Back to Journals » Infection and Drug Resistance » Volume 15
Epidemiology of Carbapenem-Resistant Enterobacterales Infection and Colonization in Hospitalized Patients at a University Hospital in Thailand
Authors Wangchinda W , Laohasakprasit K, Lerdlamyong K, Thamlikitkul V
Received 3 February 2022
Accepted for publication 9 April 2022
Published 25 April 2022 Volume 2022:15 Pages 2199—2210
DOI https://doi.org/10.2147/IDR.S361013
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Walaiporn Wangchinda, Kanokwan Laohasakprasit, Kanokorn Lerdlamyong, Visanu Thamlikitkul
Division of Infectious Diseases and Tropical Medicine, Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Visanu Thamlikitkul, Division of Infectious Diseases and Tropical Medicine, Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, 2 Wanglang Road, Bangkoknoi, Bangkok, 10700, Thailand, Tel +66 81-820-6271, Fax +66 2-412-5994, Email [email protected]
Purpose: To investigate the epidemiology of carbapenem-resistant Enterobacterales (CRE) colonization or CRE infection relative to the natural history and clinical course of CRE colonization or CRE infection in hospitalized patients during admission and after discharge.
Material and Methods: Two adult cohorts were enrolled. Cohort I comprised hospitalized patients who had CRE isolated from their clinical specimens during 2018– 2020. CRE colonization or CRE infection was based on the absence/presence of clinical features of infection. Information regarding the natural history and clinical course of these patients was collected during hospitalization. Stool samples were evaluated for CRE once a week during hospitalization, and then once every few months after discharge until negative for CRE. Cohort II comprised patients who had CRE isolated from clinical specimens during hospitalization and who were discharged during 2015– 2018. CRE in stool samples collected from these patients every few months was assessed to determine duration of CRE in stool.
Results: CRE in stool was detected in 69.7% of 353 patients in cohort I. K. pneumoniae was the predominant CRE isolated from clinical samples (76.8%) and stool samples (65.7%). Among the 225 CRE-colonized patients, 20.4% developed subsequent CRE infections with a median duration from CRE colonization to CRE infection of 14 days. Among 174 CRE-infected patients, the most common infection was pneumonia with mortality at discharge of 47.7%. Duration of CRE colonization in stool was < 1 year in 50.0% of cohort I patients, and < 2 years in 91.4% of patients in cohort II.
Conclusion: CRE isolated from clinical specimens in hospitalized patients are more likely to cause colonization than infection. Patients with CRE colonization are at risk of subsequent CRE infection with high mortality. Stool culture for CRE is needed to verify if contact precautions can be discontinued because the duration of CRE colonization in stool varied from days to years.
Keywords: epidemiology, carbapenem-resistant Enterobacterales, infection, colonization, patients, university hospital, Thailand
Introduction
Enterobacterales are Gram-negative bacilli that inhabit the gastrointestinal tract of humans and animals. The occurrence of carbapenem-resistant Enterobacterales (CRE) is being increasingly reported worldwide and has become a significant threat to public health.1,2 According to Thailand’s National Antimicrobial Resistance Surveillance of antimicrobial resistance, the carbapenem resistance rate of Escherichia coli and Klebsiella pneumoniae has increased from 0.5% in 2014 to 3.2% in 2020, and 3.3% in 2015 to 11.7% in 2020, respectively.3 The major drivers of CRE acquisition include healthcare exposures and receiving broad-spectrum antibiotics, especially carbapenems.4,5 CRE can colonize in the gastrointestinal tract and other areas of the human body without features of infection, especially in hospitalized and previously hospitalized patients. Individuals with CRE colonization are at risk of developing CRE infection, which is difficult to treat due to the limited number of effective antibiotics, and this results in high mortality among CRE-infected patients.6 Patients with CRE colonization or infection are reservoirs of CRE, and CRE from these patients can be transmitted to other patients, to their family members, to healthcare personnel, and to the environment.7 Therefore, infection prevention and control (IPC) measures, especially contact precautions, such as isolation of CRE-colonized or CRE-infected patients in a single room or cohort area, healthcare personnel using personal protective equipment (PPE) whenever they are in contact with known CRE-colonized or CRE-infected patients, and cleaning of the surrounding environment, must be implemented to prevent transmission of CRE.8 As a result, management of CRE-infected patients and implementation of the aforementioned IPC measures to be employed for CRE-colonized and CRE-infected patients requires a large amount of resources. Any patient at our center who has or once had CRE isolated from any site of his/her body will have the acronym “CRE” stamped on his/her medical record to inform/remind relevant healthcare personal to employ contact precautions. These precautions are to be observed to determine whether the patient is hospitalized or ambulatory, and whether the patient is currently CRE-positive or CRE-negative. In addition to these recommended protocols for interacting with current or former CRE patients being cost-, resource-, and labor-intensive, they also have a stigmatizing effect that adversely affects both healthcare personnel and the patient. Hence, information specific to the epidemiology of CRE colonization or infection in healthcare setting is needed to determine the level of risk, and to guide the development and implementation of effective and efficient measures to prevent and contain CRE colonization and CRE infection in hospitalized patients.
