Back to Journals » Infection and Drug Resistance » Volume 15
Emergence of High Prevalence of Extended-Spectrum Beta-Lactamase and Carbapenemase Producing Acinetobacter Species and Pseudomonas aeruginosa Among Hospitalized Patients at Dessie Comprehensive Specialized Hospital, North-East Ethiopia
Authors Tilahun M , Gedefie A , Bisetegn H , Debash H
Received 12 January 2022
Accepted for publication 24 February 2022
Published 8 March 2022 Volume 2022:15 Pages 895—911
DOI https://doi.org/10.2147/IDR.S358116
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Mihret Tilahun, Alemu Gedefie, Habitye Bisetegn, Habtu Debash
Department of Medical Laboratory Sciences, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
Correspondence: Mihret Tilahun, Department of Medical Laboratory Science College of Medicine and Health Sciences, Wollo University, PO.Box: 1145, Dessie, Ethiopia, Tel +251 920988307, Fax +251 333115250, Email [email protected]
Background: The emergence of extended spectrum beta lactamase and carbapenemase production of Acinetobacter and Pseudomonas aeruginosa is a great concern and major cause of nosocomial infections due to its ability to production of extended spectrum beta lactamase and carbapenemase enzymes.
Objective: To assess Emergence of high prevalence of extended-spectrum beta-lactamase and Carbapenemase producing Acinetobacter species and Pseudomonas aeruginosa among hospitalized patients at Dessie Comprehensive Specialized Hospital, North-East Ethiopia.
Materials and Methods: A hospital-based cross-sectional study was conducted from February–August 2021 at Dessie Referral Hospital in the North eastern Ethiopia. A total of 423 clinical samples taken from admitted patients. Clinical specimens were collected aseptically and inoculated on blood agar and MacConkey agar media. Antimicrobial susceptibility test, ESBL and carbapenemase production were performed as CLSI guideline. The data were entered into the Epi-data and imported to Statistical Package for Social Science version 25. P value of < 0.05 with odds ratio and 95% confidence interval was considered as statistically significant.
Results: Out of 423 clinical specimens 17.7% (75/423) were culture positive nosocomial infection. The proportions of nosocomial infection were higher in blood stream followed by wound infection which accounted 24.6%, 20.8%, respectively. Overall, 32/75 (42.7%) and 19/75 (25.3%) patients had infection with ESBL and CP producing bacterial infection. P. aeruginosa was the most predominant isolated bacteria 46/75 (52.9%). The overall multidrug resistance rate of the isolated bacteria was 88% (66/75). The majority of highest resistance rate was Piperacillin tazobactam 50 (66.7%) and Aztreonam 26 (56.5%), respectively, while least resistance rate was Amikacin 27 (36%).
Conclusion: The incidence rates of ESBL, carbapenemase production and antimicrobial resistant Acinetobacter species and P. aeruginosa infections are high. Therefore, treatment should be based on culture and antimicrobial test result and minimize the use of antibiotics empirically.
Keywords: nosocomial infections, extended-spectrum beta-lactamase, carbapenemase, Acinetobacter, Pseudomonas aeruginosa, drug resistance
Background
Antimicrobial resistance is frequent and has risen in Pseudomonas aeruginosa (P. aeruginosa) and Acinetobacter baumannii (A. baumannii) throughout the years, with a number of strains becoming resistant to frequently prescribed antibiotics. Due to multidrug resistant, carbapenemase and extended spectrum beta-lactamases (ESBLs) production treating infections caused by these organisms is difficult and expensive.1 P. aeruginosa has recently emerged as one of the Gram-negative bacteria with the highest carbapenem resistance. With the exception of aztreonam, it can breakdown beta-lactam antibiotics, including penicillins, cephalosporins, and carbapenems.2 It is difficult to treat infections caused by Pseudomonas spp that produce ESBLs, multidrug-resistant and overexpress chromosomal AmpC-lactamases.3
Carbapenems became increasingly important for treating life-threatening infections related to recent medical procedures and practices, such as transplantation, intensive care unit admission, and highly technical surgery as a result of the extensive occurrence of community-acquired bacterial isolates capable of hydrolyzing nearly all beta-lactam antibiotics except carbapenems.3,4 The development of carbapenemase has been linked to the later emergence of carbapenem resistance. However, because many countries around the world do not disclose antibiotic susceptibility rates, the true incidence of carbapenemase-producing bacterial strains is unknown.5
P. aeruginosa and Acinetobacter spp., both are multidrug resistant and causes of health-care-associated illnesses around the world. Carbapenems are effective against diseases caused by multidrug resistant Pseudomonas and Acinetobacter species.6,7 Both Acinetobacter species and P. aeruginosa have established resistance to a wide range of antimicrobial drugs. Additionally, in developed countries with high levels of knowledge and strong nosocomial infection surveillance, it established high carbapenem resistance infection. Carbapenems, on the other hand, are still the first-line treatment for Acinetobacter and P. aeruginosa infections.8,9
Hospital acquired infections are common admitted patients in the intensive care unit (ICU) and immunocompromised those who are not admitted. Following trauma, urinary catheters, mechanical ventilators, and venous blood collection nosocomial infection of wound, urinary tract, lower respiratory tract and blood stream are common to Acinetobacter species and P. aeruginosa. Duration of hospital stays may increase the chance of infections and death during admission.10
Carbapenem-resistant P. aeruginosa and Acinetobacter baumannii were among the World Health Organization’s 2017–2018 global priority list of pathogens, which indicated that these bacteria have become one of the global problems.11 These organisms became resistant to wide range of antibiotic which makes them a risk in the hospital setting, intermittent outbreaks and has posed considerable issues for healthcare management around the world.12
As a result, infections caused by Acinetobacter and P. aeruginosa are becoming a major public health concern in both hospital and community-acquired diseases. There are limited data in Ethiopia, especially in the study area. Therefore, a study on ESBL and carbapenemase production in Acinetobacter and P. aeruginosa among patients is critical to collect baseline data, in order to guide local empirical therapy, create local infection control programs, and develop antibiotic prescription procedures for various illnesses. Thus, the goal of this investigation was to see the magnitude of ESBL and CP Acinetobacter and P. aeruginosa isolated from patients presumptive for different bacterial infections.
