Back to Journals » International Journal of General Medicine » Volume 7
Endoscopic alterations in a cohort of hemodialysis patients: a cross-sectional study
Authors Bacci MR , Russo F, Carvalho G, Zimberg Chehter E, Jordao VDCR, Fonseca FLA
Received 9 June 2014
Accepted for publication 30 June 2014
Published 16 September 2014 Volume 2014:7 Pages 459—461
DOI https://doi.org/10.2147/IJGM.S68999
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
MR Bacci,1 FT Russo,1 GD Carvalho,1 EZ Chehter,2 VC Jordao,1 FL Fonseca1
1Department of General Practice, 2Department of Gastroenterology, Faculdade de Medicina do ABC (ABC Medical School), Santo André, Brazil
Introduction: Although the association between chronic kidney disease and dyspepsia is widely known, it remains poorly investigated. Among the types of gastric inflammation that lead to symptoms, erosive antral gastritis is the most common form. A direct correlation between the urea serum levels and the time in hemodialysis with the onset of gastric metaplasia and dyspepsia can be observed. The aim of this study was to report the endoscopic alterations found in hemodialysis patients.
Methods: This is a cross-sectional study based on the medical records of 95 patients older than 18 years who were diagnosed with chronic kidney disease. The results of endoscopies performed up to 6 months before the beginning of the study were included.
Results: Among the 95 studied patients, 56.84% were male, 60% were Caucasian, and 71.57% used proton pump inhibitors. The endoscopic alteration most frequently observed was erosive gastritis (77% of the cases); however, the frequency of the alteration that caused the symptoms was irrelevant. The antrum was the most common site of involvement (55.79%).
Conclusion: Patients with chronic kidney disease often show dyspeptic symptoms. Other abnormalities are common but are not correlated with such symptoms. In conclusion, this study identified the endoscopic alterations that are most often observed in hemodialysis patients; erosive and enanthematous gastritis were the most common forms observed.
Keywords: hemodialysis, chronic kidney disease, dyspepsia
Introduction
Although the association of chronic kidney disease (CKD) with dyspepsia is widely known, its origin is poorly investigated.1
The concept of dyspepsia has changed in recent decades, and the lack of a consensus on the theme has hindered a complete understanding of its prevalence. Talley defined dyspepsia as discomfort in the upper abdominal area with a structural or biochemical correlation. The absence of such conditions defines the existence of a functional (nonorganic) disorder.2
Endoscopic alterations are common in patients with CKD, especially in those undergoing dialysis treatment. Among such alterations, erosive antral gastritis is the most common form, followed by erosive duodenitis.2,3 A direct correlation between the onset of these alterations and the length of time patients undergo hemodialysis, urea serum levels, and years spent in kidney replacement therapy can also be observed.3
The association between dyspepsia and Helicobacter pylori in patients with CKD suggests a correlation between the onset of the former and the genesis of ulcerous disease. However, the presence of CKD was not identified as a severity factor.4
Patients with CKD have elevated gastrin levels in gastric secretion; however, this is not merely a consequence of the reduction in the clearance of gastrin. There is a compensatory effect caused by the neutralization of gastric juices resulting from an increase in the ammonia levels.1
Peritoneal dialysis patients tend to show more gastrointestinal symptoms (eg, dyspepsia) than hemodialysis patients do.5 Dyspepsia was present in 55% of peritoneal dialysis patients and in only 38% of hemodialysis patients.5
The aim of the current study was to report the endoscopic alterations found in hemodialysis patients.
Methods
This was a cross-sectional study. The project was approved by the Local Ethics Committee (number 067/2011).
Hemodialysis patients with CKD who were older than 18 years were recruited to participate in the study after providing signed informed consent, and the data in their medical records were analyzed. The results of endoscopies performed no more than 6 months before the day of the interview were included in the analysis, and in the absence of such data, a new endoscopy was requested.
The following conditions were considered to be endoscopic alterations for the purposes of clinical correlation: duodenal and gastric ulcer, erosive esophagitis, and acute gastric mucosal injury.
To characterize the CKD, 20 mL of blood was collected before the hemodialysis session so that the creatinine and urea levels could be measured. The samples were processed using the modified Jaffé method for creatinine analysis, and absorbance spectrophotometry for urea analysis. All results were confirmed in duplicate experiments according to good clinical laboratory practices.
There was no calculation of a sample size number, as we intended to include all patients who gave their informed consent. A convenience sample was chosen.
The continuous variables were expressed as the mean and standard deviation, and the categorical variables were expressed as a relative frequency.
Results
A total of 97 patients were included. From that number, two refused to undergo a new endoscopic exam and were therefore excluded from the study, leaving a sample of 95 patients. Table 1 shows the demographic and clinical characteristics of this group of patients, with a higher number of men (56.84%), Caucasians (60%), proton pump inhibitor users (71.57%), and Helicobacter pylori-infected subjects (30.52%).
  | Table 1 Clinical and demographic data of patients (N=95) |
About 82 patients had to perform an endoscopy, as they had not performed one in the last 6 months. Another 13 could retrieve their results from the file records.
