Back to Journals » International Journal of General Medicine » Volume 15
Epidemiology of End-Stage Renal Disease in Mogadishu, Somalia: First Report at a Tertiary Care Hospital
Authors Mohamed AH , Jeele MOO
Received 26 May 2022
Accepted for publication 15 July 2022
Published 21 July 2022 Volume 2022:15 Pages 6259—6267
DOI https://doi.org/10.2147/IJGM.S375280
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Abdikarim Hussein Mohamed,1 Mohamed Osman Omar Jeele2
1Urology Department, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Somalia; 2Internal Medicine Department, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Somalia
Correspondence: Abdikarim Hussein Mohamed, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Somalia, Tel +252 61 516 7182, Email [email protected]
Background: End-stage renal disease (ESRD) in Somalia remains unexamined due to a lack of a national registry system, and the impact of the disease in the country is not estimated yet. The present study is the first report that aims to evaluate the epidemiological characteristics, causes, and dialysis-related factors associated with readmissions in ESRD patients who were going to routine hemodialysis.
Patients and methods: This cross-sectional observational study enrolled 208 patients with ESRD. Also, this study investigated patients readmitted to the hospital (n=135) after they enrolled in hemodialysis. The sociodemographic characteristics, risk factors, and comorbidities associated with these patients were reviewed. Admission site, length of hospital stay, outcome, and dialysis-related factors associated with readmissions in the first six months after being on a regular hemodialysis program were also assessed.
Results: The mean age of the patients was 52.7± 15.0 years, 43.3% were > 60 years, and 61.5% were male. The most common cause was diabetes at 39.4%, followed by hypertension (35.6%) and 12.5% for postrenal obstruction. The prevalence of 6-month hospital readmissions was 65%. The most common dialysis-related factor associated with readmissions was uremic complications due to missed hemodialysis sessions (40%), vascular access/catheter infection (20%), and anemia (17.8%) (95% CI: 0.825– 5.357, OR: 3.017, p< 0.04). Female cases were more vulnerable to vascular catheter site infection, anemia, and hyponatremia (p< 0.001). 27.5% of the patients were admitted to the intensive care unit (ICU), and the most common reason for ICU admissions was pulmonary edema (53.8%), sepsis (42.8%), and uremia due to hemodialysis skip (26.4%) (95% CI: 1.507– 13.632, OR: 2.08, p=0.01). The mortality rate was 5.2%.
Conclusion: The prevalence of unplanned hospital readmissions within six months was very high, and a missed hemodialysis session was identified as the leading cause. Inadequate knowledge, wrong social beliefs about the concept of dialysis and a lack of a health insurance system that covers the higher costs of each dialysis session are believed to be the causes of missed dialysis occasions.
Keywords: end-stage renal disease, Sub-Saharan Africa, hemodialysis
Introduction
End-stage renal disease (ESRD) is defined as a significant reduction in the kidney’s ability to function properly, as well as a glomerular filtration rate of less than 15mL/min.1 Even though the prevalence of chronic kidney disease (CKD) in Somalia was not examined before, CKD in sub-Saharan Africa was found to be 6.8% in 2020, as reported by Muiru et al.2
CKD is becoming the leading cause of mortality, associated with increased cardiovascular morbidity and mortality.3 The mortality rate of ESRD is very high, with about 20 to 50% deaths in the first 24 months. Cardiovascular disease is considered the most common cause of death in CKD patients.4
Well-established risk factors for CKD include diabetes, hypertension, metabolic syndrome, and obesity.3
Patients with end-stage renal disease going to routine hemodialysis (HD) programs are often more vulnerable to being hospitalized and readmitted than the general population.5 İt is said that in 2018, 34% of patients going to hemodialysis in the United States were readmitted to the hospital in just 30 days.6,7
The hospital readmissions will impact the quality of life of the patients negatively and will increase the morbidity and mortality of ESRD patients.7–9 Also, these readmissions burden the emplaced health system as they will increase the annual cost of ESRD patient care worldwide.10 Hence, reducing the possibility of readmissions in HD patients became an essential part of the patients’ management for the clinicians and the policymakers.11
İn Somalia, a country that has a long history of civil war, there is a lack of a health insurance system that covers and monitors the annual cost of ESRD patients.12 Needless to say, decreasing the readmission possibilities will not only improve their quality of life but also manage the financial burden of the patients.
