Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
Enlightening chronic obstructive pulmonary disease through patients’ and caregivers’ narratives
Authors Gatti V, Banfi P , Centanni S, D'Antonio S, Giustini S, Piraino A , Zibellini M, Marini MG
Received 25 April 2018
Accepted for publication 5 August 2018
Published 5 October 2018 Volume 2018:13 Pages 3095—3105
DOI https://doi.org/10.2147/COPD.S172214
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Valeria Gatti,1 Paolo Banfi,2 Stefano Centanni,3 Salvatore D’Antonio,4 Saffi Giustini,5 Alessio Piraino,6 Marco Zibellini,1 Maria Giulia Marini1
1Health Care Area, Fondazione ISTUD, Milan, Italy; 2Fondazione Don Carlo Gnocchi IRCCS, Milan, Italy; 3Respiratory Unit, ASST San Paolo e San Carlo, Department of Health Sciences, University of Milan, Milan, Italy; 4Italian Patient’s Association “BPCO ONLUS”, Rome, Italy; 5Italian General Practitioners’ Association “SIMG”, Florence, Local Health Unit of Montale, Pistoia, Italy; 6Chiesi Farmaceutici S.p.A, Parma, Italy
Purpose: The primary aim of this research was to raise awareness for COPD through real narratives of patients, caregivers, and pulmonologists. The second objective includes providing clinicians new means of caring for and treating patients with COPD.
Methods: Using narrative medicine, testimonies from patients, their caregivers, and clinicians were collected through an online questionnaire enriched by a narrative plot. Narrations were analyzed throughout descriptive statistics and an elaboration of recurring words and expressions.
Results: Throughout the project, 350 narratives were collected from 235 patients, 55 caregivers, and 60 physicians. Though a generally neutral reaction had been observed upon diagnosis, COPD had been found to have a high impact on the patients’ and caregivers’ lives. Metaphors utilized by patients and caregivers were suggestive of fear and panic unlike those utilized by clinicians who usually had a more technical approach. Smoking was a significant concern for not only patients and caregivers but also clinicians.
Conclusion: Physicians are therefore challenged to find new ways of communicating COPD to raise awareness on this pathology and encourage corrective habits. An important social objective should be the implementation of a health system that is able to optimize patients’ and caregivers’ lives.
Keywords: COPD, quality of life, narrative medicine, communication
Introduction
Disease characteristics and risk factors
COPD is defined as a “common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities”.1
The Italian document on the clinical and integrated management of COPD2 instead defines COPD as a pathological condition resulting from different diseases, such as chronic bronchitis, small airways disease, and pulmonary emphysema. Such a definition seems to be more adherent to pathophysiological mechanisms and different clinical symptoms of this syndrome. Although COPD is currently the fourth leading cause of death worldwide,3 with an estimated prevalence of 2.83% in Italy,4 its incidence has been increasing with experts estimating that it would become the third leading cause of death by 2030.
Such a prediction can be attributed to the aging population and low awareness for the disease and its risk factors.5 Considering that the primary symptoms of COPD include breathlessness and coughing, its onset is often misinterpreted. Patients usually associate these symptoms with aging or consider them a natural consequence of smoking, thereby delaying the diagnosis,6 lowering adherence to therapy,7 and increasing the difficulty of smoking cessation,8 all of which contribute to increased COPD burden.
The main risk factor for COPD is tobacco smoking9 wherein smokers are 3–5 times more likely to develop COPD than non-smokers.10 Other risk factors include genetics or other conditions. Accordingly, the best known genetic factor is the deficiency of the serine protease α1 antitrypsin,11 while secondary environmental factors are occupational exposure, outdoor and indoor pollutants, and decreased lung function due to aging or previous pathologies like infections or asthma.12
Although COPD can be adequately controlled through therapy, adherence to treatment has been less than 50% in Italy, Europe, and the US with detrimental effects on patients’ quality of life and illness progression.13–15 Progression to severe COPD significantly impacts quality of life considering that patients are no longer able to walk as fast as before, maintain a regular sleep pattern, and carry weight, thereby limiting their activities.16,17 Informal caregivers’ quality of life can also be affected in the form of health, leisure/social, and professional problems resulting from caregiving activities.18
Narrative medicine
The practice of narrative medicine has been defined as that “circumscribed between the physician and the patient, from the collection of information on events before the disease, to how it has been revealed, focusing on psychological, social, and ontological implications”.19 Narrative medicine, through collection and analysis of narratives written by the many stakeholders involved, including patients, health and social providers, and family members,20 provides insight and understanding on how different subjects live with the illness. This generates a better view regarding the many facets involved in the care pathway.21 Narrative medicine can also be a powerful tool for augmenting information obtained from questionnaires given that writing about illness experiences and context of life provides meaning to statistics.22 Many physicians have started to experiment on narrative medicine, understanding the strength of this approach either in decreasing patients’ and professionals’ anxiety and insecurities or revealing gaps in disease treatment, patient support, and care.23
Considering the current health care system, narrative medicine can be used as a complementary tool to improve efficacy and efficiency from an organizational point of view.24
Study objectives
The aim of this research was to raise awareness for COPD through authentic narratives of patients, caregivers, and pulmonologists, consequently “enlightening” hidden aspects of living with this condition. The second objective was to provide clinicians a new way to communicate with their patients through which they could improve their relationship and treatment of patients with COPD, as well as limit the severity of the disease due to continued risk factor exposure. Accordingly, the project was named “FARO”, which means lighthouse in Italian.
