Back to Journals » Drug Design, Development and Therapy » Volume 14
Enteric-Coated Strategies in Colorectal Cancer Nanoparticle Drug Delivery System
Authors Wathoni N , Nguyen AN, Rusdin A, Umar AK , Mohammed AFA, Motoyama K, Joni IM, Muchtaridi M
Received 23 July 2020
Accepted for publication 23 September 2020
Published 21 October 2020 Volume 2020:14 Pages 4387—4405
DOI https://doi.org/10.2147/DDDT.S273612
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Qiongyu Guo
Nasrul Wathoni,1,2 An Ny Nguyen,3 Agus Rusdin,1 Abd Kakhar Umar,1 Ahmed Fouad Abdelwahab Mohammed,4 Keiichi Motoyama,5 I Made Joni,2,6 Muchtaridi Muchtaridi2,7
1Department of Pharmaceutics and Pharmaceutical Technology, Faculty of Pharmacy, Universitas Padjadjaran, Sumedang 45363, Indonesia; 2Functional Nano Powder University Research Center of Excellence, Universitas Padjadjaran, Sumedang 45363, Indonesia; 3Department of Pharmacy, Faculty for Chemistry and Pharmacy, Ludwig Maximilians Universität Munich, Germany; 4Department of Pharmaceutics, Faculty of Pharmacy, Minia University, Minia 61519, Egypt; 5Graduate School of Pharmaceutical Sciences, Kumamoto University, Kumamoto 862-0973, Japan; 6Department of Physics, Faculty of Mathematics and Natural Sciences, Universitas Padjadjaran, Sumedang 45363, Indonesia; 7Department of Pharmaceutical Analysis and Medicinal Chemistry, Universitas Padjadjaran, Sumedang 45363, Indonesia
Correspondence: Nasrul Wathoni
Department of Pharmaceutics and Pharmaceutical Technology, Faculty of Pharmacy, Universitas Padjadjaran, Jatinangor 45363, Indonesia
Tel +6222 842 888888
Email [email protected]
Abstract: Colorectal cancer is one of the most common cancer diseases with the increase of cases prevalence > 5% every year. Multidrug resistance mechanisms and non-localized therapy become primary problems of chemotherapy drugs for curing colorectal cancer disease. Therefore, the enteric-coated nanoparticle system has been studied and proved to be able to resolve those problems with good performance for colorectal cancer. The highlight of our review aims to summarize and discuss the enteric-coated nanoparticle drug delivery system specific for colorectal cancer disease. The main and supporting literatures were collected from published research articles of journals indexed in Scopus and PubMed databases. In the oral route of administration, Eudragit pH-sensitive copolymer as a coating agent prevents the degradation of the nanoparticle system from the gastric fluid and releases drug to intestinal-colon track. Therefore, it provides a colon-specific targeting ability. Impressively, enteric-coated nanoparticles having a sustained release profile significantly increase the cytotoxic effect of chemotherapeutic drugs and achieve cell-specific target delivery. The enteric-coated nanoparticle drug delivery system represents an excellent modification to improve the effectiveness and performance of anticancer drugs for colorectal cancer disease in terms of the oral route of administration.
Keywords: drug delivery system, oral route, cytotoxic, anticancer drugs
Introduction
Colorectal cancer is one of the most common cancers in the world with about 1.9 million new colorectal cancer (CRC) cases reported in 2018 and 900,000 deaths, making it the third most commonly diagnosed cancer worldwide.1 In 2020, around 147,950 individuals will be predicted with CRC, 53,200 might die from these diseases.2 Even though the prognosis of CRC patients has improved over the last few decades in many developed countries, mostly due to improved prevention and treatment,3–6 the incidence and mortality in low-and middle-income countries are rising rapidly, in part due to adaptation of western-lifestyle.7
Conventional colon cancer treatment depending on the tumor stage consists mainly of surgery, chemotherapy, and radiation.3,8–11 However, these methods bear several risks. Besides, the usual risks of surgery such as major blood loss and infections, colectomy might lead to serious tissue damage causing leakage of the anastomosis.12–19 It is also worth mentioning that the risk of fecal and urinary incontinence after radiation therapy is high.5,20–25 Another problem associated with radiotherapy and chemotherapy is tissue toxicity as both cancerous and healthy cells are affected.26–28
In addition, the application of chemotherapeutics is greatly limited, ascribable to multi-drug resistance caused by efflux mechanisms, enhancement of drug inactivation, or mutations of the drug target.28–31 Besides that, common chemotherapeutics like 5-Fluorouracil have a poor site-specificity leading to the fact that a growing dose size of anti-cancer drugs is required, which increases toxic side effects.32 For example, the overall response rate for 5-Fluorouracil regarding colorectal cancer alone is only 10% to 15%.29 Furthermore, researchers are challenged to overcome the limitations of conventional cancer therapy with new approaches.
Targeted anti-cancer agents such as Bevacizumab and Cetuximab have been developed. Both are monoclonal antibodies specific for molecular targets, which block transduction pathways or cancer proteins. These targeted monoclonal agents are able to reach the tumor site specifically.12,33,34 Currently, first-line treatments combine targeted therapy and fluoropyrimidine-based chemotherapy.35,36
In order to increase anti-tumor efficacy, current therapeutic methods involve the combination of different chemotherapeutic drugs in a series of cycles.3,12,31 However, the emergence of drug-resistant tumor cells reduces the efficacy of chemotherapeutics and endure a crucial problem in colon cancer chemotherapy.37
One promising approach to improve the efficacy and to reduce the systematic side effects of anti-cancer agents is nanoparticle drug delivery systems. They are biodegradable, nano to submicronic colloidal systems with a diameters range between 3 and 200 nm, able to effectively carry the anti-cancer agents to the tumor site,30,34,38 attaining a high local drug concentration by site-specific targeting, enhanced permeability, and greater retention.27,39–44 Thus, the use of nanocarriers can reduce the unwanted systemic side effects and drug resistance.27,45
However, nanoparticles for colon-targeted oral drug delivery systems have to overcome pH-sensitivity and transit time in the stomach. For oral administration, the formulation must be protected in order to prevent degradation, premature drug release and absorption before reaching the colon.46,47 These problems can be overcome by enteric coating of the nanoparticle delivery system. The enteric coating acts as a barrier protecting the loaded drug against the stomach acidic environment and controlling its release to reach sites in the lower gastrointestinal tract.32,48–52
In recent years more and more nanoparticles for various purposes have been developed. Previous review articles discussed the application of polymers in delivering cancer drugs to colorectal cancer individually.53–55 This review article summarizes and discusses the enteric-coated nanoparticles as oral drug delivery systems for treating colorectal cancer. In this review, the comparison of different applied formulations and polymers for enteric-coated nanoparticles in colorectal cancer drug delivery system were discussed.
Methodology
This review is focused on published articles indexed in Scopus and PubMed database using the keyword “enteric-coated nanoparticle colorectal cancer,” “enteric-coated nanoparticle cancer,” and “enteric-coated nanoparticles.” Opinions, assessments, and unrelated subjects such as pharmacological characteristics and bioactivities have been utilized for exclusion criteria. The flowchart of the methodology can be seen in Figure 1. The distribution of articles based on the year of publication can be seen in Figure 2.
 |
Figure 1 Flowchart of methodology. |
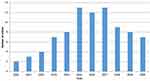 |
Figure 2 Distribution of colorectal cancer articles based on the year of publication. |
In this review, we examined the studies on nano-sized cancer drugs with a macroporous sponge and multilayer dispersion system from macro to nano-sized. This system serves as a protection, targeted delivery to cancer cells, modification of release, and enhancing cell uptake in cancer drugs. Therefore, we also discussed the enteric-coated nanoparticle drug system for non-colorectal cancer and its development in targeted delivery to colorectal cancer.
Colorectal Cancer
Colorectal cancer is a type of cancer that grows in the large intestine (colon), or at the very end of the large intestine that is connected to the rectum. The term colorectal cancer refers to cancer that develops slowly. Its development starts from tumor or tissue growth in the inner lining of large intestine or rectum.56 In general, colorectal cancer originates from the inner wall of colorectal epithelial layer as a polyp, which then invades the lymph node and muscles surrounding it. In the next stage, colorectal cancer will spread to other organs, especially the liver. Recurrence and widespread cancer (metastatic) distribution are the two main factors that are affecting the survival of patients with colorectal cancer. The chance of survival of colorectal cancer patients can reach up to around 90% for 5 years if colorectal cancer did not metastasize. But the survival rate is reduced to around 12% in patients with metastatic colorectal cancer.1,57,58 Several factors are influencing the incidence of colorectal cancer including age, gender and genetic factors. Concomitant chronic diseases such as ulcerative colitis, diabetes, and obesity can increase the risk of developing colorectal cancer.58–61 At this time, patients with colorectal cancer are being treated by surgical removal of the tumor, chemotherapy as well as radiation therapy.62,63
Nanoparticle Drug Delivery System
Nanoparticles are defined as size structures ranging from 1 to 100 nm in at least one dimension. However, the “nano” prefix refers to nanostructured particles, is usually used for particles up to several hundred nanometers in secondary size contained nano-sized primary particles.64,65 Nanocarriers have certain physicochemical and biological characteristics, which makes it easier to enter cells in comparison to larger molecules, so they can successfully deliver active substances intracellularly,66–68 and have the ability to carry cancer drugs having small or large molecular weights including genes or proteins. Thus, nanocarriers can be used for targeted anticancer delivery approaches for better accumulation in cancer cells.34,69–74 In addition, nanocarriers can increase the solubility of hydrophobic drugs, protect drugs from degradation, reduce renal clearance, increase the half-life, and can be used for controlled systemic release.34,75
Nanotechnology has been widely developed as a new strategy for drug delivery and cancer treatment. When compared to conventional drug delivery systems, nanotechnology-based drug delivery systems have superior potential in several aspects, for example, targeting specific organs, increased circulation times and controlled systemic release.75 The application of nanotechnology has the potential to overcome drug resistance especially through reversing Multi-Drug Resistance (MDR). Thus, allowing sufficient drugs to accumulate in the cytoplasm resulting in remarkable improvement in chemotherapy efficiency.76–81
Enteric Nanoparticle Development
In 1930, the first ingredient used in the enteric coating system was shellac. The enteric coating technique was first introduced by Unna in 1984 in the form of keratin-coated pills. Micro- to nano-encapsulated forms were then developed due to various needs in improving the quality and stability of drugs such as controlling drug release, reducing gastrointestinal irritation, and preventing drug interactions. This delivery system was first developed by Bodmeier et al (1989) using chitosan and alginate as coatings.82,83 Furthermore, the development of nano-sized enteric coating systems has been developed to date with various coating modifications and the addition of cell targeting or magnetic labeling agents (see Figure 3).