Materials and Methods
Study Design, Period, and Setting
A hospital-based cross-sectional study was done from February to August 2021 at Dessie Comprehensive Specialized Hospital, North-eastern Ethiopia. Dessie Comprehensive Specialized Hospital (DCSH) is a tertiary level hospital that serves more than 12 million people with referral health treatment. It contains over 600 beds in medical, surgical, orthopedic, and pediatric departments, as well as adult and neonatal intensive care units, with an average of 600 health professionals on staff. The hospital sees 650 patients per day in several outpatient departments (OPDs), including adult, pediatric, emergency, TB, and HIV. Every month, about 900 patients were admitted.
Study Population
During the study period, the source population was all hospital admitted patients. Patients who were clinically presumptive for various nosocomial infections were included in the study. The research consisted patients who had been admitted for more than 48 hours and had clinical evidence of nosocomial wound infections, bloodstream infections, lung infections, or urinary tract infections.
Inclusion and Exclusion Criteria
The study included patients of all ages and genders who had been admitted for more than 48 hours and were suspected of having a nosocomial infection (such as wound infections, bloodstream infections, respiratory and urinary tract infections). Patients in a coma or shock, as well as those who did not provide complete data and acceptable specimens, as well as those who had insufficient volume of all specimens, were all omitted.
Variables
Prevalence of Acinetobacter species and Pseudomonas aeruginosa, their ESBL and carbapenemase production and multi-drug resistance patterns were dependent variables, whereas socio demographic characteristics like (age, sex, educational back ground, occupation, residence), patient admission area (Ward), history of previous admission, invasive or surgical procedures, extended hospital stay, history of prolonged exposure to antibiotics, number of drugs previously used and Chronic diseases were independent variables.
Sample Size Determination and Sampling Technique
The sample size was computed by using a single population proportion with prevalence of extended spectrum beta-lactamase (24.8%) taken from previous study conducted in Felege Hiwot Referral Hospital Ethiopia.13 Thus, the total sample size was obtained to be 235. But to decrease the chance of error, we included 423 hospitalized patients who clinically suspected of nosocomial bloodstream, wound, respiratory, and urinary tract infections were enrolled consecutively.
Data Collection
Patients admitted to different wards were evaluated for the development of the surgical site, urinary tract, lower respiratory tract and bloodstream NI by internists and surgeons followed prospectively according to the European Centre for Disease Prevention and Control criteria.14 Data on demographic characteristics of study participants and potential risk factors gathered through face-to-face interviews using a structured questionnaire, complemented with a review of patients’ medical records and chart review. In the case of children, the guardian/caregiver was interviewed. As soon as NI was suspected, clinical specimens such as sputum, urine, blood, and wound swabs were obtained. A separate data collection spreadsheet was used to record the isolates’ antimicrobial susceptibility testing results, as well as their ESBL and CP profiles.
Specimen Collection and Processing
All required specimens were collected from study participants in leak-proof containers using normal microbiological techniques.15
Wound/Pus Sample
Following Levine’s technique, purulent exudates, pus, and discharges were collected aseptically from the depth of the incision with a syringe or sterile cotton swabs dipped in normal saline.16 The cotton swab was inserted into a tube of Brain Heart Infusion transport medium and transferred within 30 minutes for all obtained specimens.15
Blood Sample
Aseptically collected ten milliliters of venous whole blood from adults, five milliliters from children, and two milliliters from neonates. Each patient’s samples were taken in duplicate from a separate location within a 30-minute time frame. The blood was immediately added to 5–10 mL of tryptic soy broth and incubated at 37°C. The inoculated broth was incubated aerobically at 35–37°C overnight and inspected daily for bacterial growth. Gram staining of blood culture bottles revealed obvious growth, followed by sub-culturing onto MAC agar and BA plate incubated aerobically at 35–37°C for 24 hours and examination for bacterial growth. The tryptic soy broth was subsequently cultured for 7 days after no growths were noticed before being reported as negative.15,17
Urine Sample
Using a calibrated wire loop, 0.001mL of a freshly voided midstream urine sample was inoculated into Cysteine Lactose Electrolyte Deficient Medium (HiMediaTM). Inoculated plates were incubated for 24 hours at 37°C. Colonies on blood agar were counted, and substantial bacteriuria was confirmed using a colony counter. Cultures from catheterized and non-catheterized patients that grew ≥102 CFU/mL and ≥105 CFU/mL, respectively, were taken as significant bacteriuria and processed further (significant bacteriuria) from CLED (HiMediaTM) medium were then sub-cultured into MacConkey agar (MAC) (HiMediaTM) and Blood agar (BA) plates (HiMediaTM), and then incubated at 37°C for 24 hr under.17,18
Sputum Sample
About 2mL purulent sputum was collected with a sterile wide-mouth container after the patients were momentarily instructed to rinse their mouths with water. Microbiological methods were not used on sputum specimens that had a lot of watery saliva. The sputum was smeared and analyzed right away to see if it was suitable for culture. Specimens with more than 25 polymorphonuclear leukocytes and less than 10 epithelial cells were inoculated into MAC agar and BA plates and incubated for 24 hours at 37°C.17,19
Identification of Bacterial Isolates
For biochemical and antimicrobial susceptibility test, positive growth on Blood agar and MacConkey agar (HiMediaTM) were subcultured onto Nutrient agar (HiMediaTM). In general, or identification of bacterial isolates, colony characteristics, TSI (glucose and lactose non fermenter), pigment production on culture media, motility, oxidase and catalase test, LDC and indole test biochemical test were used. Additionally, species that were difficult to differentiate were confirmed by automated Vitek 2 Compact.19
Antimicrobial Susceptibility Test
Antimicrobial susceptibility to all identified bacterial isolates was performed using Kirby-Bauer disk diffusion method based on the Clinical and Laboratory Standards Institute (CLSI2020). To prepare bacterial inoculums corresponding to the 0.5 McFarland turbidity standard, 3–5 Pure culture colonies of 24-hour growth were suspended in a tube with 4mL of physiological saline. The colony suspension was equally inoculated onto Muller–Hinton agar (HiMediaTM, India) with a sterile cotton swab, and the antibiotic discs were then placed on MHA plates. Antibacterial Medicines were chosen based on CLSI recommendations and local prescription habits. The standard antibiotic discs (Oxoid) and concentrations used for Acinetobacter species are as follows: Ceftazidime (30μg), Ciprofloxacin (5μg), Gentamicin (10μg), Meropenem (10μg), Amikacin (30μg) Piperacillin-tazobactam (100/10μg), Cefotaxime (30μg), Trimethoprim-sulfamethoxazole (1.25/23.75μg), Tetracycline (30μg). The antibiotics discs and concentrations used for Pseudomonas aeruginosa are as follows: Piperacillin-tazobactam (100/10-g), Ceftazidime (30-g), Meropenem (10-g), Gentamicin (10-g) Amikacin (30-g), Ciprofloxacin (5-g), Aztreonam (30-g) [CLSI2020]. The plates were then incubated at 37°C for 16–18 hours. A digital caliper was used to measure the sizes of the zones of inhibition surrounding the disks. The antimicrobial susceptibility test findings were classified as sensitive, moderate, or resistant depending on the results CLSI2020.20