The aim of this study was to investigate the epidemiology of CRE colonization or CRE infection relative to the natural history and clinical course of CRE colonization or CRE infection in hospitalized patients during admission and after discharge from the hospital.
Materials and Methods
The protocol for this study was approved by the Institutional Review Board of the Faculty of Medicine Siriraj Hospital, and it was conducted in accordance with the principles and guidelines set forth by the 1964 Declaration of Helsinki and all of its subsequent amendments. The study was conducted between November 2018 and November 2020 at Siriraj Hospital, which is a 2300-bed tertiary care university hospital located in Bangkok, Thailand. Written informed consent was obtained from all enrolled patients.
This study included two cohorts of patients in order to determine the natural history and clinical course of patients with CRE colonization or CRE infection during hospitalization and after discharge from the hospital.
Cohort I consisted of hospitalized patients aged ≥18 years who had CRE isolated from clinical specimens submitted to the microbiology laboratory on randomly selected surveillance days from 2018 to 2020. Those patients were classified as CRE-colonized patients or CRE-infected patients based on the absence (CRE colonization) or presence (CRE infection) of clinical features of infection at the time of collection of CRE-positive clinical specimens. Information specific to the natural history and clinical course of CRE-colonized or CRE-infected patients was collected during hospitalization and until hospital discharge. Medical management of all CRE-colonized patients or CRE-infected patients was determined by each patient’s attending physicians. Antibiotic therapy and the outcome of treatment in CRE-infected patients were also observed. Stool or rectal swab samples collected from each enrolled patient were transported to the laboratory in Cary-Blair transport medium for CRE culture once a week until the patient was discharged from the hospital or died. Stool samples of patients who still had CRE on their stools before hospital discharge were collected every few months by the patient or a relative. The stool samples collected at home were stored in Cary-Blair transport medium and sent to the research team for detection of CRE until their stool samples were negative for CRE.
Cohort II consisted of patients aged ≥18 years who had CRE isolated from clinical specimens submitted to the microbiology laboratory and who were discharged from hospital between 2015 and 2018. The aim of cohort II was to determine the duration of CRE colonization in the gastrointestinal tract. Stool samples were collected at home by the patient or a relative. Stool samples were stored in Cary-Blair transport medium and sent to the research team for detection of CRE until their stool samples were negative for CRE.
