Back to Journals » Infection and Drug Resistance » Volume 15
Epidemiological and Clinical Characteristics of COVID-19 Patients in Northern Ethiopia: A Retrospective Cohort Study
Authors Temesgen Abebe H, Mitiku Ashebir M, Mohamedniguss Ebrahim M , Berhe Zelelow Y , Mulugeta Bezabih A, Redae Tefere G , Fseha Teklehaimanot B, Hintsa S, Leul Welderufael A
Received 30 December 2021
Accepted for publication 21 June 2022
Published 7 July 2022 Volume 2022:15 Pages 3579—3588
DOI https://doi.org/10.2147/IDR.S345936
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Haftom Temesgen Abebe,1,2 Mengistu Mitiku Ashebir,1 Mohamedawel Mohamedniguss Ebrahim,3 Yibrah Berhe Zelelow,3 Afework Mulugeta Bezabih,1 Getachew Redae Tefere,1 Berhane Fseha Teklehaimanot,4 Solomon Hintsa,5 Abadi Leul Welderufael3
1School of Public Health, College of Health Sciences, Mekelle University, Mekelle, Ethiopia; 2Laboratory Interdisciplinary Statistical Data Analysis, College of Health Sciences, Mekelle University, Mekelle, Ethiopia; 3School of Medicine, College of Health Sciences, Mekelle University, Mekelle, Ethiopia; 4Department of Public Health, College of Health Sciences, Adigrat University, Adigrat, Ethiopia; 5Department of Public Health, College of Health Sciences, Axum University, Axum, Ethiopia
Correspondence: Haftom Temesgen Abebe, School of Public Health, College of Health Sciences, Mekelle University, P.O.Box 1871, Mekelle, Ethiopia, Tel +251941982945, Email [email protected]
Purpose: COVID-19, caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), is an emerging global public health problem. The disease is believed to affect older people and is accompanied by clinical features such as fever, shortness of breath, and coughing. Currently, there is a lack of information regarding the characteristics of COVID-19 patients in Ethiopia. Thus, this paper aims to evaluate the epidemiological and clinical features of COVID-19 patients in Tigray, Northern Ethiopia.
Patients and Methods: A total of 6,637 symptomatic and asymptomatic COVID-19 patients collected from six isolation and treatment centers in Tigray between May 7 and October 28, 2020 were retrospectively analyzed. Chi-square test or Fisher’s exact test was used to compare the epidemiological and clinical characteristics of COVID-19 patients as appropriate. A p-value < 0.05 was considered statistically significant.
Results: The mean age of the patients was 31.3± 12.8. SARS-CoV-2 infects men more than women with a ratio of 1.85:1. About 16% of the patients were symptomatic, of which 13.3% (95% CI=11.3– 15.4%) were admitted to intensive care units and 6.1% (95% CI=4.5– 7.6%) were non-survivors. The mortality rate was increased up to 40.3% (95% CI=32.1– 48.4%) among patients with severe illness. A higher proportion of deaths were observed in men (73.2%) and 55.4% were in the age group of ≥ 50 years. About 4.3% (282 of 6,637) had one or more coexisting comorbidities; the most common being cardiovascular diseases (30.1%) and diabetes mellitus (23.8%). The comorbidity rate in the non-survivor group was significantly higher than in the survivor group (p-value < 0.001).
Conclusion: The proportion of symptomatic patients was low. Non-survival was linked with old age and the existence of comorbidities. The findings of this study can help in the design of appropriate management strategies for COVID-19 patients, such as giving due emphasis to COVID-19 patients who are old and with comorbidities.
