Back to Journals » International Journal of General Medicine » Volume 15
Epidemiology and Risk Factors of Convulsive Status Epilepticus Patients Admitted in the Emergency Department of Tertiary Hospital in Mogadishu, Somalia
Authors Sheikh Hassan M , Sidow NO , Ali Adam B , GÖKGÜL A, Hassan Ahmed F, Ali IH
Received 24 September 2022
Accepted for publication 9 December 2022
Published 14 December 2022 Volume 2022:15 Pages 8567—8575
DOI https://doi.org/10.2147/IJGM.S391090
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Scott Fraser
Mohamed Sheikh Hassan,1 Nor Osman Sidow,1 Bakar Ali Adam,1 Alper GÖKGÜL,1 Fardowsa Hassan Ahmed,2 Ibrahim Hussein Ali3
1Department of Neurology, Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somalia; 2Department of Pediatrics, Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somalia; 3Department of Emergency Medicine, Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somalia
Correspondence: Mohamed Sheikh Hassan, Email [email protected]
Introduction: Status epilepticus (SE) is one of the most common neurologic emergencies and is associated with significant morbidity and mortality. The underlying cause of SE varies between patients with epilepsy and those presenting without. The aim of this study was to evaluate the epidemiology, risk factors and outcomes of patients presenting with convulsive SE in the emergency department (ED) of a tertiary hospital in Mogadishu.
Methods: This was a cross-sectional study conducted between July 2021 and June 2022. The study included both patients with epilepsy and those without epilepsy presenting to the ED with SE. Risk factors and underlying etiologies were evaluated in the patients in both the pediatric group (0– 18 years) and adult group (18 years and above). Clinical history, neurologic examinations, neuroimaging, electroencephalography findings, and laboratory investigations were all evaluated.
Results: The mean age for pediatric patients was 6 (SD± 4.7), while the mean age for adult patients was 38 (SD± 10.4). About 33 (36%) of the subjects had previous history of epilepsy, while 59 (64%) presented to the ED with their first seizure. About 80 (87%) had generalized seizure while 12 (13%) had focal seizure. Poor antiepileptic compliance was the most common risk factor for SE 20 (21.7%), followed by CNS infections 14 (15%), and prolonged febrile seizures 7 (7.6%). Poor antiepileptic drug compliance, cerebrovascular disorders, electrolyte imbalance, metabolic conditions, and drug abuse were the most common underlying etiologies of SE in patients older than 18 years. Prolonged febrile seizure, meningitis, encephalitis, systemic infections, and structural brain abnormalities were the most common underlying etiologies of SE in patients younger than 18 years.
Conclusion: CNS infections, CVDs, metabolic disturbances, electrolyte imbalances, and systemic infections are major etiological risk factors of SE in patients without prior history of epilepsy. Medication adherence was the major etiological risk factor for SE identified in patients with epilepsy.
Keywords: status epilepticus, emergency room, risk factors
Introduction
Status epilepticus (SE) is defined as a seizure with 5 minutes or more of continuous clinical and/or electrographic seizure activity or recurrent seizure activity in which the patient does not regain consciousness in between. Previously, status epilepticus was defined as continuous seizure activity for duration of 30 minutes or a series of seizures in which the patient’s consciousness is not regained in between seizures.1,2 SE is a neurological emergency and life-threatening condition that needs immediate intervention and particular attention to prevent permanent cerebral damage.3
Status epilepticus is a life-threatening condition and is associated with significant rates of mortality and morbidity if not urgently managed. To prevent this catastrophe, rapid initiation of IV antiepileptic treatment is required to control such a fatal condition and ensure the survival of the patients.4,17 Adults with status epilepticus have a mortality rate of 15% to 20%, whereas children have a rate of 3% to 15%. Hyperthermia, pulmonary edema, cardiac arrhythmias, and cardiovascular collapse are all hallmarks of acute complications. Epilepsy (20% to 40%), encephalopathy (6% to 15%), and localized neurologic impairments are some of the long-term consequences (9 to 11%).5,6
The American Epilepsy Society Guidelines for the Evaluation and Management of Status Epilepticus from 2016 and the Neurocritical Care Guidelines from 2012 both describe status epilepticus (SE) as a seizure that lasts longer than 5 minutes. The guidelines additionally define refractory status epilepticus (RSE) as a seizure that persists despite treatment with an appropriate doses of a benzodiazepine (4-mg intravenous (IV) injection of lorazepam) plus the appropriate dose of one antiepileptic medication.25,26
The etiology of SE differs widely from patient groups. Underlying causes vary according to age and the epileptic history of patients. In people known to be epileptic, poor compliance and drug withdrawal are the commonest causes of SE. In contrast, patients with no epileptic history, metabolic causes, electrolyte imbalance, cerebrovascular disorders, head traumas, central nervous system (CNS) infections, cardiac arrests, and drug intoxications are the most common causes.7,8
Status epilepticus is a common neurologic emergency we frequently see in the emergency department of our hospital. There are different etiologies for SE seen in the evaluation of these patients. One major risk factor for SE in these patients, especially in adults, is lack of compliance with antiepileptic medications. Since there was no previous study evaluating the epidemiological profile and risk factors of SE in the country, we aimed to assess the epidemiology and risk factors of convulsive SE among patients admitted to the emergency department of our hospital; we also assessed the outcomes (intrahospital mortality) of these patients so that patients who are at risk can be diagnosed and treated early in the course of the disease to reduce mortality.
