Back to Journals » Infection and Drug Resistance » Volume 13
Eradication Treatment of Helicobacter pylori Infection Based on Molecular Pathologic Antibiotic Resistance
Authors Gao C , Du SY, Fang L, Fan YH, Song AP, Chen H
Received 23 September 2019
Accepted for publication 17 December 2019
Published 7 January 2020 Volume 2020:13 Pages 69—79
DOI https://doi.org/10.2147/IDR.S232169
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sahil Khanna
Chun Gao, 1 Shi-Yu Du, 1 Long Fang, 1 Yan-Hua Fan, 1 Ai-Ping Song, 2 Huang Chen 2
1Department of Gastroenterology, China-Japan Friendship Hospital, Ministry of Health, Beijing 100029, People’s Republic of China; 2Department of Pathology, China-Japan Friendship Hospital, Ministry of Health, Beijing 100029, People’s Republic of China
Correspondence: Yan-Hua Fan
Department of Gastroenterology, China-Japan Friendship Hospital, Ministry of Health, No. 2 Yinghua East Road, Beijing 100029, People’s Republic of China
Tel/Fax +86-10-84205503
Email [email protected]
Background: Unfortunately, the eradication rate of Helicobacter pylori (H. pylori) treatment is markedly decreasing in recent years and the major reason is antibiotic resistance. Our study was designed to determine the effect and safety of H. pylori eradication treatment based on the molecular pathologic antibiotic resistance.
Methods: 261 patients were analyzed retrospectively, including 111 patients who were treated for the first time (one group as First-treated) and 150 patients who failed at least once in bismuth quadruple therapy (another group as Re-treatment). Antibiotic resistance was examined by Real-time PCR detection and conventional PCR and sequencing method. The eradication rate (ER) was compared per intention to treat (ITT) and per protocol (PP) between the two groups.
Results: The resistance rates to amoxicillin, clarithromycin, fluoroquinolone and tetracycline were 5.5%, 42.1%, 41.7% and 12.9% in the 111 first-treated patients, and 11.7%, 79.7%, 70.7% and 30.0% in the 150 re-treatment patients. The ERs in the ITT and PP analyses were 92.79% (95% CI, 87.98– 97.60%, n=111) and 98.10% (95% CI, 95.48– 100%, n=105), respectively, in the first-treated patients and 90.67% (95% CI, 86.01– 95.32%, n=150) and 95.10% (95% CI, 91.57– 98.64%, n=143), respectively, in the re-treatment patients. No significant differences were shown in the ERs between two group patients, and no serious adverse events were found.
Conclusion: H. pylori eradication treatment based on molecular pathologic antibiotic resistance showed good effect and safety in both first and re-treated patients.
Keywords: Helicobacter pylori, antibiotic resistance, eradication, first treatment, re-treatment, molecular pathology
Introduction
Helicobacter pylori (H. pylori), which infects more than 50% of the entire world’s population, has become a global health problem associated with numerous benign and malignant gastric diseases, including chronic gastritis, gastric and duodenal ulcers, gastric cancer and gastric MALT (mucosa-associated lymphoid tissue) lymphomas.1–3 In developing countries, H. pylori has been found in the stomachs of 70% to 90% of the people, and in Western nations, 25% to 50% of the total population carries H. pylori.3 Plenty of studies over the past decades have demonstrated that eradication treatment of H. pylori infection is of great importance to H. pylori-associated diseases, such as ulcer healing, regression of MALT lymphomas and decreased cancer risk.4
Four important consensus reports for the management of H. pylori infection have been published in the past 4 years, including Management of H. pylori infection- the Maastricht V/Florence Consensus Report, Kyoto global consensus report on H. pylori gastritis, the Toronto consensus for the treatment of H. pylori infection in adults and Fifth Chinese National Consensus Report on the management of H. pylori infection.5–8 Eradication treatment regimens for H. pylori infection recommended by these guidelines included clarithromycin-based triple therapy (proton pump inhibitor/PPI + amoxicillin + clarithromycin), nonbismuth quadruple regimen (sequential, concomitant and hybrid therapy) and bismuth-containing quadruple therapy.8
For standard bismuth quadruple therapy, our Fifth National Consensus recommends seven therapy regimens and six antibiotics are commonly used, including amoxicillin, clarithromycin, levofloxacin, metronidazole, furazolidone and tetracycline.8 However, unfortunately, the eradication rate of H. pylori treatment is markedly decreasing and the major reason is the antibiotic resistance.5–8 As far as the primary resistance is concerned, recent studies showed that the resistance rates of H. pylori to clarithromycin, metronidazole and levofloxacin are 20–50%, 40–70% and 20–50%, respectively.8–11 To improve the H. pylori eradication rate, performing the drug sensitivity test before treatment may have a comparative advantage.8,12
With the rapid development of molecular pathology, some molecular markers have been confirmed to be associated with antibiotic resistance, for example the 23S rRNA point mutations, including A2143G, A2142G and A2142C of domain V, which have been found in more than 90% of patients with clarithromycin resistance.13–15 For the antibiotic resistance in H. pylori infection, bacterial culture and disc diffusion method are recommended by the Clinical Laboratory Standard Institute (CLSI).16–18 However, compared with H. pylori culture, molecular pathological detection based on molecular markers, such as real-time polymerase chain reaction (PCR) and conventional PCR analysis, is a very simple and economic approach which also takes less time. Our study was designed to determine the effect and safety of H. pylori eradication therapy based on the results of molecular pathologic antibiotic resistance.