Keywords: COVID-19, comorbidity, symptomatic, mortality rate
Introduction
COVID-19, a severe acute respiratory infection (SARI) that emerged in early December 2019 in Wuhan, China, has continued to be a global threat.1 It is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which belongs to a group of single stranded and enveloped RNA viruses.2 The outbreak has rapidly spread out across the global and was declared an emergency public health problem and pandemic on January 30, 2020 and March 11, 2020, respectively, by the World Health Organization.3
At the end of March 2020, a report on COVID-19 from 199 countries indicated over 800,000 cases and 39,000 deaths, with the United States, Italy, Germany, Great Britain, Spain and France experiencing high levels of COVID-19 cases and death rates and later Brazil, Iran, Russia, India, and other nations faced the burden of the disease.4 Now, the number of cases and deaths exceeds 525 and 6.2 million, respectively.5 In Ethiopia, the first COVID-19 confirmed case was detected on March 13, 2020. Following the identification and documentation of the first case, the pandemic spread-out to other regions of the country, including Tigray region, wherein this research was conducted. On October 19, 2020 Tigray region had a total of 6,188 COVID-19 confirmed cases and 38 deaths.6
COVID-19 is transmitted by close contact and droplets and is found to have a mean incubation period of 3–9 days.7–11 In most circumstances, about 20% of cases remain asymptomatic.12–14 A number of studies have revealed that asymptomatic patients have the potential to infect others.15,16 COVID-19 symptoms have a tendency to disappear after 10 days though viral shedding continues.17,18 Infection with SARS-CoV-2 primarily attacks individuals in the age category of 30–80 years.1,19 Moreover, the highest comorbidities rates are seen among COVID-19 cases with existing disease states of hypertension, diabetes mellitus, and cardiovascular diseases.20–23 Mild symptoms of fever, cough, sore throat, and myalgia are commonly experienced by most COVID-19 cases. Severe clinical conditions such as multiple organ failure, acute respiratory distress syndrome, pulmonary edema, and pneumonia are also observed in some cases.21
In Ethiopia and particularly in the Tigray region, COVID-19 management efforts were in place. There had been quarantine/isolation and treatment centers and vast information about cases were documented. However, the epidemiology and clinical features of the cases managed in the region’s isolation and treatment centers have not yet been synthesized, analyzed, and presented for comprehension by policy- and decision-makers. This study, therefore, aims at presenting the epidemiology and clinical characteristics of COVID-19 patients in Tigray region, Northern Ethiopia.
Materials and Methods
Study Design and Area
A retrospective cohort study design that involved 6,637 COVID-19 cases (Figure 1A) was conducted from six COVID-19 isolation and treatment centers of Tigray region, namely: Mekelle, Maichew, Axum, Adigrat, Shire, and Humera centers. The centers were designated to manage COVID-19 positive cases where all laboratory confirmed cases were admitted for isolation, care, and support. To enhance the identification of COVID-19 cases, the government of Tigray regional state implemented mass screening of all travelers who enter the region, individuals who had been in contact with confirmed cases of COVID-19 and individuals from high risk settings (health care workers, private business employees, long track drivers, merchants). Cases were confirmed by Polymerase Chain Reaction (PCR) in the treatment centers. Regardless of signs and/or symptom development, all individuals with laboratory confirmed SARS-CoV-2 infection were admitted to the isolation and treatment centers within 24 hours. Figure 1 Continued. Figure 1 (A) Flowchart of the study design and participants. (B) Distribution of participants by centers. (C) Number of confirmed COVID-19 patients by age and sex.

Study Participants and Period
The study participants were all laboratory-confirmed positive cases of SARS-CoV-2, who were admitted to the aforementioned isolation and treatment centers between May 7 and October 28, 2020.
Data Source and Sample
The data were collected using a standardized form from electronic medical records. The data set contains demographic characteristics, clinical information, and outcomes of the patients. All laboratory-confirmed COVID-19 patients who were admitted to the isolation and treatment centers between May 7 and October 28, 2020 were included in this study.
Inclusion and Exclusion Criteria
All COVID-19 patients who were admitted to the six isolation and treatments centers during the study period were included. Patient data with incomplete demographic and treatment outcome related electronic medical record information was excluded.
