADHD in adults is estimated to be between 2% and 5%.4–8 In Sweden, ADHD in adults has been reported to account for 2.7% of all psychiatric diagnoses.9 In general, it is thought that <20% of patients with ADHD are formally diagnosed, and only a small proportion receive pharmacologic treatment for their condition.8,10 A study conducted in the USA, based on a national survey and follow-up interviews, revealed that only 10.9% of adults with ADHD received pharmacologic treatment in the year prior to the interview.6
Diagnosis of ADHD requires a comprehensive review of symptoms and related functional impairments. Criteria routinely used for diagnosis of children and adults with ADHD are the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders – 5th Edition (DSM-5),11 which replaced the previous version (Diagnostic and Statistical Manual of Mental Disorders – 4th Edition [DSM-IV])12 in 2013, and the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10).13 Both the DSM-5 and ICD-10 focus on describing the behavioral problems associated with ADHD, but differences exist in the diagnostic approach; for example, the DSM-5 divides symptoms into 2 groups, inattention and hyperactivity-impulsivity, which the ICD-10 does not. Neither of these diagnostic instruments, however, addresses adult ADHD symptoms comprehensively, with some symptoms of adult ADHD absent from the diagnostic criteria, such as emotional dysregulation.11,13–15 The diagnostic procedure in Sweden includes a clinical diagnostic interview with the patient and significant others (usually parents or spouses) to assess the patient’s developmental and current medical history. Assessment of comorbid disorders, physical examination, and tests for cognitive and executive functioning are also performed.16 DSM-5 criteria are most commonly used for diagnosis in clinical practice in Sweden (and may be converted into an ICD-10 diagnosis using the DSM converter).17
ADHD in adulthood is an important health issue both for the individual and at a societal level.10 ADHD affects the working and social life of patients and is linked to unemployment.18 Furthermore, ADHD is associated with higher use of health care services; for example, due to increased risk of injuries and transport accidents, criminality, smoking, and substance use disorders (SUDs).6,19–21 In general, ADHD frequently coexists with other psychiatric disorders and social problems. It has been reported that ~80% of individuals with ADHD (both children and adults) have at least one registered psychiatric comorbidity,22 such as depression, anxiety, SUD, bipolar disorder, antisocial personality disorder, and impulse control disorders.6,10,23,24 Consequently, in addition to ADHD-specific pharmacologic treatment, many patients with ADHD also use psychotropic medications,25 such as antidepressants, antipsychotics, hypnotics, or sedatives, or medications used to treat addiction disorders.3,22,25
During the period of the current study (2006–2011), no registered pharmaceuticals were approved for treatment of ADHD in adults. Since then, osmotic release oral system methylphenidate (OROS-MPH) has been approved for continued treatment in adulthood in 2011, atomoxetine (ATX) for adults in 2013, and methylphenidate extended release in 2014 for adults newly diagnosed with ADHD. In Sweden, psychiatry specialists and trained pediatric neurologists can initiate pharmacologic treatment with MPH in patients with ADHD, while the authority to prescribe ATX is not restricted to psychiatry specialists.17 During the period studied, amphetamines (amphetamine and dexamphetamine) were recommended in Sweden as the last treatment option and were only available on a named-patient basis.17 Since December 2013, the long-acting prodrug lisdexamfetamine (LDX) has been available in Sweden: it was initially approved for treatment of ADHD in children and adolescents (6–17 years) when response to previous MPH treatment was considered clinically inadequate.26 Since March 2015, LDX has also been approved for the treatment of ADHD in adults.26
In Nordic countries including Sweden, awareness of ADHD appears to be increasing, with higher reported rates of diagnosis and treatment in recent years,3,22,25,27 and an increase in ADHD prescriptions over time, for both sexes and irrespective of age.3,28 Despite such increases, adults with ADHD may still be undertreated, and rates of treatment discontinuation in adolescents and young adults are higher than expected considering the persistence of the disorder in later life.28 A comprehensive overview of the prevalence and treatment of ADHD in adults in Sweden is needed to inform clinicians and aid resource planning for patient management in the future.
The objectives of this study were to explore over time the overall prevalence of diagnosed ADHD between 2006 and 2011, and the incidence of newly registered ADHD diagnoses between 2007 and 2011 in Swedish adults, and to assess comorbidities and pharmacologic treatment use in this population.
Methods
This was a retrospective, longitudinal, observational, register study in Sweden of all adults with a registered diagnosis of ADHD between 2006 and 2011, and adults newly diagnosed with ADHD between 2007 and 2011. Data were derived through the linkage of two national population-based registers (using unique personal identification numbers): the National Patient Register (NPR) and the Prescribed Drug Register (PDR), both held by the National Board of Health and Welfare (Stockholm, Sweden).29 The NPR has nationwide coverage of about 75% for psychiatric outpatient care since 2001 and includes information on patient characteristics such as age and sex, date of the visit, primary discharge diagnosis, and up to 7 secondary diagnoses assigned by the treating medical doctor in accordance with ICD-10.13 The PDR provides information on all prescribed medications since 2005, with identity data for more than 99.7% of patients.30 Data were unidentified when analyzed, and the study was approved by the Regional Ethical Review Board (protocol reference number: 2012/1315-31/3) in Stockholm. As this was a retrospective register study, informed consent by participants was not sought and the Regional Ethical Review Board deemed this ethically acceptable.