The collected stool or rectal swab sample from each patient in cohort I during hospitalization was determined for the presence of CRE at the microbiology laboratory of the Division of Infectious Diseases and Tropical Medicine, Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University. Briefly, the sample was inoculated onto MacConkey agar supplemented with ceftriaxone 4 mg/L, and then incubated at 35°C for 18 hours. Bacterial colonies grown on ceftriaxone supplemented agar were identified by species of Enterobacterales and antimicrobial susceptibility to carbapenems (ertapenem, meropenem, and imipenem) by disk diffusion method, according to the Clinical and Laboratory Standards Institute (CLSI) guidelines.9 CRE was defined as Enterobacterales that were resistant to at least one of the three tested carbapenems. Detection of CRE in stool samples collected at and sent from home was performed using chromogenic selective agar to detect CRE directly from clinical specimen (CHROMagar mSuperCARBATM, CHROMagar Company, Paris, France). Briefly, the stool or rectal swab sample was inoculated onto chromogenic selective agar and then incubated at 35°C for 18–24 hours. A positive CRE result was characterized by the presence of blue or pink colonies on the chromogenic selective agar after incubation. Species identification of blue or pink colonies was performed using conventional biochemical tests. Determination of suspected carbapenemase production in Enterobacterales was screened for by using the modified carbapenem inactivation method.9 Phenotypic screening of carbapenemases was performed by double-disc synergy of phenylboronic acid or EDTA with meropenem.10–12
Statistical Analysis
The data were analyzed using SPSS Statistics version 16.0 (SPSS, Inc., Chicago, IL, USA). Comparisons of categorical data were performed using Fisher’s exact test or chi-square test, and the results are shown to be number and percentage. Comparisons of continuous data were performed using Student’s t-test for normally distributed data, and using Mann–Whitney U-test for non-normally distributed data. The results of those comparisons are presented as mean plus/minus standard deviation and median and range, respectively. A p-value less than or equal to 0.05 was considered statistically significant for all tests.
Results
Demographic and Clinical Characteristics of Patients in Cohort I
A total of 353 patients who met the eligibility criteria for this study were included between November 2018 and November 2020. The enrolled study population included 225 CRE-colonized patients (63.7%) and 128 CRE-infected patients (36.3%) at the time of CRE detection from patient clinical specimens.
Demographic and clinical characteristics of all study patients in cohort I (N = 353), and compared between CRE-colonized patients and CRE-infected patients are shown in Table 1. The mean age was 66.7 years, and just over half were male. The vast majority of patients had comorbid conditions (92.9%) and had received prior antimicrobials within the preceding 3 months before isolation of CRE (98.9%). Intensive care unit (ICU) admission was significantly more frequent in CRE-infected patients than in CRE-colonized patients. In contrast, CRE-colonized patients had a significantly higher mean age, a higher rate of previous use of beta-lactam/beta-lactamase inhibitors or penicillins, a higher rate of urinary catheterization, and a longer length of hospital stay compared to CRE-infected patients.
 |
Table 1 Demographic and Clinical Characteristics of All Study Patients in Cohort I (N = 353), and Compared Between CRE-Colonized Patients (N = 225) and CRE-Infected Patients (N = 128) |
The types of CRE isolates in clinical specimens and stool or rectal swab samples from 353 study patients at enrollment in cohort I are shown in Table 2. Among the clinical specimens found to be positive for CRE, K. pneumoniae was the most common (76.8%), followed by Enterobacter spp. (13.0%), E. coli (12.7%), and Citrobacter spp. (1.7%). CRE was detected in 69.7% of stool or rectal swab samples at study enrollment. K. pneumoniae was also the most common type of CRE in stool (65.7%), followed by E. coli (13.6%) and Enterobacter spp. (4.5%).
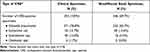 |
Table 2 Types of CRE Isolates in Clinical Specimens and Stool or Rectal Swab Samples of 353 Study Patients at Enrollment in Cohort I |
Among the CRE isolates with carbapenemase production, class B carbapenemases were detected in 68%, class A in 28.2%, and class D in 16.5%. Concomitant class A and class B carbapenemase producers were observed in 12.6%.
CRE-Colonized Patients
The characteristics and natural history of 225 CRE-colonized patients are summarized in Table 3. Urine was the most common site of CRE colonization (60.9%), followed by sputum (42.2%), body fluid (9.3%), and tissue (1.3%). CRE was detected in 67.6% of stool samples collected from all study patients at enrollment. Among the 225 CRE-colonized patients, 46 (20.4%) developed subsequent CRE infections. Of those, 43 patients had carbapenem-resistant K. pneumoniae infection, and 3 patients had carbapenem-resistant E. coli infection. Hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP) were common sites of subsequent CRE infection in patients with CRE colonization. The interval between the first detection of CRE colonization and subsequent CRE infection ranged from 2 to 71 days (median: 14 days). Among the 179 CRE-colonized patients who did not develop CRE infection, 115 patients (64.2%) had concomitant CRE colonization in stool. Absence of CRE colonization before discharge was observed in 26.1% of 69 CRE-colonized patients who had ≥2 stool or rectal swab samples collected and had CRE in the initial stool or rectal swab sample. The median (range) duration from the first CRE detection to the absence of CRE in stool before discharge was 16.5 days (range: 6–78).