Methods and Materials
This was a cross-sectional study conducted at Mogadishu Somali Turkish Training and Research Hospital between July 2021 and June 2022. All patients who presented to the emergency department with convulsive status epilepticus who were eligible to the inclusion criteria were evaluated. The participants of the study were both patients with a history of epilepsy and those without epilepsy, of all ages, presenting to the ER with status epilepticus. Patients with psychogenic non-epileptic seizures and patients with epileptic seizures but did not the the definition of SE were excluded from the study. Risk factors and underlying risk factors were evaluated in the patients. Clinical history, neurologic examinations, cerebral imaging, electroencephalographic findings and laboratory investigations (including complete blood count, full biochemistry profile) were all assessed by a team of neurologists, pediatricians and emergency physicians. The data related to seizure onset, nature, and length was collected by a team of neurologists and emergency physicians at the emergency visit and following hospital admission. The neurological examinations were made by neurologists both at the emergency visit and after the patient’s recovery from the seizure (this was made to clearly define that the neurological deficit was not due to the seizure itself). The EEG recordings were made within the first 20 hours of patients’ admission to the emergency room and were interpreted by consultant neurologists at our hospital.
The data were collected by 4 researchers, and other researchers reviewed the appropriateness of all patients included and excluded. The patients’ medical records were partially obtained from the hospital database (FONET system), while some other data were given by the patients/relatives. The collected data included patients’ demographics (age, gender), laboratory tests (albumin, sodium, potassium, calcium, magnesium, glucose, aspartate aminotransferase, alanine aminotransferase), past medical history (ischemic stroke, hemorrhagic stroke, previous history of epilepsy, diabetes mellitus, coronary artery disease, traumatic brain injury), seizure classification (generalized convulsive, and focal motor). Patients’ brain imaging (CT/MRI) and EEG were performed within 20 hours of admission. Since we could not measure antiepileptic drug levels, interruption or discontinuation of anticonvulsive medication as a trigger of SE was considered as a poor/lack of compliance of AEDs. All patients had neuroimaging studies (CT/MRI) and EEG recordings. The neuroimaging was assessed by neurologists and radiologists in the hospital, and based on the analysis; it was classified into normal and abnormal imaging findings. The EEG recordings were interpreted by consultant neurologists and classified into normal, generalized epileptic discharges, focal epileptic discharges, focal slowing, and generalized slowing patterns. The outcome (mortality) of patients was assessed in both pediatric and adult patients, and comparisons were made in both groups to identify if there was a statistically significant difference in mortality rates.
Case Definition
SE was defined as a seizure with 5 minutes or more of continuous seizure activity or recurrent seizure activity without recovery between seizures. We enrolled all patients who met the definition of status epilepticus regardless of age, seizure type, or epileptic history. Furthermore, 10 patients were excluded from the study due to psychogenic non-epileptic seizures (PNES).