Patients
Through the NPR, adults (18 years and above) with a diagnosis of ADHD or hyperkinetic disorder defined by the ICD-10 codes F90.0–F90.9 and F98.8, either as the primary or secondary diagnosis, were identified. The F98.8 code was included to minimize the risk of missing any ADHD cases, as this code was used for ADHD without hyperactivity during this time period in some regions of Sweden. Data on age, sex, and the comorbid diagnoses (ICD codes are listed in Table 1) of autism, atypical autism, anxiety, Asperger syndrome, bipolar disorder, depression, eating disorder, impulse control disorder, personality disorder, oppositional defiant disorder, schizophrenia, and SUD were obtained. The PDR provided data (including dispensing date) on ADHD medications, including OROS-MPH, immediate-release methylphenidate (MPH-IR), modified-release methylphenidate (MPH-MR), ATX, amphetamine, dexamphetamine, and modafinil. Medications with the Anatomical Therapeutic Chemical (ATC) code substring “N06BA” were considered to be ADHD medications.31 Although ATX and OROS-MPH were not approved for use in adults at the time of the study, both were approved for use in children and adolescents, and were used off-label for adults with ADHD. Modafinil is not indicated for use in ADHD but is prescribed off-label for this indication.32 Information on concomitant medications was also obtained through the PDR. The categories of psychotropic medications used were anxiolytics, hypnotics, selective serotonin reuptake inhibitors (SSRIs), serotonin–norepinephrine reuptake inhibitors (SNRIs), antipsychotics, non-selective antidepressants, and other antidepressants; the ATC codes for the medications within each of these categories are listed in Table 1.
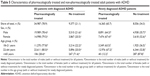
  | Table 1 Independent variables used in multiple linear regression with PDD as response variable |
A cross-sectional dataset included information from January 1, 2006 through December 31, 2011, to estimate the prevalence of diagnosed ADHD. A longitudinal dataset was created, including data from January 1, 2007 through December 31, 2011, to estimate the rate of newly diagnosed adult ADHD and to analyze pharmacologic treatment patterns. For patients to be included in the longitudinal dataset, a 12-month period prior to their first appearance in the NPR with defined ADHD diagnosis, during which no ADHD medication (stimulants or non-stimulants) was dispensed, was required. Each patient was followed for a maximum of 5 years after the index date (until December 31, 2011).
Measures
Estimated prevalence of diagnosed ADHD and estimated incidence of newly diagnosed ADHD
In Sweden, assessment of ADHD in adults is performed at outpatient clinics by multi-professional teams, including a psychiatrist and a psychologist, and often an occupational therapist and a nurse. Detailed recommendations regarding ADHD diagnostic assessments are published by the Swedish National Board of Health and Welfare.16 DSM-5 criteria are commonly used for diagnosing ADHD, and the diagnosis must be reported in the NPR using an ICD-10 code; DSM codes may be translated to an ICD code using a specific code key.
The estimated prevalence rate of ADHD was calculated by dividing the total number of patients with a registered diagnosis of ADHD in the cross-sectional data set per year by the population statistics for Sweden per year overall and by age group (18–21 years, 22–64 years, ≥65 years).33 It was assumed that the size of the population in Sweden was stable during the year and equal to the value measured on November 1 of each year.
The estimated incidence of newly diagnosed ADHD was calculated by dividing the number of newly diagnosed patients in the longitudinal dataset per year by the population statistics for Sweden per year, overall and by age group.
The proportions of patients according to sex and age group, and median and mean (SD) age, were calculated for both the cross-sectional and longitudinal datasets to generate yearly rates.
Comorbidities
All unique adults with diagnosed ADHD in the cross-sectional dataset with registered comorbidities (secondary diagnoses translated from DSM codes to ICD-10 criteria) during the study period were identified. The proportion of patients with at least one registered comorbid disorder was estimated, and the total number of each type of comorbidity was divided by: 1) the total number of all comorbid diagnoses; 2) the total number of patients with at least one comorbid diagnosis; and 3) the complete dataset, to determine the frequency of each of the comorbidities. The same procedure was conducted for the longitudinal dataset to describe the most frequently occurring comorbidities in adults newly diagnosed with ADHD.
Pharmacologic treatment
All patients from the cross-sectional and longitudinal datasets who received ADHD medication at any point during the study period following the patients’ index hospital stay or visit were identified and categorized by sex and age group. For patients in the cross-sectional dataset, age group categorization was based on the age of the patient when first registered to be dispensed ADHD medication. The total numbers of non-medicated patients and newly diagnosed patients were also estimated and presented by age group and sex.