Methods
The study had been carried out from October 2016 to July 2017 under Italian associations of pulmonologists (SIP and AIPO), two Italian associations of general practitioners (FIMMG and SIMG), and two patients’ associations (Associazione Pazienti Onlus BPCO and FederAsma Allergie). Patients and caregivers were invited through a promotional campaign on social media and stakeholders’ collaboration to write their experience. An informative brochure about the project was distributed, and physicians were directly invited to answer to the questionnaire. Survey instruments received approval from a multidisciplinary scientific board before the launch of the project. Moreover, the present study had been approved by the Ethics committee of the Don Carlo Gnocchi Foundation prior to initiation. The project was conducted in accordance with the principles outlined in the Declaration of Helsinki. Each narrative was collected after written informed consent had been provided. In particular, patients and caregivers received separate informed consents that included an introduction to the project together with a guarantee to respect anonymity in analyzing narratives and reporting results as indicated in the Italian Privacy Law.25 To gather quantitative and qualitative data from patients and caregivers, a questionnaire enriched with a narrative plot had been constructed (Tables 1 and 2), while physicians were provided a list of five questions that sought to understand their approach toward key topics of COPD (Table 3). To help patients and caregivers overcome writer’s block,26 the narrative plot was structured using prompts arranged in chronological order following Greenhalgh’s methodology:27 “falling ill”, “being ill”, “getting better”, or “getting worse”. Meanwhile, questions for physicians addressed their relationships with patients and, in particular, how clinicians deal with relevant themes, such as diagnosis communication, explanation of COPD, therapy adherence, and smoking cessation. Inclusion criteria were as follows: for patients, 1) COPD diagnosis, 2) the ability to read and write in Italian, and 3) age over 18 years; for caregivers, 1) caring for a patient with COPD, 2) the ability to read and write in Italian, and 3) age over 18 years; and for physicians, being a pulmonologist or general practitioner managing patients with COPD. Patients, caregivers, and physicians were given the option of filling out the questionnaires online (www.medicinanarrativa.eu/faro) or through printed copies thereof. All data were self-reported and submitted anonymously. All narratives were subsequently uploaded to an online survey platform, SurveyGizmo (www.surveygizmo.com), and downloaded as a Microsoft Excel spreadsheet upon the conclusion of the study.
  | Table 1 The semi-structured plot created for patients |
  | Table 2 The semi-structured plot created for caregivers |
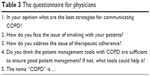  | Table 3 The questionnaire for physicians |
Data and text analysis
Sociodemographic variables of patients and caregivers were analyzed using descriptive statistics (mean, ranges, and classes), while frequencies were reported as percentages. Narratives written in Italian were analyzed using the “grounded theory” approach28 for qualitative interpretation of texts. Reading and interpretation of texts were conducted by three independent researchers to reduce bias.29 A specific semantic evaluation software (NVIVO 10) had been used to analyze narratives, find recurrent words and common synonyms, and obtain clusters. In addition to the grounded theory approach, narrative analysis was carried out in accordance with Kleinman’s30 and Launer’s31 classifications. Accordingly, Kleinman’s classification is used to understand whether the narrative is more “disease-centered”, “illness-centered”, or “sickness-centered”. A “disease-centered” narrative can be described as a biomedical model with a technical and harsh language not open to emotional considerations. An “illness-centered” narrative focuses on living with a particular condition using open language and flowing narration on emotional, familial, and social perspectives. A “sickness-centered” narrative is based on beliefs and habits that the extended society has on a condition or group of patients, that is, sickness depending on others’ perspectives. Launer’s classification, on the other hand, divides narratives into three groups: “progressive”, “stable”, and “regressive”. “Progressive” narratives describe how individuals learn to cope with a disease, “stable” narratives describe no change in attitude, and “regressive” narratives describe worsening of patient’s attitude without coping throughout the narration. To better understand the actual impact COPD had on patients’ and caregivers’ lives, respondents had been requested to utilize metaphors when describing their pathology and breathing.24,32 Responses then underwent ex post, ad hoc analysis, clustering different metaphors into homogeneous groups.