Materials and Methods
Patients, Inclusion and Exclusion Criteria
A total of 261 patients, who had been subjected to H. pylori treatment based on molecular pathologic antibiotic resistance, were retrospectively analyzed, including 111 patients who were treated for the first time (one group as First-treated) and 150 patients who failed at least once in bismuth quadruple therapy (another group as Re-treatment). The whole process of our research is in full compliance with the principles of the Declaration of Helsinki and our research project was approved by the Human Research Ethics Committee of our hospital. Written informed consent was obtained from all patients. Inclusion criteria included: (1) patients who were aged between 18 and 80 years old; (2) patients who were diagnosed with H. pylori infection by histopathological examination; and (3) patients who can be followed up successfully. Exclusion criteria included: (1) patients who had received antimicrobial therapy 2 months prior to gastroscope examination; (2) patients who had received upper gastrointestinal surgery; (3) patients who had been diagnosed with malignancies; and (4) patients who had serious diseases of heart, lung, liver or kidney.
Specimens Collection
For each patient, gastric body and/or antral biopsies were collected when they underwent upper gastrointestinal endoscopy. The gastric biopsies were prepared following the requirements of molecular pathological detection and should be sufficient for further polymerase chain reaction (PCR) and real-time PCR analysis.
PCR Detection of UreA and CYP2C19 Genotypes in Gastric Biopsies
For confirmation of the presence of H. pylori infection in gastric biopsies, UreA gene was detected by the conventional PCR method.19,20 Primers for PCR amplification of UreA (F: 5ʹ-GCCAATGGTAAATTAGTT-3′ R: 5ʹ-CTCCTTAATTGTTTTTAC-3′)20 was designed according to published study and synthesized at the NewLife Inc. (China). Moreover, the effect of PPI in H. pylori eradication therapy treatment can be affected by the CYP2C19 gene polymorphisms.21 Three main alleles have been found, including CYP2C19*1 (wild-type), CYP2C19*2 (mutation in exon 5) and CYP2C19*3 (mutation in exon 4).21,22 The sequences of primers were designed and synthesized for CYP2C19*2 (F: 5ʹ-AATTACAACCAGAGCTTGGC-3′ R: 5ʹ-TATCA CTTTCCATAAAAGCAAG-3′) and CYP2C19*3 (F: 5ʹ-TATTATTATCTGTTA ACTAATATGA-3′ R: 5ʹ-ACTTCAGGGCTTGGTCAATA-3′).21 They were detected by PCR amplification and the products were analyzed and sequenced at the NewLife Inc.
Real-Time PCR Detection of Mutations Associated with Clarithromycin Resistance
Three main 23S rRNA point mutations, including A2143G, A2142G and A2142C of domain V (Supplementary Table 1), have been found to be associated with more than 90% of patients with clarithromycin resistance.13–15,20 A TaqMan real-time PCR allelic discrimination assay (NewLife, Beijing, China) was used to determine these point mutations, according to the description provided by previously published references.15,20 Primers and probes were designed for both DNA wild type and mutated DNA, and the sequences are shown in Supplementary Table 2. The attachment of minor groove binder (MGB) to oligonucleotides and the shorter fluorogenic probes were used,20,23 and the probes were labeled with two different fluorescent dyes (VIC dye and FAM dye). The real-time PCR detection was performed following the manufacturer’s instructions. Positive and negative controls were used simultaneously, and all samples were detected for two times.