Operational Definitions
The COVID-19 cases were all individuals tested by PCR in the treatment centers and found to be infected with SARS-CoV-2. Symptomatic cases were defined as any SARS-CoV-2 positive individual with at least one sign or symptom for COVID-19, including but not limited to: cough, fever, headache, sore throat, pain, shortness of breath, diarrhea, and vomiting. Asymptomatic cases were any individual who tested positive for SARS-CoV-2 but did not have any of the symptoms. COVID-19 cases with comorbidity are those with at least one known preexisting chronic medical illness. Severity of COVID-19 was defined according to the diagnostic and treatment guidelines for SARS-CoV-2. Severe COVID-19 cases are with clinical signs of pneumonia (fever, cough, dyspnea, fast breathing) and have one of the following criteria: i) respiratory rate interval > 30 breaths/min; ii) SpO2 (saturation of peripheral oxygen) <93% at rest; iii) severe respiratory distress, and iv) oxygenation index (artery partial pressure of oxygen/inspired oxygen fraction, PaO2/FiO2) <300 mmHg.
Statistical Data Analysis
The data were coded, cleaned, and checked for completeness. STATA version 16 software was used for data processing and statistical analyses. The continuous variables were summarized as mean and standard deviation (SD), while categorical variables were presented as frequencies (%). Chi-square test or Fisher’s exact test was used to compare the epidemiological and clinical characteristics of COVID-19 patients as appropriate. A p-value of less than 0.05 was considered statistically significant.
Results
Socio-Demographic Characteristics
Our study population consisted of 6,637 confirmed COVID-19 cases that were reported from May 7, 2020 to October 28, 2020. In total, 5,593 were asymptomatic cases, of these 5,143 have recovered and discharged, while 450 were still in the isolation centers at the end of the study period. Of the symptomatic cases (1,044 (15.7%) of 6,637), 56 had died, 869 had recovered, and 119 were in the isolation and treatment centers at the end of the study period (Figure 1A). About 61% of the patients were isolated and treated in Mekelle center and 18.8% were in the Axum center (Figure 1B).
The mean age of the study participants was 31.3 years (SD=12.8). A total of 10.4% (95% CI=9.7−11.1%) of patients were younger than 20 years, 44.8% (95% CI=43.6–46.0%) were in the age range of 20–29 years, 24.5% (95% CI=23.5–25.5%) were between 30–39 years, 9.8% (95% CI=9.1−10.5%) were between 40–49 years, and 10.5% (95% CI=9.7–11.2%) were older than 49 years.
Among the symptomatic patients (1,044 of 6,637), 13.3% (95% CI=11.2–15.4%) were admitted to intensive care units due to the severity of their disease, of whom 70% (95% CI=67.2–72.8%) were male patients. Of the symptomatic patients, 6.1% (95% CI=4.6–7.5%) were non-survivors. The patients in the non-survivor group were much older than those in the survivor group [mean=53.1 years (SD=22.8) versus mean=30.8 years (SD=12.2), p-value <0.001]. About 60% of the non-survivor patients were older than 49 years. Regarding the occupation of the patients, about 6% (391 of 6,637) were health care workers and 31.2% (122 of 391) of them declared having contact with COVID-19 patients. Age was significantly correlated with the severity of the disease and treatment outcome of COVID-19 patients. The majority of COVID-19 patients (64.9%; 95% CI=63.7–66.0%) were males. Similarly, 73.2% (41 of 56) of COVID-19 deaths were in males and 55.4% (31 of 56) were in the age group of ≥50 years (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Confirmed COVID-19 Patients of Tigray, Northern Ethiopia, 2020 |
Of the male patients (4,305 (64.9%) of 6,637), a high proportion (41.4%) of confirmed COVID-19 infections were in the middle aged individuals (the age group of 20–39 years) and a lower proportion (2.0%) were in the older age groups (>69 years). From the female patients (2,332 (35.1%) of 6,637), 51.1% of COVID-19 infections were in the age group of 20–39 years and 1.6% were in the age group >69 years (Figure 1C).