Results
From October 2016 to July 2017, 235 patients, 55 caregivers, and 60 physicians participated in the study, ultimately including 350 experiences. The results of the analysis were introduced using sociodemographic data, after which three key topics on COPD were presented: diagnosis and care, activities of daily living, and smoking. Two other subparagraphs concerning the language and perspective of physicians were included.
Sociodemographic profile
Patients
Narratives represented 17 of the 21 Italian regions and were equally distributed between Northern (38%), Central (26%), and Southern (36%) Italy. Gender distribution was nearly homogeneous: 46% and 54% of respondents were women and men, respectively. The most represented age group was that from 60 to 70 years old (43%), though younger individuals were also included (22% were below 60 years old). Disease severity had been self-evaluated by the patients: 12% declared very severe COPD, 33% severe, 41% moderate, and 14% mild (Table 4).
  | Table 4 Sociodemographic profile of the patients |
Caregivers
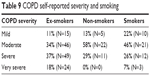
Though caregiver narratives from Southern Italy were prevalent (45%), some were also from Northern (32%) and Central (23%) Italy. Majority of the respondents were women (76%), which can be attributed to their role in the family considering that women generally take care of both elderly individuals and children. Moreover, women usually tend to share their feelings and experiences. Age, occupation, and years of caregiving distributions are presented in Table 5.
  | Table 5 Sociodemographic profile of the caregivers |
Diagnosis and care
Patients
The first symptoms perceived by individuals suffering from COPD usually include shortness of breath, fatigue, coughing, and activity intolerance. Although such symptoms occur during everyday activities, some individuals report their first symptoms during hospitalization for other health problems or after a respiratory crisis. The duration between first symptom appearance and diagnosis was less than 1 year and less than 5 years in 40% and 44% of the cases, respectively. Meanwhile, 12% of the patients waited for more than 5 years to be diagnosed with COPD with a residual 4% declaring more than 20 years. Upon diagnosis communication, 30% of the patients declared to have had a neutral reaction as reported in some narratives: “I felt normal”, “I didn’t care about it”. Indeed, 55% of the patients knew nothing about this pathology and its implications. Another obstacle to the perception of COPD severity includes the difficult technical acronym, which stands for COPD. Patients reported not being able to fully understand what the disease was about, usually believing that it is a “recurrent”, “easy to treat” bronchitis. Patients were found to have different reactions considering their behavior after the diagnosis. Majority of them reacted positively given that 60% decided to take care of themselves and follow doctor’s advices. Moreover, 11% decided to take care of themselves, search for more information, and engage in exercise. Other patients, however, reacted negatively such that 16% decided to give up and limit their activities, while 9% decided to maintain negative habits and do nothing to improve health. A residual 4% decided to search for information to better understand the disease.
The patients evaluated the relationship with general practitioner as “not good” in 14% of cases, “good” in 57% of cases, and “very good” in 29% of cases, while for pulmonologist, 9% declared to have a “not good” relationship, 34% said “good”, and 58% “very good”. Finally, 11% of patients even do not have a trusted pulmonologist.
Caregivers
Upon diagnosis, 44% of caregivers felt concerned about the health of their relatives, 28% felt lost, 22% felt sad, while 6% decided to do something to help their relatives. Moreover, 60% of caregivers expressed strong dedication toward their relatives, 24% showed mixed attitudes between dedication and burden of care activities, while 16% described the burden of care activities as particularly high: “It is very heavy both physically and psychologically”.
The activity that the caregivers do more often was bringing the patient to medical examinations (64%) and to do shopping (39%), while keeping company was considered by caregivers as an activity they “often” (37%) or “sometimes” do (41%). Also, 13% and 15% of the caregivers declared that they dress up and wash the patients “often”, respectively (Table 6).
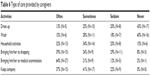  | Table 6 Type of care provided by caregivers |
With regard to hours spent on care activities, 43% of the caregivers spent 1–2 hours per day, while 16% spent more than 8 hours per day. These data are relevant considering that 53% of caregivers were workers who needed to balance working life with care activities. Moreover, 43% of the caregivers declared that care activities had an impact on working life. In particular, 38% had to request for working permits to care for their relatives (Table 7).
  | Table 7 Impact of COPD on caregivers’ working activities |
Activities of daily living
Patients
With regard to patient’s daily activities, home activities were described as “normal” in only 30% of the narratives, while 40% considered it “limited” given that patients needed to implement strategies to carry out activities without getting tired or out of breath: “I do almost all the housework but with a lot of effort and in different ‘episodes’, I cannot lift heavy stuff”, “I do almost all activities but very slowly”. Moreover, 13% of patients engaged in only “soft” activities like watching TV, using their personal computers, and reading, while 17% of the patients stated that they abstained from any domestic work. Evidently, patients with moderate disease severity were less limited, though no relation was found between severity and activity.
