Back to Archived Journals » Patient Intelligence » Volume 8
Empowerment in people with COPD
Authors Disler R, Appleton J, Smith T, Hodson M, Inglis S, Donesky D, Davidson PM
Received 25 May 2015
Accepted for publication 15 October 2015
Published 30 December 2015 Volume 2016:8 Pages 7—20
DOI https://doi.org/10.2147/PI.S61195
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Johnny Chen
Rebecca T Disler,1–3 Jessica Appleton,1 Tracy A Smith,4,5 Matthew Hodson,6 Sally C Inglis,1,2 DorAnne Donesky,7 Patricia M Davidson8
1Faculty of Health, University of Technology Sydney, 2Centre for Cardiovascular and Chronic Care, Faculty of Health, University of Technology Sydney, 3Improving Palliative Care through Clinical Trials (ImPACCT), Sydney, 4Department of Respiratory and Sleep Medicine, Westmead Hospital, Westmead, 5Faculty of Medicine, University of NSW, Sydney, NSW, Australia; 6ACERS, Integrated Medicine and Rehabilitation Services Division, Homerton University Hospital NHS Foundation Trust, London, UK; 7Department of Physiological Nursing, UCSF School of Nursing, San Francisco, CA, 8School of Nursing, Johns Hopkins University, Baltimore, MD, USA
Background: Patient empowerment is recognized as an important aspect of chronic disease management. There is an increasing expectation that health providers engage patients as active participants in their own self-management. This engagement is crucial to the chronic care model as patients with COPD and their families manage the majority of the care in the community. Understanding what influences empowerment will help health care professionals to better engage in collaborative care planning and decision making that meet the needs of this new generation of health consumers.
Aim: The aim of the present study was to identify interventions or approaches that empower patients in the management of COPD.
Methods: An integrative review was undertaken following the preferred reporting items for systematic reviews and meta-analyses approach. Papers were included if they 1) provided a definition or conceptualization of empowerment, and 2) reported interventions or approaches fostering empowerment in patients with COPD. Thematic analysis was used to develop conceptual themes on patient empowerment in COPD. These conceptual themes were validated by a panel of specialists in COPD, chronic disease management, self-management, and patient education.
Results: Literature searching revealed 183 papers of which 15 studies conceptualized or defined empowerment interventions or approaches to support COPD management. These were grouped into the following five categories: pulmonary rehabilitation, social support, web-based interventions, approaches that support knowledge development, and the approach taken by the health care professional.
Conclusion: Pulmonary rehabilitation, knowledge acquisition, social support, telehealth and web-based interfaces, and collaboration with health care professionals empower patients to recognize their own strengths and to manage the impact of the condition. Patients' abilities to direct their own care are additionally influenced by physical debilitation, treatment complexity, economic status, and health literacy. Health care professional–patient relationships must shift to a more collaborative approach that recognizes the patient as an expert in their own condition and facilitates patients to determine their own plan of care and life goals.
Keywords: COPD, chronic disease, empowerment, peer support, telehealth care, self-efficacy, active participation
Introduction
COPD is a common and debilitating condition, with the majority of care being managed by patients and their families in the community.1–4 Patient empowerment, or patients’ ability to determine the approach in one’s own life, is increasingly recognized as an important aspect of chronic disease management.5–8
Empowerment is at times difficult to define and conceptualize. As a process and an outcome, it is best understood within a specific context, for example, within empowerment for chronic disease management in COPD.8 In this context, empowerment is most often conceptualized as a reciprocal relationship between the health professional and the client, in which the client develops skills, knowledge, and confidence to determine the focus of their own health care approach.5,6,8 Four key models of empowerment influence chronic disease literature, such as Funnell et al,9 Dowling et al,8 Powers,10 and Skelton.11 The work by Funnell et al on empowerment in patients from culturally disadvantaged groups with diabetes focuses on empowerment through behavioral change based on the following principles:9
- Affirming that the person is responsible for and in control of daily self-management.
- Educating patients to promote informed decision making rather than adherence/compliance.
- Learning to set behavioral goals so that patients can make changes of their own choice.
- Integrating clinical, psychosocial, and behavioral aspects of self-management.
- Affirming the participants as experts on their own learning needs.
- Affirming the ability of participants to determine an approach to self-management that will work for them.
- Affirming the innate capacity of patients to identify and solve their own problems.
- Respecting cultural, ethnic, and religious beliefs of the target population.
- Creating opportunities for social support.
- Providing ongoing self-management support.9
The model of Dowling et al8 presents a different focus with empowerment based on the patients’ capacity for motivation to change, competence to communicate effectively, knowledge to problem solving, and active participation. While Dowling et al8 argue strongly that these are positive and worthy causes, as a bystander, these still appear to imply that success is measured on patients’ ability to comply and be competent in health professional defined behavioral changes, rather than empowerment through goals that meet self-determined priorities.8 Skelton11 alludes to this in arguing that often behind the notion of empowerment “lurks an older view that ‘the professional knows best”’. This claim is also implied by Powers10 who argues that empowerment is often a strategy employed by one person over the another, and in health care, patients are only considered as empowered “if and only if they make correct choices as defined by the health care provider”. In this view of empowerment, health care professionals prescribe those parameters of behavioral change that are required for success.
