Back to Journals » OncoTargets and Therapy » Volume 12
Endoscopic submucosal dissection of tracheal deep benign fibrous histiocytoma using hybrid knife
Authors Ma J, Miao Y , Lin X , Wang Q, Wang W, Kang J, Hou G
Received 28 April 2019
Accepted for publication 24 June 2019
Published 11 July 2019 Volume 2019:12 Pages 5609—5613
DOI https://doi.org/10.2147/OTT.S213747
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Leo Jen-Liang Su
Jiang-wei Ma,1 Yuan Miao,2 Xu-yong Lin,2 Qiu-yue Wang,1 Wei Wang,1 Jian Kang,1 Gang Hou1
1Department of Pulmonary and Critical Care Medicine, First Hospital of China Medical University, Shenyang, People’s Republic of China; 2Department of Pathology, The First Hospital and College of Basic Medical Sciences, China Medical University, Shenyang, People’s Republic of China
Abstract: Deep benign fibrous histiocytoma (FH) is an uncommon and poorly recognized tumor that arises in subcutaneous or deep soft tissue. Deep benign FH of the trachea is even more rare. Deep benign FH recurs in approximately 20% of cases, so surgical resection is the recommended treatment for FH. However, some patients are afraid of the trauma and potential complications from the resection of tracheal tumors, so they do not accept surgical resection. With the development of interventional pulmonology, bronchoscopic intervention plays a key role in the treatment of benign tracheal tumors. Novel tools have emerged in interventional pulmonology and optimized the traditional techniques. Here, we report a case of deep benign FH of the trachea with broad base relapse after electrocautery with snare, argon plasma coagulation (APC) and radiotherapy. It was treated successfully by endobronchial resection with a hybrid knife (HK) and APC. The HK is a hybrid device that combines an electrocautery knife with a water jet in one instrument. Submucosal injection and circumferential cutting and dissection of lesions as well as coagulation of bleeding can be performed only with the HK. During the 6 months follow-up, the deep benign FH of the trachea did not relapse. In the case reported herein, the HK enabled submucosal injection and circumferential cutting and dissection of lesions as well as access to submucosal lesions to gain further adequate APC treatment, thereby allowing a better clinical response than that achieved by traditional electrocautery with snare and APC. In conclusion, the HK with a water jet is a feasible and effective endoscopic method for management for benign or low-grade malignant neoplasms of the trachea, especially those with a wide base and submucosal involvement.
Keywords: tracheal tumors, interventional pulmonology, fibrous histiocytoma, electrocautery, hybrid knife
Introduction
Benign fibrous histiocytoma (FH) is one of the most common mesenchymal neoplasms of the skin. Deep benign FH is an uncommon and poorly recognized clinical subtype that arises in subcutaneous or deep soft tissue.1 Tracheal deep benign FH is rare. Limited information is available concerning the clinical behavior of deep FH due to the paucity of the literature. Although the preferred therapy is surgery for such benign tracheal tumors, bronchoscopic interventions are important and effective alternatives.2–4
A variety of techniques, such as electrocautery, argon plasma coagulation (APC), laser, and cryotherapy through a flexible or rigid bronchoscope, have been applied to treat tracheal-bronchial tumors. However, electrocautery is suitable for tumors with peduncular structures and limited in tumors with a wide base. For tracheal tumors with a wide base and membranous wall involvement, the depth of APC treatment is approximately 3–4 mm (although relatively safer but not deep enough for elimination of the tumor), and treatment with laser has the risk of perforation. The hybrid knife (HK) treatment was first applied in the endoscopic submucosal dissection (ESD) of gastrointestinal neoplasms. It is a hybrid device that combines an electrocautery knife with a water jet in one instrument. It should simplify and accelerate ESD, because submucosal injection and circumferential cutting and dissection of lesions as well as coagulation of bleeding can be performed with the same device.5 The membrane wall is a special portion of the trachea with a continuous muscular layer, which enables the application of the HK for submucosal injection, circumferential cutting and dissection of lesions, and exposure of submucosal lesions to gain further adequate treatment.
Here, we reported a case of deep benign FH of the trachea with a broad base relapse after electrocautery with snare, APC and radiotherapy. It was treated successfully by HK and APC without relapse. The patient provided written informed consent to have the case report and any accompanying images published. Institutional approval was obtained from the Institutional Ethical Review Board of First Hospital of China Medical University to publish the case details.
Case report
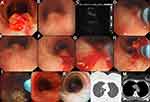
A 32-year-old female was admitted to our department for recurrent tracheal tumor. Half a year ago, she presented with progressive exertional dyspnea and wheezing for 1 month. A chest computed tomography (CT) revealed an endotracheal mass of 11 mm in diameter and approximately 30 mm from the carina (Figure 1A). The patient underwent bronchoscopy that showed a well circumscribed posterior soft mass occluding over 90% of the tracheal lumen (Figure 1B). The patient refused surgical resection of the trachea and accepted bronchoscopic treatment with electrocautery snare and APC (Figure1C).