The prevalence, causes, and reasons associated with unplanned readmission of ESRD patients in Somalia remain unexamined. Therefore, the present study is the first report that aims to evaluate the epidemiological characteristics, causes, and dialysis-related factors associated with readmissions in ESRD patients who were going to routine hemodialysis.
Method
This cross-sectional observational study enrolled all end-stage renal disease patients in the maintenance hemodialysis program at Mogadishu Somalia Turkish Training and Research Hospital (the only referral dialysis center in Mogadishu) from 1 July 2021 to 1 January 2022. A total of 208 patients with ESRD who are going on routine hemodialysis programs were included in the study. Also, this study investigated patients readmitted to the hospital (n=135) after enrolling in the hemodialysis program for any reason, regardless of age and sex, to include in this study. Acute renal failure, those patients with chronic renal failure not needing renal replacement therapy, and patients with missed data were excluded from the study.
The sociodemographic and clinical characteristics of the patients (age, gender, hemodialysis duration and sessions per week, hemodialysis site (fistula, graft, and hemodialysis catheter), hemodialysis compliance of the cases either regular or skip, defined of hemodialysis miss of ≥ two times per month, hemodialysis cost funding, quality of life, diet and medication compliance), risk factors and comorbidities associated with ESRD recruited from electronic medical records on hospital information system (HIS) were studied among the patients at hemodialysis program. Patients were grouped into four categories: <18 years, 19–39 years, 40–59 years, and >60 years old. The authors recognized a poor quality of life in patients with ESRD who lost their preceded work due to chronicity of the disease, work absenteeism, lack of public awareness of the disease and the hemodialysis itself, discrimination, and social pressure on the patients.
Risk factors for ESRD assessed were included diabetes, hypertension, postrenal obstruction (Stone, cancers, and others), glomerular diseases based on the presence of proteinuria and absence of other identifiable causes, medications (analgesics use), cystic renal disease (polycystic kidney disease), and idiopathic etiology.
Regarding assessment for reasons associated with readmissions; admission site, duration of hospital stay, cost of hospital stay, outcome (recovered, not improved, and death), and dialysis-related factors associated with readmissions in the first six months after being on routine hemodialysis program were among the extracted data from HIS using date and ICD-10 codes. The definition of not improved was taken as the patients who did not die during the study and did not improve to the level of discharging them from the hospital. If a patient were readmitted multiple times, we counted his first unplanned readmission.
This study was carried out according to the Helsinki Declaration and was approved by Mogadishu Somalia Turkish Training and Research Hospital’s ethical committee (REF. MSTH-6745). The study’s objective was explained in detail to the participants, all patients, and the parents of the patients under 18 years obtained and signed written informed consent. Statistical analyses were used in the Statistical Package for Social Sciences ((SPSS v23, IBM, Armonk, NY, USA)) software. The frequencies and proportions were presented as point estimates in categorical variables, while the mean ±SD was employed in quantitative variables. A bivariate analysis was performed to assess the association between independent and dependent variables. A p-value of <0.05 was considered statistically significant. The odds ratios (ORs) and their 95% confidence intervals (CIs) were calculated. The multivariate logistic regression model exhibited variables that showed statistical significance under the bivariate analysis.
Results
This study included 270 patients going to regular hemodialysis at Mogadishu Somali Turkish Research and Training Hospital. A final number of 208 patients who did not have any missing data and gave their consent to participate in the study were examined.
The epidemiological characteristics of the patients were evaluated; the mean age was 52.7±15.0 years, with a range of 14–86 years old. Most cases were elderly (>60 years), accounting for 43.3%, and 128 cases were male, representing 61.5% of the patients. The hemodialysis status of the patients was as follows; 37.5% of the cases were on a hemodialysis program for 2–3 years, 28.8% for > 3 years, 74.5% had arteriovenous fistula, and 21.2% had hemodialysis catheter. One hundred fifty-eight patients (76%) underwent two sessions of hemodialysis per week. Regarding hemodialysis compliance of the patients, 93.3% of the cases had good compliance since 57, 7% of the funding themselves, without health insurance, although 94.2% living with poor quality of life. Nearly two-thirds of the cases had no regular diet control (eating a salt and sugar diet), though more than two-thirds had good medication compliance. Table 1 summarizes the sociodemographic and clinical characteristics of the patients.