 |
Figure 3 The development of enteric nanoparticle. |
Enteric-Coated Nanoparticle Formulations for Non-Colorectal Cancer
Each part of the digestive tract has a different pH. The stomach has an acidic pH environment (1–3) while the small intestine has a slightly acidic to neutral environment pH (5.9 −7.8). The colon has a pH ranging from 5 to 8.84–86 Based on physiological conditions of the gastrointestinal tract, targeted drug delivery systems that are suitable for certain parts of the gastrointestinal release the active compounds triggered by pH. pH-dependent coating technology is usually applied to protect active substances from degradation by gastric acid and as targeted delivery in certain parts of the digestive tract.87,88 Enteric-coated drug delivery systems are designed to be able to survive in the acidic environment and disintegrate at a higher pH environment, preventing the degradation of active compounds by gastric fluid components.88,89 Some examples of enteric-coated drug formulas for non-colorectal cancer are summarized in Table 1.
 |  |  |
Table 1 Enteric-Coated Nanoparticle Formulations for Non-Colorectal Cancer |
The application of enteric-coated in several studies has successfully delivered drugs through the gastric channel (low pH) by maintaining the stability of active substances, even those in the form of peptides and proteins such as vaccines,99,104,125 and insulin94,95,98 to be absorbed via lymphatic or bile pathways. These formulas can be used as innovators in the development of targeted delivery systems to colon cancer cells.
Natural or synthetic polymers are used in the enteric-coated system. However, in the colorectal drug delivery system, the polymers used need to be modified in order to deliver drugs to the targeted cells and increase its bioavailability. Therefore, mediators such as receptors, peptides, and other compounds are needed to be linked to the surface of the carrier. The mediators facilitate the attachment of the drug to the cell and increase its uptake.
Enteric-Coated Nanoparticle Formulations for Colorectal Cancer
Enteric-coated nanoparticles are one of the drug delivery technologies that can improve the bioavailability of drugs by oral administration,50,133–135 increase intracellular penetration and retention time, control the release of encapsulated drugs and targeted delivery in specific parts of the gastrointestinal tract such as in the treatment of colorectal cancer.136 Cellular uptake and efficacy of nanoparticle drug delivery systems for colorectal cancer therapy are influenced by several factors, namely, size, shape, and surface chemistry.137–139 The size of the drug delivery carrier plays an important role in colorectal cancer therapy. Nanoparticles sizes around 100–200 nm have better cancer-targeting properties than larger particles. This can increase selective accumulation in the colon tissue due to the epithelial-enhanced permeability and retention effect. This can increase selective accumulation in the colon tissue.140 In order to be absorbed into the cells, the particle size of the drug should not exceed 104 nm. With a particle size of 102 nm, nanoparticle drugs are generally absorbed via the clathrin pathway.141 The illustration of anticancer drug delivery and its release in the colon can be seen in Figure 4.
 |
Figure 4 The illustration of nanosized drug entrapped in polymeric matrix (A) and its mechanism in release and delivery at colon (B). |
Materials used for enteric coating are usually water-resistant or pH-sensitive (Table 2). Enteric-coated systems use polymer coatings that do not dissolve in a gastric fluid consequently prevent or slowing down the release of drug compounds in stomach.89 Eudragit is a pH-dependent enteric-coated polymer, dissolves in a pH>5.5 medium,142 and has the highest entrapment ability compared to other polymers.143,144 It protects the active ingredient from gastric fluid, improves drug effectiveness, and enables targeting specific areas at intestine. Eudragit polymers are versatile polyacrylate polymers with various degrees of solubility, which make it suitable for sustained release formulation. Eudragit S100 has solubility characteristics above pH 7, making it suitable for use in colonic release targeting. Therefore, it is often used as an enteric coating in the drug delivery system for colorectal cancer.
 |
Table 2 Enteric-Coated Nanoparticle Formulations for Colorectal Cancer |
Chitosan Nanoparticle
In 2017, Sun et al tried to develop a nanoparticle system for 5-Fluorouracil as drug payload by using ionic gelation. In this study, they used chitosan as the main carrier. The observed mean particle size was around 283.9 nm, with 44.28% of entrapment efficiency and 20.12% loading capacity. The highest entrapment efficiency and drug-loading could be achieved by using a 1:1 mass ratio of 5-FU and Chitosan. The PDI was around 0.252, indicating that the distribution is relatively homogeneous. In addition, the nanoparticle system showed good stability with a zeta-potential of about 45.3 mV. Impressively, the in vitro and in vivo drug release study implies that compared to the normally used 5-FU solution, a notably sustained and extended drug release by 5-FU Chitosan nanoparticles can be observed. Regarding the bioavailability in rats, the AUC value of 5-FU Chitosan nanoparticles showed more than 2-fold increase to the solution. Furthermore, the nanoparticles show the same in vitro cytotoxic efficacy on gastric cancer SGC-7901 as conventional 5-FU injections.145
Another study from Tummala et al in 2015 demonstrated that nanoparticle formulations with enteric coating become an excellent modification of the previously mentioned nanoparticles. In this study, the solvent emulsification evaporation technique was used to prepare the same type of nanoparticles, which were additionally coated with an enteric coating (Eudragit S100) to protect the nanoparticles from degradation in gastric fluid and to achieve drug release when the carrier reaches the intestine. Comparing the 1:1 mass ratio formulations of S. Tummala and L. Sun, the particle size with about 192 nm which is much smaller, even though having an extra enteric coating. Moreover, the average particle size of the formulation prepared using a 1:3 mass ratio was about 138 nm, which is even smaller. In addition, the study revealed a significantly higher entrapment efficiency (69.18%) and drug loading (28.14%), using a drug: polymer ratio of 1:3. In contrast to the study of Sun et al the drug loading did not increase with the increase of 5-FU. Other than that, the other particle characteristics regarding stability and distribution showed similar results.
In in vitro study, non-enteric-coated 5-FU chitosan nanoparticles released up to 70% of 5-FU before reaching the colonic fluid. Due to the Eudragit S100 coating, which contains acidic functional groups, dissolving only in alkaline colonic medium, the enteric-coated nanoparticles remain stable in gastric fluids and reach the tumor sites in the colon. Drug release of enteric-coated nanoparticles started only after 4h in simulated intestinal fluid and showed a sustained release profile over 24h of a time period, whereas non-enteric-coated nanoparticles released about 50% of 5-FU after 2 to 3 hours and up to 70% before reaching colonic fluid.32
Continuing the previous study, Tummala et al focused on improving 5-FU anti-cancer activity of 5-FU loaded enteric-coated chitosan nanoparticles, they have evaluated their apoptotic activity in vitro using HCT 116 colorectal cancer cells. A decrease in the IC50 value of 5.5 folds compared to pure drugs was shown, whereas plain nanoparticles showed no toxicity indicating the safety of nanoparticles. Furthermore, the research demonstrated the ability in localizing the drug at the colon and releasing the majority of the payload once it arrives at the ascending colon after 4 h. Moreover, the improved apoptotic activity of enteric-coated nanoparticles was determined compared with free nanoparticles and pure 5-FU133
In conclusion, an enteric-coated nanoparticle system with a significant sustained and localized release and enhanced anticancer activity for colorectal cancer treatment was successfully developed.
As for various cancer diseases including colorectal cancer hyaluronic acid (HA) receptors in tumor cells are overexpressed, making it a suitable target for anticancer drugs, which seems to be a promising approach to improve orally targeted drug delivery systems for colorectal cancer.
In a study from Jain et al in 2010 hyaluronic-acid coupled Oxaliplatin (L-OHP) loaded nanoparticles with Chitosan as the main carrier were prepared using ionotropic gelation as an attempt to develop an optimal targeted delivery system for colorectal cancer. Afterward, the nanoparticles were processed into pellets, which were then coated with Eudragit S100.
Characterization studies showed that HA-coupled chitosan nanoparticles had similar characteristics as the previously mentioned nanoparticles. However, compared to uncoupled nanoparticles, the entrapment efficiency of HA-coupled nanoparticles was significantly less.
