Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
Emergency department management of acute exacerbations of chronic obstructive pulmonary disease: factors predicting readmission
Authors Bartels W , Adamson SL, Leung L, Sin DD , van Eeden SF
Received 20 January 2018
Accepted for publication 19 March 2018
Published 23 May 2018 Volume 2018:13 Pages 1647—1654
DOI https://doi.org/10.2147/COPD.S163250
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Wiebke Bartels, Simon Adamson, Lisa Leung, Don D Sin, Stephan F van Eeden
Centre for Heart Lung Innovation, Department of Medicine, University of British Columbia, Vancouver, BC, Canada
Rationale: Readmissions are common following acute exacerbations of chronic obstructive pulmonary disease (AECOPD) and are partially responsible for increased morbidity and mortality in COPD. Numerous factors have been shown to predict readmission of patients previously admitted to hospital for AECOPD; however, factors related to readmission in patients who are triaged in emergency departments (EDs) and sent directly home are poorly understood. We postulate that patients seen in the ED for AECOPD and directly sent home have a high readmission rate, and we suspect that inadequate management and follow-up contribute to this high readmission rate.
Methods: We conducted a 1-year retrospective study of all patients seen in the ED for AECOPD at an inner-city tertiary care hospital; 30- and 90-day readmission rates for COPD and all-cause admissions to the ED and hospital were determined. Patients discharged directly home from the ED were compared with those admitted to hospital for management. Patient, treatment, and system variables that could potentially impact readmission were documented. Multivariate Poisson regression models were used to determine which factors predicted readmissions.
Results: The readmission rates in the ED group (n=240) were significantly higher than that in the hospitalized group (n=271): 1) the 90-day ED readmissions (1.29 vs 0.51, p<0.0001) and 30-day ED readmissions (0.54 vs 0.20, p<0.0001) (ED vs hospitalized groups) were significantly higher in the ED group; 2) the time to first readmission was significantly shorter in the ED group than in the hospitalized group (24.1±22 vs 31.8±27.8 days; p<0.05). Cardiovascular comorbidities (p<0.00001), substance abuse disorder (p<0.001), and mental illness (p<0.001) were the strongest predictors of readmission in the ED group. Age (p<0.01), forced expiratory volume in 1 second (p<0.001), and cardiovascular comorbidities (p<0.05) were the best predictors for both 30- and 90-day COPD readmission rates in the ED group. Only 50% of the ED group patients received bronchodilators, oral steroids, and antibiotics inclusively, and only 68% were referred for community follow-up. The need for oral steroids to treat AECOPD predicted future 90-day COPD readmissions in the ED group (p<0.003).
Conclusion: Patients discharged directly home from EDs have a significantly higher risk of readmission to EDs than those who are hospitalized. One possible reason for this is that COPD management is variable in EDs with <50% receiving appropriate therapy.