In chronic disease literature, empowerment is commonly used interchangeably with self-management, active participation, or self-efficacy;8,12 however, empowerment distinctly emphasizes self-determination.12 Nonetheless, patients who are empowered are likely to have greater self-efficacy for self-management, known in COPD to improve symptom control, slow disease progression, and health-related quality of life.13,14
Traditional models of health care delivery have focused on the health care professional as the authoritative figure, with an obligation on the part of the patient to comply and adhere to therapeutic goals prescribed by this expert.6 There is growing recognition, in chronic disease in particular, that patients should be supported as collaborative decision makers and empowered to determine the approach in one’s own life, and therefore, their individual needs and priorities in health care.6,12,15–17 This shift in perspective challenges health care professionals to relinquish the authoritative role in place of an equal partnership.6
Research questions
This review sought to describe those interventions or approaches that empower patients in the management of COPD. Understanding what influences empowerment will help health professionals to support patients in collaborative decision making.18–20
Specific questions asked in the review are as follows:
- What interventions or approaches empower patients in the management of COPD?
- What key factors support empowerment in this patient group?
- How do current clinical relationships facilitate empowerment in this patient group?
Method
An integrative approach following the preferred reporting items for systematic reviews and meta-analyses (PRISMA) approach21 was used to understand the empirical and theoretical literature on patient empowerment in COPD.22 This approach is particularly useful in undertaking a structured approach to a review of literature, while identifying the conceptual themes that contribute to the field of work.22
Eligibility criteria
Papers were included if they were published in peer reviewed journals, written in the English language, and published between 1995 and 31 March 2015. Papers written prior to 1995 were excluded to ensure consistency with current clinical approaches.
Papers were included if they discussed interventions or approaches that are related to the development of empowerment in patients with COPD, and if they presented a definition of empowerment. Some papers did not always present a definition but did conceptualize empowerment in their discussion or approach, these papers were also included. Original research papers, systematic reviews, and reviews were considered. Opinion pieces and case studies were excluded from this review.
Information sources
The electronic databases MEDLINE, PsycINFO, CINAHL, and Google Scholar were searched using medical subject headings and keywords. Table 1 outlines the MEDLINE Ovid search strategy; this was translated into all other databases. The search terms and strategy were reviewed by a health informatics expert with the following appropriate derivatives used: “chronic obstructive pulmonary disease”, “chronic obstructive airways disease”, “COPD” OR “COAD”, and “empowerment” OR “power” OR “empower” OR “patient participation” OR “patient driven” OR “active participation”. The World Wide Web was searched using Google Scholar and Google search engine for related electronic documents. Journals held locally were hand searched for relevant articles.
  | Table 1 Example search strategy (MEDLINE Ovid) |
Study selection
Papers were assessed for eligibility for inclusion by two independent investigators (RTD and JA) with consensus gained from a third independent investigator as necessary (DAD).
Data collection process
Data were extracted by a single investigator using a structured data extraction table (JA), and accuracy of data was verified by an independent investigator (RTD). The data extraction table included author details, journal details, methodological approach, data utilized and data sources, any statement about empowerment, definition or conceptualization of empowerment, summary of findings, and conclusion.
Data analysis
Thematic analysis was used to develop conceptual themes on patient empowerment in COPD.22 These conceptual themes were validated by a panel of specialists in COPD, chronic disease management, self-management, and patient education (RTD, DAD, SCI, and MH).
Results
Literature searching revealed 183 papers of which 82 met the inclusion criteria on title and abstract review (Figure 1). A further 67 were excluded after full-text review: 59 did not conceptualize or define empowerment, four included other diagnoses from which COPD responses could not be deciphered, and four were case studies or opinion pieces.
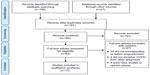  | Figure 1 PRISM flow diagram. |
A total of 15 papers were included in the review and reported on eleven different studies23–26 (two papers reported on one study27,28), two literature reviews8,29 and one was a discussion paper (Table 2).30 Ten of the studies were qualitative, including five interview studies, four focus group studies, and one using online data collection. One study was quantitative, using a quasi-experimental with matched control design and used a quantitative measure of empowerment.23 Three of the qualitative studies were nested within large randomized controlled trials.24–26 Papers were presented from the following countries and regions: Continental Europe,29,31 UK and Republicof Ireland,8,24,25,30–32 Scandinavia,26–28,31,33 Australia,34,35 Canada,23 Russia,31 People’s Republic of China (Hong Kong),31 Brazil,29 and Iran.36 The strong representation from the Western world, with exception to the USA, may influence an individualized view of empowerment and self-management.14 A summary of the included studies can be found in Table 2.