Other than that, zeta potentials of uncoupled chitosan nanoparticles (CTNPOP) and HA-coupled chitosan nanoparticles (HACTNPOP) formulations were observed to be around 40.3 and 10.0 mV, which mean that the stability differs significantly. It was also concluded that the optimal total weight gain regarding the film thickness is 10%. In this range, the coat is stable enough to pass gastric fluids in the upper gastrointestinal tract without degradation but is still able to ensure an optimum drug release in the colon. In terms of the in vitro drug release, non-coupled nanoparticles had a higher drug release profile than the HA-coupled ones. HA coupling might act as an additional barrier for drug diffusion, which has to be overcome. Furthermore, the mural study could confirm, that coated nanoparticles mainly started to release the drug in the ascending colon after 4 to 5 hours, which implies, that colon-specific delivery of L-OHP was achieved after oral administration of enteric-coated nanoparticles and, that the enteric coating process was successful.
As expected, the biodistribution studies show, that HA-coupled nanoparticle increased the drug concentration at the tumor site more effectively than the uncoupled nanoparticles or the free drug, which means that the researchers were able to achieve a more specific targeted approach to the colorectal cancer site by using hyaluronic acid as targeting ligand. Impressively, tumor regression studies on C57 Balb/c mice could successfully confirm HA-coupled nanoparticles being able to stop tumor proliferation more effectively than free L-OHP and CTNPOEPs. It could be observed that the growth of tumor cells could be delayed for about 8 days, which is twice as long as non-coupled nanoparticles. These results imply that nanoparticles coupled with targeting ligand like hyaluronic acid have a significant effect.39 Five years later in 2015, Jain et al used 5-FU instead of Oxaliplatin and attempted to optimize the chitosan nanoparticles. The preparation method was comparable to the study from 2010 and very similar results regarding the characterization could be observed.155
Pectin-Eudragit Nanoparticle
Subudhi et al attempted to prepare Eudragit S100-coated nanoparticles, which are loaded with 5-FU for colon targeting in cancer therapy. Instead of using Chitosan like in the previously mentioned articles, citrus pectin was used. Conveniently, citrus pectin also acts as a target mediator at the same time since it additionally functions as a ligand for galectin-3 receptors. Like hyaluronic acid receptors, Galectin-3 receptors are also overexpressed in colorectal cancer, making it a promising and specific target for anticancer medication. With a mean particle size of about 218.12 nm the enteric-coated nanoparticles are slightly bigger than coated nanoparticles consisting of Chitosan.
Surprisingly the zeta potential of the coated citrus pectin nanoparticles could be found around the value of −27.5 mV. Compared to the same non-coated nanoparticles with −18.4 mV, an enormous improvement could be found, but the optimal stability could not be achieved as the zeta potential should be >|30| mV to provide good stability of colloidal dispersions. In contrast to chitosan nanoparticles of previously mentioned articles, citrus pectin nanoparticles showed less entrapment efficacy of only around 35.15%. That being said, regarding particle size and entrapment efficacy, citrus pectin nanoparticles seem to be less optimal for colon targeted delivery systems than chitosan nanoparticles.
Thus, the effective drug delivery depends on the size, stability of the suspension and provide well-dispersed nanoparticles. The morphology of the nanoparticles also plays an important role on the hydrodynamic of the drug delivery and consequently affect the kinetic reactivity of the colloidal systems.
The in vitro drug release study in simulated gastrointestinal fluid mediums at different pH values showed that the enteric-coated nanoparticles did not release a significant amount of 5-FU within the first 4 hours in simulated intestinal fluid, which is similar to the result of S. Tummala et al, whereas the release rate from nanoparticles starts to increase with the increasing pH values of the release medium. Therefore, as expected, the amount of drug release of non-coated and coated nanoparticles differs significantly. Eudragit S100 coating was able to reduce the drug release by about 19% after 24 hours. In medium containing 2% rat cecal content, it could be stated that the drug release of both coated and non-coated nanoparticles was drastically increased by the numerous anaerobic bacteria, which could digest pectin, leading to 5-FU being released.
All in all, it can be concluded, that the prepared coated citrus nanoparticles have a controlled and sustained release profile. Based on sulforhodamine B assay, it was successfully proven that the cytotoxicity could be increased by using citrus pectin nanoparticles as dosage form (LC50 = 36.4 μg/mL) compared to the free drug solution, but when coated with Eudragit S100 the nanoparticles (LC50 = 94.2 μg/mL) showed less cytotoxicity than the free 5-FU (LC50 = 56.7 μg/mL), which is probably due to the Eudragit S100 coating, that remains mostly stable in acidic pH of the medium used in the cell cytotoxicity study.
As expected, it was verified that the nanoparticles covered with Eudragit S100 released the least amount of drug in the upper GIT compared to the non-coated nanoparticles and free drug solution. In addition, there was a significant increase in colon 5-FU concentration in the case of Eudragit-coated citrus pectin nanoparticles due to facilitated microflora degradation in the colonic region.
The plasma drug concentration was analyzed to evaluate drug absorption. The maximum drug plasma level of non-coated nanoparticles was reached after 8 h, mainly released in the small intestine, also showing a prolonged and delayed-release profile due to low permeability. On the other hand, enteric-coated nanoparticles reached their maximum plasma level after 12h, slowly releasing the drug in the colon within 12 hours, achieving a higher drug concentration and prolonged effect in the colon site compared to the non-coated nanoparticle and the free solution. In addition, Eudragit-coated nanoparticles showed a relatively low drug plasma level at all time points, and as a result, the risk of severe systematical side effects is reduced and the exposure time to the tumor site in the colon is prolonged.149
PMMA-Eudragit Nanoparticle
In 2015 another approach on developing nanoparticles as a colon targeted delivery system was attempted. Ma et al first prepared Cy5-labelled PMMA-Eudragit RS PO nanoparticles (Cy5 NPs). Subsequently, they were incorporated in IR750-dyed-chitosan-Hypromellose microcapsules using ionotropic gelation. The microcapsules were then coated with Eudragit S100 eventually. Other than the previously mentioned studies, the nanoparticles were not loaded with an anti-cancer agent. Thus, the nanoparticles were not coupled with a specific target mediator for tumor cells in the colon site. In the study, they tried to compare site-specificity of free nanoparticles and nanoparticles in a microcapsule-system and evaluated their potential for colon-targeting.
After 2 hours of in vitro incubation in simulated gastric fluid and 6 hours in intestinal fluid, only less than 4% of nanoparticles from Eudragit S100-coated IR750 MCs were released. Another 9% were released in the following 6 hours in simulated colonic fluid, which not only demonstrates an overall relatively slow release rate but also showing that Cy5 nanoparticles could be at least successfully released from Chitosan-HPMC microcapsules in colonic fluids. Moreover, a significant number of nanoparticles have been already released in the small intestine before reaching the colon. Therefore, the aim of colon-specificity could not be achieved.
To have a significant therapeutic effect, the NP must not only be released but also penetrate into the tumor tissue. In order to investigate the cellular uptake of Cy5 nanoparticles, human colon adenocarcinoma (HT29) and embryonic fibroblast (NIH/3T3) cells were used. Altogether it could be noted that the general NP from Eudragit S100-coated IR750 MCs uptake increased with the increase of NP concentration and time of exposure. Due to the higher proliferation rate of cancerous cells, the NP uptake in HT29 was higher than the uptake in NIH/3T3 cells.
Surprisingly, in contrast to the in vitro study, all of the drug was released in vivo in the lower small intestine. Altogether it could be concluded that there is an efficient, but non-specific uptake of nanoparticles in both normal and cancerous cells. After oral administration in mice, the biodistribution of free Cy5 NPs and Eudragit S100-coated Cy5 NP-in-IR750 microcapsules was examined by using fluorophore-based animal imaging. It could be stated that free Cy5 NPs and Eudragit S100-coated Cy5 NP-in-IR750 MCs, showed stomach retention over 24 hours, owing to adhesion to the gastric mucosal surface.
Over 24 hours after oral administration, the non-encapsulated nanoparticles had a restricted allocation in the colon. On the other hand, the enteric-coated MCs increased the delivery of nanoparticles to the colon due to prolonged nanoparticle residence in the gastrointestinal tract of the mouse and reduced nanoparticle excretion in feces, although the MCs had poor colon specificity.150
PLGA-Eudragit Nanoparticle
In 2011, Nassar was able to prepare nanocapsules loaded with Docetaxel using PLGA [poly(lactic-co-glycolic acid)] as the main carrier, which was then embedded in microparticles coated with Eudragit L. The average diameter and zeta potential values of the NCs formed were around 300 nm and −60.1 mV to −37.7mV, which is the prevalent size for PLGA nanoparticles, and also demonstrates that the solution is stable. Interestingly, the nanoparticle-microparticle system showed a significant better oral absorption and higher bioavailability compared to both, the docetaxel solution and the free docetaxel NC formulation.
Cell viability assay, MTT, on Walker 256 cells could demonstrate, those blank microcapsules alone have a certain toxic effect due to the cytotoxicity of Eudragit L. A higher intrinsic cytotoxic activity can be seen when testing free docetaxel nanoparticles.
Interestingly, there were even more pronounced cytotoxic impacts of nanocapsulated docetaxel microparticles than blank microparticles and Docetaxel in solution. At a Docetaxel concentration around 5 µg/mL, it could be observed that cytotoxicity increased significantly compared with the free solution and blank nanocapsules. These results could be found for an incubation time of 72 hours in a cell growth medium. When incubating only for 3 hours, we can surprisingly see that the docetaxel solution has a significantly higher cytotoxic effect than the microparticle system. Comparable results could be observed in the studies of M. Subudhi, where coated nanoparticles had less cytotoxicity effect than free nanoparticles and free drug solution. It can be assumed that the enteric coating could be the reason for this result. Only 3 hours of incubation may not be enough time for the polymer to degrade, which might show a delayed-release profile because Eudragit L is only soluble at pH level above 6.156 Furthermore, the microcapsules showed promising stability for one hour in a solution with a pH of 1.2, whereas a complete degradation of the enteric coating could be observed at pH value of 7.5.