Keywords: COPD, readmissions, substance abuse, mental illness, cardiovascular disease
Introduction
Acute exacerbations of chronic obstructive pulmonary disease (AECOPD) is defined as an acute worsening of respiratory symptoms beyond baseline level including dyspnea, cough, and sputum production that require a change in medication in mild cases and emergency department (ED) visits or hospitalization in more severe cases.1 AECOPD is associated with an increased morbidity and mortality in COPD patients with an increased frequency of exacerbation leading to higher mortality,2 lower quality of life,3 an accelerated decline in lung function,4 and future adverse events.5 In the period up to 3 months following an acute exacerbation, there is a higher risk for subsequent exacerbations,6 mortality,7 and indication that even then some patients do not have full recovery in lung function.8 Furthermore, there are high health care costs9 for COPD exacerbations with acute care and ED readmissions contributing the largest amount of readmissions in Canada.10
The importance of AECOPD management has been emphasized due to the adverse effect on patient outcome and the burden to the health care system these events have. Therefore, the goal of AECOPD treatment is to minimize the impact of the exacerbation in order to reduce the frequency of future events.1 Thus, many studies have looked at the factors that are associated with exacerbation frequency to find which can be modifiable. Certain disease factors (severity of disease [forced expiratory volume in 1 second {FEV1}],11,12,19,20 exacerbation history,12,14,15,18,19 comorbidities,11,15,16,18,20 body mass index,13 previous surgeries,13 long-term oxygen therapy14), social factors (smoking,12,19 drug addiction, living without a partner/spouse,11 quality of life,12,14 socioeconomic status13,16,17), patient factors (age,12,15 physical activity,14 compliance with treatment20), and management factors (intervention programs, treatment13,14,21,22) have previously been shown to predict exacerbations and readmission of patients admitted to the hospital for AECOPD. Decision support algorithms incorporating the above-mentioned variables have been reported to assist physicians to determine whether hospital admission or ED management and observation with discharge home from the ED in AECOPD are appropriate.23–26 However, the adoption and utility of these tools are unclear and are complicated for practical use in a busy ED, and decisions to admit patients with COPD are often and mostly based on clinical judgment of the attending physician. Numerous factors have been associated with readmissions following AECOPD;12–22 however, readmission rates in patients seen in the ED for AECOPD and directly sent home are understudied, particularly the factors that predict readmissions in this population.
Approximately half of the patients seen in the ED for AECOPD are hospitalized. Of concern, adherence to guidelines for AECOPD management in the ED is typically low in the USA and Canada.27 Previous studies have examined the factors that predict relapse, admission frequency, poor outcomes, and hospital admission after an ED visit for AECOPD, few have specifically looked at patients who were directly sent home, and none looked at readmissions up to 90 days or compared the patient group treated just in the ED with those who are hospitalized.28–36 We hypothesize that readmission rates are higher in patients with AECOPD discharged directly from the ED compared with patients managed in the hospital.
This study was designed to compare the readmission rates and patient population demographics of patients visiting the ED for AECOPD and discharged directly from the ED, to patients visiting the ED and who are then hospitalized for AECOPD. We were also interested to determine the factors that predict readmission of the patients directly discharged from the ED with the primary diagnosis of AECOPD. The primary outcome measure was the total all-cause and COPD-related readmissions at 30 and 90 days post-index visit/admission for COPD. The secondary outcomes were patient factors (disease and social factors) and system factors (ED management) or variables associated with readmission.
Methods
Patient population
This was a 1-year (March 2012 to March 2013) retrospective study of all patients who were seen and managed in an inner-city tertiary hospital for AECOPD (St Paul’s Hospital, Vancouver, Canada). All patients were seen and managed in the ED and either directly sent home after stabilization or admitted to hospital for further management. The attending physician made the diagnosis of AECOPD based on clinical acumen. To be included in this analysis, the principal diagnosis of the ED visit had to be AECOPD. The index admission in both the groups was defined as the first admission for AECOPD (to ED in ED group and to hospital in hospitalized group) after the set start date.
Study design
Patient data were retrospectively collected by using patient charts and hospital’s electronic databases (that include dictations, laboratory records, radiology reports, and lung function reports). To ensure that readmissions to other hospitals or deaths were not missed, a provincial-wide electronic database was used to cross-check the data (patients who were documented as “not resident” to the area were excluded from analysis). All patients were assigned a unique study number, and all research-related information collected was attached to this number to protect patient confidentiality. No personal information that could identify a patient has been or will be used in presentations or publications. All information and data collected were kept secure, and only the principal investigator or his/her designate had access to personal information or any information that could potentially identify the patients. Ethics approval for this retrospective chart review study was obtained from the University of British Columbia and Providence Health Care Research Institute Research Ethics Board. No personal consent from the patients included in the study was obtained or required by the ethics board.