Pharmacologic treatment patterns
The longitudinal dataset was used to analyze pharmacologic treatment patterns for patients diagnosed during the study period. Only one substance or product was followed per patient; if patients were dispensed more than one first-line ADHD medication on the same day, as different medications or different formulations of the same medication, the medication with the highest number of defined daily doses (DDDs) was assumed to be the main first-line treatment for that patient.
To estimate the most frequently dispensed first-line formulations, the number of newly diagnosed patients receiving each type of formulation as first-line treatment was divided by the total number of newly diagnosed patients receiving pharmacologic treatment.
Second-line treatments were estimated in the longitudinal dataset by identifying treatment switches. After the addition of a second dispensed ADHD medication, the patient was followed for a 90-day period (the maximum time period for a prescription in Sweden) to ensure no reappearance of the first-line ADHD medication. To identify the most frequently dispensed second-line ADHD medications, the total number of newly diagnosed patients receiving each type of formulation as second-line treatment was divided by the total number of newly diagnosed patients receiving second-line treatment.
Add-on medication was defined as ADHD medication dispensed in addition to the first-line medication (but not constituting a medication switch within the 90-day review period). The number of newly diagnosed patients treated with 1, 2, 3, or more than 3 ADHD medications at the same time was divided by the total number of newly diagnosed patients receiving ADHD medication.
Concomitant medication was defined as an entry during the same time period as the main first-line ADHD medication. The number of newly diagnosed patients with concomitant medication was divided by the total number of newly diagnosed patients receiving ADHD pharmacologic treatment.
Mean dose of the most frequently prescribed ADHD medication
The average dispensed patient daily dose (PDD) of the most frequently prescribed ADHD medication was identified using the variable “DDD” in the PDR. The number of dispensed PDDs was multiplied by the DDD assigned by the World Health Organization (WHO)31 and divided by the number of days included in the study as a proxy for days on treatment. The mean PDD of the medication (presented as DDDs) was calculated using the cross-sectional dataset to represent the mean dose for all adults registered with an ADHD diagnosis, as well as in the longitudinal dataset to describe the mean dose used in newly diagnosed patients.
As more than one observation may exist for each patient in the cross-sectional dataset, potentially captured in different age groups and including different prescribed doses, all patient observations were considered in the analysis. The mean PDD, mean DDD, and distribution of DDDs were calculated separately for males and females, as well as for each age group. The independent t-test and analysis of variance were used to identify potential statistical differences in the mean dose between sexes and age groups, respectively.
The influence of individual characteristics on the PDD was explored using linear regression analysis with PDD as the continuous response variable. The selected patient characteristics for the starting model are presented in Table 1. Dummy variables were used for qualitative independent variables (eg, presence of certain comorbidities). Variables in <5% of patients were excluded from the analysis. Variable selection was based on a forward selection process with a significance level of 10% selected for variable exclusion to minimize the risk of including variables by chance. The PDD was transformed through the natural logarithm, and the regression coefficients are presented as percentage change in PDD. The final model was selected based on R2 adjusted for number of coefficients and model interpretation (validity of variable and regression coefficient).
SAS Version 9.3 (SAS Institute Inc., Cary, NC, USA) was used in all statistical analyses. If not stated otherwise, the two-sided t-test (5% level of significance) was used for comparisons of means. The p-values presented are descriptive and are uncorrected for multiple comparisons and should be interpreted as non-inferential.
Results
Estimated prevalence of diagnosed ADHD
The cross-sectional dataset included 44,364 patients, aged 18 years and older, registered with an ADHD diagnosis during the study period (2006–2011). Over time, the estimated prevalence of diagnosed ADHD increased from 4,149 patients in 2006 to 26,820 patients in 2011, an increase in the total estimated prevalence from 0.58 per 1,000 persons in 2006 to 3.54 per 1,000 persons in 2011 (Table 2). The mean (SD) age increased from 30.8 (10.8) years in 2006 to 31.7 (11.6) years in 2011, and the proportion of males decreased from 62.5% in 2006 to 55.2% in 2011 (Table 2).
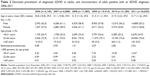  | Table 2 Estimated prevalencea of diagnosed ADHD in adults, and characteristics of adult patients with an ADHD diagnosis, 2006–2011 |
Estimated incidence of newly diagnosed ADHD
The longitudinal dataset included 24,921 adults newly diagnosed with ADHD between 2007 and 2011. The yearly number increased from 2,809 in 2007 to 6,816 in 2011, translating to estimated incidence rate for newly diagnosed patients of 0.39 per 1,000 persons in 2007 and 0.90 per 1,000 persons in 2011 (Table 3). The mean (SD) age increased from 31.4 (10.7) years in 2007 to 32.4 (11.9) years in 2011, and the proportion of male patients decreased from 60.3% in 2007 to 53.1% in 2011.
  | Table 3 Estimated incidencea and characteristics of newly diagnosed adult patients, 2007–2011 |
Comorbidities
In the cross-sectional dataset, 23,344/44,364 (52.6%) adults with diagnosed ADHD were diagnosed with at least one comorbidity during the study period. In the longitudinal dataset (13,447/24,921 [54.0%]), patients newly diagnosed with ADHD had 1 or more comorbidities. In both groups of patients, the comorbidities most commonly observed were anxiety, SUD, and depression, and the least commonly observed comorbidities were impulse control disorder and oppositional defiant disorder (Table 4).