Results from review of literature
The following interventions or approaches were assessed as contributing to empowerment in COPD: pulmonary rehabilitation, social support, approaches that support knowledge development, telemonitoring and web-based interventions, and the knowledge and attitude of the health care professional (Table 3).
  | Table 3 Interventions or approaches that support patient empowerment in COPD |
Pulmonary rehabilitation
Pulmonary rehabilitation is a cornerstone of COPD management and is “an evidence-based, multidisciplinary, and comprehensive intervention”37 framed within the chronic care model.38 This multimodal approach includes exercise, self-management education, and behavioral components in an individualized plan designed to “reduce symptoms, optimize functional status, increase participation, and reduce health care costs”.37 Five studies (six papers) explored pulmonary rehabilitation as a key intervention in promoting empowerment, both overtly as an underlying framework and inadvertently as part of increasing patients’ self-determination and confidence for engaging in activities of life.8,24,29,32–34
The Pulmonary Rehabilitation In Nurse-led Community Environments (PRINCE) study is a 5-year, two-armed randomized controlled study, clustered by general physician practice, in which participants either received Structured Education Pulmonary Rehabilitation Program (SEPRP) or usual care.8,24 As part of this trial, the authors developed a model of empowerment in chronic illness as part of their initial concept analysis and also discussed empowerment in reporting the study outcomes.8,24 The program used the transtheoretical model of behavioral change. Qualitative interviews with 16 patient participants with COPD revealed themes of a complex balance between treatment activities and retaining a life they wanted, adapting living to the limitations of breathlessness, and learning coping strategies to maintain independence. Having knowledge and knowing when to escalate treatment and access supports was a strong theme, as was having access to help to facilitate decision making. The SEPRP was noted to have changed patients’ attitudes to their disease with feelings of increased control and positive outlook.24 A qualitative study on pulmonary rehabilitation experience by Denn32 similarly noted that patients were empowered through increased physical confidence and in learning to cope with and accept their condition.
A study by Hellem et al33 also used the transtheoretical model of behavioral change in their qualitative study exploring COPD patients’ perceptions of the elements for success in an exercise maintenance program. The approach taken focused on health and beneficial change rather than disease cause and on recognizing patient strengths and ability for adjustment.33 A key to empowerment was the physiotherapists’ knowledge and ability to tailor the program to individuals’ capabilities so that patients felt safe in this context and able to “exert themselves close to their limit”. This was elucidated in the theme “the personal manner and empowering skills of the therapist” in which the patient felt recognized, valued, and taken seriously. The theme “regular appointments with someone who cares” additionally raised the importance of having a regular agreed time and an environment where they felt valued and part of a group. Negative experiences equally led patients to disengage.33
Milne et al34 in their qualitative study exploring hope in patients following a home exercise program did not overtly target empowerment. However, their qualitative research undertaken after the program identified “hope through empowerment” as a key theme. This was related to increased self-confidence in their ability to cope and manage their breathlessness and therefore be able to live a normal life. Patients were able to manage the impact of their condition on their day-to-day life through knowledge of what COPD was and how to pace activities and use coping strategies. Coping mechanisms, in particular, were seen to give back self-control and self-determination. An important element of empowerment is in the ability for people to keep doing those things that they enjoy in life. Participants in the Milne et al34 study were facilitated to learn how to adapt their hopes into achievable self-determined goals such as spending time with grandchildren and walking to the park. Increased confidence “in coping with episodes of breathlessness resulted in them feeling empowered, this in turn increased participants” hope to be able to enjoy a more “normal life”.35 Access to a more normal life was similarly highlighted in the PRINCE study.24
The positive benefits of self-determined, tailored goals of care were also raised in the systematic review of eight qualitative research studies on patient experience in pulmonary rehabilitation by de Sousa Pinto et al.29 Being able to take back the control of life, not only in increased physical capability and mechanisms to cope with day-to-day symptoms but also in the confidence to interpret symptoms and take a course of action and seek help when necessary.29 Increased hope for the future was also a key to the empowerment outcome, with patients being provided with the resources and mechanisms to overcome and deal with barriers, thereby facilitating a positive outlook of a future in which the condition of the impact is managed.29 Pulmonary rehabilitation, in particular, the support and education provided, facilitates “…the development of patients’ empowerment”.29
Empowerment through provided social support
Peer and social support has long been recognized as an important factor in the quality of life and self-management in COPD,39,40 in addition to the emerging online peer support mentioned later. Empowerment through peer support was identified in three studies and one literature review looking at pulmonary rehabilitation.29,32–34 The exercise maintenance program by Hellem et al33 reported that the identification with peers gave patients a sense of normalcy that allowed them to engage freely in their activities without feeling the need to hide their symptoms. Peer support and friendship in the exercise group were noted as markedly more important as a motivational factor than family and friends.33 Similarly, in the focus group study by Denn,32 patients often found their condition isolating and feeling embarrassed to show breathlessness in social settings. Participants in this study expressed a sense of relief and ease at exercising with others who experienced the same condition. The systematic review of de Sousa Pinto et al29 similarly noted that patients felt able to express feelings and thoughts without recrimination or judgment during the group exercise. In the qualitative study by Milne et al,34 social support through a variety of relationships, including health professionals, was identified as a crucial element in the maintenance and development of hope for the future. Relationships with friends and family were felt to encourage and motivate patients through increased sense of self-worth. While it is recognized that the social support from these studies was experienced within the context of pulmonary rehabilitation, the social interaction activity was highlighted specially as an important aspect of empowerment.