Relationships remained “positive” in 74% of the narratives given that patients were able to maintain bonds and were supported by relatives and friends. In some cases, patients stated that they invited friends over to their home to address the difficulty of going out.
Outdoor activities were problematic for individuals with COPD. Accordingly, 32% of the patients stated that outdoor activities were hard to perform. The three main influencing factors found among narratives were weather conditions, obstacles like climbing stairs and going uphill, and oxygen management (35% of the patients used oxygen daily). Interestingly, 29% of the patients describe going out as “positive”. The term “positive” could be interpreted as “freedom”: “going out is a liberation”, “going out make me feel happy as long as I can do it”.
Although COPD has often been observed among elderly individuals who were already retired, only 26% of the patients declared to be retired upon diagnosis. This meant that COPD had some impact on working life. In particular, 21% of the employees had to stop working, while 12% of the self-employed had to interrupt their activities (Table 8).
  | Table 8 Impact of COPD on patients’ working activities |
Twenty-three percent of respondents declared to have difficulties during self-care and domestic activities such as “take a shower”, “dress me up, tie my shoes”, “do shopping”, and “housekeeping”; 31% declared difficulties in doing physical activities like walking and climb stairs; and 13% declared difficulties in the social context like “make people accept my limitations”, “I cannot find a job because of disease”, and “bureaucracy”. For 10%, the difficulties were given by COPD symptoms like “cough”, “dyspnea”, and “lack of breath”. Other patients gave generic answers like no/few (11%) or many (13%) difficulties.
Considering the achievements, 33% declared the resumption of activities, 25% declared to have accepted the disease, 10% declared a physical improvement, 3% said they had stopped smoking, and 28% declared they did not have any achievement.
Caregivers
COPD also had an impact on the activities of relatives who needed to change their daily routine. Among a list of five items (“going out for short period”, “going out for long period”, “travel in Italy”, “travel in foreign countries”, and “have leisure time”), the most influenced were those about traveling. Accordingly, 50% of the caregivers considered it very difficult to travel to foreign countries, while 50% found it difficult to travel even within Italy. Moreover, 33% of the participants considered it very difficult to be away for long periods.
Difficulties faced when dealing with different situations resulted from caregiving activities (21%), as underlined in some expressions (“Finding outside and suddenly arriving at an attack, not having the cortisone to intervene”, and “do not know how to intervene immediately”), and psychological support (79%) (“To make him understand that he still has residual capacities to exploit”, “To give him courage and patience”), while achievements were linked to COPD management (25%) and activities (75%).
Smoking
Patients
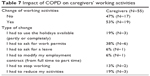
Among the patients included, 60% declared to have been past smokers who had quit after COPD diagnosis, 20% were still smoking, and the remaining 20% had never smoked. Considering the relationship between COPD self-reported severity and smoking habits, we found that none of the non-smokers considered the COPD as very severe, while 7% of the smokers declared to have very severe COPD (Table 9). This result can be considered as aligned with several studies; smokers with COPD generally experience more rapid deterioration of lung function33 that probably affects patients’ quality of life, and consequently, more severe symptoms associated with an advanced disease could also be perceived in a worse manner by patients who have not already quit with smoking than who has never smoke.
  | Table 9 COPD self-reported severity and smoking |
With regard to patients’ feelings about cigarettes, 62% refused smoking completely, 28% felt dependent, and 10% felt nostalgic. The words most frequently used by patients to describe smoking were “poison”, “enemy”, “problem”, “nightmare”, and “harmful”, as well as “important” and “memory”. Moreover, 20% of the non-smokers declared that they developed COPD for two main reasons: previous respiratory pathologies, like infections or asthma, and occupational exposure or passive smoking.
Caregivers
Caregivers considered smoking the cause of their relative’s disease. Thus, the predominant feeling was hate with frequently used words in the narratives including “bad”, “to abolish”, and “cancer”.
Language of the narratives
After analyzing the language following Kleinman’s classification, majority of the patients’ and caregivers’ narratives were found to be “illness-centered” with only a few of the patients’ narratives and none of the caregivers’ narratives being “sickness-centered” (Table 10). Using Launer’s classification, caregiver’s narratives were found to be more progressive than patients’ narratives (Table 11).
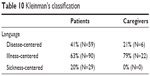  | Table 10 Kleinman’s classification |
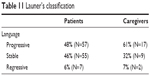  | Table 11 Launer’s classification |
Metaphors
Patients
Images selected to describe COPD can be clustered in four categories: breathlessness, sadness, fragility, and desperation. Considering that the sentences were threatening in nature, metaphors help us understand that despite the initial neutrality upon diagnosis communication, patients perceive the illness with fear (“a tsunami”, “an ordeal”), anxiety (“I’m closed in a bag”, “An iron cage that tightens your chest”), and sadness (“a completely bare tree”). Many of the metaphors indicate how COPD strongly limits their activities.