Pharmacologic treatment
In the cross-sectional dataset, 78.9% of adults with diagnosed ADHD were dispensed ADHD medication at some point during the study period, while in the longitudinal dataset, only 65.7% of newly diagnosed patients received ADHD medication. ADHD medication was dispensed less frequently among elderly patients (≥65 years of age; 28.4% of adults with ADHD and 12.2% of newly diagnosed adults) than in younger adults (22–64 years of age; 80.0% of adults with ADHD and 67.2% of newly diagnosed adults; Table 5).
Pharmacologic treatment patterns
Treatment patterns are reported for the longitudinal dataset (2007–2011) comprising adults newly diagnosed with ADHD.
First-line ADHD medication
OROS-MPH was the most frequently dispensed first-line ADHD medication. In 2011, 69.3% of treated patients between 18 and 21 years of age received OROS-MPH, 15.7% received MPH-MR, and 11.0% received ATX. For patients between 22 and 64 years of age, the corresponding proportions were 65.0%, 16.7%, and 13.0%, respectively (data not shown). For adults ≥65 years of age, the proportions were 81.8%, 0.0%, and 18.2%, respectively.
Second-line ADHD medication
In patients who experienced a treatment switch, MPH-MR was the most commonly used second-line medication; 39.4% of treatment-switched patients received MPH-MR, 20.5% were switched to OROS-MPH, 19.1% to MPH-IR, and 14.5% to ATX.
Add-on ADHD medication
Among newly diagnosed patients treated with ADHD medication (n=16,365), 64.7% received no add-on ADHD medication, while 35.3% received at least one add-on medication. A quarter (25.3%) of the newly diagnosed patients who were treated with ADHD medication received one add-on ADHD medication, and 8.0% received 2 add-on medications. The most frequent add-on formulation was MPH-IR (44.0%) followed by MPH-MR (29.4%). The proportions of patients receiving 1, 2, 3, or more than 3 products were similar across age groups (data not shown).
Concomitant medication
A total of 7,323 (22.5%) patients were dispensed concomitant treatment with anxiolytics, 6,677 (20.5%) with hypnotics, and 6,015 (18.5%) with SSRIs. Fewer patients received antipsychotics (4,184, 12.8%), SNRIs (3,087, 9.5%), non-selective antidepressants (989, 3.0%), and other antidepressants (4,304, 13.2%).
Mean dose of OROS-MPH
In the cross-sectional dataset, the mean (SD) PDD of OROS-MPH in adults with diagnosed ADHD was 51.5 (31.0) mg, which corresponds to ~1.72 DDDs when applying the WHO recommendation of DDD = 30 mg. As presented in Table 6, the mean (SD) PDD for males (54.4 mg [33.3]; 1.81 DDDs) was significantly higher (p<0.05) than for females (47.9 mg [27.7]; 1.60 DDDs). Furthermore, the mean PDD was significantly lower (p<0.05) for patients aged 18–21 years than for those aged 22–64 and ≥65 years (Table 6).
  | Table 6 Patient daily dose and defined daily dose of OROS-MPH among all adult patients with diagnosed ADHD treated with OROS-MPH during the study period (cross-sectional dataset; 2006–2011) |
A quarter (25.0%; 5,476) of adults treated with OROS-MPH received a mean dose of <1 DDD, while 9,951 (45.4%) received 1–2 DDDs and 6,499 (29.6%) received ≥2 DDDs (Table 7). A mean dose of <1 DDD was most common in those aged 18–21 years (29.7%), and a dose of ≥2 DDDs was most common (33.1%) in those aged 22–64 years. In the longitudinal dataset, the mean PDD of OROS-MPH received by newly diagnosed adults with ADHD was 48.4 mg (~1.61 DDDs). The mean PDD was higher for males (50.9 mg [1.70 DDDs]) than for females (45.5 mg [1.52 DDDs]). The mean (SD) PDD of OROS-MPH varied across age groups: 18–21 years, 40.7 mg (21.4); 22–64 years, 50.5 mg (30.3); and ≥65 years, 45.6 mg (26.5) (data not shown).
  | Table 7 Proportions of patients receiving OROS-MPH <1 DDD, 1–2 DDDs, and ≥2 DDDs during the study period (cross-sectional dataset) |
Predictors of OROS-MPH dose level
The regression analysis of individual parameters influencing the PDD of OROS-MPH suggested that the presence of at least one add-on medication, comorbid SUD, drug holiday (gap between observations for a patient in the PDR exceeding 90 days), and male sex were the strongest predictors of an increase in PDD (ie, higher mean dose) of OROS-MPH (all p<0.0001; Table 8). In addition, a later expedition year (ie, year when the medication was dispensed), concomitant treatment with an antipsychotic, comorbid personality disorder, concomitant treatment with hypnotics, concomitant treatment with an SNRI, ADHD of combined subtype, and older age were associated with an increase in PDD (Table 8). The strongest predictors of a decrease in PDD (ie, lower mean dose) were living in Stockholm or west Sweden, presence of comorbid bipolar disorder, and ADHD diagnosis F90.0C (all p<0.0001; Table 8).