The study was also able to show, that an enormous improvement in docetaxel oral absorption was achieved by this nanoparticle system. A higher bioavailability and lower clearance could be observed compared to both the docetaxel solution and the docetaxel NCs injected intravenously.157
Sodium Alginate-Eudragit Nanoparticle
Research conducted by Ma (2013) shows a double coating of indomethacin-complexed Eudragit RS nanoparticles that are incorporated into alginate microcapsules successfully delivering indomethacin to the colon with 60% drug loading. The nanoparticles’ size ranges from 116 nm with a drug loading of 5%. The entrapment efficiency increases when the nanoparticle-microcapsule system was drained (0.7% alginate). The nanoparticles also release the drug immediately in the gastric and intestinal tract by 90%. But, the double coating using alginate as the outer layer can maintain the drug entrapment up to the colon and reduce systemic toxicity from indomethacin.152 Meanwhile, research conducted by Rajpoot and Jain (2020) resulted in targeted cancer drug delivery to colon cancer cells using radio labelling and the addition of folic acid to solid lipid nanoparticles as ligand cell targeting. The solid lipid nanoparticles (SLN) that have been labeled and given the ligand were then encapsulated into the S-100 eudragit polymer and alginate. The results showed that the maximum drug accumulation was achieved to the cancerous tissue in the colon in the alb/c mouse model.153
Albumin Nanoparticle
The delivery system of indomethacin to the colon has also been studied by Cerchiara et al by using a multi-coating system. The increased solubility of Indomethacin was significant with increasing cyclodextrin concentrations. However, the swelling index of the indomethacin-cyclodextrin complex was smaller than that of indomethacin-albumin. The swelling index of Indomethacin-cyclodextrin-albumin was greater in an alkaline atmosphere with the release rate following zero order. However, this system still releases some drugs in an acidic atmosphere. With a multi-coating system using Eudragit as the outer layer, the release of drugs in an acidic atmosphere can be reduced.154
Size and Mechanism Comparison
Some of the encapsulation forms described in the previous sections vary in size and shape of the system used. This difference will lead to different deliveries and endocytosis mechanisms. The comparison of size and coating system can be seen in Figure 5.
Figure 5 describes that the enteric-coated nanoparticle drug formulations for colorectal cancer system can be in the form of a single drug coating or in the form of a matrix. The single form of coating generally aims to prevent drug aggregation and targeted delivery39,127,153 while the matrix form aims to increase solubility and controlled release.150,154 For anionic charged drugs that reach target cells in the 102 nm size will be uptaken via the clathrin pathway. Whereas those with cationic and neutral charges with a larger size (not to exceed 104 nm) will be uptaken via other channels besides clathrin.141
As enteric-coated polymer, eudragit releases nearly 90% drug in a zero-order pattern at 10 h time at small intestinal pH. Meanwhile, ethylcellulose and cellulose acetate phthalate released 90% of the drug at 20 hours. When compared with these polymers, shellac has a more sensitive response to intestinal pH where drug release reaches 100% at 10 hours.158 However, when compared to natural polymers, eudragit is more reproducible and is not absorbed, so they do not give systemic side effects.159
The Perspective of the Author
In the last decades, researchers have been developing and using nanoparticle systems with controlled drug release profiles. It was possible to elaborate nanoparticles for sustained and delayed drug release, which prolongs release and extends the drug effect, leading to a significant increase of bioavailability.
Chitosan polymer is often used in nanoparticle technology, as studies prove that it shows low toxicity. Besides, it is biodegradable and biocompatible.160
In order to improve the delivery efficiency of oral nanoparticle systems even more, the enteric coating seems to be a promising approach, but every dosage form taken orally has to face the problem of degradation, resulting in reduced oral availability. This can be prevented by enteric coating. So far enteric-coated nanoparticles for various purposes have been developed. For instance, oral delivery of insulin,94,111,161,162 antihypertensive agents,97 anti-glioma therapeutics,163 and cancer therapeutics for colorectal cancer.
As for nanoparticle system in colorectal cancer treatment, Eudragit has been used commonly as an enteric coating. These copolymers are perfectly suitable for colon-specific targeting as their dissolution is pH-depended, which is necessary since there are several milieus of different pH levels throughout the gastrointestinal tract,156 making it a perfect option as an enteric coating of oral nanoparticle systems. In the previously mentioned articles, Eudragit S100 was commonly used taking advantage of the fact that it dissolves above a pH level of 7, which makes it perfectly suitable for colon-specific release.
As a summary, the reviewed articles discussed the enteric coating of the nanoparticles significantly improves the delayed and prolonged drug release in the colon. Also, the sustained drug release profile can be enhanced. Thus, a more localized release at the tumor site could be achieved leading to a significantly enhanced antitumor activity.
Moreover, nanoparticles modified with ligand seem to be a promising attempt to improve specific active colorectal tumor targeting, although they did not show optimal characteristics compared to non-modified nanoparticles. Therefore, more research has to be conducted to optimize these modified nanoparticles, but other than that, combining enteric coating with modified nanoparticles could enhance the colon-specific targeting and release, which is essential for antitumor agents in colorectal cancer therapy.
As for the anticancer activity, in vitro studies should consider the characteristics of enteric coating. Cell toxicity assays should be tested in a medium similar to the colonic fluids instead of acidic cell medium. Only then, studies can be informative and comparable.
Further, more in vivo studies should be taken into consideration that optimal colon-targeted drug release depends on many various factors, which can hardly be simulated fully in vitro.
Conclusion
In recent years the field of nanotechnology in cancer treatment has been expanding rapidly. Nanoparticles used as oral drug delivery systems seem to be one of the most promising approaches in colorectal cancer therapy these days. The development of different formulations and technologies has been carried out to improve colon-specific drug delivery by controlled drug release. The overall research, which has been conducted so far, showed that enteric-coated nanoparticles were able to enhance the controlled drug release. An improved delayed, prolonged, and sustained drug release profile in the colonic area could be confirmed, leading to an enhanced antitumor activity on tumor cells. Enteric-coated nanoparticles showed a great potential to increase the effect of anticancer agents like 5-FU significantly, which could be a big next step in colorectal cancer therapy.
Furthermore, for the future development of drug delivery systems in colorectal cancer therapy not only target pH-stimulated release but also combined with specific targeting of colorectal cancer cells. The interaction between the targeted ligands decorated on the nanoparticle surface and certain receptors that are overexpressed at the diseased site or certain cells is expected to increase the adhesion and internalization of the nanoparticles. This effect will lead to selective drug accumulation at the target site which can increase therapeutic efficacy and reduce side effects.
Acknowledgment
Many thanks to Lisna Meylina for the valuable advice and suggestions in the writing of the manuscript.
Funding
We would like to thanks to Fundamental Research Grant (1827/UN6.3.1/LT/2020), Ministry of Research and Higher Education, Republic of Indonesia and Work From Home Grant, Universitas Padjadjaran (1733/UN6.3.1/LT/2020) that funding of this study.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
2. Siegel RL, Miller KD, Goding Sauer A, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145–164. doi:10.3322/caac.21601
3. Brouwer NPM, Bos ACRK, Lemmens VEPP, et al. An overview of 25 years of incidence, treatment and outcome of colorectal cancer patients. Int J Cancer. 2018;143(11):2758–2766. doi:10.1002/ijc.31785
4. Haggar FA, Boushey RP. Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg. 2009;22(4):191–197. doi:10.1055/s-0029-1242458
5. Häfner MF, Debus J. Radiotherapy for colorectal cancer: current standards and future perspectives. Visc Med. 2016;32(3):172–177. doi:10.1159/000446486
6. Aiello P, Sharghi M, Mansourkhani SM, et al. Medicinal plants in the prevention and treatment of colon cancer. Oxid Med Cell Longev. 2019;2019:1–51. doi:10.1155/2019/2075614
7. Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66(4):683–691. doi:10.1136/gutjnl-2015-310912
8. Mishra J, Drummond J, Quazi SH, et al. Prospective of colon cancer treatments and scope for combinatorial approach to enhanced cancer cell apoptosis. Crit Rev Oncol Hematol. 2013;86(3):232–250. doi:10.1016/j.critrevonc.2012.09.014
9. Bertelsen CA, Neuenschwander AU, Jansen JE, et al. Disease-free survival after complete mesocolic excision compared with conventional colon cancer surgery: a retrospective, population-based study. Lancet Oncol. 2015;16(2):161–168. doi:10.1016/S1470-2045(14)71168-4
10. Angenete E. The importance of surgery in colorectal cancer treatment. Lancet Oncol. 2019;20(1):6–7. doi:10.1016/S1470-2045(18)30679-X
11. Green BL, Marshall HC, Collinson F, et al. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg. 2013;100(1):75–82. doi:10.1002/bjs.8945
12. Terriere L, Holvoet J, Schrijvers D. Colorectal cancer. ESMO Handb Cancer Prev. 2008;1:127–135. doi:10.1038/nrdp.2015.65
13. Tevis SE, Kennedy GD. Postoperative complications: looking forward to a safer future. Clin Colon Rectal Surg. 2016;29(3):246–252. doi:10.1055/s-0036-1584501
14. Climent M, Martin ST. Complications of laparoscopic rectal cancer surgery. Mini-Invasive Surg. 2018;2018. doi:10.20517/2574-1225.2018.62.