The management of the AECOPD was done by the attending physician (emergency physician in the ED group and either general internist or respirologist in the hospitalized group). The in-hospital management of AECOPD in all patients was guided by a standardized hospital-wide admission protocol for the management of AECOPD based on the GOLD strategic document.1 The AECOPD in the ED group was managed by the attending emergency physician. As there is no standardized protocol for ED management of AECOPD, specific data regarding patient assessment (investigations such as imaging, laboratory tests, and other diagnostics), patient treatment (medication given and prescribed on discharge), and patient follow-up (referrals for further testing and interventions such as pulmonary rehabilitation or follow-up by the patient’s family physician or respirologist) were collected.
Outcomes
The primary outcomes were both 30 and 90 days post-ED index and hospitalized index admission and were determined for all-cause and COPD readmissions.
Secondary outcomes were factors that predict ED readmissions after discharge from the ED for AECOPD.
Data analysis
All analyses were performed by using RStudio (Version 1.0.153 © 2009–2017; RStudio, Inc., https://www.rstudio.com/). Tests employed were two-tailed and p-values <0.05 were considered significant. Statistical tests to compare the demographics of the ED index admission and the hospitalized index admission groups were chosen depending on whether the variable was continuous or proportional and whether the data were normally distributed. Continuous variables were first tested for normality using the Shapiro–Wilk test and if not normally distributed, the Wilcoxon ranked-sum test (also called Mann–Whitney U test) was used to determine whether means were significantly different between the two groups. For proportional variables, the chi-squared tests were used to determine whether the index admission group was associated with a variable. The Yates’ correction for continuity was not applied as sample sizes were large and there were no expected frequencies less than five. Readmission rates and average time until first readmission between the ED group and hospitalized group were compared again using the Wilcoxon ranked-sum test.
Multivariate Poisson regression models were used to determine the factors that predict readmissions of patients seen in the ED for AECOPD. RStudio was used to run automated stepwise regressions, which uses lowest Akaike information criterion to determine the best model by using both forward selection and backward elimination approaches. Two types of models were created; one for patient factors and one for system factors that relate to both 30- and 90-day all-cause or COPD admissions. The regression coefficient (β) was converted to an incidence rate ratio (IRR) (X=eβ), implicating the change in the rate at which events occur with one unit change in the predictor variable.
Results
Demographics
Eligibility criteria were met for 240 patients in the ED index admission group and for 271 patients in the hospital index admission group. The demographic comparison between the two groups is shown in Table 1. The ED index admission group compared with the hospitalized index admission group was significantly younger by about 10 years (p<0.001), with milder COPD severity (as indicated by higher FEV1; p=0.001). There were 26% more current smokers (p<0.001), 13% more ever smokers (p=0.001), and 30% more substance abusers (p<0.001) in the ED group versus hospital group. Furthermore, the ED group had a higher mean number of comorbidities (p<0.001) and had 20% more mental health comorbidities (p<0.001) than the hospitalized group. The ED group had a high proportion of patients living without a partner (88.8%) and high prevalence of cardiovascular comorbidity (43.8%).
Readmissions of ED versus hospitalized patients (primary outcome)
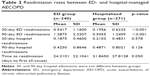
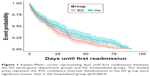
Readmission rates of the two groups are shown in Table 2. The 90-day ED readmissions (1.29 vs 0.51, p<0.001) and 30-day ED readmissions (0.54 vs 0.20, p<0.001) were significantly higher in the ED group. The 30- and 90-day hospital readmissions were not significantly different between the two groups. In the ED group, 31% of the 90-day readmissions were COPD related and 33% of the 30-day readmissions were COPD related. Time to the first all-cause readmission was significantly shorter in the ED group compared with the hospitalized group (24.21 vs 31.85 days, p<0.01) (Figure 1).