Histopathological findings: sections from routine formalin fixation and paraffin embedded tissue stained with hematoxylin and eosin revealed ovoid to spindle shaped histiocytes in a storiform pattern accompanied by stromal fibrous tissue hyperplasia with sclerosis (Figure1D, E), Immunohistochemically tumor cells were positive for vimentin and CD68 (Figure 1F, G), negative for CD34 and epidermal membrane antigen (EMA). Hence, the histology was in consistent with the diagnosis of deep benign fibrous histiocytoma. She also accepted radiotherapy after endobronchial resection with 60Gy/30f. Unfortunately, 6 months later, tumor recurrence was observed (Figure 2A, B). Considering the insufficient depth of the electrocautery snare and APC treatment may have contributed to the relapse, with full informed consent, the HK was used to dissect the tumor and expose the lesion located in the basal layer. Tumor basal depth and blood flow was assessed by endobronchial ultrasound (EBUS) before treatment (Figure 2C). We used a water jet HK (Erbe Hybrid Knife® T-type I-jet, ERBE Elektromedizin) to perform electrosurgical circumferential cutting and dissection of the base of the tracheal lesion, and we used a water jet to inject a solution of 2% lidocaine into the submucosal layer with 30 Bar pressure (Figure 2D, E). After making a pinhole in the margin of the elevated mucosa with the HK (Figure 2F), the tip of the HK was inserted into the hole, and a circumferential incision was made (VIO mode ENDO CUT Q, effect3-width1-interval of incision4, Coagulation effect2 and 30W) (Figure 2G, H). Finally, the incised piece of lesion was collected using a cryoprobe. The lesion in the submucosal layer was fully exposed and then treated with APC (Figure 2I, J). The pathological result was still benign FH. There was no recurrence at 9 months follow-up on bronchoscopy and chest CT (Figure 2K–M).
Discussion
FH is a mesenchymal tumor first described by O’Brien and Stout6 and occurs predominantly in the soft tissue and bones. Tracheal FH is very rare. Due to the limited number of cases in the literature, the biological behavior of this tracheal neoplasm is unclear at present. A complete analysis suggested that this neoplasm might be evaluated as a low-grade malignancy.7
Surgical resection is the recommended treatment for FH because local recurrence may occur if the tumor is incompletely excised.8–10 Deep benign FH recurs in approximately 20% of cases, and metastases are rare.1 Some patients are afraid of the trauma and potential complications of the surgical resection of tracheal tumors, so they do not accept surgical resection, and some patients with long lesion cannot accept surgical resection. With the development of interventional pulmonology, bronchoscopic intervention plays a key role in treating benign tracheal tumors.11–13 Conforti et al14 reported a case of tracheal FH in an infant successfully treated by endoscopy and Nd:YAG(neodymium:yttrium alluminum garnet) laser. Because a few of the benign or low-grade malignant tumors are prone to recur or change to malignancy, it is very important to repeat bronchoscopies for follow-up. We must carefully practice interventional bronchoscopy to avoid hampering possible surgery in the future.15 Our patient accepted electrocautery and APC, but the tumor relapsed shortly after. We considered the main cause of the local recurrence was due to the inadequate depth and width of the endoscopic treatment, and the elimination of the lesions located in the submucosal layer was insufficient. Worrying about the risk of tracheal perforation with the laser, we used the HK as a treatment option. The HK is a novel electrosurgical instrument, which combines submucosal injection and electrocautery. The feasibility of this new device has been assessed in animal stomach, esophagus and colon and there are quite a number of initial experiences in humans.16,17 Besides the treatment of early stage gastrointestinal tumors, the hybrid knife has been reported in en bloc transurethral resection of bladder tumour which is nonmuscle invasive,18 and treatment of primary tracheal mucosa-associated lymphoid tissue lymphoma,19 also for the diagnosis of pleural effusions.20 Based on the previous experience of using a HK via semirigid thoracoscopy for electrocautery biopsy of the pleura,20 we hypothesized that the HK could make the dissection of a tracheal lesion large and deep enough without obvious damage because of the submucosal water cushion, making APC treatment of the fully exposed base more effective. The clinical response of our case supported our hypothesis. Our case demonstrated that the HK is a potential tool for sufficient resection of benign or low-grade malignant tracheal tumors with a wide base and membranous wall involvement, the base can be completely elevated and dissected and exposure of submucosal lesions to gain further adequate APC treatment.
The most common complications in the treatment of tumors of the membranous trachea are bleeding and perforation. The combination of electrocautery and electrocoagulation may decrease the risk of bleeding. The HK can create an adequate submucosal cushion, and the direction of dissection can be targeted tangentially to the surface of the lesion at the submucosal layer to minimize the risk of perforation.5 Additionally, the thermal and mechanical damage of the resection bed is less pronounced because of the tissue-sparing blunt dissection of the submucosa by the higher amount of injected fluid and the water jet HK.5
However, there are several limitations. We reported only one case, and more cases of benign or low-grade tracheal malignancies should be evaluated. In addition, long-term follow-up should be performed to observe the long-term efficacy of the HK method.