Conventional PCR and Sequencing for Detection of Mutations Associated with Amoxicillin, Fluoroquinolone and Tetracycline Resistance
As shown in Supplementary Table 1, gene mutations of PBP1, gyrA and 16S rRNA have been confirmed to be associated with H. pylori resistance to amoxicillin, fluoroquinolone and tetracycline, respectively.24–28 Conventional PCR and sequencing method was used to detect these mutation sites, and Supplementary Table 3 shows the sequences of primers focused on target genes. All of the reactions were performed in a 25 μL volume and the PCR amplifications were performed using an MJR PTN-200 PCR machine (MJ Research Inc, Watertown, USA) according to manufacturer’s directions. The PCR amplification products were separated by 2% agarose gel electrophoresis and further sequencing was done by the NewLife, China.
Eradication Treatment of H. pylori Infection Based on Molecular Pathologic Antibiotic Resistance
Before the initiation of eradication therapy, all the patients were diagnosed with H. pylori infection by histology examination (Warthin-Starry silver staining) and PCR detection of UreA gene. They were subjected to H. pylori eradication therapy for 14 days based on the results of antibiotic resistance by molecular pathologic tests. Four weeks after the end of eradication treatment, these patients were detected by UBT (13C-urea breath test) and/or histopathological examinations to determine the status of H. pylori infection. Eight weeks after treatment, UBT were repeated for these patients to confirm the effect of H. pylori eradication therapy. At the end of treatment, liver and renal functions were examined, and adverse events were recorded and compared. The eradication rates were used as the main outcome measure.
Statistical Analyses
SPSS 20.0 for Windows (SPSS Inc., Chicago, IL, USA) were performed for statistical analyses. Chi-square test or Fisher’s exact test was used to conduct the comparison of eradication rates, most of the patients’ demographic characteristics, results of antibiotic resistance by molecular pathologic examinations, treatment regimens of H. pylori eradication, and frequencies of adverse events. The eradication rate in each group was analyzed per intention to treat and per protocol, with 95% confidence interval. A P<0.05 was considered significant and all P values quoted are two-sided.
Results
Patients’ Demographics
Two hundred and sixty-one patients were analyzed retrospectively, including 111 first-treated patients and 150 re-treatment patients (Figure 1). The patients’ demographics are shown in Table 1. For the 261 patients, the mean age was 52.3 ± 15.4 years and 116 patients were male. Upper gastrointestinal endoscopy showed that 146 patients were diagnosed with chronic superficial gastritis (CSG) and 115 patients had chronic atrophic gastritis (CAG). In addition, peptic ulcer was found in 42 patients, including 34 with duodenal ulcer and 8 with gastric ulcer (Table 1).
 |
Table 1 Patients’ Demographics |
 |
Figure 1 Flow diagram of this study. |
The diagnosis of H. pylori infection was confirmed by two methods, including Warthin-Starry silver staining and PCR detection of UreA gene. Before the H. pylori eradication treatment, antibiotic resistance was determined and the treatment regimens were chosen based on the results of molecular pathologic examinations detection. The CYP2C19 gene polymorphisms were obtained for 237 patients, including 108 patients were rapid metabolizer (RM), 105 patients were intermediate metabolizer (IM) and 24 patients were poor metabolizer (PM). As shown in Table 1, compared with patients who had not received prior H. pylori eradication treatment, those patients who failed in bismuth quadruple therapy had a higher percentage of female patients (42.3% vs 65.3%, P=0.033). No significant differences were found by univariable analysis for mean age, endoscopic findings and CYP2C19 gene polymorphisms (Table 1).
Antibiotic Resistance of H. pylori Infection by Molecular Pathologic Examinations
Four antibiotics commonly used for H. pylori eradication treatment were examined, including amoxicillin (AMPC/A), clarithromycin (CAM/C), fluoroquinolone (FLQ/F) and tetracycline (TET/T). The choice of antibiotics in treatment regimens of H. pylori eradication were based on antibiotic resistance by molecular pathologic examinations. Metronidazole (MNZ) and furazolidone (FZD) was not determined in our study and furazolidone could be also used for H. pylori eradication treatment considering that the percentage of furazolidone resistance was very low in our country.29,30
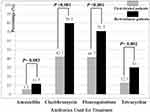
Table 2 and Figure 2 show the results of molecular pathologic examinations. The total resistance rates to amoxicillin, clarithromycin, fluoroquinolone and tetracycline were 9.0%, 63.6%, 58.5% and 22.2%, respectively. For the 111 first-treated patients, the rates of antibiotic resistance were 5.5% (AMPC), 42.1% (CAM), 41.7% (FLQ) and 12.9% (TET), respectively; whereas for the 150 re-treatment patients, the rates were 11.7% (AMPC), 79.7% (CAM), 70.7% (FLQ) and 30.0% (TET), respectively. Significant differences were found by univariable analysis for the rates of antibiotic resistance to clarithromycin (P<0.001), fluoroquinolone (P<0.001) and tetracycline (P=0.002) between those first-treated patients and re-treatment patients (Table 2).