Screening and Confirmation for ESBL Production
The thicknesses of zones of inhibition produced by either ceftazidime (30 µg g) or cefotaxime (30 µg) on the antimicrobial susceptibility test on MHA were measured according to CLSI standards for first screening for ESBL. The criteria for ceftazidime and cefotaxime that indicated suspicion of ESBL formation were ≤ 22mm and ≤ 27mm, respectively. Afterward initial screening, ESBL production was confirmed by combined disk approach based on CLSI guidelines.20 The organism to be tested was uniformly seeded onto Mueller–Hinton Agar plate. For phenotypic confirmation of the existence of ESBLs, ceftazidime (30µg) and cefotaxime (30 µg) disks alone and in combination with clavulanic acid (30 µg/10) were used at the same time. These four discs were placed 25 mm apart on a Muller Hinton agar plate inoculated with 0.5 McFarland turbidity standards bacterial suspension and incubated overnight (24 hrs) at 3737 C. A 5mm increase in the diameter of the zone of inhibition for either the ceftazidime-clavulanate or cefotaxime-clavulanate disk combination over the zone diameter of the respective cephalosporin disks alone was considered positive, and the isolate was classified as an ESBL producer.20
Phenotypic Detection of Carbapenemase Production
On the other hand, all Acetobacter species and Pseudomonas aeruginosa that shows resistance for imipenem or meropenem or zone of inhibition ≤ 19mm for imipenem or meropenem will be suspicious as Carbapenemase producer. Acetobacter species and Pseudomonas aeruginosa isolates that were susceptible to meropenem were checked for the occurrence of carbapenemase using modified carbapenem inactivation method (mCIM) based on CLSI guideline.20 It was carried out using the Modified Hodge Test (MHT), in which a Mueller–Hinton agar plate was inoculated with a 1:10 dilution of a 0.5 densitometer standardized suspension of over-night sub-cultured E. coli ATCC 25922 and streaked for confluent growth using a swab, and the meropenem-susceptible strain showed no or limited growth inhibition (E. coli ATCC 25922) CLSI recommendation.20
Quality Assurance
Questionnaire that has been pre-tested for data collection on socio-demographic traits and associated factors, a guided interview was employed. The questionnaire was pretested on 5% admitted patients those developing infection at Boru Meda hospital. During and after data collection, the data was reviewed for completeness and proper recording on the worksheet. Quality control procedures were rigorously followed for all laboratory experiments. The sterility of the media was tested overnight by incubating 5% of the batch at 35–37 °C. Before using the media, reagents, and antibiotic disks, the expiration dates were checked. The American Type Culture Collection (ATCC) reference strains of E. coli (ATCC 25922) and P. aeruginosa (ATCC 27853) were used as quality control throughout the study to check the abilities of the prepared media supporting bacterial growth for culture and antimicrobial susceptibility testing. The quality of Muller Hinton agar for antimicrobial susceptibility test was checked by enterococcus faecalis ATCC29212. For ESBL detection, E. coli ATCC 25922 and K. pneumoniae ATCC 700603 were employed as positive and negative controls, respectively. Klebsiella pneumoniae ATCC BAA1705 and K. pneumoniae ATCC BAA1706 were used as positive and negative quality control strains for carbapenemase detection, respectively. The results were interpreted in accordance with the CLSI guidelines.20
Data Analysis
Every day, the data were input into Epi-data version 4.0.0.6, then imported and analyzed using the Statistical Package for Social Science (SPSS) version 25.0 (IBM USA). To show the frequency of demographic parameters, the volume of nosocomial infections, and drug resistance profiles, descriptive statistics were calculated and summarized in graphs and tables. Logistic regression was used to show the association of different variables with the dependent variable. Uni-variate and multi-variate analyses were computed to identify factors that are independently influenced the occurrence of dependent variables. Odds ratio (OR) and 95% confidence intervals (CIs) were calculated to measure the strength of the association. P value of <0.05 was considered as statistically significant.
Ethics Approval and Consent to Participate
The study protocol was approved by the Review Board of College of Medicine and Health Sciences, Wollo University, and ethical clearance was obtained with approval number CMHS/MLS-05/009/2013. All laboratory experiments were conducted out in accordance with the relevant rules and legislation. Before collecting data, Amhara Public Health Institute and DCSH provided consent letters. Furthermore, each participant’s written informed agreement was obtained prior to the start of the study. In order to acquire information from youngsters and individuals who are unable to offer data, written agreement and consent forms were also obtained from parents and surrogates. By providing only codes for questionnaires, subject confidentiality was maintained. Participants who tested positive for the infection were referred to a doctor for treatment and any additional care that was required. Furthermore, this research was carried out in compliance with the Helsinki Declaration.
Results
Socio-Demographic and Clinical Characteristics of Study Participants
The study included 423 patients with clinical signs of nosocomial infection from various locations. Males comprise the majority of the study participants which accounted 226 (53.4%). The age of the study participants ranged from 0 to 90 years with a median age of 33 years. Moreover, majority 257 (60.8%) of the participants were rural dwellers. About 174 (41.13%) of the participants were illiterate in educational status. About 150 (35.5%) study participants were merchant and daily laborer occupation. Clinical profiles of study participants showed that majority of them were from medical wards 179 (42.3%). About 293 (69.9%) of study participants had no history of previous admission and 149 (35.22%) of participants had underlying chronic disease. However, majority of participants 284 (67.1%) had taken different types of antimicrobials previously and 278 (65.7%) participants utilized IV cannula during their medication (Table 1).
Nosocomial Infection Rate
As Figure 1 shows 423 clinical samples were collected. Of them patients 75/423 (17.7%) were culture positive nosocomial infection. The proportions of culture confirmed blood stream, urinary tract, wound infection and LRTI were 24.6%, 13.6%, 20.8% and 10%, respectively. The proportion of nosocomial infection was 45 (19.9%) for male vs female 20 (15.2%) for out-patients. The proportion of nosocomial infection was significantly higher among rural than urban dwellers 51 (19.8%) Vs 24 (14.5%). Patients who had chronic diseases had higher percentages 32 (21.7%) of infection than the counter 43 (15.7%). Similarly, patients who were previously admitted to hospital had higher proportion 25 (19.2%) of nosocomial infection than the counter (Table 1).