Factors predicting readmissions in ED-managed patients (secondary outcome)
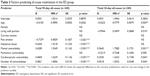
Mental health and cardiovascular comorbidities were the strongest variables associated with both 30- and 90-day readmissions in the ED group (Table 3). Thirty-day readmissions were associated with younger age (IRR =0.98, p<0.01), lack of a partner/spouse (IRR =0.37, p=0.010 or p<0.01), mental illness (IRR =1.76, p<0.01), cardiovascular comorbidities (IRR =1.42, p<0.05), and an increase in total number of comorbidities (IRR =1.05, p<0.05) (Table 3). Ninety-day readmission rates were associated with substance abuse disorder (IRR =1.53, p<0.001), mental illness (IRR =1.53, p<0.001), cardiovascular comorbidities (IRR =1.62, p<0.001), and the number of comorbidities (IRR =1.09, p<0.001). Patients who had stopped smoking (past smokers) had 52% lower risk of all-cause readmissions (p<0.001). Table 4 summarizes the risk factors associated with COPD-specific admissions. Factors with the strongest association with COPD readmissions in the ED-managed group were younger age, cardiovascular comorbidities, and FEV1.
ED management
Table 5 shows the ED management of AECOPD, demonstrating both the investigation conducted to exclude other potential causes for the patients’ symptoms and the treatment provided. Chest X-ray was requested in the majority of patients (92.9%), 55.8% of patients had workup for potential cardiovascular causes for dyspnea, and 74.1% had an infectious workup. Only 49.1% received bronchodilators, antibiotics, and steroids inclusively, and 68% of patients were referred for additional follow-up by their family physician, respirologist, or respiratory therapist for puffer training or pulmonary rehabilitation.
Interestingly, the emergency physicians’ decision to conduct an infectious workup (IRR =1.34, p<0.05) was associated with an increase in the 90-day readmission rate and a cardiovascular workup with a 90-day (IRR =1.34, p<0.01) and 30-day (IRR =1.39, p<0.05) all-cause readmission rate. Receiving bronchodilators was associated with a 47% (p<0.001) 90-day and 36% (p<0.001) 30-day reduction in all-cause readmissions. Thirty- (IRR =1.93, p<0.05) and 90-day (IRR =1.93, p<0.007) COPD readmissions were associated with the need to do a cardiovascular workup. The need to use systemic steroids was associated with an increase in 90-day COPD-related readmissions (IRR =2.13, p<0.001).
Discussion
AECOPDs are a major source of ED visits in North America and are associated with substantial morbidity and mortality.5 Many patients with AECOPD return for a repeated ED visit following discharge.6 In the present study, we showed that on average patients experience another 0.7 admissions to the ED within 30 days and 1.7 admissions within 90 days of discharge from the index ED visit. Interestingly, these rates are significantly higher than those experienced by patients who are hospitalized for their AECOPD and are subsequently discharged home although ED-discharged patients were significantly younger and had better lung function than those discharged from hospital wards.
Although the exact reasons for the higher rates of readmissions in the ED-discharged patients are not fully known, there were several important observations in our study that deserve emphasis. First, the ED-discharged patients were more likely to be current smokers and have more comorbidities (and especially substance abuse disorders and mental illnesses). Substance abuse disorder has been identified as a strong predictor for readmission following hospitalization.22 Comorbidities are common in COPD patients and adversely impact disease outcome because of many sharing risk factors and compounding effects on disease severity.37,38 Cardiovascular comorbidities were present in 44% of the patients in the ED group. Cardiovascular comorbidities have been shown to be important in COPD patients because of their prevalence and negative effects on patient outcomes.39–45 In particular, in terms of AECOPD, underlying cardiovascular diseases are associated with a higher risk for exacerbation.46,47 In addition, cardiovascular events are often triggered by AECOPD (heart failure, myocardial damage, and arrhythmia such as atrial fibrillation).48–53 This combination tends to make exacerbations more severe/complicated and raises the need for hospitalization,52,54,55 resulting in lengthened recovery times56,57 and increased mortality.45,58 Acute exacerbation of COPD may also trigger acute coronary syndrome, myocardial infarction (heart attack), stroke, and sudden cardiac death.57,58 The strong association of underlying cardiovascular comorbidities in our ED group and its association with increased readmission rates suggest that ED management of AECOPD should always include a workup for potential associated cardiovascular events.