Approaches that support knowledge development
Knowledge development is recognized as a key factor that enables patients to make educated decisions about their care as part of collaborative decision making. While there were no studies that explored education as a sole intervention to improve empowerment, development of knowledge was raised as a key element in the pulmonary rehabilitation studies noted previously.8,24,29,34 The PRINCE study24 noted earlier raised the importance of developing knowledge as a key to empowerment, with specific knowledge of coping strategies that assisted patients to manage their condition to achieve the life they wanted.24 Such knowledge also assisted patients to make informed decisions without panic, including knowing when to escalate treatment and access supports.24 Knowledge was an important aspect of the SEPRP in changing patients’ attitudes to their disease, with feelings of increased control and positive outlook.24 Knowledge was also noted as a facilitator to active decision making and improved self-confidence found in the theme “hope through empowerment” in the qualitative study by Milne et al.34 Similarly, Fairbrother et al25 also noted that increased “knowledge and empowerment” was a key theme in patients being able to determine how they interpreted and responded to condition changes, and therefore, their ability to be active participants in their own care and life management.
Tele- and web-based interfaces
Tele- and web-based interfaces are increasingly recognized as vehicles to deliver information and promote patient engagement and peer interaction.15,41,42 Limited literature was found that explored tele- and web-based interfaces with reference to empowerment in COPD directly, with three studies exploring telemonitoring25,27,28 and one study exploring empowerment through online chat rooms.29,30
The telemonitoring study by Huniche et al26 explored an integrated health care system for patients with COPD in which patients received a home telemonitoring, as well as home-based exercise prescription, and provision of a pedometer and Wii console.26 Their study conceptualized empowerment as based in social action and self-help, with a renewed focus on patient perspectives of their goals in everyday life.26 Some patients used telemonitoring measurements to temper daily activities and in deciding whether to seek help from a health professional.26 Huniche et al26 noted that patients felt “grateful for the easy and legitimate access to specialized health professionals” and reassured in knowing that their condition fluctuation was being monitored.
Fairbrother et al25 similarly implemented a telemonitoring intervention for COPD in which patients entered symptom and oximetry scores into the system, as well as having access to telephone and home visits from a community respiratory team. In the post-randomized controlled trial qualitative study, participants voiced that the intervention provided them, for the first time, access to clinical data about their condition, which is crucial for collaborative decision making.25 Access to this data allowed the patients to learn to recognize their normal symptoms, thereby increasing their confidence to undertake day-to-day activities and validation of their decisions to escalate treatment when unwell.25 The participants, both patients and nurses, valued these tools as contributing to patient empowerment.25 Sicotte et al23 also reported a prospective interventional study that compared telemonitoring and telephone support with traditional homecare and found that empowerment, measured using quantitative questionnaire, was high in both the experimental and the comparison groups following the trial. Those receiving telemonitoring increased their use of consultations and phone calls for advice over the period.23
Health care professionals in two of these telemonitoring trials23,25 raised concerns that the increased interaction with health care professionals was an indicator of fixation and increased dependence. However, a health care professional raising this issue also noted that one patient had substantially dropped acute service utilization, only having been admitted once in 12 months over the duration of the telemonitoring intervention.25 Additionally, patients in the same study noted that increased access to advice meant that they consulted earlier in deterioration and were more likely to start newly prescribed treatments, whereas previously they would have waited until condition deterioration warranted contact with health services to raise ongoing issues.25 Increased consultation dependence through telemonitoring could in fact be reinterpreted as increased engagement in collaborative decision making. An argument supported by Huniche et al,26 who support home telemonitoring as a promising approach to provide accurate and reliable data, enables patient to better manage their lives.26
Peer support through online social media groups has been increasingly recognized to improve social well-being, enhance self-management and self-efficacy, and provide a sense of belonging and normalcy across many chronic diseases.15–17,43–47 Only the Danish study by Wentzer and Bygholm27,28 explored empowerment specifically in COPD through online peer support. This study undertook a text analysis of discussion posts from an online COPD peer group. The main activities in the COPD group were knowledge sharing and shared experience and recognition, with sharing typically focused on smoking, exercise and coping techniques, and also more existential discussions of the burden of disease and challenges faced in dealing with COPD impact. Interestingly, while the authors noted that individuals experienced empowerment through this sharing, there remained a tone of compliance with participants reaffirming health care professional recommendations;27,28 however, self-determination and engaging with health professionals recommendations should not be viewed as mutually exclusive.