 |
Table 2 Antibiotic Resistance of H. pylori: Molecular Pathologic Results |
Moreover, we analyzed the percentages of patients who had drug resistance to two antibiotics, and compared the differences between first-treated and re-treatment patients (Table 2). Because the rate of amoxicillin resistance was low and only 23 patients had amoxicillin resistance, the numbers of patients who had antibiotic resistance to AMPC + CAM, AMPC + FLQ and AMPC + TET were 14, 13 and 10, respectively, and no significant differences were found between those patients. As shown in Table 2, compared with first-treated patients, those re-treatment patients had higher rates of antibiotic resistance to CAM + FLQ (25.0% vs 58.0%, P<0.001), CAM + TET (9.9% vs 24.6%, P=0.005), and FLQ + TET (8.1% vs 21.7%, P=0.006).
Treatment Regimen of H. pylori Eradication
For all the 261 patients, whether they were treated for the first time or re-treated, bismuth quadruple therapy was used and the two antibiotics were chosen based on the results of antibiotic resistance by molecular pathologic examinations. In our study, seven patients were not treated by any regimen because 6 patients were resistant to all available antibiotics and one patient was intractable (Figure 1). In the 254 patients who received H. pylori eradication therapy, four treatment regimens were used for more than 90% of them (Table 3), including AMPC + CAM (59 patients, 23.2%), AMPC + FLQ (65, 25.6%), AMPC + TET (62, 24.4%), and AMPC + FZD (43, 16.9%). Between first-treated and re-treated patients, significant differences were found for all these four regimens (P<0.001, P=0.015, P=0.001 and P=0.014).
 |
Table 3 Treatment Regimen of H. pylori Eradication |
Eradication Rates of H. pylori Infection
As shown in Figure 1, 261 patients were included in the intention to treat (ITT) analysis, and after our study was completed, 248 patients were included in the per-protocol (PP) analysis. Six patients were lost to follow up. The eradication rates in the ITT and PP analyses were 92.79% (95% confidence interval/CI, 87.98–97.60%, n=111) and 98.10% (95% CI, 95.48–100%, n=105), respectively, in the first-treated patients and 90.67% (95% CI, 86.01–95.32%, n=150) and 95.10% (95% CI, 91.57–98.64%, n=143), respectively, in the re-treatment patients (Figure 3). No significant differences were found in the ITT (P=0.445) and PP (P=0.309) analyses.
Safety and Comparison of Adverse Events
Adverse events were recorded, including diarrhea, black stool, abdominal pain, heart burn, flatulence, nausea/vomiting, belching, skin rash, headache, dysgeusia, fever, constipation, anorexia, fatigue and dizziness. Besides the dysgeusia induced by the drug of clarithromycin, no significant differences were observed (Table 4).
 |
Table 4 Safety and Comparison of Adverse Events |
Discussion
Considering the markedly decreased eradication rate of H. pylori infection and rapid development of molecular pathology, our study was designed to determine the effect and safety of H. pylori eradication therapy regimens based on the results of antibiotic resistance by molecular pathologic examinations. Our study included 111 patients who had not received prior eradication treatment and 150 patients who failed at least once in bismuth quadruple therapy, and found that good effect and safety could be obtained in both first-treated and re-treatment patients when treatment regimens were determined based on the molecular pathologic antibiotic resistance.
Primary resistance and secondary resistance are the two kinds of H. pylori antibiotic resistance, and secondary resistance means drug resistance after treatment failure.8 The Fifth Chinese National Consensus Report on the management of H. pylori infection mentioned that the primary resistance rates to clarithromycin, metronidazole and levofloxacin are 20–50%, 40–70% and 20–50%, respectively.8 In our study, the primary resistance rates to clarithromycin and fluoroquinolone are 42.1% and 41.7%, which are similar to the results of previous reports.