Second, adherence to national and international guidelines for managing AECOPD in the ED was relatively low in the present study, consistent with another study in the USA and Canada.27 We found that while nearly 90% of ED patients were treated with bronchodilators, 63% with antibiotics, and 71% with a course of steroids for their AECOPD in the ED and/or prescribed to complete at home, only 49.1% received all three treatment modalities. This relative under-treatment of AECOPD may contribute to the high recurrence and readmissions rates. Interestingly, if the emergency physician deems it necessary to do a workup for potential underlying infection (complete blood count, C-reactive protein, and blood or sputum cultures) or a cardiovascular reason for dyspnea (electrocardiogram, troponin, and brain natriuretic protein), these interventions predict future readmissions. ED management analysis suggests that the patients with comorbidities (predominantly cardiovascular) and more severe COPD were correctly identified in the ED and given appropriate tests and treatment. Yet the higher readmission rates among these patients indicate that the management plan was not sufficient to prevent future exacerbations or readmissions. Better follow-up and community support are needed to monitor treatment, to do counseling on smoking cessation, to provide action plans and puffer training, and to address other factors such as substance abuse.22 Interestingly, the use of bronchodilators in the ED and at home was strongly associated with fewer readmissions (all-cause and COPD readmissions), underlying recent studies that showed the importance of proper use of bronchodilators, specifically long-acting bronchodilators in reducing AECOPD.1 The need for systemic steroids to treat AECOPD also predicts future COPD readmissions, and we suspect that the need for steroids may be just a surrogate marker for the severity of AECOPD.
There were several notable limitations in this study. Our study population is from the inner city with a large fraction of the study patients of low socioeconomic status with high prevalence of substance abuse and mental illness (more so in the ED group); therefore, the results of the study are limited in their generalizability to the wider COPD population. Since this is a retrospective study, not all variables were available for all patients. Furthermore, the ED management of AECOPD is currently not protocolized with inconsistent documentation in the discharge summary as to whether all patients received a COPD action plan or whether current smokers received smoking cessation counseling.
Conclusion
We conclude that patients managed in the ED for AECOPD and discharged directly home have a higher 30- and 90-day readmission rate than patients admitted for in-hospital management. Factors that contribute to this higher readmission rate are underlying cardiovascular disease, mental illness, and substance abuse disorder. We also identify weaknesses in the management of the patients in the ED, specifically as only 50% were given bronchodilators, steroids, and antibiotics inclusively. Other important interventions such as smoking cessation counseling, providing an action plan and referral to appropriate follow-up services such as pulmonary rehabilitation, or a respiratory specialist, were lacking. We postulate that a protocolized management plan for AECOPD in the busy ED could reduce short-term readmissions.
Disclosure
Doctor SF van Eeden is the GlaxoSmithKline-Canadian Institutes of Health Research Professor in COPD. The authors report no other conflicts of interest in this work.