Discussion
This Swedish population-based study elucidated information regarding the prevalence of diagnosed ADHD and incidence of newly diagnosed ADHD in adults, as well as data on the common comorbidities and patterns of pharmaceutical treatment in this patient population. From 2006 to 2011, there was an increase in the number of adults registered with an ADHD diagnosis in Sweden. The majority of patients with an ADHD diagnosis received both an ADHD medication and a concomitant medication. The most commonly prescribed ADHD medication during the period studied was OROS-MPH. The mean dose of OROS-MPH was heavily influenced by the presence of at least one add-on ADHD medication, comorbid SUD, drug holidays, and male sex. Psychiatric comorbidities were recorded in more than half of the patients.
The increase in both the number of newly diagnosed adults with ADHD from 2007 to 2011 and the overall estimated prevalence of adults with a registered ADHD diagnosis in Sweden from 2006 to 2011 found in this study is consistent with other Nordic studies,3,22,24,25,27,28 and may reflect an increased awareness of the manifestations of ADHD over the lifespan of the patient,8 leading to a higher rate of diagnosis and/or treatment in adults. Such increased recognition of adults with ADHD was found to be a contributing factor to the increased incidence rates of diagnosed ADHD reported in Denmark, as was a general increase in patients seen in psychiatry.34 In Sweden, access to mental health care services has not changed during the time this study was conducted. However, resources may have been prioritized for certain disorders, including ADHD, which may also have contributed to the increased estimated incidence and prevalence rates seen in the study. Previous studies have reported the “dispensing prevalence”, that is, ADHD prevalence irrespective of the registered diagnosis. One study reported that the dispensing prevalence among individuals aged 6–45 years increased from 2.93 per 1,000 in 2006 to 6.98 in 2009, with a larger increase in women than in men.28 In a Danish register-based study, which included age groups from 0–1 to ≥50 years, the dispensing prevalence for ADHD in the general population increased from 1995 until 2008, but was stable from 2009 until the end of the study period in 2011.27 This trend for stabilizing prevalence rates was not observed in the current study of Swedish register data, possibly reflecting the inclusion of only adults in the Swedish study population. As ADHD has been studied more extensively in children than in adults, the inclusion of children as well as adults in the Danish study population may have stabilized the prevalence of ADHD. In addition, the increasing awareness of ADHD in adults may have boosted prevalence rates in an adult-only population. In the USA, the incidence and prevalence of diagnosed ADHD also increased over the period between 2006 and 2009.35
The estimated prevalence among patients with a registered ADHD diagnosis in Sweden (clinical cases) reported in the present study (3.55 per 1,000 persons in 2011) was lower than the worldwide prevalence estimates of ADHD (between 2% and 5%) that were reported in studies seeking to identify all current ADHD cases, both diagnosed and undiagnosed.4–8 Biederman et al estimated that only 20% of ADHD cases in adults are diagnosed, which translates to 4 to 8 cases per 1,000 persons, numbers comparable with the results of the current study.10 Furthermore, differences in diagnostic procedures might produce different prevalence estimates, with studies using ICD-10 to identify ADHD cases estimating significantly lower prevalence rates than studies based on DSM-IV criteria.36
There was no difference in estimated prevalence of ADHD diagnosis between sexes in the present study, which contrasts with the finding of a higher dispensing prevalence in males than in females in a study by Zetterqvist et al.28 However, the Zetterqvist study evaluated the period between 2006 and 2009, while the present study explored the period from 2006 to 2011, and showed that the proportion of females with ADHD increased over time (from 37.5% in 2006 to 44.8% in 2011).
The current study found several psychiatric disorders to be comorbid in patients with ADHD, consistent with previous studies.6,10,24 Kessler et al reported anxiety disorders to be the most common psychiatric comorbidity in adult respondents with ADHD (47.1%), followed by mood disorders (38.3%), impulsive control disorder (19.6%), and any SUD (15.2%).6 While these prevalence estimates do not fully tally with the proportions obtained in the current study, possibly due to differences in definitions of comorbid disorders, anxiety, SUD, and depression are 3 of the most common psychiatric comorbidities reported in both studies. When assessing comorbidities in patients with ADHD, it is important to consider the risk of ADHD masquerading as the coexisting conditions, for example, ADHD symptoms may be similar to those of anxiety.