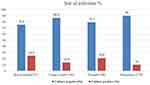 |
Figure 1 Proportion of culture confirmed nosocomial infection among patients in at Dessie Comprehensive Specialized Hospital, North eastern Ethiopia, from February–August 2021. |
Prevalence of β-Lactamase Infection
Overall, 32/75 (42.7%) and 19/75 (25.3%) patients had infection with ESBL and CP producing bacterial infection. The percentage of ESBL producing bacterial infection in blood stream, urinary tract, wound infection, and pneumonia from the total isolated bacterial was 50%, 57.9%, 51.4%, and 40%, respectively. The proportion of CP production in blood stream, urinary tract, wound infection and LRT was 18.8%, 22.1%, 22.9% and 25%, correspondingly (Table 2).
Proportion of Bacterial Isolates
Overall, P. aeruginosa was the most common 46/75 (52.9%) isolate vs Acinetobacter species. 29/75 (18.5%) but from the total blood culture. Total of 75 bacterial pathogens were isolated clinical specimens. In urine, the overall culture positivity rate (Acinetobacter spp. and Pseudomonas aeruginosa) of participants was 13.6% (19/140). The proportion of Pseudomonas aeruginosa in blood stream infection was high 75%. However, in wound/pus with higher proportion of Acinetobacter spp. was isolated 51.4% (Table 2).
ESBL and Carbapenemase Production Profiles of the Isolates
As shown in Table 3, overall, 32 (42.7%) of the bacterial isolates were ESBL producers. Among them, 20 (43.4%) of Pseudomonas aeruginosa and 12 (41.3%) of Acinetobacter species showed ESBL production. Among the bacterial isolates, 29 (38.7%) were MEM, and 19 (25.3%) were CP. Pseudomonas aeruginosa 14 (30.4%) and Acinetobacter species 5 (17.2%) were the identified carbapenemase producers.
Antibiotic Resistance Profiles of Acinetobacter spp. and Pseudomonas aeruginosa
The majority of bacterial isolates exhibited the highest resistance rate to Piperacillin tazobactam 50 (66.7%), and Aztreonam 26 (56.5%), respectively, while least resistance rate was observed for Amikacin 27 (36%). However, Acinetobacter spp. showed more resistance rate to piperacillin tazobactam 22 (75.8%), doxycycline 21 (72.4%) (93.8%) and cefotaxime 20 (68.9%) and least resistance rate for meropenem 10 (34.5%) followed by amikacin 11 (37.9%). Similarly, Pseudomonas aeruginosa is more resisted by Piperacillin tazobactam 28 (60.8%) and aztreonam 26 (56.5%) and least resistance rate for amikacin 16 (34.8%) followed by meropenem 19 (41.3%) (Table 4).
Multiple Drug Resistance Patterns of the Isolates
Overall, 89.33% (67/75) bacterial isolates were resistant to at least one antimicrobial class and the overall multidrug resistance (MDR ≥3 antimicrobial categories) rate of the isolated bacteria was 88% (66/75). About 27 (93.1%) of Acinetobacter species and 39 (84.8%) Pseudomonas aeruginosa isolates developed MDR (Figure 2 and Table 5).
 |
Table 5 Multi Drug Resistance Profile of Isolated Acinetobacter Species and Pseudomonas aeruginosa at Dessie Comprehensive Specialized Hospital, North Eastern Ethiopia, from February–August 2021 |
Factors Associated with Nosocomial Infection
Finding risk factors for nosocomial infection revealed that type of admission ward, number of antimicrobials taken at admission, illiteracy, rural residence, merchant and daily laborer, urinary catheter invasive procedure, and having chronic illnesses/diseases were all risk predictors of nosocomial infection for Acinetobacter spp. and/or P. aeruginosa. Being illiterate (AOR: 5.6; 95% CI: 1.65–45.68), being rural residence AOR: 4.5; 95% CI (1.23–55.8), merchant and daily laborer (AOR: 5.8; 95% CI: 2.5–45.89), admitted patients in the surgical ward (AOR: 10.66; 95% CI: 1.22–93.23), and orthopedics (AOR: 12.31; 95% CI: 6.5–165), and admitted patients having a primary chronic disease such as (AOR: 3.84; 95% CI: 1.33–68.99) were statistically suggestively at risk of nosocomial infection when related to hospitalized patients with no underlying chronic condition. According to the study, individuals who received three or more antibiotic kinds upon admission were 94% more protected from nosocomial infection than those who did not receive any antimicrobial (Table 6).
Discussion
Bacteria that produce ESBL and carbapenemase resistance Acinetobacter and Pseudomonas aeruginosa, two bacterial infections with substantial clinical and treatment implications, limit therapy decisions for hospitalized patients. Antimicrobial resistance profiles differed around the world depending on the type of clinical sample, ward, and institution.21 It is possible that this is due to a lack of infection-control methods in the research area. Study participants who were linked from other healthcare facilities had a greater infection rate than their peers. Similar finding was found in Uganda and Bahir Dar, Ethiopia.13 The findings of the current investigation indicated that Acinetobacter and Pseudomonas aeruginosa are the major bacteria that cause infections in both admitted and ambulatory patients. In the study area, rural dwellers had a larger percentage of infection than urban dwellers. This could be linked to differences in patients’ antibiotic exposure, which is a crucial contributor in drug resistance selection. Furthermore, the proportion of patients with chronic diseases who were infected was higher than the general population, this could be because immunocompromised individuals are more likely to cross-infect with germs from other patients, health-care staff, and hospital settings.
In the current study, 17.7% of patients were infected with Acinetobacter species and/or Pseudomonas aeruginosa. This it was relatively higher compared to reports with previous report in Addis Ababa, Ethiopia (11%),22 Hiwot Fana hospital, Ethiopia (2%),23 Bahir Dar, Ethiopia (8.4%)24 and Italy (9.3%).25 In contrast, the current study was lower than study done in Ghana (23.5%).26 This could be due to differences in sample size, infection site, patient age, different types of specimens from different wards, hospital setting, length of stay, and patients’ exposure to connected gadgets.