15. Chiu -C-C, Lin W-L, Shi H-Y, et al. Comparison of oncologic outcomes in laparoscopic versus open surgery for non-metastatic colorectal cancer: personal experience in a single institution. J Clin Med. 2019;8(6):875. doi:10.3390/jcm8060875
16. Bedirli A, Salman B, Yuksel O. Laparoscopic versus open surgery for colorectal cancer: a retrospective analysis of 163 patients in a single institution. Minim Invasive Surg. 2014;2014:1–6. doi:10.1155/2014/530314
17. Song X-J, Liu Z-L, Zeng R, Ye W, Liu C-W. A meta-analysis of laparoscopic surgery versus conventional open surgery in the treatment of colorectal cancer. Medicine (Baltimore). 2019;98(17):e15347. doi:10.1097/MD.0000000000015347
18. Yang X-F, Pan K. Diagnosis and management of acute complications in patients with colon cancer: bleeding, obstruction, and perforation. Chin J Cancer Res. 2014;26(3):331–340. doi:10.3978/j.issn.1000-9604.2014.06.11
19. Kirchhoff P, Clavien P-A, Hahnloser D. Complications in colorectal surgery: risk factors and preventive strategies. Patient Saf Surg. 2010;4(1):5. doi:10.1186/1754-9493-4-5
20. Beraldo FB, Yusuf SAI, Palma RT, Kharmandayan S, Goncalves JE, Waisberg J. Urinary dysfunction after surgical treatment for rectal cancer. Arq Gastroenterol. 2015;52(3):180–185. doi:10.1590/S0004-28032015000300005
21. Cicchetti A, Avuzzi B, Palorini F, et al. Predicting late fecal incontinence risk after radiation therapy for prostate cancer: new insights from external independent validation. Int J Radiat Oncol. 2018;102(1):127–136. doi:10.1016/j.ijrobp.2018.05.013
22. Birgisson H, Påhlman L, Gunnarsson U, Glimelius B. Late adverse effects of radiation therapy for rectal cancer – a systematic overview. Acta Oncol (Madr). 2007;46(4):504–516. doi:10.1080/02841860701348670
23. Lange MM, van de Velde CJH. Urinary and sexual dysfunction after rectal cancer treatment. Nat Rev Urol. 2011;8(1):51–57. doi:10.1038/nrurol.2010.206
24. Lange MM, den Dulk M, Bossema ER, et al. Risk factors for faecal incontinence after rectal cancer treatment. Br J Surg. 2007;94(10):1278–1284. doi:10.1002/bjs.5819
25. Lange MM, van de Velde CJH. Faecal and urinary incontinence after multimodality treatment of rectal cancer. PLoS Med. 2008;5(10):e202. doi:10.1371/journal.pmed.0050202
26. Kim JH, Jenrow KA, Brown SL. Mechanisms of radiation-induced normal tissue toxicity and implications for future clinical trials. Radiat Oncol J. 2014;32(3):103–115. doi:10.3857/roj.2014.32.3.103
27. Malam Y, Loizidou M, Seifalian AM. Liposomes and nanoparticles: nanosized vehicles for drug delivery in cancer. Trends Pharmacol Sci. 2009;30(11):592–599. doi:10.1016/j.tips.2009.08.004
28. Brigger I, Dubernet C, Couvreur P. Nanoparticles in cancer therapy and diagnosis. Adv Drug Deliv Rev. 2012;64(SUPPL):24–36. doi:10.1016/j.addr.2012.09.006
29. Zhang N, Yin Y, Xu SJ, Chen WS. 5-Fluorouracil: mechanisms of resistance and reversal strategies. Molecules. 2008;13(8):1551–1569. doi:10.3390/molecules13081551
30. Cho K, Wang X, Nie S, Chen Z, Shin DM. Therapeutic nanoparticles for drug delivery in cancer. Clin Cancer Res. 2008;14(5):1310–1316. doi:10.1158/1078-0432.CCR-07-1441
31. Luqmani YA. Mechanisms of drug resistance in cancer chemotherapy. Med Princ Pract. 2005;14(SUPPL. 1):35–48. doi:10.1159/000086183
32. Tummala S, Satish Kumar MN, Prakash A. Formulation and characterization of 5-Fluorouracil enteric coated nanoparticles for sustained and localized release in treating colorectal cancer. Saudi Pharm J. 2015;23(3):308–314. doi:10.1016/j.jsps.2014.11.010
33. Štabuc B. Systemic therapy for colorectal cancer. Arch Oncol. 2003;11(4):255–263. doi:10.2298/AOO0304255S
34. Pérez-Herrero E, Fernández-Medarde A. Advanced targeted therapies in cancer: drug nanocarriers, the future of chemotherapy. Eur J Pharm Biopharm. 2015;93:52–79. doi:10.1016/j.ejpb.2015.03.018
35. Edwards MS, Chadda SD, Zhao Z, Barber BL, Sykes DP. A systematic review of treatment guidelines for metastatic colorectal cancer. Color Dis. 2012;14(2):31–47. doi:10.1111/j.1463-1318.2011.02765.x
36. Tol J, Koopman M, Cats A, et al. Chemotherapy, bevacizumab, and cetuximab in metastatic colorectal cancer. N Engl J Med. 2009.
37. Lee G, Joung JY, Cho JH, Son CG, Lee N. Overcoming P-glycoprotein-mediated multidrug resistance in colorectal cancer: potential reversal agents among herbal medicines. Evid Based Compl Altern Med. 2018;2018:1–9. doi:10.1155/2018/3412074
38. Bahrami B, Hojjat-Farsangi M, Mohammadi H, et al. Nanoparticles and targeted drug delivery in cancer therapy. Immunol Lett. 2017;190:
39. Jain A, Jain SK, Ganesh N, Barve J, Beg AM. Design and development of ligand-appended polysaccharidic nanoparticles for the delivery of oxaliplatin in colorectal cancer. Nanomedicine Nanotechnology, Biol Med. 2010;6(1):179–190. doi:10.1016/J.NANO.2009.03.002
40. Ruoslahti E, Bhatia SN, Sailor MJ. Targeting of drugs and nanoparticles to tumors. J Cell Biol. 2010;188(6):759–768. doi:10.1083/jcb.200910104
41. Dadwal A, Baldi A, Kumar Narang R. Nanoparticles as carriers for drug delivery in cancer. Artif Cells Nanomed Biotechnol. 2018;46(sup2):295–305. doi:10.1080/21691401.2018.1457039
42. Sykes EA, Chen J, Zheng G, Chan WCWW. Investigating the impact of nanoparticle size on active and passive tumor targeting efficiency. ACS Nano. 2014;8(6):5696–5706. doi:10.1021/nn500299p
43. Yu X, Trase I, Ren M, Duval K, Guo X, Chen Z. Design of nanoparticle-based carriers for targeted drug delivery. J Nanomater. 2016;2016:1–15. doi:10.1155/2016/1087250
44. Gonda A, Zhao N, Shah JV, et al. Engineering tumor-targeting nanoparticles as vehicles for precision nanomedicine. Med One. 2019;4. doi:10.20900/mo.20190021
45. Bazak R, Houri M, El Achy S, et al. Cancer active targeting by nanoparticles: a comprehensive review of literature. J Cancer Res Clin Oncol. 2016;141(5):769–784. doi:10.1007/s00432-014-1767-3.Cancer
46. Amidon S, Brown JE, Dave VS. Colon-targeted oral drug delivery systems: design trends and approaches. AAPS Pharm Sci Tech. 2015;16(4):731–741. doi:10.1208/s12249-015-0350-9
47. Pridgen EM, Alexis F, Farokhzad OC. Polymeric nanoparticle technologies for oral drug delivery. Clin Gastroenterol Hepatol. 2014;12(10):1605–1610. doi:10.1016/j.cgh.2014.06.018
48. Hussan SD. A review on recent advances of enteric coating. IOSR J Pharm. 2012;2(6):05–11. doi:10.9790/3013-2610511
49. Leopold CS. Coated dosage forms for colon-specific drug delivery. Pharm Sci Technol Today. 1999;2(5):197–204. doi:10.1016/S1461-5347(99)00151-0
50. Hao S, Wang B, Wang Y, Xu Y. Enteric-coated sustained-release nanoparticles by coaxial electrospray: preparation, characterization, and in vitro evaluation. J Nanoparticle Res. 2014;16(2):2204. doi:10.1007/s11051-013-2204-2
51. Li C, Zhou K, Chen D, et al. Solid lipid nanoparticles with enteric coating for improving stability, palatability, and oral bioavailability of enrofloxacin. Int J Nanomedicine. 2019;14:1619–1631. doi:10.2147/IJN.S183479
52. Bhadra S, Prajapati A, Bhadra D. Development of pH sensitive polymeric nanoparticles of erythromycin stearate. J Pharm Bioallied Sci. 2016;8(2):135. doi:10.4103/0975-7406.171691