Knowledge and attitude of the health care professional
Training of health care professionals, in particular, approaches that encourage patient empowerment and self-determination, were also raised as important. A study by Robinson et al35 trained community-based nurses to use the transtheoretical model of behavioral change to promote self-management through motivational interviewing with patients with COPD. The qualitative study exploring the nurses’ experiences found that there was a shift in the nurses’ approach from a fatalistic and prescriptive to a patient-centered, facilitative, and consultative approach determined by the life goals set by the client.35 Patients interpreted as noncompliant, depressed, and not willing to listen were recognized as facing an unpredictable and unrelenting condition, with nurses then changing their focus to “do the best they can every day”.35 In the PRINCE study, there was a noted shift to a more collaborative relationship between patients and health care professionals, both in the programs ability to tailor activities to the need of the patient and in patients feeling empowered to ask their health professionals outside the program questions that are important to them.24 A similar approach, solution focused brief therapy, is described in the discussion piece of Smith and Kirkpatrick.30 This framework is designed to guide patients to consider self-determined positive futures and life desires with a focus on inherent patient strengths and wellness rather than pathology. Through this technique, patients are helped to see that change, and adaptation is possible, no matter what the symptom burden is.30 Health care professionals were trained to adopt a position of “not knowing” with the patient as the expert and to avoid judgment and censure of patients for nonadherence, preferring to focus on a positive vision of change in the future.30
The influence of the health professional’s approach was again raised in the multinational qualitative study by Davies et al.31 This study does not present an intervention but rather clinicians’ views on self-management of COPD exacerbation through at home rescue packs of antibiotics and steroids and empowerment as one possible outcome from this. From the comments of the clinicians, there was an acknowledgment that having medication at home might provide a sense of control over acute events and improve early treatment when access to health services was limited, but that this was only appropriate in a particular cohort of patients.31 A mutually trusting relationship between the patient and the clinician was a factor in whether this opportunity would be given to patients, as was the viewpoint of the individual clinician, with some participants believing that antibiotics and steroids should never be used as a home-based rescue pack, and rather a consultation with the prescribing clinician is required. Time for adequate education was also raised as a barrier, with clinicians commenting that it was easier to have the patient make contact with them than to provide a rescue pack with detailed education for the patient to use at home. As noted by the authors, while these concerns are sound, they undermine the intent of self-management interventions to provide the patient with the knowledge, skill, and tools to manage symptoms, both acute and long term, and improve confidence in decision making. The authors further state that “There appears to be a gap between what is seen as a self-management intervention in the literature and what is available or actually implemented in routine care”.31
The qualitative study by Milne et al34 noted that positive relationships with health professionals, doctors in this case, had a marked impact on patients’ hopes around their illness. Additionally, comfort was gained from the perception that the health professional understood the impact of the illness and given time for the patients to talk about their illness.34 Negative relationships equally made patients feel isolated, unimportant, and with little hope for the future. Trust in health care providers was raised as a key theme in the qualitative study by Fotoukian et al36 on the barriers and facilitators to empowerment in older Iranian patients with COPD. Positive relationships with health care professionals both endorsed the care provided and motivated patients to engage in treatment activities. Conversely, other participants noted that some health professionals did not appear to see empowerment, or the facilitation of self-management, as part of their role, and viewed this as an extra responsibility. It was voiced that the training of health professionals was required to enable them to support patients in collaborative condition management.36
Discussion
In recognizing the patient’s empowerment as an important aspect of chronic disease management, this review sought to describe those interventions or approaches that sought to empower patients in the management of their COPD. Understanding what interventions or approaches facilitate empowerment and what influences patients ability to engage in care planning will help health professionals to better engage in collaborative care planning and to focus on their patients’ individual care priorities.
Key findings
The review included 15 papers that conceptualized or defined empowerment as part of interventions or approaches to support COPD management and were grouped into the following five categories: pulmonary rehabilitation, approaches that support knowledge development, social support, web-based interventions, and the knowledge and attitude of the health care professional.
Pulmonary rehabilitation is recognized as a cornerstone of COPD management and was similarly found through this review to be an important approach and consistent theme in promoting patient empowerment.8,24,29,32–34 The focus on increased function, coping strategies, and knowledge within this multimodal, individualized approach is closely aligned with empowerment literature.5–8,24,29,32–34,37 Empowerment through self-determination was increased in pulmonary rehabilitation through tailoring treatment approaches to the patients’ own life goals and in increasing disease-specific knowledge necessary for collaborative decision making.29,32,33 Development of coping strategies and increased confidence similarly allowed patients to manage the impact of their condition, thereby increasing social engagement and a positive outlook for the future.8,24,29,32–34
Knowledge development was also a key factor in patient empowerment throughout the discussions in the literature.8,24,29,34 No studies explored education as a sole intervention, a likely finding given chronic disease management literature has long acknowledged the need for multimodal interventions that include a behavioral component in addition to education.48–50 It is difficult to elucidate the distinct impact of education alone, for example, in the context of pulmonary rehabilitation goal setting and psychological coaching. However, knowledge development is acknowledged as essential in patients’ abilities to interpret treatment approaches when engaging in collaborative decision making8,24,29,34 and to respond to the change in condition.8,24,29,34,51 Knowledge is integral to self-management and empowerment and should be viewed as something that develops through interactions with health care professionals and through the experience of living with their disease.8,24,29,34
A focus on a normal life and strength instead of pathology