Conclusion
The HK is a novel tool for endoscopic management of benign or low-grade malignant tracheal neoplasms, especially those with a wide base and submucosal involvement.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gleason BC, Fletcher CD. Deep “benign” fibrous histiocytoma: clinicopathologic analysis of 69 cases of a rare tumor indicating occasional metastatic potential. Am J Surg Pathol. 2008;32(3):354–362. doi:10.1097/PAS.0b013e31813c6b85
2. Guo L, Wang K, Zhu H, Liu N, Zhu D. Treatment of primary tracheal glomus tumors: two case reports and a literature review. Medicine (Baltimore). 2018;97(15):e0374. doi:10.1097/MD.0000000000010374
3. Scarlata S, Fuso L, Lucantoni G, et al. The technique of endoscopic airway tumor treatment. J Thorac Dis. 2017;9(8):2619–2639. doi:10.21037/jtd.2017.07.68
4. Rabeau A, Mazieres J, Hermant C, Projetti F, Didier A, Guibert N. Bronchoscopic multimodal management of tracheal neurofibroma. J Bronchology Interv Pulmonol. 2016;23(4):340–342. doi:10.1097/LBR.0000000000000220
5. De-la-Pena J, Calderon A, Esteban JM, et al. Experimental study of hybrid-knife endoscopic submucosal dissection (ESD) versus standard ESD in a Western country. Rev Esp Enferm Dig. 2014;106(2):98–102.
6. O’Brien JE, Stout AP. Malignant fibrous xanthomas. Cancer. 1964;17:1445–1455. doi:10.1002/1097-0142(196411)17:11<1445::aid-cncr2820171112>3.0.co;2-g
7. Ozturk S, Kutlay H, Sak SD, Yavuzer S. Fibrohistiocytic tumor of the trachea in a child. Eur J Cardiothorac Surg. 1999;16(4):464–468. doi:10.1016/s1010-7940(99)00288-2
8. Sandstrom RE, Proppe KH, Trelstad RL. Fibrous histiocytoma of the trachea. Am J Clin Pathol. 1978;70(3):429–433. doi:10.1093/ajcp/70.3.429
9. Gonzalez-Campora R, Matilla A, Sanchez-Carrillo JJ, Navarro A, Galera H. ‘Benign’ fibrous histiocytoma of the trachea. J Laryngol Otol. 1981;95(12):1287–1292.
10. Sculerati N, Mittal KR, Greco MA, Ambrosino MM. Fibrous histiocytoma of the trachea: management of a rare cause of upper airway obstruction. Int J Pediatr Otorhinolaryngol. 1990;19(3):295–301.
11. Handa A, Fujita K, Yamamoto Y, Komori K, Miyakawa T. Tracheal Tumor. J Pediatr. 2016;173:262–262 e261. doi:10.1016/j.jpeds.2016.03.017
12. Isaac BT, Christopher DJ, Thangakunam B, Gupta M. Tracheal schwannoma: completely resected with therapeutic bronchoscopic techniques. Lung India. 2015;32(3):271–273. doi:10.4103/0970-2113.156252
13. Miller SM, Bellinger CR, Chatterjee A. Argon plasma coagulation and electrosurgery for benign endobronchial tumors. J Bronchology Interv Pulmonol. 2013;20(1):38–40. doi:10.1097/LBR.0b013e318282d3ca
14. Conforti S, Bonacina E, Ravini M, Torre M. A case of fibrous histiocytoma of the trachea in an infant treated by endobronchial ND:YAG laser. Lung Cancer. 2007;57(1):112–114. doi:10.1016/j.lungcan.2007.01.023
15. Gao H, Ding X, Wei D, et al. Endoscopic management of benign tracheobronchial tumors. J Thorac Dis. 2011;3(4):255–261. doi:10.3978/j.issn.2072-1439.2011.09.02
16. Schumacher B, Charton JP, Nordmann T, Vieth M, Enderle M, Neuhaus H. Endoscopic submucosal dissection of early gastric neoplasia with a water jet-assisted knife: a Western, single-center experience. Gastrointest Endosc. 2012;75(6):1166–1174. doi:10.1016/j.gie.2012.02.027
17. Takeuchi Y, Uedo N, Ishihara R, et al. Efficacy of an endo-knife with a water-jet function (Flushknife) for endoscopic submucosal dissection of superficial colorectal neoplasms. Am J Gastroenterol. 2010;105(2):314–322. doi:10.1038/ajg.2009.547
18. Islas-Garcia JJ, Campos-Salcedo JG, Lopez-Benjume BI, et al. Surgical technique for en bloc transurethral resection of bladder tumour with a Hybrid Knife((R)). Actas Urol Esp. 2016;40(4):263–267. doi:10.1016/j.acuro.2015.11.001
19. Li Y, Jiang J, Herth FJF, et al. Primary tracheal mucosa-associated lymphoid tissue lymphoma treated with a water-jet hybrid knife: a case report. Respiration. 2019;97(2):168–172. doi:10.1159/000494064
20. Yin Y, Eberhardt R, Wang XB, et al. Semi-rigid thoracoscopic punch biopsy using a hybrid knife with a high-pressure water jet for the diagnosis of pleural effusions. Respiration. 2016;92(3):192–196. doi:10.1159/000448556
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.