The magnitude of ESBL producing Acinetobacter species and/or Pseudomonas aeruginosa isolates (42.7%) in this study is comparable with research done from Iran 40.8%27 and India 48.27%,28 However, variable results were documented from different parts of Ethiopia (28.2% and 78.6%)29 and Burkina Faso (58%).30 Different studies have found a higher prevalence of ESBL, which could be related to higher colonization of Acinetobacter species and/or Pseudomonas aeruginosa in hospitals, which boosts the transmission of ESBL genes in health-care-associated strains.31 Although the magnitude of ESBL varies, all studies point to an increase in ESBL-producing isolates in developing countries, which could be due to extensive use of cephalosporins, inadequate antibiotic use control, and empirical therapy.
Moreover, the proportion of ESBL producing bacterial infection in blood stream, urinary tract, wound infection, and pneumonia from the total isolated bacterial was 50%, 57.9%, 51.4%, and 40%, respectively. A similar finding was reported in Bahir Dar, Ethiopia.13 This revealed that the most common ESBL producers are P. aeruginosa and Acinetobacter. This could be owing to the bacteria’s constant exposure to a range of β-lactams, which causes beta-lactamase synthesis. Furthermore, beta-lactamase enzymes mediated by plasmid and chromosomal genes are significant causes of antibiotic resistance.
The magnitude of CR among Acinetobacter species and/or Pseudomonas aeruginosa bacterial isolates in the present study was 25.3%. This is relatively higher compared with the previous report in Addis Ababa, Ethiopia (12.1% and 2%)29,32 Bahir Dar, Ethiopia 5.2%,13 Taiwan,33 Indonesia,34 Nepal,35 and Romania36 reported 15.4%, 13.7%, 11.2% and 21.6% of Carbapenemase production, respectively, which are much lower than the present finding, whereas reports in Nigeria,37 India,38 which accounted 34.5% each also much higher than the present study. However, systematic review also indicated that 0.96% to 35% CR was reported in other countries of East Africa.39 This suggests that carbapenemase resistance is spreading at an alarming rate, which is a big issue for impoverished nations like Ethiopia because these medications are the final resort for superbug treatment and are still not frequently provided. Additionally, settings, bacterial species, carbapenemase recognition methods, local antibiotic practice, and infection prevention systems were also considered.
The major carbapenemase producing bacteria were found from the proportion of carbapenemase production in blood stream, urinary tract, wound infection was 18.8%, 22.1%, 22.9% and 25%, correspondingly in the current study. It is true that Pseudomonas aeruginosa (30.4%) was the identified carbapenemase producers the most carbapenemase producer in clinical sample in the current study. Correspondingly, carbapenemase producing bacteria were isolated from the principal carbapenemase producing bacteria in the present study were P. aeruginosa (27.6%) in Bahir Dar, Ethiopia.13 In spite of percentage P. aeruginosa (2.6%) was the major carbapenemase producing isolates in Algeria.40 Likewise, P. aeruginosa (66%) was the one of the common carbapenemase producing organisms in Taiwan41 and study done 50 out of 104 was carbapenemase resistance.42 Carbapenem resistance in P. aeruginosa strains is caused by a number of factors. This might be carbapenemase driven by plasmids or integrons, enhanced efflux system expression, reduced porin expression, and increased chromosomal cephalosporinase activity have all been identified as contributing factors.43
Acinetobacter species and Pseudomonas aeruginosa have long been recognized as major causes of nosocomial infections over the world, with a wide range of antibiotic resistance, which makes them a hazard in the hospital setting, as seen by periodic outbreaks, and has posed considerable issues for healthcare management around the world.20,44 In the present study, Acinetobacter species and Pseudomonas aeruginosa isolates revealed high levels of resistance to Piperacillin tazobactam 50 (66.7%), and Aztreonam 26 (56.5%). This might be due to the wide availability and the blind prescription of these antibiotics in the areas.
Our result showed that Acinetobacter spp. showed more resistance rate to piperacillin tazobactam 22 (75.8%), doxycycline 21 (72.4%) (93.8%) and cefotaxime 20 (68.9%) and least resistance rate for meropenem 10 (34.5%) followed by amikacin 11 (37.9%) supported by Bahir Dar, Ethiopia,24 Vietnam,45 Kenya.46 The present study showed that resistance rates of Pseudomonas aeruginosa to P. aeruginosa are more resisted by Piperacillin tazobactam 28 (60.8%) and Aztreonam 26 (56.5%) and least resistance rate for amikacin 16 (34.8%) followed by meropenem 19 (41.3%) which is comparable to previous findings in Ugandan intensive care units, piperacillin/tazobactam.47 The resistance of the current meropenem 94.5% is lower than study conducted in Iran.48 Our findings suggest that the highest levels of resistance to third-generation cephalosporins (cefotaxime and ceftazidime) for Acinetobacter spp. and Pseudomonas aeruginosa could be connected to overuse and misuse of these antibiotics in the area that causes selective pressure and the emergence of MDR. Both Acinetobacter spp. and P. aeruginosa have lower proportions of resistance to meropenem and amikacin in this study, which could be linked to the lack of meropenem and Amikacin prescription practice in Ethiopia, as these antibiotics are used as a last resort in the treatment of serious infections and are comparatively more expensive. Furthermore, because P. aeruginosa and Acinetobacter quickly adapt to selective changes in the environmental pressures, a high turnover of experienced health professionals, a high patient load, and ineffective prevention measures could all contribute to an elevated overall drug resistance prevalence rate across different drug categories.
In this study, 88% the bacterial isolates were resistant to three or more classes of antimicrobial categories. About 93.1% of Acinetobacter species and 84.8% P. aeruginosa isolates developed MDR. A similar MDR was obtained from study conducted at Iran 88.5%.48 Higher rate of MDR was obtained from India 93% and 95%,49,50 Addis Ababa 92.9%51 and Bahir Dar, Ethiopia 100%24 and Kenya 85%.46 Whereas our result is higher than those obtained in USA 46%,52 Bosnia and Herzegovina 78.4%,53 India 54.7%,54 Saudi Arabia 69%55 and India 37 out of 73 were MDR.56 The high MDR strains of P. aeruginosa and Acinetobacter spp. found in this investigation could be owing to the fact that our study participants were admitted patients in a hospital where many antibiotics are circulating, which could function as a selective pressure for increasing MDR isolates. Furthermore, widespread prescription of common antibiotics, particularly third-generation cephalosporins, as well as drug use outside of hospitals, may contribute to the high resistance rate of Acinetobacter spp. and Pseudomonas aeruginosa to various antibiotic classes. Other possible explanations for differences in the prevalence of MDR between the current study and other similar investigations carried out elsewhere include differences in the panel of antimicrobial drugs utilized for drug sensitivity testing.