 |
Table 3 Characteristics and Natural History of 225 CRE-Colonized Patients |
Clinical characteristics compared between CRE-colonized patients who developed CRE infection and those who did not develop CRE infection are summarized in Table 4. The factors found to be significantly associated with the development of CRE infection in CRE-colonized patients were ICU admission, use of antibiotics during hospitalization (including fluoroquinolones and vancomycin), receiving renal replacement therapy, central-line insertion, mechanical ventilation, and CRE colonization in sputum, stool, or at multiple sites. However, use of cephalosporins during hospitalization was significantly more frequent among CRE-colonized patients without subsequent CRE infection.
 |
Table 4 Clinical Characteristics Compared Between CRE-Colonized Patients Who Developed CRE Infection (N = 46) and Those Who Did Not Develop CRE Infection (N = 179) |
CRE-Infected Patients
The characteristics and clinical course of 174 CRE-infected patients, which included 128 CRE-infected patients at enrollment and 46 patients with CRE infections that developed subsequent to CRE colonization, are summarized in Table 5. HAP/VAP was the most common site of CRE infection (34.5%), followed by urinary tract infection (29.3%), intra-abdominal infection (17.8%), primary bacteremia (7.5%), catheter-related blood stream infection (5.7%), and skin and soft tissue infection (5.2%). Concomitant CRE colonization in stool or rectal swab sample was found in 131 patients (75.3%). Combination of colistin and fosfomycin was the most commonly used antibiotic regimen (36.8%) for treatment of CRE infections, followed by colistin monotherapy (19.5%). The mortality rate among CRE-infected patients at the end of treatment was 21.8%. Microbiological assessment at the end of treatment was available in 141 patients, and microbiological response was observed in 48.9% of CRE-infected patients. Overall mortality among CRE-infected patients at discharge was 47.7%. The factors significantly associated with mortality among CRE-infected patients are shown in Table 6. The presence of CRE in stool samples at the time of enrollment and having hospital-acquired pneumonia/ventilator-associated pneumonia were found to be significantly associated with mortality, whereas patients with urinary tract infection were significantly more likely to be alive at discharge. The mortality of patients who received monotherapy was not significantly different from the mortality of those who received combination therapy. Among the 131 CRE-infected patients who had CRE colonization in their stool, there were 83 patients who had ≥2 stool or rectal swab samples collected and had CRE in the initial stool or rectal swab sample. An evaluation of CRE status at discharge of these 83 patients revealed no CRE in the stool of 15 patients (18.1%) before discharge, whereas 68 patients (81.9%) had persistent CRE colonization in their stools before discharge. The median (range) duration from the first CRE detection in stool to the absence of CRE in stool before discharge was 24 days (range: 4–98).
 |
Table 5 Characteristics of and Clinical Course in 174 CRE-Infected Patients |
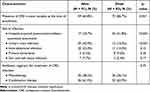 |
Table 6 The Number and Percentage of Patients Having Risk Factors Significantly Associated with Mortality Compared Between Those Who Lived and Those Who Died Among 174 CRE-Infected Patients |
Duration of CRE Fecal Carriage After Discharge
Among the 42 patients in cohort I who had CRE colonization in their stool before discharge and who sent follow-up stool samples to the research team, no CRE was isolated from 23 patients (54.8%) during follow-up. The percentage of these patients who had negative CRE in their stool samples was 33.3% and 50.0% within 6 months and 1 year, respectively. The duration from the first CRE detection in stool during hospitalization to the absence of CRE in stool after discharge from the hospital in these 19 patients ranged from 37 to 486 days (median: 119 days). Among the 19 patients (45.2%) who had persistent CRE colonization in their stool from the first detection of CRE in stool to the last follow-up stool culture, CRE was still recovered from stool up to 1 year of follow-up in 2 patients (10.5%), and the longest duration of CRE colonization in stool was up to 512 days of follow-up stool culture.