For the secondary resistance, our study demonstrates that the resistance rates to clarithromycin and fluoroquinolone are 79.7% and 70.7% in the patients who failed at least once in bismuth quadruple therapy. Compared with primary resistance rates, these numbers showed that the acquired drug resistances to clarithromycin and fluoroquinolone were easier than to other antibiotics, for example amoxicillin and tetracycline. The Maastricht V/Florence Consensus Report mentions that, when the resistance rate to clarithromycin is more than 15%, PPI-clarithromycin-containing triple therapy without prior susceptibility testing should be abandoned.5 Considering the high clarithromycin and fluoroquinolone resistance in our country,8 performing the drug sensitivity test before treatment may have a comparative advantage.
A wealth of research suggests that H. pylori resistance to clarithromycin is the most important factor for eradication failure.31,32 Are there any definite time span and/or external factors which influence led to the occurrence of clarithromycin resistance and 23S rRNA point mutations? One study was performed to evaluate the primary clarithromycin resistance and associated mutations in children in Poland during 1998–2000.33 The authors found that most of the primary resistance was caused by an A2143G mutation and the prevalence of clarithromycin resistance in children was increased from 17.0% to 23.5% over the 3 years.33 Some researchers from Spain showed that clarithromycin resistance was significantly associated with patients who were previously treated, with patients born in Spain, and with pediatric patients.34 In addition, they found the relationship between clarithromycin resistance, the vacA s2/m2 genotype and cagA negative-expression.34 Hakemi Vala et al deduced that the primary resistance could be related to cross-reactivity between other macrolides.32
As shown in Table 1, the percentage of female patients who had failed reaction to bismuth quadruple therapy was higher than male patients. It is in line with some previous studies.35,36 One study showed that female gender (OR, 1.73; 95% CI, 1.15 to 4.25) and clarithromycin resistance (OR, 19.13; 95% CI, 9.35 to 35.09) were strongly associated with eradication failure.35 Another study also showed that female gender and smoking were associated with the treatment failure.36 The reason may be also related to clarithromycin resistance and point mutation. Research suggested that the 2143G point mutation in the 23S rRNA was a risk factor for eradication failure and the presence of 2143G was significantly associated with female sex.37
Our study also shows that the primary and secondary resistance rates of H. pylori to amoxicillin are 5.5% and 11.7%, whereas these rates to tetracycline are 12.9% and 30.0%, respectively. A prospective serial study conducted in Beijing of China found that the primary resistance rates of H. pylori were 6.7% and 4.9% to amoxicillin and tetracycline.9 Another study conducted in Shanghai of China reported the amoxicillin resistance rate was 8.3%.38 For amoxicillin resistance, we obtained the similar result; however, for tetracycline, the rate is slightly higher than others and the reason may be associated with the patient population and prior used same class drugs.8 Because the primary resistance rates to amoxicillin and tetracycline remain low in our country, it may be not necessary to consider the drug sensitivity test before use.8
For the effect and safety of H. pylori eradication treatment, our study showed that the ERs in the ITT and PP analyses were 92.79% and 98.10%, respectively, in the first-treated patients and 90.67% and 95.10%, respectively, in the re-treated patients. We compared our results with others from different geographical regions.39–41 One study which was conducted in the Japan used vonoprazan-based eradication therapy and found that the ERs were 91.24% (427/468) and 95.45% (42/44), respectively, for the first-line therapy and the second-line therapy.39 The researchers from the Iran evaluated the efficacy of bismuth-based quadruple therapy and showed that the ERs in the ITT and PP analyses were 90.2% and 91.9%, respectively.40 Another study from the Northwest Ethiopia adopted the standard triple therapy and reached the overall eradication rate of 90.3% (379/421).41 Compared with these studies, good effect and safety were obtained in our study for both first-treated and re-treatment patients, although the high resistance rates to some antibiotics were found, and more than half the patients failed in bismuth quadruple therapy. Our results indicated that satisfactory ER could be also obtained based on the molecular pathologic antibiotic resistance.
The best effort was that the antibiotic resistance of H. pylori was determined by molecular pathologic examinations, including Real-time PCR detection and conventional PCR and sequencing method, especially the TaqMan real-time PCR allelic discrimination assay which was used to detect the clarithromycin resistance. Compared with the E-test and agar dilution method,42,43 the molecular pathologic examinations gave the similar results. Moreover, satisfactory eradication rates were obtained which indicated that these examinations could be used routinely.