In the present study, all nosocomial infections observed among patients with associated invasive devices like IV cannula, urinary catheter and others. Being illiterate (AOR: 5.6; 95% CI: 1.65–45.68), being rural residence (AOR: 4.5; 95% CI: 1.23–55.8), merchant and daily labour (AOR: 5.8; 95% CI: 2.5–45.89), patients admitted in the surgical ward (AOR: 10.66; 95% CI: 1.22–93.23), and orthopaedics (AOR: 12.31; 95% CI: 6.5–165) were significantly at risk to develop nosocomial infection as compared to patients admitted in the medical ward. Admitted patients having an underlying chronic disease such as AOR: 3.84; 95% CI: 1.33–68.99 were statically significant at risk of nosocomial infection compared to admitted patients who had no underlying chronic disease. This was consistent with previous study in Taiwan,57 North India58 and Bahir Dar, Ethiopia24 in India: diabetes, HIV, neurological disease,54 Bosnia and Herzegovina: diabetes.53 This could be owing to patients’ significant exposure to the two viruses from the hospital environment, healthcare professionals, linked gadgets, and cross contamination. This could be because patients with underlying chronic diseases are more likely to attend hospitals, potentially exposing them to nosocomial infections.
Conclusion and Recommendation
The prevalence of nosocomial associated infection in current study was 17.7% (75/423). Among them, predominant isolates were P. aeruginosa. Overall, 42.7% and 25.3% patients had infection with ESBL and CP producing bacterial infection. The overall multidrug resistance rate of the isolated bacteria was 88%. The majority of bacterial isolates exhibited the highest resistance rate to Piperacillin tazobactam 66.7%, and aztreonam 56.5%, respectively, while amikacin and meropenem were effective drugs. Carbapenem resistance linked with a high rate of MDR, carbapenemase and extended spectrum beta-lactamases producing isolates is alarmingly increasing among isolates of nosocomial infection in the study area. Third-generation cephalosporin resistance is also a serious issue. To alter the routine use of antimicrobials, it is necessary to improve the infection prevention strategy and conduct more national surveillance on the profile of carbapenem resistance, carbapenemase, and ESBL production and their determining genes among nosocomial infection clinical isolates.
Limitations of the Study
Carbapenemase and ESBL were not genotypically performed due to a deficiency of confirmatory kits. A genotype and molecular examination for characterization of ESBL and carbapenemase gene were not performed from isolated Enterobacteriaceae. Healthy participants from the community were not included as a control even it was beyond the scope of the study.
Abbreviations
ATCC, American Type Culture Collection; AMR, Antimicrobial Resistance; BA, Blood Agar; BSI, Blood Stream Infection; CR, Carbapenem Resistance; CP, Carbapenemase Producing; CLSI, Clinical Laboratory and Standards Institute; DCSH, Dessie Comprehensive Specialized Hospital; ESBL, Extended Spectrum Beta-Lactamases; LRTI, Lower Respiratory Tract Infections; MAC, MacConkey Agar; MHA, Muller-Hilton Agar; NI, Nosocomial Infection; NICU, Neonatal Intensive care unit; SPSS, Statistical Package for Social Sciences; UTI, Urinary Tract Infection.
Data Sharing Statement
The findings of this study are based on the data that was collected and evaluated using the methods and materials that were specified. The manuscript contains all important information.
Acknowledgments
We would like to thank Dessie comprehensive specialty hospitals for allowing us to conduct our research in their facilities. We also appreciate the technical assistance provided by the Dessie comprehensive specialty hospitals’ staff. We also thank the Amhara Regional Health Bureau for allowing us to conduct the research in the Dessie comprehensive specialized hospitals. We also want to express our gratitude to all of the patients who took part in this research.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work.
Disclosure
The authors declared that no competing interest exists in this work.
References
1. Kaur A, Singh S. Prevalence of extended spectrum betalactamase (ESBL) and metallobetalactamase (MBL) producing Pseudomonas aeruginosa and Acinetobacter baumannii isolated from various clinical samples. J Pathog. 2018;2018:6845985.
2. Qureshi MA, Bhatnagar RK. Phenotypic characterization of ESBL, AmpC and MBL producers among the clinical isolates of multidrug resistant Pseudomonas aeruginosa. Int J Curr Microbiol App Sci. 2016;5(10):749–758. doi:10.20546/ijcmas.2016.510.081
3. Ettu A, Oladapo B, Oduyebo O. Prevalence of carbapenemase production in Pseudomonas aeruginosa isolates causing clinical infections in Lagos University Teaching Hospital, Nigeria. African J Clin Exp Microbiol. 2021;22(4):498–503. doi:10.4314/ajcem.v22i4.10
4. Codjoe FS, Donkor ES. Carbapenem resistance: a review. Med Sci. 2018;6(1):1. doi:10.3390/medsci6010001
5. Nordmann P, Dortet L, Poirel L. Carbapenem resistance in Enterobacteriaceae: here is the storm! Trends Mol Med. 2012;18(5):263–272. doi:10.1016/j.molmed.2012.03.003
6. Kateete DP, Nakanjako R, Namugenyi J, Erume J, Joloba ML, Najjuka CF. Carbapenem resistant Pseudomonas aeruginosa and Acinetobacter baumannii at Mulago Hospital in Kampala, Uganda (2007–2009). Springerplus. 2016;5(1):1–11. doi:10.1186/s40064-016-2986-7
7. Kateete DP, Nakanjako R, Okee M, Joloba ML, Najjuka CF. Genotypic diversity among multidrug resistant Pseudomonas aeruginosa and Acinetobacter species at Mulago Hospital in Kampala, Uganda. BMC Res Notes. 2017;10(1):1–10. doi:10.1186/s13104-017-2612-y
8. Almasaudi SB. Acinetobacter spp. as nosocomial pathogens: epidemiology and resistance features. Saudi J Biol Sci. 2018;25(3):586–596. doi:10.1016/j.sjbs.2016.02.009
9. Nørgaard SM, Jensen CS, Aalestrup J, Vandenbroucke-Grauls CM, de Boer MG, Pedersen AB. Choice of therapeutic interventions and outcomes for the treatment of infections caused by multidrug-resistant gram-negative pathogens: a systematic review. Antimicrob Resist Infect Control. 2019;8(1):1–13. doi:10.1186/s13756-019-0624-1
10. Centers for Disease Control and Prevention. Pseudomonas Aeruginosa in Healthcare Settings. Centers for Disease Control and Prevention; 2019.