Among the 93 patients in cohort II who had CRE in their clinical specimens during their hospitalization, 47.3% and 91.4% of them had absence of CRE in their stool at 1 year and 2 years after first detection of CRE in clinical specimens, respectively. CRE was still recovered from stool up to 1 year of follow-up in 5 patients (5.4%), and the longest duration of CRE colonization in stool was up to 515 days of follow-up stool culture.
Discussion
This study did not enroll all of the hospitalized patients with CRE isolated from their clinical specimens during the study period of cohort I because there were so many patients, and the study team had limited time and resources to enroll all of them. Therefore, we decided to enroll eligible patients only on certain days of the week during the study period. This method of study subject enrollment resulted in a variation in the duration of follow-up of enrolled subjects. However, we were concerned that the follow-up duration for many cohort I patients would not be long enough, so we enrolled cohort II patients who were adult subjects with CRE isolated from their clinical specimens during hospitalization, and they were discharged alive from Siriraj Hospital from 2015 to 2018. Cohort II was enrolled to compensate for the number of CRE-colonized patients who had longer duration of follow-up than CRE-colonized patients in cohort I.
The methods of CRE detection in stool or rectal swab samples collected from subjects during hospitalization (conventional culture and antibiotic susceptibility testing for detection of CRE) and after discharge from the hospital (chromogenic selective agar for detection of CRE) were different because chromogenic selective agar for detection of CRE was not available when this study began in 2018. Therefore, we continued to use conventional culture and antibiotic susceptibility testing for detection of CRE in stool or rectal swab samples collected from subjects during hospitalization even though chromogenic selective agar for detection of CRE was available in 2019; however, we used chromogenic selective agar for detection of CRE for stool samples collected from patients after they were discharged from hospital. The chromogenic selective agar technique for detection of CRE that was used in this study was reported to be very accurate for detection of CRE in rectal swab specimen with a limit of detection of CRE that ranged from 101 to 102 CFU/mL.13,14 Moreover, a validation of agreement between conventional culture and antibiotic susceptibility testing for detection of CRE and chromogenic selective agar for detection of CRE that was performed on 120 stool or rectal swab samples in our laboratory also confirmed chromogenic selective agar for detection of CRE to be simple, accurate, and fast (CRE-positive result within 24 hours).
The results of our study revealed that 63.7% of hospitalized patients with isolated CRE from their clinical samples were actually colonized, especially if CRE was isolated from urine samples, whereas only approximately 40% had CRE infection. Therefore, the responsible physician should assess if a patient with isolated CRE from clinical specimen really has CRE infection before prescribing antibiotic therapy for CRE infection. Most patients with CRE colonization or CRE infection in the present study had chronic comorbid diseases, received antibiotics, and underwent medical interventions - all of which were reported to be major drivers of CRE acquisition.15–17 Therefore, any avoidable drivers of CRE colonization or CRE infection, especially unnecessary use of broad-spectrum antibiotics and unnecessary medical interventions, should be avoided or withdrawn from the patient as soon as possible in order to prevent CRE colonization or CRE infection.
The present study found K. pneumoniae to be the most common species of CRE in patients with CRE colonization or CRE infection. The prevalence of carbapenem resistance in E. coli was much lower than in K. pneumoniae even though E. coli is the predominant Enterobacterales in the gastrointestinal tract of humans, and E. coli infection is more common than K. pneumoniae infection in both community- and hospital-acquired infections. Class B carbapenemases were the most common carbapenemases detected among CRE isolates in this study. This is similar to the findings of previous studies on the molecular characterization of CRE isolates in Thailand that reported class B carbapenemase (ie, metallo-beta-lactamases) production to be the predominant mechanism of carbapenem resistance in Enterobacterales.18,19
CRE colonized patients are at risk of developing CRE infection. In the present study, 20.4% of patients with CRE colonization developed CRE infection during hospitalization. Factors found to be associated with the development of CRE infection in CRE-colonized patients included ICU admission, use of antibiotics during hospitalization, receiving renal replacement therapy, insertion of a central line, mechanical ventilation, and CRE colonization in sputum, stool, or at multiple sites. Therefore, CRE-colonized patients with one or more of the aforementioned risk factors should be closely monitored for early diagnosis and appropriate treatment of CRE infection. Colistin is still the antibiotic of choice for therapy of CRE infections in the present study because it is active against 87% of CRE isolates, including metallo-beta-lactamase producing isolates. Other anti-CRE antibiotics with activity against metallo-beta-lactamase producing CRE, especially cefiderocol, are not available in Thailand. Clinical and microbiological outcomes of treatment in patients with CRE infection in this study were unfavorable with overall mortality at discharge of nearly 50%. Half of CRE-infected patients with concomitant CRE colonization had persistent CRE colonization at discharge from the hospital, and these patients might transmit CRE to other family members and to the environment in their community. Measures to prevent CRE colonization and CRE transmission are important, and they should be applied to all hospitalized patients and to all CRE-colonized patients after hospital discharge to prevent CRE infection and CRE transmission.