Clinical Characteristics
Based on the patients’ body temperature on admission, 89.3% of the patients had temperature <37.1°C, 8.4% had 37.1–38°C and 2.3% had >38°C. These values were different between severe and non-severe patients (p-values <0.001). Of the total 6,637 COVID-19 cases, 15.7% (95% CI=14.8–16.6%) were symptomatic. Among the hospitalized patients (1,044 of 6,637), the most common symptoms at the onset of the disease as reported by patients were cough in 74.1% and fever in 39.7% of the cases. This is followed by sore throat in 27.9%, body weakness in 24.9%, and shortness of breath in 23.4% of the cases. Headache was less common, only found in 17.2% of the patients.
Among the non-survivor patients (56 (6.1%) of 925), 78.6% had shortness of breath, 76.8% had cough, 51.8% had body weakness, 33.9% had pain, 28.6% had sore throat, 26.8% had fever, and 26.8% had headache. Of the symptomatic COVID-19 cases, 13.3% were severely ill and the mortality rate among the severe COVID-19 was 40.3% (95% CI=32.1–48.4%).
From the total study participants, the sources of infection for about 50% of the COVID-19 patients were community infections, while 34.2% of the patients were imported. Among the COVID-19 patients in the study, 33.4% of the patients had a travel history.
With regard to the outcome between groups, the proportion of severely ill in the non-survivor group was significantly higher than in the survivor group (p-value <0.001). Two hundred and eighty-two (4.25%) of the patients had one or more coexisting medical conditions; the most frequent comorbidity being cardiovascular diseases accounting for 30.1%. This is followed by diabetes mellitus and respiratory diseases, 23.8% and 19.9%, respectively. The comorbidity rate in the non-survivor group was higher than that of the survivor group (44.6% versus 10.5%, p-value <0.001), and it was also higher in the severely ill group than the non-severe group (28.8% versus 10.4%, p-value <0.001). A large proportion of cardiovascular diseases, diabetes mellitus, respiratory diseases, renal diseases, and traumatic injury were observed in the non-survivor group and non-severe group (Table 2).
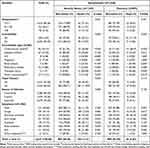 |
Table 2 Clinical Characteristics of 6,637 Confirmed COVID-19 Patients of Tigray, Northern Ethiopia, 2020 |
Among the patients with comorbidities, 43% were in the age group ≥50 years, 22% were in the age group 30–39 years, 21% were in the age group 20–29 years, 14% were in the age group 40–49 years, and 5% were in the age group <20 years. Of the patients with COVID-19, older age groups tended to have a higher proportion of cardiovascular, diabetes, and respiratory disease than younger age groups (Figure 2).
 |
Figure 2 Comorbidities among confirmed COVID-19 cases by age. *Other comorbidities: gastritis, malignancy, allergic, psychotic disorder, rabies, arthritis, epilepsy, neurological. |
Discussion
A total of 6,637 patients were admitted to the six COVID-19 isolation and treatment centers in Tigray region (Mekelle, Maichew, Axum, Adigrat, Shire, and Humera) during the study period. The mean age of patients was 31 years old (SD=12.8). Of the total, 44.8% were in the age range of 20–29 years and 34.3% were between 30–39 years.
The result showed that COVID-19 infects men more than women, with a male-to-female ratio of 1.85:1. These findings are consistent with the findings of the previous studies.24–33 The reason for the higher proportion of infections among males than females could be due to the variation in hormone concentrations of males and females which contributes to differences in immune system packages and disease susceptibility patterns. Moreover, biological sex affects the immune response to foreign bodies, resulting in sex differences in responses to infections. In this regard, studies have confirmed that males are at higher risk of diseases caused by deleterious X-linked alleles.25 Based on previous studies, evidence suggests that men tended to develop more serious COVID-19 cases and high mortality than women,24,27 which is also in line with our finding.