11. Shrivastava SR, Shrivastava PS, Ramasamy J. World health organization releases global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics. J Med Soc. 2018;32(1):76. doi:10.4103/jms.jms_25_17
12. Shrivastava SR, Shrivastava PS. Emergence of antibiotic resistance: a global public health and a political priority. Hamdan Med J. 2019;12(4):236. doi:10.4103/HMJ.HMJ_93_18
13. Alebel M, Mekonnen F, Mulu W. Extended-spectrum β-lactamase and carbapenemase producing gram-negative bacilli infections among patients in intensive care units of Felege Hiwot Referral Hospital: a prospective cross-sectional study. Infect Drug Resist. 2021;14:391. doi:10.2147/IDR.S292246
14. Plachouras D, Kärki T, Hansen S, et al. Antimicrobial use in European acute care hospitals: results from the second point prevalence survey (PPS) of healthcare-associated infections and antimicrobial use, 2016 to 2017. Eurosurveillance. 2018;23(46):1800393. doi:10.2807/1560-7917.ES.23.46.1800393
15. Murray PR, Rosenthal KS, Pfaller MA. Medical Microbiology E-Book. Elsevier Health Sciences; 2020.
16. Levine NS, Lindberg RB, Mason JAD, Pruitt JBA. The quantitative swab culture and smear: a quick, simple method for determining the number of viable aerobic bacteria on open wounds. J Trauma. 1976;16(2):89–94. doi:10.1097/00005373-197602000-00002
17. Cheesbrough M. District Laboratory Practice in Tropical Countries, Part 2. Cambridge University Press; 2005.
18. Mahmood T, Yang P-C. Western blot: technique, theory, and trouble shooting. N Am J Med Sci. 2012;4(9):429. doi:10.4103/1947-2714.100998
19. Levinson W. Review of Medical Microbiology and Immunology. McGraw-Hill Education; 2014.
20. Weinstein MP, Lewis JS. The clinical and laboratory standards institute subcommittee on antimicrobial susceptibility testing: background, organization, functions, and processes. J Clin Microbiol. 2020;58(3):e01864–19. doi:10.1128/JCM.01864-19
21. Kunz AN, Brook I. Emerging resistant gram-negative aerobic bacilli in hospital-acquired infections. Chemotherapy. 2010;56(6):492–500. doi:10.1159/000321018
22. Bitew A. High prevalence of multi-drug resistance and extended spectrum beta lactamase production in non-fermenting gram-negative bacilli in Ethiopia. Infect Dis Res Treat. 2019;12:1178633719884951.
23. Tolera M, Abate D, Dheresa M, Marami D. Bacterial nosocomial infections and antimicrobial susceptibility pattern among patients admitted at Hiwot Fana Specialized University Hospital, Eastern Ethiopia. Adv Med. 2018;2018:89–94.
24. Motbainor H, Bereded F, Mulu W. Multi-drug resistance of blood stream, urinary tract and surgical site nosocomial infections of Acinetobacter baumannii and Pseudomonas aeruginosa among patients hospitalized at Felege Hiwot Referral Hospital, Northwest Ethiopia: a cross-sectional study. BMC Infect Dis. 2020;20(1):1–11. doi:10.1186/s12879-020-4811-8
25. De Francesco MA, Ravizzola G, Peroni L, Bonfanti C, Manca N. Prevalence of multidrug-resistant Acinetobacter baumannii and Pseudomonas aeruginosa in an Italian hospital. J Infect Public Health. 2013;6(3):179–185. doi:10.1016/j.jiph.2012.11.006
26. Agyepong N, Govinden U, Owusu-Ofori A, Essack SY. Multidrug-resistant gram-negative bacterial infections in a teaching hospital in Ghana. Antimicrob Resist Infect Control. 2018;7(1):1–8. doi:10.1186/s13756-018-0324-2
27. Sharif MR, Soltani B, Moravveji A, Erami M, Soltani N. Prevalence and risk factors associated with extended spectrum beta lactamase producing Escherichia coli and Klebsiella pneumoniae isolates in hospitalized patients in Kashan (Iran). Electron Phys. 2016;8(3):2081. doi:10.19082/2081
28. Shaikh S, Fatima J, Shakil S, Rizvi SMD, Kamal MA. Risk factors for acquisition of extended spectrum beta lactamase producing Escherichia coli and Klebsiella pneumoniae in North-Indian hospitals. Saudi J Biol Sci. 2015;22(1):37–41. doi:10.1016/j.sjbs.2014.05.006
29. Legese MH, Weldearegay GM, Asrat D. Extended-spectrum beta-lactamase-and carbapenemase-producing Enterobacteriaceae among Ethiopian children. Infect Drug Resist. 2017;10:27. doi:10.2147/IDR.S127177
30. Ouedraogo A-S, Sanou M, Kissou A, et al. High prevalence of extended-spectrum ß-lactamase producing Enterobacteriaceae among clinical isolates in Burkina Faso. BMC Infect Dis. 2016;16(1):1–9. doi:10.1186/s12879-016-1655-3
31. Amladi AU, Sudarsanam TD, Kandasamy S, Kekre N, Veeraraghavan B, Sahni RD. Evaluation of CHROMagar™ TMmSuperCARBA™ as a phenotypic test for detection of carbapenemase producing organisms. J Clin Diagn Res. 2019;13(9):19–22.
32. Beyene D, Bitew A, Fantew S, Mihret A, Evans M. Multidrug-resistant profile and prevalence of extended spectrum β-lactamase and carbapenemase production in fermentative gram-negative bacilli recovered from patients and specimens referred to National Reference Laboratory, Addis Ababa, Ethiopia. PLoS One. 2019;14(9):e0222911. doi:10.1371/journal.pone.0222911
33. Chang -Y-Y, Chuang Y-C, Siu LK, et al. Clinical features of patients with carbapenem nonsusceptible Klebsiella pneumoniae and Escherichia coli in intensive care units: a nationwide multicenter study in Taiwan. J Microbiol Immunol Infect. 2015;48(2):219–225. doi:10.1016/j.jmii.2014.05.010
34. Saharman YR, Lestari DC. Phenotype characterization of Beta-lactamase producing Enterobacteriaceae in the intensive care unit (ICU) of Cipto Mangunkusumo hospital in 2011. Acta Medica Indonesiana. 2016;45(1):11–16
35. Kayastha K, Dhungel B, Karki S, et al. Extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella species in pediatric patients visiting International Friendship Children’s Hospital, Kathmandu, Nepal. Infect Dis Res Treat. 2020;13:1178633720909798.