53. Shahdadi Sardo H, Saremnejad F, Bagheri S, Akhgari A, Afrasiabi Garekani H, Sadeghi F. A review on 5-aminosalicylic acid colon-targeted oral drug delivery systems. Int J Pharm. 2019;558:367–379. doi:10.1016/j.ijpharm.2019.01.022
54. Khotimchenko M. Pectin polymers for colon-targeted antitumor drug delivery. Int J Biol Macromol. 2020;158:1110–1124. doi:10.1016/j.ijbiomac.2020.05.002
55. Lang X, Wang T, Sun M, Chen X, Liu Y. Advances and applications of chitosan-based nanomaterials as oral delivery carriers: a review. Int J Biol Macromol. 2020;154:433–445. doi:10.1016/j.ijbiomac.2020.03.148
56. Marley RA, Nan H. Epidemiology of colorectal cancer. Int J Mol Epidemiol Genet. 2016;96(2):105–114. doi:10.2169/naika.96.200
57. Siegel R, DeSantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin. 2014;64(2):104–117. doi:10.3322/caac.21220
58. Naeem M, Awan UA, Subhan F, et al. Advances in colon-targeted nano-drug delivery systems: challenges and solutions. Arch Pharm Res. 2020;43(1):153–169. doi:10.1007/s12272-020-01219-0
59. Dong Y, Zhou J, Zhu Y, et al. Abdominal obesity and colorectal cancer risk: systematic review and meta-analysis of prospective studies. Biosci Rep. 2017;37(6):1–12. doi:10.1042/BSR20170945
60. Ma Y, Yang Y, Wang F, et al. Obesity and risk of colorectal cancer: a systematic review of prospective studies. PLoS One. 2013;8:1. doi:10.1371/journal.pone.0053916
61. Tsilidis KK, Kasimis JC, Lopez DS, Ntzani EE, Ioannidis JPA. Type 2 diabetes and cancer: umbrella review of meta-analyses of observational studies. BMJ. 2015;350(January):1–11. doi:10.1136/bmj.g7607
62. You X, Kang Y, Hollett G, et al. Polymeric nanoparticles for colon cancer therapy: overview and perspectives. J Mater Chem B. 2016;4(48):7779–7792. doi:10.1039/c6tb01925k
63. Jeon G, Ko YT. Enhanced photodynamic therapy via photosensitizer-loaded nanoparticles for cancer treatment. J Pharm Investig. 2019;49(1). doi:10.1007/s40005-017-0363-3
64. Wilczewska AZ, Niemirowicz K, Markiewicz KH, Car H. Nanoparticles as drug delivery systems. Pharmacol Rep. 2012;64(5):1020–1037. doi:10.1016/S1734-1140(12)70901-5
65. Tiwari JN, Tiwari RN, Kim KS. Zero-dimensional, one-dimensional, two-dimensional and three-dimensional nanostructured materials for advanced electrochemical energy devices. Prog Mater Sci. 2012;57(4):724–803. doi:10.1016/j.pmatsci.2011.08.003
66. Li Z, Tan S, Li S, Shen Q, Wang K. Cancer drug delivery in the nano era: an overview and perspectives (Review). Oncol Rep. 2017;38(2):611–624. doi:10.3892/or.2017.5718
67. Behzadi S, Serpooshan V, Tao W, et al. Cellular uptake of nanoparticles: journey inside the cell. Chem Soc Rev. 2017;46(14):4218–4244. doi:10.1039/C6CS00636A
68. Foroozandeh P, Aziz AA. Insight into cellular uptake and intracellular trafficking of nanoparticles. Nanoscale Res Lett. 2018;13(1):339. doi:10.1186/s11671-018-2728-6
69. Gou M. Promising application of nanotechnology in anticancer drug delivery. Drug Des Open Access. 2013;02:02. doi:10.4172/2169-0138.1000e117
70. Kumar M, Sharma HK. Targeted nanotechnology for anticancer drug delivery: current issue and challenge. J Drug Deliv Ther. 2018;8(5):23–27. doi:10.22270/jddt.v8i5.1882
71. Rodzinski A, Guduru R, Liang P, et al. Targeted and controlled anticancer drug delivery and release with magnetoelectric nanoparticles. Sci Rep. 2016;6(1):20867. doi:10.1038/srep20867
72. Sutradhar KB, Amin ML. Nanotechnology in cancer drug delivery and selective targeting. ISRN Nanotechnol. 2014;2014:1–12. doi:10.1155/2014/939378
73. Xin Y, Yin M, Zhao L, Meng F, Luo L. Recent progress on nanoparticle-based drug delivery systems for cancer therapy. Cancer Biol Med. 2017;14(3):228. doi:10.20892/j.issn.2095-3941.2017.0052
74. Safhi MM, Sivakumar SM, Jabeen A, et al. Nanoparticle system for anticancer drug delivery: targeting to overcome multidrug resistance. In: Grumezesc Multifunctional Systems for Combined Delivery, Biosensing and Diagnostics. Elsevier; 2017:159–169. doi:10.1016/B978-0-323-52725-5.00008-3
75. Liu J, Huang Y, Kumar A, et al. PH-Sensitive nano-systems for drug delivery in cancer therapy. Biotechnol Adv. 2014;32(4):693–710. doi:10.1016/j.biotechadv.2013.11.009
76. Khatoon N, Alam H, Khan A, Raza K, Sardar M. Ampicillin silver nanoformulations against multidrug resistant bacteria. Sci Rep. 2019;9(1):6848. doi:10.1038/s41598-019-43309-0
77. Yang J, Zhang H, Chen B. Application of nanoparticles to reverse multi-drug resistance in cancer. Nanotechnol Rev. 2016;5:5. doi:10.1515/ntrev-2016-0023
78. AlMatar M, Makky EA, Var I, Koksal F. The role of nanoparticles in the inhibition of multidrug-resistant bacteria and biofilms. Curr Drug Deliv. 2018;15(4):470–484. doi:10.2174/1567201815666171207163504
79. Chand Dakal T, Pal M. Nanotechnology for combating multi-drug resistance: a next generation antimicrobial therapy. J Drug Metab Toxicol. 2017;08:02. doi:10.4172/2157-7609-C1-009
80. Kwon S-I, Kyung K-H, Park J-Y, et al. Uniform anti-reflective films fabricated by layer-by-layer ultrasonic spray method. Colloids Surf A Physicochem Eng ASP. 2019;580((August):123785):123785. doi:10.1016/j.colsurfa.2019.123785
81. Kotelevets L, Chastre E, Desmaële D, Couvreur P. Nanotechnologies for the treatment of colon cancer: from old drugs to new hope. Int J Pharm. 2016;514(1):24–40. doi:10.1016/j.ijpharm.2016.06.005
82. Bodmeier R, Chen H, Paeratakul O, Novel A. Approach to the oral delivery of micro- or nanoparticles. Pharm Res an off J Am Assoc Pharm Sci. 1989;6(5):413–417. doi:10.1023/A:1015987516796
83. Fattal E, Youssef M, Couvreur P, Andremont A. Treatment of experimental salmonellosis in mice with ampicillin-bound nanoparticles. Antimicrob Agents Chemother. 1989;33(9):1540–1543. doi:10.1128/AAC.33.9.1540
84. Collnot EM, Ali H, Lehr CM. Nano- and microparticulate drug carriers for targeting of the inflamed intestinal mucosa. J Control Release. 2012;161(2):235–246. doi:10.1016/j.jconrel.2012.01.028
85. Koziolek M, Grimm M, Becker D, et al. Investigation of pH and temperature profiles in the GI tract of fasted human subjects using the IntelliCap® system. J Pharm Sci. 2015;104(9):2855–2863. doi:10.1002/jps.24274
86. Zhang S, Langer R, Traverso G. Nanoparticulate drug delivery systems targeting inflammation for treatment of inflammatory bowel disease. Nano Today. 2019;176(1):82–96. doi:10.1016/j.physbeh.2017.03.040
87. Al-Gousous J, Tsume Y, Fu M, Salem II, Langguth P. Unpredictable performance of pH-dependent coatings accentuates the need for improved predictive in vitro test systems. Mol Pharm. 2017;14(12):4209–4219. doi:10.1021/acs.molpharmaceut.6b00877
88. Tran TT-D, Tran PH-L, Phan ML-N, Van TV. Colon specific delivery of fucoidan by incorporation of acidifier in enteric coating polymer. Int J Pharm Biosci Technol. 2013;9(13):14.
89. Khobragade DS, Trambak Patil A, Shamrao Khobragade D, et al. Development and evaluation of a hot-melt coating technique for enteric coating. Brazilian J Pharm Sci. 2012;48:1.