Statistical Analysis
Continuous variables are represented by means and standard deviations; frequencies and percentages were used to illustrate categorical variables. Pearson’s chi-square test was used to determine the etiological and risk factors distribution by age group of the patients. P < 0.05 was considered statistically significant. SPSS software version 26 was used to conduct the statistical analysis.
Ethical Approval and Consideration
This study was performed in line with the principles of the Declaration of Helsinki. The study was reviewed and accepted by the ethics committee of Mogadishu Somali Turkish Training and Research Hospital (Ethics Protocol No: MSTH/7418). All patients and caregivers were informed of the purpose of this study. Written informed consent was obtained from the adult patients who were able to give consent for the study. For children and adult patients (who are unable to give consent for their medical condition), the consent was obtained from their relatives or caregivers. We declare that we have followed the protocols of our work center. Patients’ data confidentiality was respected.
Results
Of the 92 patients included in this study, 52 were adults and the other 40 were less than 18 years old. The mean age for pediatric patients was 6 (SD±4.7), while the mean age for adult patients was 38 (SD±10.4). 50 (54.3%) of patients were male, while 42 (45.7%) were female. Comorbidity was present in 38 (41%) of the subjects. 33 (36%) of the subjects had a previous history of epilepsy, while 59 (64%) presented to the emergency room with status epilepticus for the first time in their lives. Of those with epilepsy history, 11 (33%) had 1–5 years of epilepsy history, 10 (30%) had epilepsy between 5–10 years, 8 (24%) had epilepsy between 10–15 years, 3 (9%) had epilepsy between 15–20 years, while 1 (3%) had epilepsy for more than 20 years. In terms of seizure type, 80 (87%) had generalized seizures, while 12 (13%) had focal seizures. Generalized seizures were slightly higher in male patients and those above 18 years of age (see Table 1). Thirty-two (32.6%) of the patients had a family history of epilepsy.
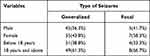 |
Table 1 Seizure Type by Gender and Age of Patients |
Following a neurologic examination, 28 (30%) of the patients had neurologic deficits, whereas 64 (70%) had a normal neurologic examination. 23 (25%) had abnormal brain imaging, while 69 (75%) had normal brain imaging. Abnormal imaging findings were more common in adult patients than in pediatric patients. This was statistically significant (P = 0.028). The most common EEG abnormality seen in 34 patients (37%), was generalized epileptic discharges; 19 patients (20.7%) had focal epileptic discharges, and 31 patients (33.7%) had normal EEG findings (Figure 1 shows the EEG findings of patients). Patients with a past history of epilepsy were more likely to have EEG pathologic findings compared to those with no past history of epilepsy. This was statistically significant (P=0.001). Regarding antiepileptic medication history, 31 (33.7%) of the patients were on antiepileptic medications. Of these, 9 (29%) were on monotherapy, while 22 (71%) were on polytherapy.
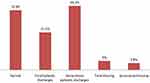 |
Figure 1 Shows EEG findings of patients. |
Regarding the underlying causes of the status epilepticus of the subjects, 20 (20.7%) were due to poor AED compliance, 8 (8.7%) were due to systemic infection, 7 (7.6%) were due to prolonged febrile seizures, 7 (7.6%) were due to electrolyte imbalance (Table 2 lists the different etiologies of status epilepticus among the patients). Among the 92 patients admitted, 18 (19.6%) died during hospitalization, while 74 (80.4%) were discharged from the hospital following successful management. 3% of the subjects became refractory status epileptics. Mortality was somewhat higher in adult patients with abnormal neuroimaging findings compared pediatric patients. This was not statistically significant (P= 0.602).
 |
Table 2 Underlying Causes of Status Epilepticus Among Patients |
The study showed variation in the etiology of status epilepticus among different age groups. Poor antiepileptic drug compliance, cerebrovascular disorders, electrolyte imbalance, metabolic conditions, and drug abuse were the most common underlying etiologies of status epilepticus in patients older than 18 years. Prolonged febrile seizures, meningitis, encephalitis, systemic infection, and structural brain abnormalities were the most common underlying etiologies of status epilepticus in patients younger than 18 years (see Table 3). In this study, there was statistical significance between the type of seizure and the outcome of the patients. Patients with generalized status epilepticus died at a higher rate than those with focal status epilepticus (P = 0.016).