 |
Table 1 The Sociodemographic and Clinical Characteristics of the Patients |
Causes of ESRD were assessed; the most common cause was diabetes in 39.4% (n=82), followed by hypertension (n=74, 35.6%), 12.5% for postrenal obstruction (Stone=17, cancers=9), glomerular disease in 4.8%, medications and cystic renal disease in 1% each, and 5.7% for unknown cause. Diabetes was the leading cause of ESRD in all age categories and gender groups (except those younger than 18 years old). Table 2 shows the distribution of causes associated with ESRD.
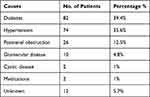 |
Table 2 Distribution of Causes Associated with ESRD |
As illustrated in Figure 1, the most common comorbidity associated with these patients was hypertension in 56.7%, heart failure in 27.9%, dyslipidemia in 26%, diabetes in 17.3%, ischemic heart disease in 11.5% and 1.5% had cerebrovascular disease.
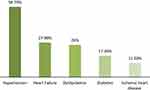 |
Figure 1 The most common comorbidities associated with ESRD patients. |
A total of 135 cases were readmitted, of which 54.8% (n=74) were male and 45.2% (n=61) were female (95% CI: 0.89–1.58, OR: 1.03, p=0.36). There was a statistically significant variation in age among readmitted patients, 48.9% of them (n=66) were aged 60, and over, 28.1% (n=38) were between 40 and 59 years old (95% CI: 1.01–1.58, OR: 1.23, p<0.02). This result indicates that an increase in the patient’s age will increase the possibility of readmission (Table 3).
 |
Table 3 Characteristics of Readmitted Patients |
Throughout the study; dialysis-related factors associated with readmission were examined, and found that 40% (n=54) of the cases had uremic complications (ie, confusion, pericarditis) due to missed hemodialysis session, 20% (n=27) had vascular access/catheter infection, 17.8% (n=24) had anemia, 10.4% (n=14) had pulmonary edema, and 5.9% (n=8) had hyponatremia (95% CI: 0.825–5.357, OR: 3.017, p<0.04). As shown in Figure 2, Female cases were more vulnerable to vascular catheter site infection (15/27), anemia (13/23), and hyponatremia (6/8) (95% CI: 1.234–9.648, OR: 3.26, p<0.001).
 |
Figure 2 Dialysis-related factors associated with readmissions regarding gender distribution. |
Concerning the admission site, 72.5% of the cases were admitted in the inpatient ward and 27.5% in the ICU. The most common reason for ICU admission was pulmonary edema (53.8%), sepsis (42.8%), uremic complications due to hemodialysis skip (26.4%), anemia (13%), and vascular catheter site infection in 12.5% (95% CI: 1.507–13.632, OR: 2.08, p=0.01).
The mean hospital stay in our study was 7.04±4.75 days with a medium range of 2 to 26 days. Half of the patients (54.8%) stayed in the hospital for 3–7 days, 25.9% for> eight days, and 19.3% in 1–3 days. The hospital stay of the patients who followed up in the intensive care unit was statistically significantly higher than the inpatient clinic patients, 40% vs 16% in > 8 days (95% CI: 0.94–2.53, 1.83, p=0.004). Also, a statistically significant difference was found between the hemodialysis duration of the cases according to the length of hospital stay, > 8 days hospital stay in 32% for hemodialysis duration > 2 years (p=0.010). There was no statistically significant association between risk factors for readmission and length of hospital stay (p=0.074).
Regarding the outcome of the patients; 91.8% of the patients were recovered successfully, four patients were not improved, and the mortality rate of our study was 5.2% of the cases (n=7), three patients had sepsis, two patients with skip dialysis, one with pulmonary edema, and patient with vascular catheter site infection were those who passed away (95% CI: 1.12–2.44, OR: 1.46, p<0.001).
The hospital costs of the cases ranged from 103 to 3050 dollars, averaging 465.10±407.01 dollars.