References
Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease 2017 report: GOLD executive summary. Am J Respir Crit Care Med. 2017;195(5):557–582. | ||
Soler-Cataluna JJ, Martinez-Garcia MA, Roman Sanchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925–931. | ||
Seemungal TA, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(5 Pt 1):1418–1422. | ||
Makris D, Moschandreas J, Damianaki A, et al. Exacerbations and lung function decline in COPD: new insights in current and ex-smokers. Respir Med. 2007;101(6):1305–1312. | ||
Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to Exacerbation in Chronic Obstructive Pulmonary Disease. N Engl J Med. 2010;363(12):1128–1138. | ||
Hurst JR, Donaldson GC, Quint JK, Goldring JJ, Baghai-Ravary R, Wedzicha JA. Temporal clustering of exacerbations in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;179(5):369–374. | ||
Suissa S, Dell’Aniello S, Ernst P. Long-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortality. Thorax. 2012;67(11):957–963. | ||
Seemungal TA, Donaldson GC, Bhowmik A, Jeffries DJ, Wedzicha JA. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;161(5):1608–1613. | ||
Mittmann N, Kuramoto L, Seung SJ, Haddon JM, Bradley-Kennedy C, Fitzgerald JM. The cost of moderate and severe COPD exacerbations to the Canadian healthcare system. Respir Med. 2008;102(3):413–421. | ||
Discharge Abstract Database, Canadian Institute for Health Information, Fichier des hospitalisations MED-ÉCHO, ministère de la Santé et des Services sociaux du Québec. All-Cause Readmission to Acute Care and Return to the Emergency Room. Ottawa, ON: Canadian Institute for Health Information; 2012. | ||
Wong AWM, Gan WQ, Burns J, Sin DD, van Eeden SF. Acute exacerbation of chronic obstructive pulmonary disease: influence of social factors in determining length of hospital stay and readmission rates. Can Respir J. 2008;15(7):361–364. | ||
Guerra B, Gaveikaite V, Bianchi C, Puhan MA. Prediction models for exacerbations in patients with COPD. Eur Respir Rev. 2017;26(143):160061. | ||
Amalakuhan B, Kiljanek L, Parvathaneni A, Hester M, Cheriyath P, Fischman D. A prediction model for COPD readmissions: catching up, catching our breath, and improving a national problem. J Community Hosp Intern Med Perspect. 2012;2(1):10. | ||
Bahadori K, FitzGerald JM. Risk factors of hospitalization and readmission of patients with COPD exacerbation – systematic review. Int J Chron Obstruct Pulmon Dis. 2007;2(3):241–251. | ||
Santibáñez M, Garrastazu R, Ruiz-Nuñez M, et al. Predictors of hospitalized exacerbations and mortality in chronic obstructive pulmonary disease. PLoS One. 2016;11(6):e0158727. | ||
Coventry PA, Gemmell I, Todd CJ. Psychosocial risk factors for hospital readmission in COPD patients on early discharge services: a cohort study. BMC Pulm Med. 2011;11:49. | ||
Chan FWK, Wong FYY, Yam CHK, et al. Risk factors of hospitalization and readmission of patients with COPD in Hong Kong population: Analysis of hospital admission records. BMC Health Serv Res. 2011;11:186. | ||
Müllerová H, Shukla A, Hawkins A, et al. Risk factors for acute exacerbations of COPD in a primary care population: a retrospective observational cohort study. BMJ Open. 2014;4(12):e006171. | ||
Montserrat-Capdevila J, Godoy P, Marsal JR, Barbé F, Galván L. Risk factors for exacerbation in chronic obstructive pulmonary disease: a prospective study. Int J Tuberc Lung Dis. 2016;20(3):389–395. | ||
Alexopoulos EC, Malli F, Mitsiki E, Bania EG, Varounis C, Gourgoulianis KI. Frequency and risk factors of COPD exacerbations and hospitalizations: a nationwide study in Greece (Greek Obstructive Lung Disease Epidemiology and health ecoNomics: GOLDEN study). Int J Chron Obstruct Pulmon Dis. 2015;10:2665–2674. | ||