In agreement with previous studies that found that MPH was the most commonly used ADHD drug, in the present study, OROS-MPH was the most commonly prescribed pharmacologic treatment for ADHD in adults in Sweden.22,27,37 The proportion of diagnosed adults treated with ADHD medications (78.9%) from 2006 to 2011 (cross-sectional dataset) was higher than the proportion (57.0%) reported by Lichtenstein et al in 2012, based on the same registers but conducted from 2006 to 2009.21 This difference may be explained by differences in the definition of ADHD medications between the 2 studies (only MPH and ATX were included in the Lichtenstein study compared with MPH, ATX, amphetamines, and modafinil in the present study), as well as the inclusion of adolescents (aged 15–17 years) in the Lichtenstein study population.
In a study in the USA (n=154), only 10.9% of adults with ADHD reported treatment with ADHD medication in the prior 12-month period;6 this is markedly lower than the proportion (78.9%) in the current study. Potential explanations for this large discrepancy may be the different methods used, with the Kessler study using DSM-IV ADHD diagnoses in a survey of a sample of patients, and the current study using ICD-10 diagnoses in a population-based register study.
The PDD analyses demonstrated that the majority of patients were treated with 1–2 DDDs of OROS-MPH, and that the highest doses were found in the group aged 22–64 years. A higher mean dose of OROS-MPH was associated with comorbid SUD, male sex, drug holidays, or the presence of at least one add-on ADHD medication. The positive association between SUD and higher mean dose could result from overuse related to patients abusing their own stimulant medication,38 or it could also be that patients with ADHD and SUD need higher doses to benefit fully from treatment than do patients without SUD.39 The association between add-on ADHD medications and higher PDDs suggests that some patients’ symptoms are more difficult to address with pharmacologic treatment. The association between drug holidays and higher mean dose could be a consequence of higher impairment due to more severe symptoms, with these patients often requiring higher doses. From the clinical experience of one of the authors (YG), patients with more severe symptoms tend to miss more appointments and fill prescriptions more frequently than patients with lower impairment (who often require comparably lower doses of medication). Drug holidays may occur for numerous reasons, and it is possible that, in this adult population, these are mostly unintended breaks.
The current study was a large population-based study with a 5-year follow-up. Population-based studies, which include all patients with a specific disease instead of only a sample, minimize the possibility that selection bias will have unintended consequences on the study results. The same holds true as potential recall bias can be avoided compared with retrospectively collected data from an interview or survey. Therefore, the results related to estimated prevalence and incidence, patient characteristics, and comorbidities should be representative for all contexts in which the DSM-5 is converted to ICD-10 codes and is subsequently used to provide a diagnosis. Pharmacologic treatment patterns could be influenced by country-specific guidelines and by reimbursement status, which means that the results from those analyses may be less generalizable to other countries.
As with all studies of administrative databases, there are limitations to this current study. As previously stated, the data from this study represent estimated prevalence of diagnosed ADHD and estimated incidence of newly diagnosed ADHD, and this should be noted when making comparisons with other studies, which may present prevalence and incidence based on pharmacotherapy use for ADHD rather than prevalence and incidence of diagnosis. The calculations were made using information from hospital and outpatient administrative data, which may have contained errors due to inaccurate coding, misdiagnosis, or fraud, and coverage may not have been complete. The coverage of psychiatric health care activities in the NPR was ~75%; therefore, 25% of all visits were not recorded and consequently were not included in the analysis. The results were based on data for diagnosed patients in routine clinical practice, and therefore this study provides valuable real-world evidence. However, such data are less stringent than, for example, data collected in a controlled clinical trial, hence prevalence may have been underestimated due to undiagnosed patients or overestimated due to the inclusion of false positives. There was a high rate (80%) of patients who were prescribed ADHD medication. It is possible that some doctors may have only recorded a diagnosis once they had decided that pharmacotherapy was appropriate.
Furthermore, these analyses assume that all relevant visits would have been to psychiatric specialists in Sweden (rather than ADHD-related visits to general clinics). Also, the PDR does not include the indication for the dispensed treatment, a problem that was partly addressed by ensuring that a diagnosis of ADHD for each patient was present in the NPR. In addition, patients may have been diagnosed with ADHD or received treatment for ADHD prior to 2006, then had a gap in treatment or in health care contacts, and reappeared during the period studied, to be incorrectly included as ‘newly diagnosed’.
Finally, as with all observational research, inferential statistics are not subject to the experimental nature of randomized controlled trials, and may therefore be biased by the influence of omitted or immeasurable variables. Causality between the variables and the PDD cannot be concluded.
Conclusion
This study provides important information about adult ADHD in Sweden, including estimated prevalence and incidence, comorbidities, and treatment, a research area in which few recent studies have been performed. Results showed that the number of adults with an ADHD diagnosis increased over time. It also demonstrated that adult ADHD is characterized by high rates of coexistent psychiatric disorders, and that the vast majority of patients are treated pharmacologically with at least one ADHD medication. The high rates of concomitant treatments suggest that current ADHD medications are not sufficient in addressing all symptoms that the adult with ADHD may present with. More resources will be needed for patient management in the future if the rate of diagnosis, and consequently the need for treatment, continue to increase. Studies monitoring patient-reported symptoms, functioning, and quality of life over a longer term, before and after initiation of treatment, through a national quality register for ADHD, are warranted.