 |
Table 3 Distribution of Etiologies of SE Among Different Age Groups |
Discussion
Status epilepticus (SE) is defined as a seizure that lasts longer than 5 minutes, or having more than 1 seizure within a 5-minute period, without returning to a normal level of consciousness between episodes.1 Status epilepticus is one of the most common neurologic emergencies seen in the ER. It can have life-threatening complications and long-term consequences if it lasts longer than 30 minutes.9 We included 92 patients (52 adult and 40 pediatric patients) who presented with status epilepticus to the emergency department of our hospital. Etiological factors such as poor AED compliance, structural CNS insult, electrolyte imbalance, metabolic disturbances, prolonged febrile seizures, central nervous system infections, neoplastic lesions, hydrocephalus, head trauma, and other factors that are associated with SE among patients were all evaluated. The scope of etiological factors in the development of SE varies according to demographic history and clinical history.
Risk factors for first time SE include head trauma, fever, stroke, alcohol use, metabolic abnormalities, anoxia/hypoxia, tumors, and drug overdose. Poor compliance of AEDs and low epileptic drug levels are the major risk factors for SE in patients with known epilepsy history.10,11,18 In this study, 64% of the patients presented to the emergency room with status epilepticus for the first time in their lives, indicating a high potential for underlying secondary causes. Risk factors for status epilepticus were different among patients with epilepsy and those presenting with status epilepticus for the first time, as well as between different age groups of patients. In our study, poor AED compliance, cerebrovascular disorders, electrolyte imbalance, metabolic conditions, and drug abuse were the most common underlying etiologies of status epilepticus in patients older than 18 years. The most common underlying etiologies of status epilepticus in patients under the age of 18 were febrile seizures, meningitis, encephalitis, systemic infection, and structural brain abnormalities.
Status epilepticus is associated with a high rate of mortality. It affects about 50/100,000 people each year and recurs in more than 13% of cases. The strongest single risk factor for generalized convulsive status epilepticus is a history of epilepsy.19 Mortality rates are 15% to 20% in adults12 and 3% to 15% in children.14 In our study, 18 (19.6%) of 92 patients admitted died during hospitalization, while 74 (80.4%) were discharged from the hospital following successful management. 3% of the subjects became refractory status epileptics. Mortality was higher in adult patients with abnormal neuroimaging findings compared pediatric patients. This was not statistically significant (P= 0.602). The mortality of our patients was related to SE and their underlying etiologies.
Acute complications resulting from hyperthermia, pulmonary edema, cardiac arrhythmias, and cardiovascular collapse are the responsible causes of death in status epilepticus patients.10 In pediatric patients, SE has been associated with CNS damage, fever, poisoning, systemic infection, low anticonvulsant levels, anatomical brain abnormalities, electrolyte imbalances, and inborn metabolic errors in children.13,14 In our study, prolonged febrile seizures, meningitis, encephalitis, systemic infection, structural brain abnormalities, and poor antiepileptic compliance were the most common underlying etiologies of status epilepticus in pediatric patients. As per a study by Coeytaux et al, cerebrovascular accidents were the most frequent risk factors in non-epileptic patients (30%). Antiepileptic drug noncompliance was the most common risk factor in epileptic patients (18.9%).15 In this study, cerebrovascular disorders accounted for 8% of the underlying etiologies in non-epileptic patients. CVD was more common in adult patients than in the pediatric group.
As Maldonado et al revealed in their study, 56.1% of the patients had abruptly interrupted or discontinued their antiepileptic medication, which was the underlying cause of their status epilepticus.16 According to a Colombian study,20 noncompliance with medication is the leading cause of SE. Non-compliance is common in Somalia, although it has not been studied. There was no single previous study evaluating antiepileptic drug compliance. In this study, the most common risk factor identified in patients with epilepsy was non- or poor compliance with AEDs (21%). Among the 33% of epileptic patients in this study, 60% of these epileptic patients came with status epilepticus to the ER due to medication noncompliance. Moreover, poor AED compliance was more common in adult patients compared to children. Poor compliance with antiepileptic medications is significantly higher in Sub-Saharan African countries, with 67% in Nigeria, 54% in Kenya, and 37% in Ethiopia, and economic factors were the primary determinants of poor compliance.21–23 The main causes of treatment failure and emergency department visits among epileptic patients are poor adherence to antiepileptic medications. Repeated seizures lead to a low quality of life, diminished productivity, and a social and economic problem associated with seizures.24
In developing countries, central nervous system infections are one of the major causes of SE in patients presenting with first-time seizures in the ER (contributing to 15% of the cases).25 Among CNS infections, encephalitis, meningitis, and brain abscess were observed in the study. Systemic infections were also responsible for almost 10% of cases of SE (including those with a history of epilepsy and those without). Therefore, in patients presenting with first-time seizures, infectious causes should be given great consideration in the differential diagnosis by performing extensive laboratory investigations and cranial imaging and CSF analysis in certain circumstances.