Discussion
End-stage renal disease is a public health challenge, particularly in low-income Sub-Saharan African countries. The prevalence, causes, and dialysis-related factors associated with unplanned readmission of ESRD patients in Somalia remain unexamined due to a lack of a national registry system, and the impact of the disease in the country is not estimated yet. The present is the first study aimed at evaluating the epidemiological characteristics, causes, and predisposing factors associated with readmissions in ESRD patients who are going to routine hemodialysis at a tertiary hospital in Mogadishu, Somalia.
In our study, the most common cause of ESRD was diabetes in 39.4%, the leading cause of ESRD in all age categories and gender groups, followed by hypertension (35.6%). Analysis of the Taiwan Renal Registry Data System (TWRDS) database from 2005 to 2012 revealed that diabetes was found in up to 47.9% of the cases.13 Another study from Egypt involved 1559 patients on routine hemodialysis, unknown etiology, and hypertension were responsible for 25% and 21.4% of ESRD, respectively.14 Variations of the causes were noticed in a study reported from Mexico; young patients (20–40 years) initiated for RRT were a result of an unknown cause (70%), whereas the elderly group (50–70 years) were a result of diabetes and hypertension in 60%, which coheres with our study findings.15 A survey of 20 countries in Latin America over ten years declared that diabetes remains the most common cause of ESRD, which coheres with our study findings.16 Public health awareness, early diagnosis, and management of diabetes and hypertension should include the most crucial steps for ESRD prevention.
Two-thirds of the ESRD cases in our study were male, and a similar male predominance was observed in a large national population-based cohort study from Korea that detected the number of male patients (58.5%) tended to be higher than that of females.16 A cross-sectional study from Palestine revealed that 57.7% of their cases were male, which supports the results of the current study.17
ESRD is a worldwide concern, resulting in undesirable impacts for patients, their families, and society. Its incidence and prevalence are progressively rising due to the increase in the leading causes of diabetes and hypertension, though they can be prevented. Nearly two-thirds of our cases have no regular diet control (eating salt and sugar daily) without regular exercise. The estimated annual cost of ESRD is $32.9 billion.18 Due to limited resources in our country, our center is the sole functional dialysis center available in the whole countryside, where the rest there is no available renal replacement therapy. Patients who were in the dialysis program had to spend the expenses by themselves (58%) or for the help of other charities.
Thirty-day hospital readmission for patients going to the hemodialysis program is about 34%.6,7 Several risk factors are associated with increased readmission rates, including anemia, hypoalbuminemia, catheter vascular access malfunctions, comorbidities such as heart failure, and myocardial infarction.19 S, Yetti K. reported that poor hemodialysis compliance and anemia were significantly correlated with hospital readmission.20 A retrospective study concerning 30-day hospital readmissions of a total of 189 patients by Plantinga LC et al said that 44% of readmissions were due to pulmonary edema.21
The prevalence of 6-month dialysis-related hospital readmissions in our study was 65%. The most common predisposing factor was found to be uremic complications due to missed hemodialysis sessions, followed by vascular access/catheter infection, anemia, and pulmonary edema. Renal replacement therapy, including hemodialysis and peritoneal dialysis, is the primary life-saving treatment for ESRD patients. Unfortunately, there is a lack of access to dialysis services for more than 63% of CKD patients in low and lower-middle-income countries. Nearly 7 million ESRD cases die due to a lack of dialysis accessibility.22 Missed hemodialysis sessions were responsible for the overcrowding of our center for receiving many ESRD patients needing regular renal replacement therapy, lack of public awareness of the disease and the hemodialysis itself, discrimination, and social pressure on the patients. In addition to this, inadequate skills of dialysis providers, higher costs belonging to each dialysis session that most of the patients are not affordable (low socioeconomic status), as well as lack of access to the center because of rural and far distance distribution of the cases were also the principal causes of missed dialysis occasions. These hospital readmissions pose an increased financial cost to the patients; the hospital costs of our cohort ranged from 103 to 3050 dollars, with an average of 465.10±407.01 dollars.23
Besides the advancements in the management of ESRD in the manner of hemodialysis (presently, about 2 million individuals are in maintenance hemodialysis programs worldwide, which represents only 10% of the patients), the mortality rate of these patients is high compared to that of general of the population (from 6% in Morocco, 10.4% in Tunisia, and 12% in Algeria).24 In Sub-Saharan African countries, few studies reported the mortality rate. In a study of a total of 661 hemodialysis patients from Cameroon, the death rate at one year of follow-up was 26.8%.25 The mortality rate among patients varied between the nations. The mortality rate of readmitted patients in our study was 5.2% of the cases (n=7). We recommend the immediate establishment and facilitation of the patients for numerous dialysis centers in the country to properly serve, reduce preventable causes of unplanned readmissions, and improve their quality of life.