Acknowledgments
Under the direction of the authors, Jocelyn Woodcock, MPhil, of Caudex, Oxford, UK and Denise Graham, PhD, for Caudex, Oxford, UK, provided writing assistance for this publication, funded by Shire International GmbH. Editorial assistance in formatting, proofreading, copy editing, and fact checking the manuscript, and coordination and collation of comments, was provided by Caudex (funded by Shire International GmbH). This research was funded by Shire Sweden AB. Although employees of Shire were involved in the design, collection, analysis, interpretation, and fact checking of information, the content of this manuscript, interpretation of the data, and decision to submit the manuscript for publication in Neuropsychiatric Disease and Treatment was made by the authors independently.
Author contributions
YG, EA, and EM contributed to study design, manuscript development, and final manuscript review. MP contributed to data collection and analysis, manuscript development, and final manuscript review. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work. All authors approved the final version of the manuscript.
Disclosure
M Polyzoi is employed by PAREXEL International, which has been funded by Shire Sweden AB. E Ahnemark is employed by Shire Sweden AB. E Medin is employed by PAREXEL International, which has been funded by Shire Sweden AB. Y Ginsberg has over the past 3 years received speaker fees, reimbursement for travel costs, and/or served as a consultant for Novartis, HB Pharma, Shire, Eli Lilly, Hogrefe, Broadman Clarke Partners, Medscape, Medibas, and Natur & Kultur. The authors report no other conflicts of interest in this work.
References
Dulcan M. Practice parameters for the assessment and treatment of children, adolescents, and adults with attention-deficit/hyperactivity disorder. American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry. 1997;36(Suppl 10):85S–121S. | ||
Faraone SV, Sergeant J, Gillberg C, Biederman J. The worldwide prevalence of ADHD: is it an American condition? World Psychiatry. 2003;2(2):104–113. | ||
National Board of Health and Welfare. Kraftig ökning av adhd-läkemedel till vuxna [Substantial increase in the prescription of ADHD drugs for adults]. 2012. Available from: http://www.socialstyrelsen.se/nyheter/2012oktober/kraftigokningavadhd-lakemedeltillvuxna. Accessed March 10, 2017. | ||
Fayyad J, De Graaf R, Kessler R, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry. 2007;190:402–409. | ||
Kessler RC, Adler L, Ames M, et al. The prevalence and effects of adult attention deficit/hyperactivity disorder on work performance in a nationally representative sample of workers. J Occup Environ Med. 2005;47(6):565–572. | ||
Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716–723. | ||
Kooij JJ, Buitelaar JK, van den Oord EJ, Furer JW, Rijnders CA, Hodiamont PP. Internal and external validity of attention-deficit hyperactivity disorder in a population-based sample of adults. Psychol Med. 2005;35(6):817–827. | ||
Simon V, Czobor P, Balint S, Meszaros A, Bitter I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry. 2009;194(3):204–211. | ||
Nylander L, Holmqvist M, Gustafson L, Gillberg C. Attention-deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) in adult psychiatry. A 20-year register study. Nord J Psychiatry. 2013;67(5):344–350. | ||
Biederman J, Wilens T, Spencer T. Diagnosis and treatment of adults with attention-deficit/hyperactivity disorder. CNS Spectr. 2007;12(6):1–15. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Arlington, VA, USA: American Psychiatric Publishing; 2013. | ||
American Psychiatric Association. Attention-deficit and disruptive behavior disorders. Attention-deficit/hyperactivity disorder. Diagnostic and Statistical Manual of Mental Disorders. Fourth edition. Arlington, VA, USA: American Psychiatric Association; 2000:85–103. | ||
World Health Organization. International Classification of Diseases (ICD-10). Geneva, Switzerland: WHO; 1992. | ||
Corbisiero S, Stieglitz RD, Retz W, Rosler M. Is emotional dysregulation part of the psychopathology of ADHD in adults? Atten Defic Hyperact Disord. 2013;5(2):83–92. | ||
Trott GE. Attention-deficit/hyperactivity disorder (ADHD) in the course of life. Eur Arch Psychiatry Clin Neurosci. 2006;256(Suppl 1):I21–I25. | ||
National Board of Health and Welfare. Stöd till barn, ungdomar och vuxna med adhd – ett kunskapsstöd [Support for children, adolescents and adults with ADHD – a knowledge support]. 2014. Available from: http://www.socialstyrelsen.se/publikationer2014/2014-10-42. Accessed March 15, 2017. | ||