Patients’ ability to influence the approach to their COPD care is influenced by their physical debilitation, the complexity and unpredictable trajectory of COPD, the complexity of associated treatments, the lack of economic status to access necessary supports, and the lack of health literacy and COPD-specific knowledge.36 Several interventions or approaches sought to focus on wellness, patient strength, and beneficial change, rather than the disease cause, using the transtheoretical model of behavioral change or focused brief therapy.24,30,33,52 Patients were facilitated to consider possible positive futures and empowered to speak about their life desires.24,30,33,52 In focusing on strengths, rather than pathology, patients recognized their natural strength and own capacity for adjustment, no matter what the symptom burden is. Adjusting the health care professional position to not knowing promoted a sense of power for patients to participate in collaborative decision making.24,30,33,52
A consistent theme throughout the review was facilitating patients to access a normal life and gain back self-control and self-determination to keep doing those things that brought joy to life, such as spending time with grandchildren.24,30,34 Coping strategies learnt during pulmonary rehabilitation were essential in managing the impact of breathlessness,24,34 and both pulmonary rehabilitation and motivational interviewing were reported to facilitate patients to adapt previously unattainable hopes into achievable, self-determined goals.24,30,34
Telehealth care and web-based interventions
Tele- and web-based interfaces are increasingly recognized as vehicles to deliver information and promote patient engagement and peer interaction.15,41 Telehealth care has been shown to significantly increase the quality of life and reduce emergency department presentations in chronic disease53,54 and has the potential to provide patients with accurate and reliable data that would enable them to better manage the impact of the disease.25,26 All the studies included in this review noted an increase in the interaction with health care professionals when telemonitoring interventions were in place.23,25,26 Access to clinical data allowed the patients to learn to interpret daily fluctuations in symptoms and validated decisions to escalate treatment when unwell.25,26 A key benefit of telemonitoring was that the ongoing monitoring gave patients a legitimate reason to connect with health care professionals outside of acute events, allowing for discussion on ongoing issues.25,26 Health care professionals would never deem to make clinically based decisions without clear knowledge of the current condition, yet, patients are often required to engage in sage and appropriate decision making without the same privilege. Concerns raised over the increased dependency on telemonitoring access could also be reinterpreted as increased engagement in collaborative decision making, particularly in the context of reported reduced utilization of acute and emergency services in these studies.25,27 While there is evidence that patients find telemonitoring useful, the economic utility of this change in approach remains unclear.55,56
Online peer support groups are recognized to improve social well-being, enhance self-management and self-efficacy, and provide a sense of belonging and normalcy across many chronic diseases.15–17,43–47 Social support through a variety of relationships, including health professionals, was identified as a crucial element in the maintenance and development of hope.34 Web-based interfaces will be an increasing adjunct to traditional face-to-face supports in the future,16–18,49 suggesting an increased need for health professionals and health care services to participate in care delivered via this medium.
Defining empowerment in COPD
The term empowerment is commonly used interchangeably with self-management and self-care in discussing patients’ involvement and decision making about their condition.7 However, patient empowerment is distinctly different from self-management in that it additionally reflects self-determination about one’s own care and future and recognizes that “knowing about an illness is not the same as knowing about a person’s life and that, by default, patients are the primary decision-makers”.6
Some might argue that increased confidence in the ability to manage COPD is in itself empowerment and would have a strong argument as described by Hellem et al “a strong sense of self-efficacy facilitates perseverance in efforts toward success”.33 Thereby, enabling patients to exert influence over their situation. However, in many current approaches, the emphasis remains on patients’ confidence to adhere to health care professional mandated tasks, rather than true self-determination related to patient-defined life goals. The complexity of the definition and overlap in conceptualization of this term, with other key concepts, may in itself be one of the barriers to implement patient empowerment strategies.
Implications for practice
One of the findings of this review has been that health professionals have an important role in supporting empowerment through informed and collaborative decision making, a finding consistent within the broader literature.6,27,28,57 Historically, health care professionals have occupied a position as the authoritative figure,6 with patients required to comply with prescribed therapeutic goals to be considered as successful self-managers.6
Empowering patients to determine the approach and priorities in their own care requires a shift in patient–health care professional to allow for shared authority with their expert patients.7,57 In doing this, the success is redefined “by the relationships they create with their patients, as well as outcomes achieved by their patients” in relation to patient-determined goals.6 This collaborative approach translates to a marked shift from patients being assessed on their ability to make correct decisions that fit in with a health professional’s defined plan of care to patients making decisions that align with their own goals and needs.27,28
It should be noted that empowerment and engagement with health care professional recommendations are not mutually exclusive, but rather patients should be empowered to make informed decisions about their own lives with relevance to their own life goals.
Limitations
The conceptualization and definition of empowerment are not without conflict. Several papers did not overtly define empowerment; however, it was felt that they did conceptualize or address empowerment in their approach. The inclusion of such papers did rely on the interpretation of the two independent investigators; however, this is consistent with data extract processes, and all conceptual themes were validated by a panel of specialists in COPD, chronic disease management, self-management, and patient education (RTD, DAD, SCI, and MH).
Few studies assessed the extent to which the interventions or approaches were successful at promoting patient empowerment. While empowerment is an important aspect of self-management of chronic disease, it is infrequently the focus of interventions or approaches to COPD care and is less frequently still assessed as an outcome. A further limitation is that there is an assumption that empowerment is always positive in patient care, which may not be the case for all people.
Future research should explore how interventions or approaches can better engage patients in self-determination of care and life goals and how training can facilitate health care professionals in undertaking more collaborative and consultative approaches to patient care.