Lemmens KM, Nieboer AP, Huijsman R. A systematic review of integrated use of disease-management interventions in asthma and COPD. Respir Med. 2009;103(5):670–691. | ||
Adamson SL, Burns J, Camp PG, Sin DD, van Eeden SF. Impact of individualized care on readmissions after a hospitalization for acute exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:61–71. | ||
Garcia-Gutierrez S, Quintana JM, Barrio I, et al; IRYSS-COPD Appropriateness Study (IRYSS-CAS) Group. Application of appropriateness criteria for hospitalization in COPD exacerbation. Intern Emerg Med. 2013;8(4):349–357. | ||
Rezaee ME, Ward CE, Nuanez B, Rezaee DA, Ditkoff J, Halalau A. Examining 30-day COPD readmissions through the emergency department. Int J Chron Obstruct Pulmon Dis. 2017;13:109–120. | ||
Garcia-Gutierrez S, Quintana JM, Bilbao A, et al; IRYSS-COPD Appropriateness Study (IRYSS-COPD) Group. Validity of criteria for hospital admission in exacerbations of COPD. Int J Clin Pract. 2014;68(7):820–829. | ||
Lippmann SJ, Yeatts KB, Waller AE, et al. Hospitalizations and return visits after chronic obstructive pulmonary disease ED visits. Am J Emerg Med. 2013;31(9):1393–1396. | ||
Cydulka RK, Rowe BH, Clark S, Emerman CL, Camargo CA Jr; MARC Investigators. Emergency department management of acute exacerbations of chronic obstructive pulmonary disease in the elderly: the Multicenter Airway Research Collaboration. J Am Geriatr Soc. 2003;51(7):908–916. | ||
Kim S, Emerman CL, Cydulka RK, Rowe BH, Clark S, Camargo CA; MARC Investigators. Prospective multicenter study of relapse following emergency department treatment of COPD exacerbation. Chest. 2004;125(2):473–481. | ||
Rowe BH, Villa-Roel C, Guttman A, et al. Predictors of hospital admission for chronic obstructive pulmonary disease exacerbations in Canadian emergency departments. Acad Emerg Med. 2009;16(4):316–324. | ||
Hasegawa K, Tsugawa Y, Tsai CL, Brown DF, Camargo CA Jr. Frequent utilization of the emergency department for acute exacerbation of chronic obstructive pulmonary disease. Respir Res. 2014;15:40. | ||
Roche N, Zureik M, Soussan D, Neukirch F, Perrotin D; The Urgence BPCO (COPD Emergency) Scientific Committee and Investigators. Predictors of outcomes in COPD exacerbation cases presenting to the emergency department. Eur Respir J. 2008;32(4):953–961. | ||
Aaron SD, Vandemheen KL, Hebert P, et al. Outpatient oral prednisone after emergency treatment of chronic obstructive pulmonary disease. N Engl J Med. 2003;348(26):2618–2625. | ||
Lau AC, Yam LY, Poon E. Hospital re-admission in patients with acute exacerbation of chronic obstructive pulmonary disease. Respir Med. 2001;95(11):876–884. | ||
Murata GH, Gorby MS, Kapsner CO, Chick TW, Halperin AK. A multivariate model for the prediction of relapse after outpatient treatment of decompensated chronic obstructive pulmonary disease. Arch Intern Med. 1992;152(1):73–77. | ||
Dahlén I, Janson C. Anxiety and depression are related to the outcome of emergency treatment in patients with obstructive pulmonary disease. Chest. 2002;122(5):1633–1637. | ||
Stehr DE, Klein BJ, Murata GH. Emergency department return visits in chronic obstructive pulmonary disease: the importance of psychosocial factors. Ann Emerg Med. 1991;20(10):1113–1116. | ||
Fabbri LM, Luppi F, Beghé B, Rabe KF. Complex chronic comorbidities of COPD. Eur Respir J. 2008;31(1):204–212. | ||
Soriano JB, Visick GT, Muellerova H, Payvandi N, Hansell AL. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest. 2005;128(4):2099–2107. | ||
Müllerova H, Agusti A, Erqou S, Mapel DW. Cardiovascular comorbidity in COPD: systematic literature review. Chest. 2013;144(4):1163–1178. | ||