90. Li P, Hao J, Li H, Guan H, Li C. Development of an enteric nanoparticle of marine sulfated polysaccharide propylene glycol alginate sodium sulfate for oral administration: formulation design, pharmacokinetics and efficacy. J Pharm Pharmacol. 2018;70(6):740–748. doi:10.1111/jphp.12902
91. Thiyagarajan V, Lin S-X, Lee C-H, Weng C-F. A focal adhesion kinase inhibitor 16-hydroxy-cleroda-3,13-dien-16,15-olide incorporated into enteric-coated nanoparticles for controlled anti-glioma drug delivery. Colloids Surfaces B Biointerfaces. 2016;141:120–131. doi:10.1016/j.colsurfb.2016.01.038
92. Sampathkumar K, Riyajan S, Tan CK, Demokritou P, Chudapongse N, Loo SCJ. Small-intestine-specific delivery of antidiabetic extracts from withania coagulans using polysaccharide-based enteric-coated nanoparticles. ACS Omega. 2019;4(7):12049–12057. doi:10.1021/acsomega.9b00823
93. He H, Zhang X, Sheng Y. Enteric-coated capsule containing β-galactosidase-loaded polylactic acid nanocapsules: enzyme stability and milk lactose hydrolysis under simulated gastrointestinal conditions. J Dairy Res. 2014;81(4):479–484. doi:10.1017/S0022029914000491
94. Yu F, Li Y, Liu CS, et al. Enteric-coated capsules filled with mono-disperse micro-particles containing PLGA-lipid-PEG nanoparticles for oral delivery of insulin. Int J Pharm. 2015;484(1–2):181–191. doi:10.1016/j.ijpharm.2015.02.055
95. Fan W, Xia D, Zhu Q, et al. Functional nanoparticles exploit the bile acid pathway to overcome multiple barriers of the intestinal epithelium for oral insulin delivery. Biomaterials. 2018;151:13–23. doi:10.1016/j.biomaterials.2017.10.022
96. Nguyen DN, Palangetic L, Clasen C, Van den Mooter G. One-step production of darunavir solid dispersion nanoparticles coated with enteric polymers using electrospraying. J Pharm Pharmacol. 2016;68(5):625–633. doi:10.1111/jphp.12459
97. Sun H, Liu D, Li Y, Tang X, Cong Y. Preparation and in vitro/in vivo characterization of enteric-coated nanoparticles loaded with the antihypertensive peptide VLPVPR. Int J Nanomedicine. 2014;9(1):1709–1716. doi:10.2147/IJN.S56092
98. Sladek S, McCartney F, Eskander M, et al. An enteric-coated polyelectrolyte nanocomplex delivers insulin in rat intestinal instillations when combined with a permeation enhancer. Pharmaceutics. 2020;12(3):259. doi:10.3390/pharmaceutics12030259
99. Xu B, Zhang W, Chen Y, Xu Y, Wang B, Zong L. Eudragit® L100-coated mannosylated chitosan nanoparticles for oral protein vaccine delivery. Int J Biol Macromol. 2018;113:534–542. doi:10.1016/j.ijbiomac.2018.02.016
100. Chaturvedi K, Ganguly K, Kulkarni AR, et al. Oral insulin delivery using deoxycholic acid conjugated PEGylated polyhydroxybutyrate co-polymeric nanoparticles. Nanomedicine. 2015;10(10):1569–1583. doi:10.2217/nnm.15.36
101. He Z, Liu Z, Tian H, et al. Scalable production of core–shell nanoparticles by flash nanocomplexation to enhance mucosal transport for oral delivery of insulin. Nanoscale. 2018;10(7):3307–3319. doi:10.1039/C7NR08047F
102. Ray L, Karthik R, Srivastava V, et al. Efficient antileishmanial activity of amphotericin B and piperine entrapped in enteric coated guar gum nanoparticles. Drug Deliv Transl Res. 2020. doi:10.1007/s13346-020-00712-9
103. Sinhmar GK, Shah NN, Chokshi NV, Khatri HN, Patel MM. Process, optimization, and characterization of budesonide-loaded nanostructured lipid carriers for the treatment of inflammatory bowel disease. Drug Dev Ind Pharm. 2018;44(7):1078–1089. doi:10.1080/03639045.2018.1434194
104. Kankala RK, Kuthati Y, Sie H-W, et al. Multi-laminated metal hydroxide nanocontainers for oral-specific delivery for bioavailability improvement and treatment of inflammatory paw edema in mice. J Colloid Interface Sci. 2015;458:217–228. doi:10.1016/j.jcis.2015.07.044
105. Tayel SA, El-Nabarawi MA, Tadros MI, Abd-Elsalam WH. Duodenum-triggered delivery of pravastatin sodium: II. Design, appraisal and pharmacokinetic assessments of enteric surface-decorated nanocubosomal dispersions. Drug Deliv. 2016;23(9):3266–3278. doi:10.3109/10717544.2016.1172367
106. Jog R, Unachukwu K, Burgess DJ. Formulation design space for stable, pH sensitive crystalline nifedipine nanoparticles. Int J Pharm. 2016;514(1):81–92. doi:10.1016/j.ijpharm.2016.08.039
107. Sun L, Liu Z, Tian H, et al. Scalable manufacturing of enteric encapsulation systems for site-specific oral insulin delivery. Biomacromolecules. 2019;20(1):528–538. doi:10.1021/acs.biomac.8b01530
108. González-Alvarez M, Coll C, Gonzalez-Alvarez I, et al. Gated mesoporous silica nanocarriers for a “two-step” targeted system to colonic tissue. Mol Pharm. 2017;14(12):4442–4453. doi:10.1021/acs.molpharmaceut.7b00565
109. Shi Y, Li K, Tian B, et al. Oral delivery of human growth hormone: preparation, characterization, and pharmacokinetics. J Biomater Appl. 2017;31(6):851–858. doi:10.1177/0885328216674347
110. Bendas ER, Abdelbary AA. Instantaneous enteric nano-encapsulation of omeprazole: pharmaceutical and pharmacological evaluation. Int J Pharm. 2014;468(1–2):97–104. doi:10.1016/j.ijpharm.2014.04.030
111. Wu ZM, Zhou L, Guo XD, et al. HP55-coated capsule containing PLGA/RS nanoparticles for oral delivery of insulin. Int J Pharm. 2012;425(1–2):1–8. doi:10.1016/j.ijpharm.2011.12.055
112. Müller C, Perera G, König V, Bernkop-Schnürch A. Development and in vivo evaluation of papain-functionalized nanoparticles. Eur J Pharm Biopharm. 2014;87(1):125–131. doi:10.1016/j.ejpb.2013.12.012
113. Salvioni L, Fiandra L, Del Curto MD, et al. Oral delivery of insulin via polyethylene imine-based nanoparticles for colonic release allows glycemic control in diabetic rats. Pharmacol Res. 2016;110:122–130. doi:10.1016/j.phrs.2016.05.016
114. Luo S, Hao J, Gao Y, Liu D, Cai Q, Yang X. Pore size effect on adsorption and release of metoprolol tartrate in mesoporous silica: experimental and molecular simulation studies. Mater Sci Eng C. 2019;100:789–797. doi:10.1016/j.msec.2019.03.050
115. Alai M, Lin WJ. Novel lansoprazole-loaded nanoparticles for the treatment of gastric acid secretion-related ulcers: in vitro and in vivo pharmacokinetic pharmacodynamic evaluation. AAPS J. 2014;16(3):361–372. doi:10.1208/s12248-014-9564-0
116. Nguyen DN, Clasen C, Van den Mooter G. Encapsulating darunavir nanocrystals within Eudragit L100 using coaxial electrospraying. Eur J Pharm Biopharm. 2017;113:50–59. doi:10.1016/j.ejpb.2016.12.002
117. Kumar PV, Maki MAA, Wei YS, et al. Rabbit as an animal model for pharmacokinetics studies of enteric capsule contains recombinant human keratinocyte growth factor loaded chitosan nanoparticles. Curr Clin Pharmacol. 2019;14(2):132–140. doi:10.2174/1574884714666181120103907
118. Eskandari S, Varamini P, Toth I. Formulation, characterization and permeability study of nano particles of lipo-endomorphin-1 for oral delivery. J Liposome Res. 2013;23(4):311–317. doi:10.3109/08982104.2013.805339
119. Shah MK, Madan P, Lin S. Preparation, in vitro evaluation and statistical optimization of carvedilol-loaded solid lipid nanoparticles for lymphatic absorption via oral administration. Pharm Dev Technol. 2014;19(4):475–485. doi:10.3109/10837450.2013.795169
120. Nguyen H-N, Wey S-P, Juang J-H, et al. The glucose-lowering potential of exendin-4 orally delivered via a pH-sensitive nanoparticle vehicle and effects on subsequent insulin secretion in vivo. Biomaterials. 2011;32(10):2673–2682. doi:10.1016/j.biomaterials.2010.12.044
121. Chen K, Chang HHR, Shalviri A, et al. Investigation of a new pH-responsive nanoparticulate pore former for controlled release enteric coating with improved processability and stability. Eur J Pharm Biopharm. 2017;120:116–125. doi:10.1016/j.ejpb.2017.08.014
122. Roy U, Ding H, Pilakka Kanthikeel S, et al. Preparation and characterization of anti-HIV nanodrug targeted to microfold cell of gut-associated lymphoid tissue. Int J Nanomedicine. 2015:5819. doi:10.2147/IJN.S68348.
123. Anwer MK, Al-Shdefat R, Ezzeldin E, Alshahrani SM, Alshetaili AS, Iqbal M. Preparation, evaluation and bioavailability studies of eudragit coated PLGA nanoparticles for sustained release of eluxadoline for the treatment of irritable bowel syndrome. Front Pharmacol. 2017;8. doi:10.3389/fphar.2017.00844.