The gastrointestinal tract is usually the reservoir of CRE colonization in humans, and the duration of CRE colonization in stool has been used to determine the duration of CRE colonization in many studies.20–22 However, our study detected CRE in stool or rectal swab samples in approximately 70% of patients who had CRE recovered from clinical samples. It should be noted that CRE in stool or rectal swab samples was not detected in approximately 30% of patients who had CRE recovered from clinical samples. This finding may be due to any one of the following possible explanations: 1) a real absence of CRE in stool; 2) an absence of CRE because the patient received antibiotics with anti-CRE activity; 3) the presence of a very small amount of CRE in the stool; or, 4) an error in random sampling of stool samples for CRE detection. Therefore, the prevalence of CRE in stool or rectal swab samples found in this study should be considered a minimum rate.
We found rates of CRE negativity in the stools of patients with CRE colonization in the gastrointestinal tract of approximately 50% and 91% at one and two years, respectively. The duration of fecal carriage of CRE in patients in cohort I and cohort II varied widely from days to years, and we were unable to propose any valid and reliable cut-off time period by which CRE colonization in stool disappeared without laboratory test if CRE in stool was absent according to the results of this study. A previous systematic review and meta-analysis found a higher rate of CRE eradication (65.4%) at one year than that observed in the present study (50%).23 However, CRE fecal carriage follow-up data with duration longer than one year remain scarce.
Patients with or who have a history of CRE infection or CRE colonization require IPC measures, especially contact precautions, which consume a lot of resources at every visit or hospitalization. Since chromogenic selective agar for detection of CRE in stool or rectal swab sample is very simple, accurate, inexpensive, and the results are quickly available, periodic testing of stool samples for CRE in these patients should be performed. This will benefit healthcare providers by reducing the burdens associated with managing patients with currently unknown CRE status, and it will benefit the patient by lessening the burdens associated with the stigma of having or being suspected of potentially having CRE colonization or infection. IPC measures were discontinued in many patients in this study after CRE was not found in their stool samples by using chromogenic selective agar for detection of CRE. Therefore, our center has decided to implement a policy to surveil the presence of CRE in stool samples sent from the homes of patients with a history of CRE colonization or CRE infection every several months to determine if CRE in stool sample is absent so that IPC measures can be discontinued in these patients. Moreover, CRE screening may be applied to all patients who will be hospitalized at Siriraj Hospital in the near future after the facility for CRE screening and the space for patients to wait for their screening results prior to hospitalization are available. However, our study found that the vast majority of patients had no CRE colonization in their stool after 2 years. Therefore, the 2-year time point might be an appropriate time to discontinue IPC measures at healthcare facilities with limited resources to perform CRE detection in stool samples.
It should be noted that CRE colonization in the stool of some patients could develop after being found to be absent in stool samples several times over a long period of follow-up, and this could be due to new acquisition of CRE after exposure to the aforementioned drivers of CRE colonization. Several studies have reported predictors of prolonged CRE carriage to be exposure to antibiotics, presence of an invasive device, higher Charlson comorbidity scores, number of hospital admissions, and transfer from another hospital or long-term care facility.15,16,21 Therefore, CRE testing in stool samples may need to be repeated even in patients with negative fecal carriage of CRE if they had exposure to one or more of the aforementioned drivers for developing CRE colonization.
Strengths and Limitations
The main strength of this study is that the data of patients with CRE isolated from their clinical specimens in cohort I were collected from patients during hospitalization to after discharge from the hospital, and there was a long duration of follow-up stool cultures to evaluate for CRE.