This study has several limitations: first, it is a single-center study; there are no capable hemodialysis centers eligible for the patients throughout the country (to date, only our center is the only referral center available which faces overcrowding), and underreporting is probable. The type of glomerular disease was not determined due to the unavailability of biopsies. Peritoneal dialysis and kidney transplantation are not available in Somalia. Besides these limitations, ESRD patients in Somalia remain unexamined due to a lack of a national registry system, and the impact of the disease in the country is not estimated yet. This present is the first study to evaluate the epidemiological characteristics, causes, and dialysis-related factors associated with readmissions in ESRD patients who are going to routine hemodialysis.
Conclusion
The prevalence of unplanned hospital readmissions within six months was higher than in many other Sub-Saharan African countries, and a missed hemodialysis session was identified as the leading cause. Uremic complications due to missed hemodialysis sessions were responsible for 40% of unplanned hospital readmissions in our study. Inadequate knowledge, wrong social beliefs about the concept of dialysis, and lack of a health insurance system that covers the higher costs of each dialysis session are believed to be the causes of missed dialysis occasions. Future studies will identify the exact reasons behind the missed hemodialysis sessions.
Abbreviations
CRF, chronic renal failure; ESRD, End stage renal disease; HD, hemodialysis; HIS, hospital information system; TWRDS, Taiwan Renal Registry Data System.
Institutional Review Board Statement
This study was carried out according to the Helsinki Declaration and was approved by Mogadishu Somalia Turkish Training and Research Hospital’s ethical committee (REF. MSTH-6745).
Data Sharing Statement
Data included in the manuscript.
Informed Consent Statement
The objective of the study was explained in detail to the patients and the parents of underage patients and all patients obtained informed consent.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Scott IA, Scuffham P, Deepali Gupta TM, Harch JB, Richards B. Going digital: a narrative overview of the effects, quality and utility of mobile apps in chronic disease self-management. Aust Health Rev. 2018;44(1):62–82. doi:10.1071/AH18064
2. Muiru AN, Charlebois ED, Balzer LB, et al. The epidemiology of chronic kidney disease (CKD) in rural East Africa: a population-based study. PLoS One. 2020;15(3):e0229649. doi:10.1371/journal.pone.0229649
3. Vinhas J, Gardete-Correia L, Boavida JM, et al. Prevalence of chronic kidney disease and associated risk factors, and risk of end-stage renal disease: data from the PREVADIAB study. Nephron Clin Pract. 2011;119(1):c35–c40. doi:10.1159/000324218
4. Genovesi S, Porcu L, Luise MC, et al. Sudden death in end stage renal disease: comparing hemodialysis versus peritoneal dialysis. Blood Purif. 2017;44(1):77–88. doi:10.1159/000464347
5. Li J, Huang N, ZhongZhong D, Wang ZA, Jiang L, Huang F. Risk factors and outcomes of cardiovascular disease readmission within the first year after dialysis in peritoneal dialysis patients. Ren Fail. 2021;43(1):159–167. doi:10.1080/0886022X.2020.1866009
6. Mathew AT, Rosen L, Pekmezaris R, et al. Potentially avoidable readmissions in United States hemodialysis patients. Kidney Int Rep. 2018;3(2):343–355. doi:10.1016/j.ekir.2017.10.014
7. Saran R, Bruce Robinson, Abbott KC, et al. US renal data system 2016 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2017;69(3):A7–A8. doi:10.1053/j.ajkd.2016.12.004
8. Li J, Jing Y, Huang N, et al. Prevalence, risk factors and impact on outcomes of 30-day unexpected rehospitalization in incident peritoneal dialysis patients. BMC Nephrol. 2021;22(1):1–9. doi:10.1186/s12882-020-02201-0
9. Plantinga LC, King L, Patzer RE, et al. Early hospital readmission among hemodialysis patients in the United States is associated with subsequent mortality. Kidney Int. 2017;92(4):934–941. doi:10.1016/j.kint.2017.03.025
10. Perl J, McArthur E, Bell C, et al. Dialysis modality and readmission following hospital discharge: a population-based cohort study. Am J Kidney Dis. 2017;70(1):11–20. doi:10.1053/j.ajkd.2016.10.020
11. Harel Z, Wald R, McArthur E, et al. Rehospitalizations and emergency department visits after hospital discharge in patients receiving maintenance hemodialysis. J Am Soc Nephrol. 2015;26(12):3141–3150. doi:10.1681/ASN.2014060614
12. Jeele MO, Addow RO, Adan FN, Jimale LH. Prevalence and risk factors associated with hepatitis B and hepatitis c infections among patients undergoing hemodialysis: a single-centre study in Somalia. Int J Nephrol. 2021;13. doi:10.1155/2021/1555775
13. Lin YC, Hsu CY, Kao CC, et al. Incidence and prevalence of ESRD in Taiwan renal registry data system (TWRDS): 2005–2012. ActaNephrologica. 2014;28(2):65–68.