124. Biswas S, Chattopadhyay M, Sen KK, Saha MK. Development and characterization of alginate coated low molecular weight chitosan nanoparticles as new carriers for oral vaccine delivery in mice. Carbohydr Polym. 2015;121:403–410. doi:10.1016/j.carbpol.2014.12.044
125. Zhao X, Shan C, Zu Y, et al. Preparation, characterization, and evaluation in vivo of Ins-SiO2-HP55 (insulin-loaded silica coating HP55) for oral delivery of insulin. Int J Pharm. 2013;454(1):278–284. doi:10.1016/j.ijpharm.2013.06.051
126. Su F-Y, Lin K-J, Sonaje K, et al. Protease inhibition and absorption enhancement by functional nanoparticles for effective oral insulin delivery. Biomaterials. 2012;33(9):2801–2811. doi:10.1016/j.biomaterials.2011.12.038
127. Li P, Yang Z, Wang Y, et al. Microencapsulation of coupled folate and chitosan nanoparticles for targeted delivery of combination drugs to colon. J Microencapsul. 2015;32(1):40–45. doi:10.3109/02652048.2014.944947
128. Nassar T, Attili-Qadri S, Harush-Frenkel O, et al. High plasma levels and effective lymphatic uptake of docetaxel in an orally available nanotransporter formulation. Cancer Res. 2011;71(8):3018–3028. doi:10.1158/0008-5472.CAN-10-3118
129. Mahjub R, Najafabadi FK, Dehkhodaei N, et al. Eudragit L-100 capsules/aromatize and quaternerize chitosan for insulin nanoparticle oral delivery on toxic oxidative stress in rat liver and kidney. Pharm Nanotechnol. 2020;8. doi:10.2174/2211738508666200628033442
130. Yus C, Irusta S, Sebastian V, Arruebo M. Controlling particle size and release kinetics in the sustained delivery of oral antibiotics using pH-independent mucoadhesive polymers. Mol Pharm. 2020;
131. Zhou K, Yan Y, Chen D, et al. Solid lipid nanoparticles for duodenum targeted oral delivery of tilmicosin. Pharmaceutics. 2020;12(8):731. doi:10.3390/pharmaceutics12080731
132. Sahu KK, Kaurav M, Pandey RS. Chylomicron mimicking solid lipid nanoemulsions encapsulated enteric minicapsules targeted to colon for immunization against hepatitis B. Int Immunopharmacol. 2019;66:317–329. doi:10.1016/j.intimp.2018.11.041
133. Tummala S, Kuppusamy G, Satish Kumar MN, Praveen TK, Wadhwani A. 5-Fluorouracil enteric-coated nanoparticles for improved apoptotic activity and therapeutic index in treating colorectal cancer. Drug Deliv. 2016;23(8):2902–2910. doi:10.3109/10717544.2015.1116026
134. Hosny KM. Alendronate sodium as enteric coated solid lipid nanoparticles; preparation, optimization, and in vivo evaluation to enhance its oral bioavailability. Santos HA, ed. PLoS One. 2016;11(5):e0154926. doi:10.1371/journal.pone.0154926
135. Valat MT. Mechanistic study of NVP-CGM097: A potent, selective and species specific inhibitor of p53-Mdm2. Drug Des Open Access. 2015;04:02. doi:10.4172/2169-0138.S1.008
136. Amini-Fazl MS, Mohammadi R, Kheiri K. 5‑Fluorouracil loaded chitosan/polyacrylic acid/Fe 3 O 4 magnetic nanocomposite hydrogel as a potential anticancer drug delivery system. Int J Biol Macromol. 2019;132:506–513. doi:10.1016/j.ijbiomac.2019.04.005
137. Choi JS, Cao J, Naeem M, et al. Size-controlled biodegradable nanoparticles: preparation and size-dependent cellular uptake and tumor cell growth inhibition. Colloids Surfaces B Biointerfaces. 2014;122:545–551. doi:10.1016/j.colsurfb.2014.07.030
138. Choi YH, Han HK. Nanomedicines: current status and future perspectives in aspect of drug delivery and pharmacokinetics. J Pharm Investig. 2018;48(1):43–60. doi:10.1007/s40005-017-0370-4
139. Banerjee A, Qi J, Gogoi R, Wong J, Mitragotri S. Role of nanoparticle size, shape and surface chemistry in oral drug delivery. J Control Release. 2016;238:176–185. doi:10.1016/j.jconrel.2016.07.051
140. Xiao B, Si X, Han M, Viennois E, Zhang M, Merlin D. Codelivery of camptothecin and curcumin by cationic polymeric nanoparticles for synergistic colon cancer combination chemotherapy. J Mater Chem B. 2015;3:7724–7733. doi:10.1039/c5tb01245g
141. Akinc A, Battaglia G. Exploiting endocytosis for nanomedicines. Cold Spring Harb Perspect Biol. 2013;5(11):a016980–a016980. doi:10.1101/cshperspect.a016980
142. Chen S, Guo F, Deng T, et al. Eudragit S100-coated chitosan nanoparticles co-loading tat for enhanced oral colon absorption of insulin. AAPS Pharm Sci Tech. 2017;18(4):1277–1287. doi:10.1208/s12249-016-0594-z
143. Karn PR, Vanić Z, Pepić I, Škalko-Basnet N. Mucoadhesive liposomal delivery systems: the choice of coating material. Drug Dev Ind Pharm. 2011;37(4):482–488. doi:10.3109/03639045.2010.523425
144. Nikam V, Kotade K, Gaware V, et al. Eudragit a versatile polymer: a review. Pharmacologyonline. 2011;1:152–164.
145. Sun L, Chen Y, Zhou Y, et al. Preparation of 5-fluorouracil-loaded chitosan nanoparticles and study of the sustained release in vitro and in vivo. Asian J Pharm Sci. 2017;12(5):418–423. doi:10.1016/J.AJPS.2017.04.002
146. Khatik R, Mishra R, Verma A, et al. Colon-specific delivery of curcumin by exploiting Eudragit-decorated chitosan nanoparticles in vitro and in vivo. J Nanoparticle Res. 2013;15:9. doi:10.1007/s11051-013-1893-x
147. Li CF, Li YC, Chen LB, Wang Y, Sun LB. Doxorubicin-loaded Eudragit-coated chitosan nanoparticles in the treatment of colon cancers. J Nanosci Nanotechnol. 2016;16(7):6773–6780. doi:10.1166/jnn.2016.11374
148. Jain A, Jain S, Jain R, Kohli DV. Coated chitosan nanoparticles encapsulating caspase 3 activator for effective treatment of colorectral cancer. Drug Deliv Transl Res. 2015;5(6):596–610. doi:10.1007/s13346-015-0255-x
149. Subudhi MB, Jain A, Jain A, et al. Eudragit S100 coated citrus pectin nanoparticles for colon targeting of 5-fluorouracil. Materials (Basel). 2015;8(3):832–849. doi:10.3390/ma8030832
150. Ma Y, Fuchs AV, Boase NRB, Rolfe BE, Coombes AGA, Thurecht KJ. The in vivo fate of nanoparticles and nanoparticle-loaded microcapsules after oral administration in mice: evaluation of their potential for colon-specific delivery. Eur J Pharm Biopharm. 2015;94:393–403. doi:10.1016/j.ejpb.2015.06.014
151. Kanthamneni N, Chaudhary A, Wang J, Phabhu S. Nanoparticulate delivery of novel drug combination regimens for the chemoprevention of colon cancer. Int J Oncol. 2010;37:177–185. doi:10.3892/ijo
152. Ma Y, Coombes AGA. Designing colon-specific delivery systems for anticancer drug-loaded nanoparticles: an evaluation of alginate carriers. J Biomed Mater Res. 2014;102(9):3167–3176. doi:10.1002/jbm.a.34988
153. Rajpoot K, Jain SK. Oral delivery of pH-responsive alginate microbeads incorporating folic acid-grafted solid lipid nanoparticles exhibits enhanced targeting effect against colorectal cancer: a dual-targeted approach. Int J Biol Macromol. 2020;151:830–844. doi:10.1016/j.ijbiomac.2020.02.132
154. Cerchiara T, Bigucci F, Corace G, Zecchi V, Luppi B. Eudragit-coated albumin nanospheres carrying inclusion complexes for oral administration of indomethacin. J Incl Phenom Macrocycl Chem. 2011;71(1–2):129–136. doi:10.1007/s10847-010-9916-z
155. Jain A, Jain SK. Optimization of chitosan nanoparticles for colon tumors using experimental design methodology. Artif Cells Nanomedicine Biotechnol. 2016;44(8):1917–1926. doi:10.3109/21691401.2015.1111236
156. Thakral S, Thakral NK, Majumdar DK. Eudragit®: a technology evaluation. Expert Opin Drug Deliv. 2013;10(1):131–149. doi:10.1517/17425247.2013.736962
157. Nassar T, Attili-Qadri S, Harush-Frenkel O, et al. High plasma levels and effective lymphatic uptake of docetaxel in an orally available nanotransporter formulation. Cancer Res. 2011;71(8):3018–3028. doi:10.1158/0008-5472.CAN-10-3118
158. Sinha VR, Kumria R. Coating polymers for colon specific drug delivery: a comparative in vitro evaluation. Acta Pharm. 2003;53(1):41–47.
159. Thakral S, Thakral NK, Majumdar DK. Eudragit®: a technology evaluation. Expert Opin Drug Deliv. 2013;10(1):131–149. doi:10.1517/17425247.2013.736962
160. Mohammed MA, Syeda JTM, Wasan KM, Wasan EK. An overview of chitosan nanoparticles and its application in non-parenteral drug delivery. Pharmaceutics. 2017;9:4. doi:10.3390/pharmaceutics9040053
161. Sonaje K, Chen YJ, Chen HL, et al. Enteric-coated capsules filled with freeze-dried chitosan/poly(γ-glutamic acid) nanoparticles for oral insulin delivery. Biomaterials. 2010;31(12):3384–3394. doi:10.1016/j.biomaterials.2010.01.042
162. Alai MS, Lin WJ, Pingale SS. Application of polymeric nanoparticles and micelles in insulin oral delivery. J Food Drug Anal. 2015;23(3):351–358. doi:10.1016/j.jfda.2015.01.007
163. Thiyagarajan V, Lin SX, Lee CH, Weng CF. A focal adhesion kinase inhibitor 16-hydroxy-cleroda-3,13-dien-16,15-olide incorporated into enteric-coated nanoparticles for controlled anti-glioma drug delivery. Colloids Surfaces B Biointerfaces. 2016;141:120–131. doi:10.1016/j.colsurfb.2016.01.038
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