36. Zaha DC, Kiss R, Hegedűs C, et al. Recent advances in investigation, prevention, and management of healthcare-associated infections (HAIs): resistant multidrug strain colonization and its risk factors in an intensive care unit of a University Hospital. Biomed Res Int. 2019;2019:2510875.
37. Kano C. Carbapenem-Resistant Enterobacteriaceae (CRE) in intensive care units and surgical wards of hospitals with no history of carbapenem usage in Kano, North West Nigeria. Niger J Microbiol. 2015;27(1):2612–2618.
38. Oberoi L, Singh N, Sharma P, Aggarwal A. ESBL, MBL and Ampc β lactamases producing superbugs–havoc in the Intensive Care Units of Punjab India. J Clin Diagn Res. 2013;7(1):70. doi:10.7860/JCDR/2012/5016.2673
39. Ssekatawa K, Byarugaba DK, Wampande E, Ejobi F. A systematic review: the current status of carbapenem resistance in East Africa. BMC Res Notes. 2018;11(1):1–9. doi:10.1186/s13104-018-3738-2
40. Hecini-Hannachi A, Bentchouala C, Lezzar A, Laouar H, Benlabed K, Smati F. Multidrug-resistant bacteria isolated from patients hospitalized in intensive care unit in University Hospital of Constantine, Algeria (2011–2015). Afr J Microbiol Res. 2016;10(33):1328–1336. doi:10.5897/AJMR2016.8257
41. Liao C-H, Lee N-Y, Tang H-J, et al. Antimicrobial activities of ceftazidime–avibactam, ceftolozane–tazobactam, and other agents against Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa isolated from intensive care units in Taiwan: results from the Surveillance of Multicenter Antimicrobial Resistance in Taiwan in 2016. Infect Drug Resist. 2019;12:545. doi:10.2147/IDR.S193638
42. Mohajeri P, Sharbati S, Farahani A, Rezaei Z. Evaluate the frequency distribution of nonadhesive virulence factors in carbapenemase-producing Acinetobacter baumannii isolated from clinical samples in Kermanshah. J Nat Sci Biol Med. 2016;7(1):58. doi:10.4103/0976-9668.175071
43. Meletis G, Exindari M, Vavatsi N, Sofianou D, Diza E. Mechanisms responsible for the emergence of carbapenem resistance in Pseudomonas aeruginosa. Hippokratia. 2012;16(4):303.
44. Exner M, Bhattacharya S, Christiansen B, et al. Antibiotic resistance: what is so special about multidrug-resistant Gram-negative bacteria? GMS Hyg Infect Control. 2017;12:Doc05.
45. Tran GM, Ho-le TP, Ha DT, et al. Patterns of antimicrobial resistance in intensive care unit patients: a study in Vietnam. BMC Infect Dis. 2017;17(1):1–7. doi:10.1186/s12879-017-2529-z
46. Musyoki VM, Masika MM, Mutai W, Wilfred G, Kuria A, Muthini F. Antimicrobial susceptibility pattern of Acinetobacter isolates from patients in Kenyatta National Hospital, Nairobi, Kenya. Pan Afr Med J. 2019;33:146.
47. Carrillo JV, Uzcategui RP, Fermín LR, Zambrano RA, Fermin LR. Caracterización química y actividad antibacteriana del aceite esencial de Mangifera indica L. [Chemical characterization and antibacterial activity of the essential oil of Mangifers indica L in three regions of Venezuela]Revista Colombiana de Química. 2019;48(3):13–18. Spanish.
48. Ranjbar R, Farahani A. Study of genetic diversity, biofilm formation, and detection of Carbapenemase, MBL, ESBL, and tetracycline resistance genes in multidrug-resistant Acinetobacter baumannii isolated from burn wound infections in Iran. Antimicrob Resist Infect Control. 2019;8(1):1–11. doi:10.1186/s13756-019-0612-5
49. Kaur T, Putatunda C, Oberoi A, Vyas A, Kumar G. Prevalence and drug resistance in Acinetobacter sp. isolated from intensive care units patients in Punjab, India; 2018.
50. Mohajeri P, Farahani A, Feizabadi M, Norozi B. Clonal evolution multi-drug resistant Acinetobacter baumannii by pulsed-field gel electrophoresis. Indian J Med Microbiol. 2015;33(1):87–91. doi:10.4103/0255-0857.148390
51. Diriba K, Awulachew E, Gemede A, Anja A. The magnitude of extended-spectrum beta-lactamase-producing Enterobacteriaceae from clinical samples in Ethiopia: a systematic review and meta-analysis. Access Microbiol. 2021;3(3). doi:10.1099/acmi.0.000195
52. Queenan AM, Pillar CM, Deane J, et al. Multidrug resistance among Acinetobacter spp. in the USA and activity profile of key agents: results from CAPITAL surveillance 2010. Diagn Microbiol Infect Dis. 2012;73(3):267–270. doi:10.1016/j.diagmicrobio.2012.04.002
53. Rebic V, Masic N, Teskeredzic S, Aljicevic M, Abduzaimovic A, Rebic D. The importance of Acinetobacter species in the hospital environment. Med Arch. 2018;72(5):325. doi:10.5455/medarh.2018.72.330-334
54. Dash M, Padhi S, Pattnaik S, Mohanty I, Misra P. Frequency, risk factors, and antibiogram of Acinetobacter species isolated from various clinical samples in a tertiary care hospital in Odisha, India. Avicenna J Med. 2013;3(4):97. doi:10.4103/2231-0770.120501
55. Al-Mously N. Acinetobacter baumannii bloodstream infections in a tertiary hospital: antimicrobial resistance surveillance. Int J Infect Control. 2013;9(2). doi:10.3396/ijic.v9i2.012.13
56. Mohajeri P, Farahani A, Mehrabzadeh RS. Molecular characterization of multidrug resistant strains of Acinetobacter baumannii isolated from intensive care units in west of Iran. J Clin Diagn Res. 2017;11(2):DC20. doi:10.7860/JCDR/2017/21156.9397
57. Tsao L-H, Hsin C-Y, Liu H-Y, Chuang H-C, Chen L-Y, Lee Y-J. Risk factors for healthcare-associated infection caused by carbapenem-resistant Pseudomonas aeruginosa. J Microbiol Immunol Infect. 2018;51(3):359–366. doi:10.1016/j.jmii.2017.08.015
58. Asif M, Alvi IA, Rehman SU. Insight into Acinetobacter baumannii: pathogenesis, global resistance, mechanisms of resistance, treatment options, and alternative modalities. Infect Drug Resist. 2018;11:1249. doi:10.2147/IDR.S166750
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.