Conclusion
Pulmonary rehabilitation, knowledge acquisition, social support, and collaboration with health care professionals empower patients to recognize their own strengths and to manage impact of the condition. Patients’ abilities to direct their own care are additionally influenced by physical debilitation, treatment complexity, economic status, and health literacy. Health care professional–patient relationships must shift to a more collaborative approach that recognizes the patient as an expert in their own condition and facilitates patients to determine their own plan of care and life goals.
Disclosure
The authors report no conflicts of interest in this work.
References
Clark NM, Dodge JA, Partridge MR, Martinez FJ. Focusing on outcomes: making the most of COPD interventions. Int J Chron Obstruct Pulmon Dis. 2009;4:61–77. | |
Kralik D, Koch T, Price K, Howard N. Chronic illness self-management, taking action to create order. J Clin Nurs. 2004;13(2):259–267. | |
Koch T, Jenkin P, Kralik D. Chronic illness self-management, locating the ‘self’. J Adv Nurs. 2004;48(5):484–492. | |
Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. | |
Fotoukian Z, Shahboulaghi FM, Khoshknab MF, Mohammadi E. Concept analysis of empowerment in old people with chronic diseases using a hybrid model. Asian Nurs Res. 2014;8(2):118–127. | |
Funnell MM, Anderson RM. Empowerment and self-management of diabetes. Clin Diabetes. 2004;22(3):123–127. | |
Scambler S, Newton P, Asimakopoulou K. The context of empowerment and self-care within the field of diabetes. Health. 2014; 18(6):545–560. | |
Dowling M, Murphy K, Cooney A, Casey D. A concept analysis of empowerment in chronic illness from the perspective of the nurse and the client living with chronic obstructive pulmonary disease. J Nurs Healthc Chronic Illn. 2011;3(4):476–487. | |
Funnell MM, Nwankwo R, Gillard ML, Anderson RM, Tang TS. Implementing an empowerment-based diabetes self-management education program. Diabetes Educ. 2005;31(1):53–61. | |
Powers P. Empowerment as treatment and the role of health professionals. Adv Nurs Sci. 2003;26(3):227–237. | |
Skelton R. Nursing and empowerment: concepts and strategies. J Adv Nurs. 1994;19(3):415–423. | |
Aujoulat I, d’Hoore W, Deccache A. Patient empowerment in theory and practice: polysemy or cacophony? Patient Educ Couns. 2007; 66(1):13–20. | |
Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2015. Available from: http://www.goldcopd.org/. Accessed November 17, 2015. | |
Disler R, Gallagher R, Davidson P. Factors influencing self-management in chronic obstructive pulmonary disease: an integrative review. Int J Nurs Stud. 2012;49(2):230–242. | |
Van Uden-Kraan CF, Drossaert CH, Taal E, Seydel ER, van de Laar MA. Participation in online patient support groups endorses patients’ empowerment. Patient Educ Couns. 2009;74(1):61–69. | |
Wicks P, Massagli M, Frost J, et al. Sharing health data for better outcomes on PatientsLikeMe. J Med Internet Res. 2010; 12(2):e19. | |
Mo PK, Coulson NS. Developing a model for online support group use, empowering processes and psychosocial outcomes for individuals living with HIV/AIDS. Psychol Health. 2012;27(4):445–459. | |
Bourbeau J. Clinical decision processes and patient engagement in self-management. Dis Manage Health Outcomes. 2008;16(5):327–333. | |
Bourbeau J, Nault D, Dang-Tan T. Self-management and behaviour modification in COPD. Patient Educ Couns. 2004;52(3):271–277. | |
Gysels M, Higginson I. Self-management for breathlessness in COPD: the role of pulmonary rehabilitation. Chron Respir Dis. 2009; 6(3):133–140. | |
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. | |
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–553. | |
Sicotte C, Pare G, Morin S, Potvin J, Moreault M-P. Effects of home telemonitoring to support improved care for chronic obstructive pulmonary diseases. Telemed J E Health. 2011;17(2):95–103. | |
Casey D, Murphy K, Cooney A, Mee L. Developing a structured education programme for clients with COPD. Br J Community Nurs. 2011; 16(5):231–237. | |
Fairbrother P, Pinnock H, Hanley J, et al. Exploring telemonitoring and self-management by patients with chronic obstructive pulmonary disease: a qualitative study embedded in a randomized controlled trial. Patient Educ Couns. 2013;93(3):403–410. | |
Huniche L, Dinesen B, Grann O, Toft E, Nielsen C. Empowering patients with COPD using tele-homecare technology. Stud Health Technol Inform. 2010;155:48–54. | |
Wentzer HS, Bygholm A. Narratives of empowerment and compliance: studies of communication in online patient support groups. Int J Med Inform. 2013;82(12):e386–e394. | |
Wentzer H, Bygholm A. Compliance or patient empowerment in online communities: reformation of health care services? Stud Health Technol Inform. 2010;157:141–147. | |
de Sousa Pinto JM, Martin-Nogueras AM, Morano MTAP, Macedo TEPM, Arenillas JIC, Troosters T. Chronic obstructive pulmonary disease patients’ experience with pulmonary rehabilitation: a systematic review of qualitative research. Chron Respir Dis. 2013;10(3):141–157. | |