Caregivers
Caregivers selected images that evoked fragility, sadness, and anguish. Some of these images suggest “lack”, for example, “a fish out of water”, “swallow without wings”, while others indicate “impossibility”, for example, “a sparrow who wants to fly, flaps his wings but fails”, “a lion that advances and retracts”. A number of caregivers imagined something that hinders breathing, for example, “something that compresses the chest”, “London wrapped in smog”, while others selected natural elements with either negative (“tornado”, “storm”) or positive (“sea”, “breeze”) connotations.
Perspective on the future
Patients
Thirty-six percent of the patients hoped to improve their condition, 11% not to get worse, 14% a situation of serenity, both for themselves and for their family, 11% expressed a desire to heal, and 12% would like to go back in time when they did not have COPD: “to have new lungs and bronchi”, “two lungs cloned by mine and to be able to continue to enjoy my family and still a little bit of life”, “that finally we can find a cure that restores breath to those like me”, “walking, seeing my city in its alleys, going to dance, going to the market at the theater and laughing because today I cannot even do what I cough”. Just 9% of patients have fear for the future and imagine the death “I will never have tomorrow, I will never get out of this disease”.
Caregivers
The caregivers’ hope for the patients’ future was frequently a stabilization of the disease (38%), an improvement of clinical condition (31%), and an improvement from a psychological point of view (31%).
Physicians’ approach
Diagnosis
Diagnosis communication is exceedingly important given that the manner in which the disease is explained to the patient can change their approach to the care pathway. Physicians communicate the diagnosis using various approaches, majority of which can be considered as “illness-centered”. Indeed, 33% of the physicians provided general information regarding COPD, while others preferred to comment on test results (7%), discuss therapies (7%), or stress the consequences of this pathology (8%). During discussions, 20% of the clinicians tried to be as understandable as possible using simple words and pictures. Moreover, 15% of the physicians stated they were able to establish a good relationship with their patients and create a therapeutic alliance, while 10% of respondents proposed social communication to raise COPD awareness. Communicating a diagnosis of COPD can be difficult due to the technical nature of its name. Indeed, 54% of the physicians believed that the name of the pathology – COPD or BPCO in Italian – was difficult for patients to understand, 22% thought that it was ineffective, and 11% stated that the definition must be explained to the patient. Only 11% of the respondents found the name to be appropriate.
Smoking
Given that smoking is the main risk factor for COPD and quitting smoking has been proven to be the most effective method for achieving clinical improvement,34 it was one of the topics included in the clinicians’ questionnaire. After analyzing physicians’ approach, 39% of the respondents were found to have a “counseling” attitude toward their patients such that they tried to understand the reason why patients continued smoking, as well as their psychological needs. Moreover, 14% of the physicians tried to negotiate with their patients. While establishing goals in terms of number of cigarettes per day, 47% opted for an intimidating approach wherein they explained all the frightening consequences of smoking: “I say that smoking for a COPD patient is like to heal a wound with muriatic acid”.
Discussion
The FARO research, whose main aim was to “enlighten” the hidden aspects of living with COPD, gathered the points of view of patients, caregivers, and doctors and gave a complete and complex picture of care and awareness of this chronic condition. Several multiperspective studies have recently highlighted the importance of the doctor–patient communication to improve the physicians’ deeper understanding of the impact of the COPD on patients’ life.35,36 Although the importance of the caregiver has been demonstrated to be crucial in COPD,37 there is still an urgent need to examine the effectiveness of strategies to assist caregivers to provide direct care, encourage adherence to health care provider recommendations, act as a health care advocate, and provide emotional and psychosocial support to individuals with COPD. No other study in the Italian context has already investigated the caregivers’ point of view. In the present research, 235 patients, 55 family members, and 60 doctors were involved.
Signs of neurological and psychological burden of people suffering from chronic respiratory diseases as COPD emerged from literature.38 In particular, using validated questionnaires, several studies revealed COPD patients’ elevated scores on hypochondria, depression, introversion, anxiety, sensitiveness, despair, and hostility due to their living with this condition.39,40 However, narrative research is shown to be more informative than data from questionnaires, being able to delve into the causes of this psychological burden. Among 40% of the patients, the duration between the first symptoms and diagnosis was less than 1 year. Recent studies have demonstrated that early diagnosis,41 smoking cessation efforts, and early treatment42,43 can have a beneficial effect on inhibiting the worsening of COPD, especially during the initial phases where loss of lung function appears to be more accelerated and significant.44
Emotional reactions to diagnosis remained “neutral” in 30% of the patients, possibly due to the lack of information regarding this pathology. This percentage is quite high considering reactions to being diagnosed with other chronic pathologies, such as chronic spontaneous orticaria,45 myelophibrosis,46 and multiple sclerosis.47 The high percentage of “neutral reaction” can be attributed to low awareness for COPD. Moreover, if we consider the reaction to other lung diseases, such as lung cancer or emphysema, the patients and family members are generally immediately alerted, while a diagnosis of COPD is met with a much subtler reaction.