According to research by Chin et al, 17% of the total included SE cases were caused either by metabolic disorders or electrolyte disturbances.6 In our study, metabolic and electrolyte imbalances were also common etiologies of SE (15%). Among the recorded etiologies are hypoglycemia, hyperglycemia, uremic encephalopathy, hyponatremia, and hypocalcemia. The differential diagnosis of patients with first-time SE should be broad and metabolic and electrolyte imbalances should be evaluated as possible etiologies for the status epilepticus.
Study Limitations
The main limitation faced during this study was the lack of sufficient previous information related to status epilepticus in its various forms in our country, as well as the associated risk factors (because there was not a single study related to status epilepticus conducted in the country before, thus this becomes the first of its kind). Another limitation was the lack of measurement of the serum levels of medications used for epileptic control because either the test could not be performed (lack of availability of the test) or patients did not usually have money to pay for such measurements. Cross-sectional study is not the best research design to measure risk factors related to a specific outcome, but it gives an overview of risk factors related to a particular outcome at a specific point of time. To reduce the possible confounding factors, we used a strict systematic approach for data collection and a consistent definition for our cases. This minimized the level of data bias and misclassification that could be present in our investigation. At this point, we think it provides useful insight into risk factors for status epilepticus in both pediatric and adult patients. We recommend further prospectively designed multicenter studies be conducted in the country.
Conclusion
This study is the first of its kind to be conducted in Somalia to determine the etiological and risk factors of status epilepticus. The findings of the study will be useful for clinicians in the management of status epilepticus. To fully understand the risk factors related to SE, further research is needed to be conducted in Mogadishu and other cities in the country.
Abbreviations
ER, Emergency Room; CVD, Cerebrovascular disorders; AED, Antiepileptic drugs; CNS, Central Nervous System; SE, Status Epilepticus.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. The study was reviewed and accepted by the ethics committee of Mogadishu Somali Turkish Training and Research Hospital (Ethics Protocol No: MSTH/7418).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Horváth L, Fekete I, Molnár M, Válóczy R, Márton S, Fekete K. The outcome of status epilepticus and long-term follow-up. Front Neurol. 2019;10:427. doi:10.3389/fneur.2019.00427
2. Berg AT, Berkovic SF, Brodie MJ, et al. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE commission on classification and terminology, 2005–2009.
3. Trinka E, Cock H, Hesdorffer D, et al. A definition and classification of status epilepticus–report of the ILAE task force on classification of status epilepticus. Epilepsia. 2015;56(10):1515–1523. doi:10.1111/epi.13121
4. Fountain NB. Status epilepticus: risk factors and complications. Epilepsia. 2000;41(s2):S23–S30. doi:10.1111/j.1528-1157.2000.tb01521.x
5. Chen JW, Wasterlain CG. Status epilepticus: pathophysiology and management in adults. Lancet Neurol. 2006;5(3):246–256. doi:10.1016/S1474-4422(06)70374-X
6. Chin RF, Neville BG, Scott RC. A systematic review of the epidemiology of status epilepticus. Eur J Neurol. 2004;11(12):800–810. doi:10.1111/j.1468-1331.2004.00943.x
7. Sutter R, Kaplan PW, Rüegg S. Outcome predictors for status epilepticus—what really counts. Nat Rev Neurol. 2013;9(9):525–534. doi:10.1038/nrneurol.2013.154
8. Ghali AA, Ahmed I, Fadel WA, Hassan GN. First attack of status epilepticus in adults: etiology and risk factors. Med J Cairo Univ. 2019;87(June):1357–1361. doi:10.21608/mjcu.2019.53426
9. Hassan MS, Sidow NO, GÖKGÜL A, et al. Epidemiology and clinical profile of neurologic patients evaluated in the emergency department of teaching hospital in Mogadishu, Somalia, cross-sectional study.