Smith S, Kirkpatrick P. Use of solution-focused brief therapy to enhance therapeutic communication in patients with COPD. Prim Health Care. 2013;23(10):27–32. | |
Davies F, Risør MB, Melbye H, et al. Primary and secondary care clinicians’ views on self-treatment of COPD exacerbations: a multinational qualitative study. Patient Educ Couns. 2014;96(2):256–263. | |
Denn D. Patient experiences of pulmonary rehabilitation programmes. Nurs Times. 2008;104(20):32–40. | |
Hellem E, Bruusgaard KA, Bergland A. Exercise maintenance: COPD patients’ perception and perspectives on elements of success in sustaining long-term exercise. Physiother Theory Pract. 2012; 28(3):206–220. | |
Milne L, Moyle W, Cooke M. Hope: a construct central to living with chronic obstructive pulmonary disease. Int J Older People Nurs. 2009; 4(4):299–306. | |
Robinson A, Courtney-Pratt H, Lea E, et al. Transforming clinical practice amongst community nurses: mentoring for COPD patient self-management. J Clin Nurs. 2008;17(11c):370–379. | |
Fotoukian Z, Mohammadi Shahboulaghi F, Fallahi Khoshknab M, Mohammadi E. Barriers to and factors facilitating empowerment in elderly with COPD. Med J Islam Repub Iran. 2014;28:155. | |
Nici L, Donner C, Wouters E. American thoracic society/european respiratory society statement on pulmonary rehabilitation. Am J Crit Care Med. 2006;173:1390–1413. | |
World Health Organization. Innovative Care for Chronic Conditions: Building Blocks for Actions: Global Report. Geneva: World Health Organization; 2002. | |
Alberto J, Joyner B. Hope, optimism, and self-care among better breathers support group members with chronic obstructive pulmonary disease. Appl Nurs Res. 2008;21(4):212–217. | |
Halding AG, Heggdal K. Patients’ experiences of health transitions in pulmonary rehabilitation. Nurs Inq. 2012;19(4):345–356. | |
Barak A, Boniel-Nissim M, Suler J. Fostering empowerment in online support groups. Comput Human Behav. 2008;24(5):1867–1883. | |
Bartlett YK, Coulson NS. An investigation into the empowerment effects of using online support groups and how this affects health professional/patient communication. Patient Educ Couns. 2011;83(1):113–119. | |
Chung JE. Social networking in online support groups for health: how online social networking benefits patients. J Health Commun. 2014;19(6):639–659. | |
Nguyen H, Carrieri-Kohlman V, Rankin S, Slaughter R, Stulbarg M. Is internet-based support for dyspnea self-management in patients with chronic obstructive pulmonary disease possible? Results of a pilot study. Heart Lung. 2005;31(1):51–62. | |
Nguyen H, Donesky-Cuenco D, Wolpin S, Paul S, Carrieri-Kohlman V. Randomized controlled trial of an internet-based versus face-to-face dyspnea self-management program for patients with chronic obstructive pulmonary disease: pilot study. J Med Internet Res. 2008;10(2):e9. | |
Nguyen H, Gill D, Wolpin S, Steele B, Benditt J. Pilot study of a cell phone-based exercise persistence intervention post-rehabilitation in COPD. Int J Chron Obstruct Pulmon Dis. 2009;4:1–13. | |
Nguyen HQ, Donesky D, Reinke LF, et al. Internet-based dyspnea self-management support for patients with chronic obstructive pulmonary disease. J Pain Symptom Manage. 2013;46(1):43–55. | |
Sassi-Dambron DE, Eakin EG, Ries AL, Kaplan RM. Treatment of dyspnea in COPD: a controlled clinical trial of dyspnea management strategies. Chest. 1995;107(3):724–729. | |
Scherer YK, Schmieder LE, Shimmel S. The effects of education alone and in combination with pulmonary rehabilitation on self-efficacy in patients with COPD. Rehabil Nurs. 1998;23(2):71–77. | |
Zimmerman BW, Brown ST, Bowman JMA. Self-management program for chronic obstructive pulmonary disease: relationship to dyspnea and self-efficacy. Rehabil Nurs. 1996;21(5):253–257. | |
McDonald VM, Higgins I, Gibson PG. Insight into older peoples’ healthcare experiences with managing COPD, asthma, and asthma–COPD overlap. J Asthma. 2013;50(5):497–504. | |
Crawford Shearer NB, Reed PG. Empowerment: reformulation of a non-Rogerian concept. Nurs Sci Q. 2004;17(3):253–259. | |
Polisena J, Tran K, Cimon K, et al. Home telehealth for chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Telemed Telecare. 2010;16(3):120–127. | |
McLean S, Nurmatov U, Liu Joseph LY, Pagliari C, Car J, Sheikh A. Telehealthcare for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2011;7:CD007718. | |
Ure J, Pinnock H, Hanley J, et al. Piloting tele-monitoring in COPD: a mixed methods exploration of issues in design and implementation. Prim Care Respir J. 2012;21(1):57–64. | |
Nasr N, Mawson S, Mountain G. A realist evaluation of a self-management technology. Gerontechnology. 2012;11(2):235. | |
Ljungdalh AK, Moller JE. The social in medicine: social techniques in patient education. Health. 2012;16(4):418–433. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