Our study also has some mentionable limitations. First, as mentioned earlier, this study did not enroll all hospitalized patients with CRE isolated from their clinical specimens during the study period of cohort I. Second, the prevalence of CRE colonization in stool observed in this study should be considered the minimum rate because there might be some patients with false-negative results for CRE from stool culture while receiving antibiotics with anti-CRE activity, or due to having a very small amount of CRE in stool, or due to an error in random sampling of stool samples for CRE culture. Third, the duration of CRE colonization in patient stool after discharge from the hospital might be overestimated because a stool sample was collected every week during hospitalization, but only every few months after discharge from hospital. Therefore, the disappearance of CRE from post-hospital discharge stool could have occurred at any time between the most recent stool sampling and the most recent previous stool sampling. Therefore, the duration of CRE colonization in stool observed in this study should be considered the maximum duration. Lastly, the duration of CRE fecal carriage after discharge was evaluated only in patients who were willing to send a stool sample from home to our research team. Therefore, the characteristics of the patients who sent stool samples from home might be different from those who did not send a stool sample from home after discharge. These differences could influence a selection bias relative to the duration of CRE fecal carriage.
Conclusion
CRE isolated from clinical specimens from hospitalized patients are more likely to cause colonization than infection. Patients with CRE colonization are at risk for subsequent CRE infection with high mortality. Stool culture for CRE is needed to verify if contact precautions can be discontinued because the duration of CRE colonization in stool varied from days to years.
Acknowledgments
The authors gratefully acknowledge the personnel of the microbiology laboratory of the Division of Infectious Diseases and Tropical Medicine, Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University for performing the laboratory testing for CRE in stool or rectal swab samples. We would also like to thank Ms. Pornsiri Chinswangwatana and Ms. Ananya Srisomnuek for study coordination, and Ms. Khemajira Karaketklang of the Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University for her assistance with statistical analysis.
Funding
This study was funded by grants from the Thailand Center of Excellence for Life Sciences (TCELS), the National Research Council of Thailand (NRCT) and the Faculty of Medicine Siriraj Hospital, Mahidol University.
Disclosure
All authors declare no conflicts of interest in this work and no personal or professional conflicts of interest relating to any aspect of this study.
References
1. Gupta N, Limbago BM, Patel JB, Kallen AJ. Carbapenem-resistant Enterobacteriaceae: epidemiology and prevention. Clin Infect Dis. 2011;53(1):60–67. doi:10.1093/cid/cir202
2. Cantón R, Akóva M, Carmeli Y, et al. Rapid evolution and spread of carbapenemases among Enterobacteriaceae in Europe. Clin Microbiol Infect. 2012;18(5):413–431. doi:10.1111/j.1469-0691.2012.03821.x
3. National Antimicrobial Resistance Surveillance Center, Thailand (NARST). [Antibiogram]; 2020. Available from: http://narst.dmsc.moph.go.th/. Thai.
4. Papadimitriou-Olivgeris M, Marangos M, Fligou F, et al. Risk factors for KPC-producing Klebsiella pneumoniae enteric colonization upon ICU admission. J Antimicrob Chemother. 2012;67(12):2976–2981. doi:10.1093/jac/dks316
5. Prabaker K, Lin MY, McNally M, et al. Transfer from high-acuity long-term care facilities is associated with carriage of Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae: a multihospital study. Infect Control Hosp Epidemiol. 2012;33(12):1193–1199. doi:10.1086/668435
6. Soontaros S, Leelakanok N. Association between carbapenem-resistant Enterobacteriaceae and death: a systematic review and meta-analysis. Am J Infect Control. 2019;47(10):1200–1212. doi:10.1016/j.ajic.2019.03.020
7. Gottesman T, Agmon O, Shwartz O, Dan M. Household transmission of carbapenemase-producing Klebsiella pneumoniae. Emerg Infect Dis. 2008;14(5):859–860. doi:10.3201/eid1405.071340
8. World Health Organization. Guidelines for the prevention and control of carbapenem-resistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in health care facilities. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO.