10. Brophy GM, Bell R, Claassen J, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3–23.
11. Lowenstein DH. Status epilepticus: an overview of the clinical problem. Epilepsia. 1999;40(Suppl 1):S3–S8. doi:10.1111/j.1528-1157.1999.tb00872.x
12. Aminoff MJ, Simon RP. Status epilepticus: causes, clinical features and consequences in 98 patients. Am J Med. 1980;69(5):657–666. doi:10.1016/0002-9343(80)90415-5
13. Riviello JJ, Ashwal S, Hirtz D, et al. Practice parameter: diagnostic assessment of the child with status epilepticus (an evidence-based review): report of the quality standards subcommittee of the American academy of neurology and the practice committee of the child neurology society. Neurology. 2006;67(9):1542–1550. doi:10.1212/01.wnl.0000243197.05519.3d
14. Alyoubi RA, Aljaafari DT, Basheikh MA, et al. The etiology and risk factors of convulsive status epilepticus in pediatric patients of tertiary center in Saudi Arabia. Neurosci J. 2021;26(1):26–30. doi:10.17712/nsj.2021.1.20200116
15. Coeytaux A, Jallon P, Galobardes B, Morabia A. Incidence of status epilepticus in French-speaking Switzerland:(EPISTAR). Neurology. 2000;55(5):693–697. doi:10.1212/WNL.55.5.693
16. Maldonado A, Ramos W, Pérez J, Huamán LA, Gutiérrez EL. Convulsive status epilepticus: clinico-epidemiologic characteristics and risk factors in Peru. Neurología. 2010;25(8):478–484. doi:10.1016/j.nrl.2010.07.010
17. Walker MC. Pathophysiology of status epilepticus. Neurosci Lett. 2018;667:84–91. doi:10.1016/j.neulet.2016.12.044
18. Power KN, Gramstad A, Gilhus NE, Engelsen BA. Prognostic factors of status epilepticus in adults. Epileptic Disord. 2016;18(3):297–304. doi:10.1684/epd.2016.0855
19. Claassen J, Lokin JK, Fitzsimmons BF, Mendelsohn FA, Mayer SA. Predictors of functional disability and mortality after status epilepticus. Neurology. 2002;58(1):139–142. doi:10.1212/WNL.58.1.139
20. Sánchez S, Rincon F. Status epilepticus: epidemiology and public health needs. J Clin Med. 2016;5(8):71. doi:10.3390/jcm5080071
21. Johnbull OS, Farounbi B, Adeleye AO, Ogunrin O, Uche AP. Evaluation of factors influencing medication adherence in patients with epilepsy in rural communities of Kaduna State, Nigeria. Neurosci Med. 2011;2(4):299–305. doi:10.4236/nm.2011.24039
22. Mbuba CK, Ngugi AK, Fegan G, et al. Risk factors associated with the epilepsy treatment gap in Kilifi, Kenya: a cross-sectional study. Lancet Neurol. 2012;11(8):688–696. doi:10.1016/S1474-4422(12)70155-2
23. Getachew H, Dekema N, Awol S, Abdi A, Mohammed M. Medication adherence in epilepsy and potential risk factors associated with non adherence in tertiary care teaching hospital in southwest Ethiopia. Gaziantep Med J. 2014;20(1):59–65. doi:10.5455/GMJ-30-45904
24. Getnet A, Woldeyohannes SM, Bekana L, et al. Antiepileptic drug nonadherence and its predictors among people with epilepsy. Behav Neurol. 2016;2016:1–6. doi:10.1155/2016/3189108
25. Glauser T, Shinnar S, Gloss D, et al. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the guideline committee of the American epilepsy society. Epilepsy Curr. 2016;16(1):48–61. doi:10.5698/1535-7597-16.1.48
26. Brophy GM, Bell R, Claassen J, et al. Neurocritical care society status epilepticus guideline writing community. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3–23.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