Table 2 shows the gastric region in which the endoscopic alterations were found. The most common site of involvement was the antrum (55.79%), followed by the gastric body (28.42%).
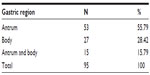  | Table 2 Gastric regions affected |
Table 3 highlights the endoscopic alterations, with erosive gastritis being the most frequent form of the condition (77.08%), followed by enanthematous gastritis (50%). Regarding the endoscopic alterations considered to cause symptoms, a low frequency was observed, with only 4.17% of the cases having gastric ulcer and 14.58% of the cases having erosive esophagitis. There were no cases of acute gastric mucosal injury in this cohort.
  | Table 3 Endoscopic alterations |
Discussion
Patients with CKD receiving dialytic treatment often have dyspepsia and symptoms related to this disorder.1
One of the reasons for this association is the lower clearance of gastrointestinal peptides, such as gastrin, motilin, cholecystokinin, glucagon, substance P, and gastrin-releasing peptide, in patients with CKD.6 Gastrin, motilin and cholecystokinin, and glucagon play essential roles in gastrointestinal motility regulation.6
In patients with angiodysplastic lesions, high blood pressure, coronary insufficiency, and congestive cardiac insufficiency, the risk for digestive bleeding is higher in the event of CKD. This risk can consequently lead to acute gastric mucosal injuries and peptic ulcers.1
Another involved factor is delayed gastric emptying as a result of gastric dysmotility, a disorder that favors the onset of dyspepsia in CKD patients. The predisposition for dysmotility is higher in men than in women, and it is related to differences in the emptying of liquids, solids, and semisolids.6,7
Interestingly, a recent study showed that the worsening of renal function had no correlation with the presence of functional or organic dyspepsia and gastroesophageal reflux disease, as previously hypothesized.8
The prevalence of endoscopic duodenitis is also higher in hemodialysis patients than in those undergoing conservative treatment.9 This finding diverges from the results obtained in the current study, in which we found that the frequency of erosive and enanthematous gastritis was high and the frequency of endoscopic duodenitis was low.
Although such endoscopic alterations were found, they did not exclusively justify the presence of the symptoms by themselves. Abnormalities such as enanthematous gastritis, enanthematous bulboduodenitis, and erosions are common, but they have no correlation with the existence of dyspeptic symptoms.9,10
The finding of the antrum and body regions of the stomach as the main sites of involvement is consistent with the previously studied series.9
Another issue to be accessed is that serum urea levels are not correlated with the duration of CKD but with the progression of the loss of kidney function. In hemodialysis patients, its predialitic levels are correlated with a higher ingest of protein, worse dialysis adequacy, and nutritional status.11
In conclusion, this study has identified the endoscopic alterations that are most frequently observed in hemodialysis patients. Enanthematous and erosive gastritis were the most common forms observed among these patients.
Disclosure
The authors report no conflicts of interest in this work.
References
Ala-Kaila K, Paronen I, Paakkala T. Increased incidence of duodenitis in chronic renal failure. Ann Clin Res. 1988;20(3):154–157. | |
Talley NJ, Vakil NB, Moayyedi P. American gastroenterological association technical review on the evaluation of dyspepsia. Gastroenterology. 2005;129(5):1756–1780. | |
Huang C, Chen Q, Jiang J, Zhang J, Bao B, Yao X. Gastric metaplasia and Helicobacter pylori infection in hemodialysis patients. Ren Fail. 2012;34(4):420–424. | |
Sugimoto M, Yamaoka Y. Review of Helicobacter pylori infection and chronic renal failure. Ther Apher Dial. 2011;15(1):1–9. | |
Strid H, Fjell A, Simrén M, Björnsson ES. Impact of dialysis on gastroesophageal reflux, dyspepsia, and proton pump inhibitor treatment in patients with chronic renal failure. Eur J Gastroenterol Hepatol. 2009;21(2):137–142. | |
Ravelli AM. Gastrointestinal function in chronic renal failure. Pediatr Nephrol. 1995;9(6):756–762. | |
Hirako M, Kamiya T, Misu N, et al. Impaired gastric motility and its relationship to gastrointestinal symptoms in patients with chronic renal failure. J Gastroenterol. 2005;40(12):1116–1122. | |
Bacci MR, Chehter EZ. Dyspepsia among patients with chronic kidney disease: a cross sectional study. Int Arch Med. 2013;6(1):43. | |
Fabbian F, Catalano C, Bordin V, Balbi T, Di Landro D. Esophagogastroduodenoscopy in chronic hemodialysis patients: 2-year clinical experience in a renal unit. Clin Nephrol. 2002;58(1):54–59. | |
Karari EM, Lule GN, McLigeyo SO, Amayo EO. Endoscopic findings and the prevalence of Helicobacter pylori in chronic renal failure patients with dyspepsia. East Afr Med J. 2000;77(8):406–409. | |
Taler SJ, Agarwal R, Bakris GL, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for management of blood pressure in CKD. Am J Kidney Dis. 2013;62(2):201–213. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