The first limitation may be that our study was conducted in one large-scale medical center of China and the selection bias may not be avoided. The patient population may be different from those patients treated in the small and medium-sized hospitals, not to speak of the hospitals located in remote regions and ethnic minority regions. In addition, a meaningful portion of the fees for molecular pathologic examinations were afforded by the patients. The second limitation may be that only 261 patients with H. pylori infection were included in our study. We wish that our results and conclusion could be validated in more patients, more hospitals and more studies.
In conclusion, good effect and safety are obtained in both first-treated and re-treated patients when treatment regimens were determined based on the molecular pathologic antibiotic resistance, although more prospective studies are required. Compared with H. pylori culture and disc diffusion method, molecular pathological detection based on molecular markers is a very simple and economic approach which also takes less time, we hope that molecular pathologic antibiotic resistance could be used widely.
Ethics Approval and Informed Consent
The whole process of our research is in full compliance with the principles of the Declaration of Helsinki and our research project was approved by the Human Research Ethics Committee of China-Japan Friendship Hospital, Ministry of Health. Written informed consent was obtained from all patients.
Author Contributions
All authors contributed toward data analysis, drafting and revising the paper, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Funding
This work was supported by Z131107000413067 from the Beijing NOVA Programme of Beijing Municipal Science and Technology Commission.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Smith SM, O’Morain C, McNamara D. Helicobacter pylori resistance to current therapies. Curr Opin Gastroenterol. 2019;35(1):6–13. doi:10.1097/MOG.0000000000000497
2. Quaglia NC, Dambrosio A. Helicobacter pylori: a foodborne pathogen? World J Gastroenterol. 2018;24(31):3472–3487. doi:10.3748/wjg.v24.i31.3472
3. Sjomina O, Pavlova J, Niv Y, Leja M. Epidemiology of Helicobacter pylori infection. Helicobacter. 2018;23(Suppl 1):e12514. doi:10.1111/hel.2018.23.issue-S1
4. Mansour-Ghanaei F, Pedarpour Z, Shafaghi A, Joukar F. Clarithromycin versus gemifloxacin in quadruple therapeutic regimens for helicobacter pylori infection eradication. Middle East J Dig Dis. 2017;9(2):100–106. doi:10.15171/mejdd.2017.58
5. Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection-the Maastricht V/Florence consensus report. Gut. 2017;66(1):6–30.
6. Sugano K, Tack J, Kuipers EJ, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut. 2015;64(9):1353–1367. doi:10.1136/gutjnl-2015-309252
7. Fallone CA, Chiba N, van Zanten SV, et al. The toronto consensus for the treatment of Helicobacter pylori infection in adults. Gastroenterology. 2016;151(1):51–69 e14. doi:10.1053/j.gastro.2016.04.006
8. Liu WZ, Xie Y, Lu H, et al. Fifth Chinese national consensus report on the management of Helicobacter pylori infection. Helicobacter. 2018;23(2):e12475. doi:10.1111/hel.2018.23.issue-2
9. Zhang YX, Zhou LY, Song ZQ, et al. Primary antibiotic resistance of Helicobacter pylori strains isolated from patients with dyspeptic symptoms in Beijing: a prospective serial study. World J Gastroenterol. 2015;21(9):2786–2792. doi:10.3748/wjg.v21.i9.2786
10. Zhou L, Zhang J, Song Z, et al. Tailored versus triple plus bismuth or concomitant therapy as initial helicobacter pylori treatment: a randomized trial. Helicobacter. 2016;21(2):91–99. doi:10.1111/hel.2016.21.issue-2
11. Xie C, Lu NH. Review: clinical management of Helicobacter pylori infection in China. Helicobacter. 2015;20(1):1–10. doi:10.1111/hel.12178