Hence, raising awareness could help people understand the seriousness of COPD and the consequences of neglecting the disease. COPD has a considerable impact on daily activities such that only 30% and 17% of the patients considered home and outdoor activities “normal”, respectively. This limitation has consequences on the lives of not only patients, who could develop a form of depression and anxiety, but also caregivers and family members48 who have to cope with the situation. Patients find it necessary to limit outdoor activities such that the house becomes a safe place. This, however, causes isolation and loneliness and becomes a metaphorical “prison”. The relevance of the daily activities is proved also by difficulties and achievements reported by patients; in fact, in the majority of cases, they are linked with “activities”: the patients are happy to have resumed to do some activities and declared that the main difficulties for them are in doing activities at home and outside.
The relationship with professionals reported by patients are basically good; in particular, from the narratives, it is possible to find that relationship with pulmonologists is a little bit better than the relationship with general practitioner (GP): 57% consider the relationship with GP as “good”, while 58% of participants consider the relationship with pulmonologist as “very good”.
Another important outcome of our study is related to the patients’ age: only 36% were more than 70 years old. Indeed, 26% of the employees and 40% of the self-employed were already retired upon diagnosis. Other patients were diagnosed with COPD during their working life, which subsequently affected their job. In fact, 76% of the employees and 65% of the self-employed stated that COPD has an impact on working activities. This is important for doctors and, in particular, general practitioners who have to broaden their vision on the patient not focusing only on symptoms but also on professional life, satisfaction, and possible future, understanding the needs of these patients who have to combine an active life with the management of the COPD. Moreover, it is important to monitor all the patients, especially smokers, encouraging prevention and early treatment.
The results of this study confirm the evidence in literature about the role of caregivers and about the burden of caregiving.37 In fact, narratives have shown the importance of their physical and psychological support and the influence that COPD has on caregivers’ lives and working activities. Indeed, 53% of the caregivers stated that COPD had an impact on their working life. In caregivers’ narratives, no correlation was found between both emotional and physical fatigue and years of informal caregiving. From the narratives, caregivers demand not only psychological support but also clear instructions and training on the patients care. Cases in which education has been delivered to caregiver and patient as a dyad with no significant improvement in outcome49 can be found in literature; maybe an education tailored on caregivers’ narratives could have more significant impact on COPD management.
For the future, both the patients and the caregivers expressed the hope for an improvement or stabilization of the disease and for have a serene future; patients’ narratives in some cases described dreams and wishes, for example, some patients hoped to heal from the COPD or to have new lungs or to go back in time and change the past. These hopes show patients’ sadness about their condition or even their sense of guilt.
The main limitation of the project was not to have considered the professionals’ narratives, but just have asked few questions. The collection of professionals’ narratives could be a future perspective of the research team. Furthermore, since the main aim of the research was not the correlation and comparison of patients’ and caregivers’ narratives from the same situation, it did not focus on this aspect, but research taking into consideration the points of view of patient, caregiver, and professional on the same case could be interesting to deepen the insight into the clinical history of patients. Finally, owing to the narrative nature of the project, that is mainly self-reported and focused on the real experiences of sufferers from COPD, one of the project limitations is not to have considered other self-assessment validated scales to integrate the qualitative research into quantitative data, for example, to evaluate the severity of the disease or measure the patients’ and caregivers’ level of stress.
The present research suggests that COPD is linked to not only smoking but also other factors considering that 20% of the patients had never smoked.50 Future research should also focus on such patients, while improving the understanding on other risk factors. Nevertheless, smoking still remains a particularly important issue for COPD. In fact, 80% of the patients were ex- (60%) or current smokers (20%). Thus, innovative campaigns to raise awareness regarding this pathology and the link between smoking and COPD should definitely be improved.
Language analysis provides several hints on possible strategies that can be adopted by physicians. Though doctors generally use technical language, patients would need another type of language to better understand the meaning of COPD and the importance of therapy. Metaphorical language could be one example given that it allows for the simple expression of complex concepts.51 Metaphors selected by patients and caregivers expressed fear and panic, which may indicate suffering: “I’m captive in a glass bubble”, “(COPD is) an iron cage that tightens your chest”, “fog”, “prison”. The aforementioned images could also be used by physicians to enrich the explanation of the diagnosis to help patients understand how COPD could eventually progress.
The medical term “COPD” is very difficult to handle for promoting awareness regarding the potential severity of this condition. The Italian translation of COPD is even more difficult to comprehend than the English term. Indeed, 89% of the physicians stated that this definition was not appropriate given that it was either difficult to understand or ineffective without proper explanation, and this has to be supported with technical explanation in an easier language, recurring also to daily life metaphors.