14. El-Arbagy AR, Yassin YS, Boshra BN. Study of prevalence of end-stage renal disease in Assiut governorate, upper Egypt. Menoufia Med J. 2016;29(2):222. doi:10.4103/1110-2098.192441
15. Gonzalez-Bedat M, Rosa-Diez G, Pecoits-Filho R, et al. Burden of disease: prevalence and incidence of ESRD in Latin America. ClinNephrol. 2015;83(7 Suppl 1):3–6.
16. Choi HS, Han KD, Oh TR, et al. Trends in the incidence and prevalence of end-stage renal disease with hemodialysis in entire Korean population: a nationwide population-based study. Medicine. 2021;100(13):e25293.
17. Khader MI, Snouber S, Alkhatib A, Nazzal Z, Dudin A. Prevalence of patients with end-stage renal disease on dialysis in the West Bank, Palestine. Saudi J Kidney Dis Transplant. 2013;24(4):832. doi:10.4103/1319-2442.113913
18. Malekmakan L, Tadayon T, Roozbeh J, Sayadi M. End-stage renal disease in the Middle East: a systematic review and meta-analysis. Iran J Kidney Dis. 2018;12(4):195.
19. Assimon MM, Flythe JE. Thirty-day hospital readmissions in the hemodialysis population: a problem well put, but half-solved. Clin J Am Soc Nephrol. 2017;12(10):1566–1568. doi:10.2215/CJN.08810817
20. Wjayantii S, Yetti K. Analysis of the factors affecting the hospital readmission incidence of hemodialysis patients in Bandar Lampung, Indonesia. Enfermeriaclinica. 2019;29:720–724.
21. Plantinga LC, Masud T, Lea JP, Burkart JM, O’Donnell CM, Jaar BG. Post-hospitalization dialysis facility processes of care and hospital readmissions among hemodialysis patients: a retrospective cohort study. BMC Nephrol. 2018;19(1):1–10. doi:10.1186/s12882-018-0983-5
22. Ejaz A, Junejo AM, Ali M, Ashfaq A, Hafeez AR, Khan SA. Outcomes of dialysis among patients with End-Stage Renal Disease (ESRD). Cureus. 2021;13(8):e17006.
23. Mathew AT, Strippoli GF, Ruospo M, Fishbane S. Reducing hospital readmissions in patients with end-stage kidney disease. Kidney Int. 2015;88(6):1250–1260. doi:10.1038/ki.2015.307
24. Msaad R, Essadik R, Mohtadi K, et al. Predictors of mortality in hemodialysis patients. Pan Afr Med J. 2019;33. doi:10.11604/pamj.2019.33.61.18083
25. Halle MP, Ashuntantang G, Kaze FF, Takongue C, Kengne AP. Fatal outcomes among patients on maintenance haemodialysis in sub-Saharan Africa: a 10-year audit from the Douala General Hospital in Cameroon. BMC Nephrol. 2016;17(1):1–9. doi:10.1186/s12882-016-0377-5
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