12. Cosme A, Lizasoan J, Montes M, et al. Antimicrobial susceptibility-guided therapy versus empirical concomitant therapy for eradication of Helicobacter pylori in a region with high rate of clarithromycin resistance. Helicobacter. 2016;21(1):29–34. doi:10.1111/hel.2016.21.issue-1
13. Beckman E, Saracino I, Fiorini G, et al. A novel stool PCR test for Helicobacter pylori may predict Clarithromycin resistance and eradication of infection at a high rate. J Clin Microbiol. 2017;55(8):2400–2405. doi:10.1128/JCM.00506-17
14. Pourakbari B, Mahmoudi S, Parhiz J, et al. High frequency of metronidazole and clarithromycin-resistant Helicobacter pylori in formalin-fixed, paraffin-embedded gastric biopsies. Br J Biomed Sci. 2018;75(2):61–65. doi:10.1080/09674845.2017.1391466
15. de Francesco V, Margiotta M, Zullo A, et al. Primary clarithromycin resistance in Italy assessed on Helicobacter pylori DNA sequences by TaqMan real-time polymerase chain reaction. Aliment Pharmacol Ther. 2006;23(3):429–435. doi:10.1111/apt.2006.23.issue-3
16. Hanafiah A, Binmaeil H, Raja Ali RA, Mohamed Rose I, Lopes BS. Molecular characterization and prevalence of antibiotic resistance in Helicobacter pylori isolates in Kuala Lumpur, Malaysia. Infect Drug Resist. 2019;12:3051–3061. doi:10.2147/IDR.S219069
17. Kouitcheu Mabeku LB, Eyoum Bille B, Tepap Zemnou C, Tali Nguefack LD, Leundji H. Broad spectrum resistance in Helicobacter pylori isolated from gastric biopsies of patients with dyspepsia in Cameroon and efflux-mediated multiresistance detection in MDR isolates. BMC Infect Dis. 2019;19(1):880. doi:10.1186/s12879-019-4536-8
18. Lee JY, Kim N, Nam RH, et al. Primary and secondary antibiotic resistance of Helicobacter pylori in Korea from 2003 to 2018. Helicobacter. 2019;e12660.
19. Patel SK, Pratap CB, Jain AK, Gulati AK, Nath G. Diagnosis of Helicobacter pylori: what should be the gold standard? World J Gastroenterol. 2014;20(36):12847–12859. doi:10.3748/wjg.v20.i36.12847
20. Krashias G, Bashiardes S, Potamitou A, Potamitis GS, Christodoulou C. Prevalence of Helicobacter pylori cagA and vacA genes in Cypriot patients. J Infect Dev Ctries. 2013;7(9):642–650. doi:10.3855/jidc.2923
21. Lin YA, Wang H, Gu ZJ, et al. Effect of CYP2C19 gene polymorphisms on proton pump inhibitor, amoxicillin, and levofloxacin triple therapy for eradication of Helicobacter pylori. Med Sci Monit. 2017;23:2701–2707. doi:10.12659/MSM.901514
22. Peng X, Song Z, He L, et al. Gastric juice-based real-time PCR for tailored Helicobacter pylori treatment: a practical approach. Int J Med Sci. 2017;14(6):595–601. doi:10.7150/ijms.18996
23. Afonina I, Zivarts M, Kutyavin I, et al. Efficient priming of PCR with short oligonucleotides conjugated to a minor groove binder. Nucleic Acids Res. 1997;25(13):2657–2660. doi:10.1093/nar/25.13.2657
24. Kim BJ, Kim JG. Substitutions in penicillin-binding protein 1 in amoxicillin-resistant Helicobacter pylori strains isolated from Korean patients. Gut Liver. 2013;7(6):655–660. doi:10.5009/gnl.2013.7.6.655
25. Gonzalez-Hormazabal P, Musleh M, Escandar S, et al. Prevalence of clarithromycin resistance in Helicobacter pylori in Santiago, Chile, estimated by real-time PCR directly from gastric mucosa. BMC Gastroenterol. 2018;18(1):91. doi:10.1186/s12876-018-0820-0
26. Lee SM, Kim N, Kwon YH, et al. rdxA, frxA, and efflux pump in metronidazole-resistant Helicobacter pylori: their relation to clinical outcomes. J Gastroenterol Hepatol. 2018;33(3):681–688. doi:10.1111/jgh.13906
27. Rimbara E, Noguchi N, Kawai T, Sasatsu M. Fluoroquinolone resistance in Helicobacter pylori: role of mutations at position 87 and 91 of GyrA on the level of resistance and identification of a resistance conferring mutation in GyrB. Helicobacter. 2012;17(1):36–42. doi:10.1111/hel.2011.17.issue-1
28. Wu JY, Kim JJ, Reddy R, et al. Tetracycline-resistant clinical Helicobacter pylori isolates with and without mutations in 16S rRNA-encoding genes. Antimicrob Agents Chemother. 2005;49(2):578–583. doi:10.1128/AAC.49.2.578-583.2005