Mascarenhas J, Lourenço P, Lopes R, Azevedo A, Bettencourt P. Chronic obstructive pulmonary disease in heart failure. Prevalence, therapeutic and prognostic implications. Am Heart J. 2008;155(3):521–525. | ||
Bhatt SP, Dransfield MT. Chronic obstructive pulmonary disease and cardiovascular disease. Transl Res. 2013;162(4):237–251. | ||
Lange P, Marott JL, Vestbo J, et al. Prediction of the clinical course of chronic obstructive pulmonary disease, using the new GOLD classification: a study of the general population. Am J Respir Crit Care Med. 2012;186(10):975–981. | ||
Høiseth AD, Neukamm A, Karlsson BD, Omland T, Brekke PH, Søyseth V. Elevated high-sensitivity cardiac troponin T is associated with increased mortality after acute exacerbation of chronic obstructive pulmonary disease. Thorax. 2011;66(9):775–781. | ||
Dalal AA, Shah M, Lunacsek O, et al. Clinical and economic burden of patients diagnosed with COPD with comorbid cardiovascular disease. Respir Med. 2011;105(10):1516–1522. | ||
Papaioannou AI, Bartziokas K, Loukides S, et al. Cardiovascular comorbidities in hospitalised COPD patients: a determinant of future risk? Eur Respir J. 2015;46(3):846–849. | ||
Matamis D, Tsagourias M, Papathanasiou A, et al. Targeting occult heart failure in intensive care unit patients with acute chronic obstructive pulmonary disease exacerbation: effect on outcome and quality of life. J Crit Care. 2014;29(2):315.e7–315.e14. | ||
MacDonald MI, Shafuddin E, King PT, Chang CL, Bardin PG, Hancox RJ. Cardiac dysfunction during exacerbations of chronic obstructive pulmonary disease. Lancet Respir Med. 2016;4(2):138–148. | ||
Terzano C, Romani S, Conti V, Paone G, Oriolo F, Vitarelli A. Atrial fibrillation in the acute, hypercapnic exacerbations of COPD. Eur Rev Med Pharmacol Sci. 2014;18(19):2908–2917. | ||
Abusaid GH, Barbagelata A, Tuero E, Mahmood A, Sharma G. Diastolic dysfunction and COPD exacerbation. Postgrad Med. 2009;121(4):76–81. | ||
Abroug F, Ouanes-Besbes L, Nciri N, et al. Association of left-heart dysfunction with severe exacerbation of chronic obstructive pulmonary disease: diagnostic performance of cardiac biomarkers. Am J Respir Crit Care Med. 2006;174(9):990–996. | ||
El-Shabrawya M, Eldamanhor AS. Study of cardiovascular diseases in hospitalized AECOPD patients. Egypt J Chest Dis. 2017;66(1):17–25. | ||
Laratta CR, van Eeden S. Acute exacerbation of chronic obstructive pulmonary disease: cardiovascular links. BioMed Res Int. 2014;2014:528789. | ||
Patel ARC, Kowlessar BS, Donaldson GC, et al. Cardiovascular risk, myocardial injury, and exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;188(9):1091–1099. | ||
Patel ARC, Donaldson GC, Mackay AJ, Wedzicha JA, Hurst JR. The impact of ischemic heart disease on symptoms, health status, and exacerbations in patients with COPD. Chest. 2012;141(4):851–857. | ||
Chang CL, Robinson SC, Mills GD, et al. Biochemical markers of cardiac dysfunction predict mortality in acute exacerbations of COPD. Thorax. 2011;66(9):764–768. | ||
Donaldson GC, Hurst JR, Smith CJ, Hubbard RB, Wedzicha JA. Increased risk of myocardial infarction and stroke following exacerbation of COPD. Chest. 2010;137(5):1091–1097. | ||
Lahousse L, Niemeijer MN, van den Berg ME, et al. Chronic obstructive pulmonary disease and sudden cardiac death: the Rotterdam study. Eur Heart J. 2015;36(27):1754–1761. | ||
Adrish M, Nannaka VB, Cano EJ, Bajantri B, Diaz-Fuentes G. Significance of NT-pro-BNP in acute exacerbation of COPD patients without underlying left ventricular dysfunction. Int J Chron Obstruct Pulmon Dis. 2017;12:1183–1189. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.