Physicians are therefore challenged to find new ways of communicating COPD, to implement campaigns that would intercept patients at a very early stage and encourage corrective habits. Finally, caring for caregivers’ lives should be among the important social objectives.
Acknowledgments
The authors acknowledge all the physicians who collaborated in the realization of the project, in particular Carla Bena and Elisabetta Iacono Pezzillo of ASL TO4 and Gherardo Siscaro of Fondazione Maugeri of Sciacca. The authors also acknowledge Agnese Di Leo, Denise D’Orio, Luigi Reale, Eleonora Volpato, and Tania Ponta for their precious support.
Disclosure
The authors report no conflicts of interest in this work.
References
Global Strategy for the Diagnosis, Management and Prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD). 2017. Available from: https://goldcopd.org/gold-reports-2017/. Accessed September 01, 2018. | ||
Bettoncelli G, Blasi F, Brusasco V, et al. The clinical and integrated management of COPD. An official document of AIMAR (Interdisciplinary Association for Research in Lung Disease), AIPO (Italian Association of Hospital Pulmonologists), SIMER (Italian Society of Respiratory Medicine), SIMG (Italian Society of General Medicine). Multidiscip Respir Med. 2014;9(1):25. | ||
Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD: role of comorbidities. Eur Respir J. 2006;28(6):1245–1257. | ||
Cazzola M, Puxeddu E, Bettoncelli G, et al. The prevalence of asthma and COPD in Italy: a practice-based study. Respir Med. 2011;105(3):386–391. | ||
Rochea N, Perez T, Neukirch F, et al. High prevalence of COPD symptoms in the general population contrasting with low awareness of the disease. Revue des Maladies Respiratoires. 2008;28(7):e58–e65. | ||
Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet. 2004;364(9434):613–620. | ||
Sanduzzi A, Balbo P, Candoli P, et al. COPD: adherence to therapy. Multidiscip Respir Med. 2014;9(1):60. | ||
Lyna P, McBride C, Samsa G, Pollak KI. Exploring the association between perceived risks of smoking and benefits to quitting: who does not see the link? Addict Behav. 2002;27(2):293–307. | ||
Eisner MD, Anthonisen N, Coultas D, et al; Committee on Nonsmoking COPD, Environmental and Occupational Health Assembly. An official American Thoracic Society public policy statement: novel risk factors and the global burden of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;182(5):693–718. | ||
Zhong N, Wang C, Yao W, et al. Prevalence of chronic obstructive pulmonary disease in China: a large, population-based survey. Am J Respir Crit Care Med. 2007;176(8):753–760. | ||
Stoller JK, Aboussouan LS. Alpha1-antitrypsin deficiency. Lancet. 2005;365(9478):2225–2236. | ||
Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370(9589):765–773. | ||
Bourbeau J, Bartlett SJ. Patient adherence in COPD. Thorax. 2008;63(9):831–838. | ||
Ágh T, Inotai A, Mészáros Á. Factors associated with medication adherence in patients with chronic obstructive pulmonary disease. Respiration. 2011;82(4):328–334. | ||
Blasi F, Raddi F, Miravitlles M. Interactive monitoring service and COPD: is it possible to reduce nonadherence? J Chron Obstruct Pulmon Dis. 2015;12(3):227–233. | ||
López-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology. 2016;21(1):14–23. | ||
Harb N, Foster JM, Dobler CC. Patient-perceived treatment burden of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2017;12:1641–1652. | ||
Miravitlles M, Peña-Longobardo LM, Oliva-Moreno J, Hidalgo-Vega Á. Caregivers’ burden in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:347–356. | ||
Greenhalgh T. Cultural contexts of health: the use of narrative research in the health sector. Copenhagen: WHO Regional Office for Europe; 2016. (Health Evidence Network Synthesis Report, No. 49.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK391066/. Accessed September 01, 2018. | ||
Charon R. At the membranes of care: stories in narrative medicine. Acad Med. 2012;87(3):342–347. | ||
Greenhalgh T, Hurwitz B. Why study narrative? In: Greenhalgh T, Hurwitz B, editors. Narrative Based Medicine: Dialogue and Discourse in Clinical Practice. London, UK: BMJ Books; 1998:3–16. | ||
Lees C. Measuring the patient experience. Nurse Res. 2011;19(1):25–28. | ||
Marini MG, Reale L, Cappuccio A, et al. Narrative medicine to highlight values of Italian pain therapists in a changing healthcare system. Pain Manag. 2014;4(5):351–362. | ||
Marini MG. Narrative Medicine. Milano, Italy: Springer; 2016. | ||