29. Zhang YW, Hu WL, Cai Y, et al. Outcomes of furazolidone- and amoxicillin-based quadruple therapy for Helicobacter pylori infection and predictors of failed eradication. World J Gastroenterol. 2018;24(40):4596–4605. doi:10.3748/wjg.v24.i40.4596
30. Xie Y, Zhang Z, Hong J, et al. Furazolidone-containing triple and quadruple eradication therapy for initial treatment for Helicobacter pylori infection: a multicenter randomized controlled trial in China. Helicobacter. 2018;23(5):e12496. doi:10.1111/hel.2018.23.issue-5
31. Djennane-Hadibi F, Bachtarzi M, Layaida K, et al. High-level primary clarithromycin resistance of Helicobacter pylori in Algiers, Algeria: a prospective multicenter molecular study. Microb Drug Resist. 2016;22(3):223–226. doi:10.1089/mdr.2015.0209
32. Hakemi Vala M, Eyvazi S, Goudarzi H, Sarie HR, Gholami M. Evaluation of clarithromycin resistance among Iranian Helicobacter pylori isolates by E-test and real-time polymerase chain reaction methods. Jundishapur J Microbiol. 2016;9(5):e29839. doi:10.5812/jjm
33. Dzierzanowska-Fangrat K, Rozynek E, Jozwiak P, et al. Primary resistance to clarithromycin in clinical strains of Helicobacter pylori isolated from children in Poland. Int J Antimicrob Agents. 2001;18(4):387–390. doi:10.1016/S0924-8579(01)00421-6
34. Agudo S, Perez-Perez G, Alarcon T, Lopez-Brea M. High prevalence of clarithromycin-resistant Helicobacter pylori strains and risk factors associated with resistance in Madrid, Spain. J Clin Microbiol. 2010;48(10):3703–3707. doi:10.1128/JCM.00144-10
35. Chang YW, Ko WJ, Oh CH, et al. Clarithromycin resistance and female gender affect Helicobacter pylori eradication failure in chronic gastritis. Korean J Intern Med. 2019;34(5):1022–1029. doi:10.3904/kjim.2018.054
36. Kim SE, Park MI, Park SJ, et al. Trends in Helicobacter pylori eradication rates by first-line triple therapy and related factors in eradication therapy. Korean J Intern Med. 2015;30(6):801–807. doi:10.3904/kjim.2015.30.6.801
37. Park CG, Kim S, Lee EJ, Jeon HS, Han S. Clinical relevance of point mutations in the 23S rRNA gene in Helicobacter pylori eradication: a prospective, observational study. Medicine (Baltimore). 2018;97(33):e11835. doi:10.1097/MD.0000000000011835
38. Chen Q, Zhang W, Fu Q, et al. Rescue therapy for helicobacter pylori eradication: a randomized non-inferiority trial of amoxicillin or tetracycline in bismuth quadruple therapy. Am J Gastroenterol. 2016;111(12):1736–1742. doi:10.1038/ajg.2016.443
39. Ashida K, Honda Y, Sanada K, Takemura Y, Sakamoto S. The safety and effectiveness of vonoprazan-based Helicobacter pylori eradication therapy; a prospective post-marketing surveillance. Expert Opin Drug Saf. 2019;18:1–7.
40. Mansour-Ghanaei F, Samadi A, Joukar F, et al. Efficacy and tolerability of fourteen-day sequential quadruple regimen: pantoprazole, bismuth, amoxicillin, metronidazole and or furazolidone as first-line therapy for eradication of Helicobacter pylori: a randomized, double-blind clinical trial. EXCLI J. 2019;18:644–652. doi:10.17179/excli2019-1613
41. Gebeyehu E, Nigatu D, Engidawork E. Helicobacter pylori eradication rate of standard triple therapy and factors affecting eradication rate at Bahir Dar city administration, Northwest Ethiopia: a prospective follow up study. PLoS One. 2019;14(6):e0217645. doi:10.1371/journal.pone.0217645
42. Silva GM, Silva HM, Nascimento J, et al. Helicobacter pylori antimicrobial resistance in a pediatric population. Helicobacter. 2018;23(5):e12528. doi:10.1111/hel.12528
43. Dekhnich N, Ivanchik N, Kozlov R, et al. Dynamics of antimicrobial resistance of Helicobacter pylori isolates in the Smolensk region of Russian Federation. Helicobacter. 2018;23(6):e12545. doi:10.1111/hel.2018.23.issue-6
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.