Of the total study participants, 5,593 (84.3%) were asymptomatic COVID-19 cases and 15.7% were symptomatic cases. Asymptomatic patients presented a hidden infection source for silent infection spread among their family, colleagues, and the community. With regards to the source of infection, earlier WHO reports34 suggested health care professionals are being infected both in the workplace (contact) and in the community, most often through infected family members. In this study, about 6% (391 of 6,637) were health care professionals with confirmed COVID-19. Of these, 57.3% (224 of 391) health care professionals got infected from the community and 31.2% (122 of 391) declared having contact with a COVID-19 patient.
Of the symptomatic patients, 11.4% were on treatment, 83.2% were discharged, and 5.4% died. Of the hospitalized patients, 13.3% were admitted to intensive care units due to the severity of their disease and 86.7% had a non-severe disease, which is consistent with previous studies conducted in south Iran and Wuhan, China.35,36 This could be due to the higher proportion of younger COVID-19 patients.
In this study, the observed overall case fatality rate among hospitalized COVID-19 patients was 6.1%, which was similar to what has been reported in China.29,37–39 However, it was significantly lower than those reported from the studies conducted in France and New York City.32,40 The overall case fatality rate of COVID-19 was 21.1% and 20.0%, respectively, in these studies. The older age of patients in those studies (median ages: 72 and 63 years, respectively) could have led to severe disease that explains the higher mortality rates.
The mortality rate increased to 40.3% among patients with severe illness. This was lower than studies conducted in France.32 The discrepancy can be due to the younger age of patients in our study that may have led to lower comorbidities and a lower mortality rate. Moreover, it could be the experience in treating COVID-19 cases and level of awareness in the later period of this pandemic. Taking the patients’ age into consideration, of the non-survival patients, 55.4% of the patients were older than 49 years and with frequent comorbidities. This finding was consistent with most previous research studies.20,27,28,32,38,39,41–43 In this study, cardiovascular diseases and diabetes mellitus were the most common comorbidities, which are aligned with the data that has been previously reported.1,27,29,32,33,39,44–46 The comorbidity rate in the non-survivor group was higher than in the survivor group (44.6% versus 10.5%, p-value <0.001), and also higher in the severe group than non-severe (28.8% versus 10.4%, p-value <0.001). Older age groups tended to have a higher proportion of cardiovascular disease, diabetes mellitus, and respiratory disease than younger age groups. Moreover, our study showed that the most frequently reported signs and symptoms on admission were cough, fever, sore throat, body weakness, shortness of breath, and pain. This was also consistent with most previous studies.20,28,47,48
Limitation
Finding the whole array of each COVID-19 patient information from the electronic medical record was a challenge as some of the records were incomplete. Hence this could limit the findings of this study.
Conclusion
The proportion of symptomatic patients was low, at only 15.7%. The observed overall case fatality rate among hospitalized COVID-19 patients was 6.1%. Non-survivors were older and had underlying comorbidities. The findings of this study can help in designing appropriate management strategies for COVID-19 patients, such as relying on mass screening, as the majority of COVID-19 cases are asymptomatic, giving due emphasis to COVID-19 patients who are old and have comorbidities such as cardiovascular diseases and diabetes mellitus would be worthy to fight the pandemic.
Abbreviations
COVID-19, Coronavirus 2019; SD, standard deviation; CI, confidence interval; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; THB, Tigray Health Bureau.
Data Sharing Statement
The dataset that are generated and analyzed for this study can be obtained from the corresponding author upon request.
Ethics
The ethics committee of the College of Health Sciences of Mekelle University approved the study with the ethical clearance registration number of IBR1826/2021. The study was conducted in accordance with the Declaration of Helsinki. The Tigray Health Bureau waived the requirement informed consent before the study started due to the urgent need to collect epidemiological and clinical data. All information collected from patient cards was kept strictly confidential as there were no personal identifiers used and neither the raw data nor the extracted data were passed to a third person.