Medical Products Agency. Uppdaterad rekommendation för läkemedelsbehandling av adhd [Updated recommendations for pharmacological treatment of ADHD]. 2016. Available from: https://lakemedelsverket.se/Alla-nyheter/NYHETER-2016/Uppdaterad-rekommendation-for-lakemedelsbehandling-av-adhd/. Accessed March 10, 2017. | ||
Able SL, Haynes V, Hong J. Diagnosis, treatment, and burden of illness among adults with attention-deficit/hyperactivity disorder in Europe. Pragmat Obs Res. 2014;5:21–33. | ||
Chang Z, Lichtenstein P, D’Onofrio BM, Sjolander A, Larsson H. Serious transport accidents in adults with attention-deficit/hyperactivity disorder and the effect of medication: a population-based study. JAMA Psychiatry. 2014;71(3):319–325. | ||
Chang Z, Lichtenstein P, Halldner L, et al. Stimulant ADHD medication and risk for substance abuse. J Child Psychol Psychiatry. 2014;55(8):878–885. | ||
Lichtenstein P, Halldner L, Zetterqvist J, et al. Medication for attention deficit-hyperactivity disorder and criminality. N Engl J Med. 2012;367(21):2006–2014. | ||
Bahmanyar S, Sundstrom A, Kaijser M, von Knorring AL, Kieler H. Pharmacological treatment and demographic characteristics of pediatric patients with Attention Deficit Hyperactivity Disorder, Sweden. Eur Neuropsychopharmacol. 2013;23(12):1732–1738. | ||
Kooij SJ, Bejerot S, Blackwell A, et al. European consensus statement on diagnosis and treatment of adult ADHD: the European Network Adult ADHD. BMC Psychiatry. 2010;10:67. | ||
Sobanski E. Psychiatric comorbidity in adults with attention-deficit/hyperactivity disorder (ADHD). Eur Arch Psychiatry Clin Neurosci. 2006;256(Suppl 1):i26–i31. | ||
Pottegard A, Bjerregaard BK, Glintborg D, Kortegaard LS, Hallas J, Moreno SI. The use of medication against attention deficit/hyperactivity disorder in Denmark: a drug use study from a patient perspective. Eur J Clin Pharmacol. 2013;69(3):589–598. | ||
FASS. Elvanse Summary of Product Characteristics. 2015. Available from: http://www.fass.se/LIF/product?8&userType=2&nplId=20140130000137&docType=6. Accessed March 10, 2017. | ||
Pottegard A, Bjerregaard BK, Glintborg D, Hallas J, Moreno SI. The use of medication against attention deficit hyperactivity disorder in Denmark: a drug use study from a national perspective. Eur J Clin Pharmacol. 2012;68(10):1443–1450. | ||
Zetterqvist J, Asherson P, Halldner L, Langstrom N, Larsson H. Stimulant and non-stimulant attention deficit/hyperactivity disorder drug use: total population study of trends and discontinuation patterns 2006–2009. Acta Psychiatr Scand. 2013;128(1):70–77. | ||
National Board of Health and Welfare. Sweden National Patient Register 2011. 2011. Available from: http://ghdx.healthdata.org/record/sweden-national-patient-register-2011. Accessed March 10, 2017. | ||
Wettermark B, Hammar N, Fored CM, et al. The new Swedish prescribed drug register-opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007;16(7):726–735. | ||
World Health Organization. WHO Guidelines for ATC classification and DDD assignment. 2015. Available from: http://www.whocc.no. Accessed March 10, 2017. | ||
Olsson J, Ahlqvist Rastad J. Läkemedelsbehandling av ADHD– Bakgrundsdokumentation: Förskrivningsmönster ADHD-läkemedel i Sverige Information från Läkemedelsverket 1:2009 [Pharmacological treatment of ADHD-background documentation: prescription pattern of ADHD medication in Sweden. Information from the medical products agency]. 2009. Available from: https://lakemedelsverket.se/upload/halso-och-sjukvard/behandlingsrekommendationer/bakg_dok/ADHD-bakgrund_webb_bokm%C3%A4rken.pdf. Accessed March 10, 2017. | ||
Statistic Sweden. Statistical database. 2013. Available from: http://www.statistikdatabasen.scb.se/pxweb/en/ssd/START__BE__BE0101__BE0101A/FolkmangdNov/?rxid=bf7d1575-c52e-49d4-a01f-32d806668c10. Accessed March 10, 2017. | ||
Mohr Jensen C, Steinhausen HC. Time trends in incidence rates of diagnosed attention-deficit/hyperactivity disorder across 16 years in a nationwide Danish registry study. J Clin Psychiatry. 2015;76(3):e334–e341. | ||
Knight TK, Kawatkar A, Hodgkins P, et al. Prevalence and incidence of adult attention deficit/hyperactivity disorder in a large managed care population. Curr Med Res Opin. 2014;30(7):1291–1299. | ||
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942–948. | ||
Zoega H, Furu K, Halldorsson M, Thomsen PH, Sourander A, Martikainen JE. Use of ADHD drugs in the Nordic countries: a population-based comparison study. Acta Psychiatr Scand. 2011;123(5):360–367. | ||
Wilens TE, Adler LA, Adams J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(1):21–31. | ||
Mariani JJ, Levin FR. Treatment strategies for co-occurring ADHD and substance use disorders. Am J Addict. 2007;16(Suppl 1):45–54. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.