Personal data code protection. Law no. 196. Ital J. 2003;174(Section 123). | ||
Marini MG, Reale L, Cappuccio A, et al. Narrative medicine to highlight values of Italian pain therapists in a changing healthcare system. Pain Manag. 2014;4(5):351–362. | ||
Hurwitz B, Greenhalgh T, Skultans V. Narrative Research in Health and Illness. London, UK: British Medical Association; 2004. | ||
Glaser BG, Strauss AL, Strutzel E. The Discovery of grounded theory: strategies for qualitative research. Nurs Res. 1968;17(4):364. | ||
Duque RL. Review: Catherine Kohler Riessman (2008). Narrative methods for the human sciences. CA, USA: SAGE publications. 2010:11(1): 244 pages. | ||
Kleinman A. The Illness Narrative, Suffering, Healing and the Human Condition. New York: Basic Book; 1989. | ||
Launer J. New Stories for Old: narrative-based primary care in Great Britain. Families, Systems and Health. 2006;24(3):336–344. | ||
Hanne M. Diagnosis and metaphor. Perspect Biol Med. 2015;58(1):35–52. | ||
Willemse BW, Postma DS, Timens W, ten Hacken NH. The impact of smoking cessation on respiratory symptoms, lung function, airway hyperresponsiveness and inflammation. Eur Respir J. 2004;23(3):464–476. | ||
Underner M, Perriot J, Peiffer G. Sevrage tabagique du fumeur atteint de bronchopneumopathie chronique obstructive. [Smoking cessation in smokers with chronic obstructive pulmonary disease]. Rev Mal Respir. 2014;31(10):937–960. French. | ||
Steiner JF, Earnest MA. The language of medication-taking. Ann Intern Med. 2000;132(11):926–930. | ||
Celli B, Blasi F, Gaga M, et al. A Perception of symptoms and quality of life – comparison of patients’ and physicians’ views in the COPD MIRROR study. Int J Chron Obstruct Pulmon Dis. 2017;12:2189–2196. | ||
Nakken N, Janssen DJA, van den Bogaart EHA, et al. Informal caregivers of patients with COPD: home sweet home? Eur Respir Rev. 2015;24(137):498–504. | ||
Rzadkiewicz M, Bråtas O, Espnes GA. What else should we know about experiencing COPD? A narrative review in search of patients’ psychological burden alleviation. Int J Chron Obstruct Pulmon Dis. 2016;11:2295–2304. | ||
Hynninen KM, Breitve MH, Wiborg AB, Pallesen S, Nordhus IH. Psychological characteristics of patients with chronic obstructive pulmonary disease: a review. J Psychosom Res. 2005;59(6):429–443. | ||
Güell R, Resqueti V, Sangenis M, et al. Impact of pulmonary rehabilitation on psychosocial morbidity in patients with severe COPD. Chest. 2006;129(4):899–904. | ||
Csikesz NG, Gartman EJ. New developments in the assessment of COPD: early diagnosis is key. Int J Chron Obstruct Pulmon Dis. 2014;9:277–286. | ||
Drummond MB, Hansel NN, Connett JE, Scanlon PD, Tashkin DP, Wise RA. Spirometric predictors of lung function decline and mortality in early chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;185(12):1301–1306. | ||
Tantucci C, Modina D. Lung function decline in COPD. Int J Chron Obstruct Pulmon Dis. 2012;7:95–99. | ||
Borrill ZL, Houghton CM, Tal-Singer R, et al. The use of plethysmography and oscillometry to compare long-acting bronchodilators in patients with COPD. Br J Clin Pharmacol. 2008;65(2):244–252. | ||
Cappuccio A, Limonta T, Parodi A, et al. Living with chronic spontaneous urticaria: a project of narrative medicine for improving the pathway of care. Acta Derm Venereol. 2017;97(1):81–85. | ||
Palandri F, Benevolo G, Iurlo A, et al. Life for patients with myelofibrosis: the physical, emotional and financial impact, collected using narrative medicine-Results from the Italian ‘Back to Life’ project. Qual Life Res. 2018;27(6):1545–1554. | ||
Storie luminose. Esperienze di straordinaria quotidianità nei racconti delle persone che vivono con la sclerosi multipla, 24 Ore Cultura. [Bright stories. Experiences of extraordinary daily life in the stories of people living with multiple sclerosis, 24 hours Culture]. 2015. Italian. | ||
Badr H, Federman AD, Wolf M, Revenson TA, Wisnivesky JP. Depression in individuals with chronic obstructive pulmonary disease and their informal caregivers. Aging Ment Health. 2017;21(9):975–982. | ||
Bryant J, Mansfield E, Boyes AW, Waller A, Sanson-Fisher R, Regan T. Involvement of informal caregivers in supporting patients with COPD: a review of intervention studies. Int J Chron Obstruct Pulmon Dis. 2016;11:1587–1596. | ||
Agustì A, Faner R. COPD beyond smoking: new paradigm, novel opportunities. Lancet Respir Med. 2018;6(5):324–326. | ||
Thibodeau PH, Boroditsky L. Metaphors we think with: the role of metaphor in reasoning. PLoS One. 2011;6(2):e16782. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