Disclosure
The authors declare that they have no competing interests.
References
1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi:10.1016/S0140-6736(20)30183-5
2. Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5(4):536–544. doi:10.1038/s41564-020-0695-z
3. World Health Organization. Global COVID-19 report;2020. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf.
4. World tracking coronavirus: map, data and timeline. Available from: https://bnonews.com/.
5. World Health Organization. Global COVID-19 report; 2022. Available from: https://covid19.who.int.
6. Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi:10.1016/S0140-6736(20)30154-9
7. Schwartz KL, Achonu C, Buchan SA, et al. Epidemiology, clinical characteristics, household transmission, and lethality of severe acute respiratory syndrome coronavirus-2 infection among healthcare workers in Ontario, Canada. PLoS One. 2020;15(12). doi:10.1371/journal.pone.0244477
8. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi:10.1056/NEJMoa2001316
9. Tindale LC, Coombe M, Stockdale JE, et al. Transmission interval estimates suggest pre-symptomatic spread of COVID-19. Med Rxiv. 2020. doi:10.1101/2020.03.03.2002998310
10. Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease. 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;10:M20–0504. doi:10.7326/M20-0504
11. Nishiura H, Kobayashi K, Miyama T, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int J Infect Dis. 2020;94:154–155. doi:10.1016/j.ijid.2020.03.020
12. Mizumoto K, Kagaya K, Zarebski A, Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25(10):2000180. doi:10.2807/1560-7917.ES.2020.25.10.2000180
13. Ng OT, Marimuthu K, Chia PY, et al. SARS-CoV-2 infection among travelers returning from Wuhan, China, N. Engl J Med. 2020;382:1476–1478. doi:10.1056/NEJMc2003100
14. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323(14):1406–1407. doi:10.1001/jama.2020.2565
15. Rothe C, Schunk M, Sothmann P. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–971. doi:10.1056/NEJMc2001468
16. Wang L, Gao YH, Lou LL, Zhang GJ. The clinical dynamics of 18 cases of COVID-19 outside of Wuhan, China. Eur Resp J. 2020;55(4):2000398. doi:10.1183/13993003.00398-2020
17. Liu Y, Ning Z, Chen Y, et al. Aerodynamic characteristics and RNA concentration of SARS-CoV-2 aerosol in Wuhan hospitals during COVID-19 outbreak. BioRxiv. 2020. doi:10.1101/2020.03.08.982637
18. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239–1242. doi:10.1001/jama.2020.264
19. Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi:10.1016/j.ijid.2020.03.017
20. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846–848. doi:10.1007/s00134-020-05991-x
21. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi:10.1016/S0140-6736(20)30566-3
22. Ma C, Gu J, Hou P, et al. Incidence, clinical characteristics and prognostic factor of patients with COVID-19: a systematic review and meta-analysis. MedRxiv. 2021. doi:10.1101/2020.03.17.20037572
23. Chen N, Zhou M, Dong XY, et al. Epidemiological and clinical characteristics of 99 cases of 2019 Novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi:10.1016/S0140-6736(20)30211-7
24. Jin JM, Bai P, He W, et al. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. 2020;8:152. doi:10.3389/fpubh.2020.00152
25. Scully EP, Haverfield J, Ursin RL, et al. Considering how biological sex impacts immune responses and COVID-19 outcomes. Nat Rev Immunol. 2020;20:442–447. doi:10.1038/s41577-020-0348-8
26. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi:10.1016/S2213-26002030079-5
27. de Souza WM, Buss LF, Candido DDS, et al. Epidemiological and clinical characteristics of the COVID-19 epidemic in Brazil. Nat Hum Behav. 2020;4:856–865. doi:10.1038/s41562-020-0928-4
28. Shahriarirad R, Khodamoradi Z, Erfani A, et al. Epidemiological and clinical features of 2019 novel coronavirus diseases (COVID-19) in the South of Iran. BMC Infectious Dis. 2020;20:427. doi:10.1186/s12879-020-05128-x
29. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel Coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi:10.1001/jama.2020.1585
30. Zhang -J-J, Dong X, Cao -Y-Y, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75(7):1730–1741. doi:10.1111/all.14238https://onlinelibrary.wiley.com/doi/full/10.1111/all.14238
31. Hassan S, Sheikh FN, Jamal S, et al. Coronavirus (COVID-19): a review of clinical features, diagnosis, and treatment. Cureus. 2020;12(3):e7355. doi:10.7759/cureus.7355
32. Vanhems P, Gustin M-P, Elias C, et al. Factors associated with admission to intensive care units in COVID-19 patients in Lyon-France. PLoS One. 2021;16(1):e0243709. doi:10.1371/journal.pone.0243709
33. Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547. doi:10.1183/13993003.00547-2020
34. World Health Organization. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19); 2020. Available from: https://www.who.int/publications/i/item/report-of-thewho-china-joint-mission-on-coronavirus-disease-2019-covid-19.