9. CLSI. Performance Standards for Antimicrobial Susceptibility Testing.
10. Birgy A, Bidet P, Genel N, et al. Phenotypic screening of carbapenemases and associated β-lactamases in carbapenem-resistant Enterobacteriaceae. J Clin Microbiol. 2012;50(4):1295–1302. doi:10.1128/JCM.06131-11
11. Tsakris A, Kristo I, Poulou A, et al. Evaluation of boronic acid disk tests for differentiating KPC-possessing Klebsiella pneumoniae isolates in the clinical laboratory. J Clin Microbiol. 2009;47(2):362–367. doi:10.1128/JCM.01922-08
12. Franklin C, Liolios L, Peleg AY. Phenotypic detection of carbapenem-susceptible metallo-beta-lactamase-producing gram-negative bacilli in the clinical laboratory. J Clin Microbiol. 2006;44(9):3139–3144. doi:10.1128/JCM.00879-06
13. García-Fernández S, Hernández-García M, Valverde A, Ruiz-Garbajosa P, Morosini MI, Cantón R. CHROMagar mSuperCARBA performance in carbapenem-resistant Enterobacteriaceae isolates characterized at molecular level and routine surveillance rectal swab specimens. Diagn Microbiol Infect Dis. 2017;87(3):207–209. doi:10.1016/j.diagmicrobio.2016.11.014
14. Soria Segarra C, Larrea Vera G, Berrezueta Jara M, et al. Utility of CHROMagar mSuperCARBA for surveillance cultures of carbapenemase-producing Enterobacteriaceae. New Microbes New Infect. 2018;26:42–48. doi:10.1016/j.nmni.2018.08.005
15. Okamoto K, Lin MY, Haverkate M, et al. Modifiable risk factors for the spread of Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae among long-term acute-care hospital patients. Infect Control Hosp Epidemiol. 2017;38(6):670–677. doi:10.1017/ice.2017.62
16. Salomão MC, Freire MP, Boszczowski I, Raymundo SF, Guedes AR, Levin AS. Increased risk for carbapenem-resistant Enterobacteriaceae colonization in intensive care units after hospitalization in emergency department. Emerg Infect Dis. 2020;26(6):1156–1163. doi:10.3201/eid2606.190965
17. Salomão MC, Guimarães T, Duailibi DF, et al. Carbapenem-resistant Enterobacteriaceae in patients admitted to the emergency department: prevalence, risk factors, and acquisition rate. J Hosp Infect. 2017;97(3):241–246. doi:10.1016/j.jhin.2017.08.012
18. Yungyuen T, Chatsuwan T, Plongla R, et al. Nationwide surveillance and molecular characterization of critically drug-resistant gram-negative bacteria: results of the Research University Network Thailand Study. Antimicrob Agents Chemother. 2021;65(9):e0067521. doi:10.1128/AAC.00675-21
19. Laolerd W, Akeda Y, Preeyanon L, Ratthawongjirakul P, Santanirand P. Carbapenemase-producing carbapenem-resistant Enterobacteriaceae from Bangkok, Thailand, and their detection by the carba NP and modified carbapenem inactivation method tests. Microb Drug Resist. 2018;24(7):1006–1011. doi:10.1089/mdr.2018.0080
20. Feldman N, Adler A, Molshatzki N, et al. Gastrointestinal colonization by KPC-producing Klebsiella pneumoniae following hospital discharge: duration of carriage and risk factors for persistent carriage. Clin Microbiol Infect. 2013;19(4):E190–6. doi:10.1111/1469-0691.12099
21. Zimmerman FS, Assous MV, Bdolah-Abram T, Lachish T, Yinnon AM, Wiener-Well Y. Duration of carriage of carbapenem-resistant Enterobacteriaceae following hospital discharge. Am J Infect Control. 2013;41(3):190–194. doi:10.1016/j.ajic.2012.09.020
22. Cheng VC, Chan JF, Wong SC, et al. Proactive infection control measures to prevent nosocomial transmission of carbapenem-resistant Enterobacteriaceae in a non-endemic area. Chin Med J. 2013;126(23):4504–4509.
23. Bar-Yoseph H, Hussein K, Braun E, Paul M. Natural history and decolonization strategies for ESBL/carbapenem-resistant Enterobacteriaceae carriage: systematic review and meta-analysis. J Antimicrob Chemother. 2016;71(10):2729–2739. doi:10.1093/jac/dkw221
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