35. El-Sokkary RH, El-Kholy A, Mohy Eldin S, et al. Characteristics and predicting factors of corona virus disease-2019 (COVID-19) among healthcare providers in a developing country. PLoS One. 2021;16(1):e0245672. doi:10.1371/journal.pone.0245672
36. Lai X, Wang M, Qin C, et al. Coronavirus disease 2019 (COVID-2019) infection among health care workers and implications for prevention measures in a tertiary hospital in Wuhan, China. JAMA Netw open. 2020;3(5):e209666. doi:10.1001/jamanetworkopen.2020.9666
37. Zhang J, Wang X, Jia X, et al. Risk factors for disease severity, un improvement, and mortality in COVID-19 patients in Wuhan, China. Clin Microbiol Infect. 2020;26(6):767–772. doi:10.1016/j.cmi.2020.04.012
38. Zhang G, Hu C, Luo L, et al. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol. 2020;127:104364. doi:10.1016/j.jcv.2020
39. Zhang X-B, Hu L, Ming Q, et al. Risk factors for mortality of coronavirus disease-2019 (COVID-19) patients in two centers of Hubei province, China: a retrospective analysis. PLoS One. 2021;16(1):e0246030. doi:10.1371/journal.pone.0246030
40. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–2059. doi:10.1001/jama.2020.6775
41. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):934–943. doi:10.1001/jamainternmed.2020.0994
42. Wang X, Fang X, Cai Z, et al. Comorbid chronic diseases and acute organ injuries are strongly correlated with disease severity and mortality among COVID-19 patients: a systemic review and meta-analysis. Research. 2020;2020:2402961. doi:10.34133/2020/2402961
43. Cao J, Tu WJ, Cheng W, et al. Clinical features and short-term outcomes of 102 patients with corona virus disease 2019 in Wuhan, China. Clin Infect Dis. 2020;71(15):748–755. doi:10.1093/cid/ciaa243
44. Haas LEM, de Lange DW, van Dijk D, van Delden JJM. Should we deny ICU admission to the elderly? Ethical considerations in times of COVID-19. Critical Care. 2020;24(1):321. doi:10.1186/s13054-020-03050-x
45. Borges NIJ, Cacic N, Abdulazeem HM, et al. Novel coronavirus infection (COVID-19) in humans: a scoping review and meta-analysis. J Clin Med. 2020;9(4):941. doi:10.3390/jcm9040941
46. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi:10.1056/NEJMoa2001017
47. Chen J. Pathogenicity and transmissibility of 2019-nCoV-A quick overview and comparison with other emerging viruses. Microbes Infect. 2020;22(2):69–71. doi:10.1016/j.micinf.2020.01.004
48. Wu J, Wu X, Zeng W, et al. Chest CT findings in patients with Corona virus disease 2019 and its relationship with clinical features. Investig Radiol. 2020;55(5):257–261. doi:10.1097/RLI.0000000000000670
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
