Back to Journals » Neuropsychiatric Disease and Treatment » Volume 14
Electroconvulsive therapy in 77-year-old patient with pacemaker: a case report
Authors Mędrala T , Pycińska A, Pyciński B, Merk W , Kucia K
Received 10 January 2018
Accepted for publication 15 February 2018
Published 17 April 2018 Volume 2018:14 Pages 1055—1058
DOI https://doi.org/10.2147/NDT.S162125
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Tomasz Mędrala,1 Anna Pycińska,1 Bartłomiej Pyciński,2 Wojciech Merk,1 Krzysztof Kucia1
1Department of Psychiatry and Psychotherapy, School of Medicine in Katowice, Medical University of Silesia, Katowice, 2Faculty of Biomedical Engineering, Silesian University of Technology, Zabrze, Poland
Abstract: The treatment of a 77-year-old patient suffering from severe psychotic depression with a cardiac pacemaker is described. Because of treatment-resistant depression, electroconvulsive therapy (ECT) was introduced. In the course of ECT, there was a great improvement in his mental state without any cardiac complications. This case may be evidence for the safety and effectiveness of ECT in the elderly, even with cardiac comorbidities. Some recommendations for ECT in patients with pacemakers are discussed.
Keywords: refractory depression, cardiac stimulator, electroconvulsive therapy
Introduction
Electroconvulsive therapy (ECT) is an effective treatment of refractory depression.1,2 It is considered a safe method in psychiatric patients with cardiac diseases.3,4 However, there are not sufficient published data on the use of ECT in patients with implanted pacemakers. The proper treatment of these patients seems to be a complex problem, especially for the elderly. Psychopharmacotherapy may not always be the preferred method, as the majority of psychotropic medications affect the cardiovascular system, eg, they prolong the QT interval or increase blood pressure. The use of psychopharmacotherapy is limited because of the risk of adverse effects in combination with medications for patients’ somatic diseases. ECT is known to be the most effective alternative method for psychiatric treatment.2 However, to the authors’ best knowledge, there have been no large, randomized clinical studies concerning the treatment of patients with cardiac pacemakers who suffer from psychiatric diseases.
A chance to meet such patients is going to increase, as Murray and Lopez in the Global Burden of Disease Study claimed that until 2020, “leading causes of disability-adjusted life years (DALYs) predicted by the baseline model will have been (in descending order): ischaemic heart disease, unipolar major depression … [and others]”.5 Therefore, psychiatrists will increasingly have to choose the right treatment for elderly cardiac patients suffering from psychiatric diseases. Also, the aging population might need more cardiac rhythm-management devices, and as ECT is a highly effective, safe, and well-tolerated antidepressant-treatment option for geriatric patients, it might be used more widely.6 In this paper, we describe a 77-year-old patient with a cardiac pacemaker who suffered from severe psychotic depression and was treated by ECT.
Case report
A 77-year-old male Caucasian widower was admitted to our ward because of severe psychotic depression. At the beginning of the hospitalization, he presented hypochondria, sin, persecution, and poverty delusions.
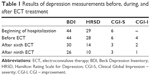
Additionally, suicidal thoughts were present. His night dreams were interrupted by frequent waking and difficulties in falling asleep again. The patient was apathetic, with low mood and prominent motor agitation. He complained about anhedonia, anergy, and loss of purposeful activity. He was focused on his health and the medications he was taking. He was absorbed by thoughts of his past and mistakes he had made. Beck Depression Inventory (BDI),7 Hamilton Rating Scale for Depression (HRSD),8 and Clinical Global Impression – severity (CGI-S) scale9 scores were 44, 29, and 6 points, respectively. The patient provided written informed consent to have the case details published.
The BDI is a 21-question, multiple-choice, self-report inventory used for measuring the severity of depression. The HRSD is used to rate the severity of depression symptoms, such as mood, feelings of guilt, suicide ideation, insomnia, agitation or retardation, anxiety, weight loss, and somatic symptoms. The patient is rated by a clinician on 17–29 items (depending on version) scored either on a 3-point or 5-point Likert-type scale. For the 17-item version, a score of 0–7 is considered normal. Scores ≥20 or higher indicate moderate, severe, or very severe depression. The CGI-S is a 7-point scale that requires the clinician to rate the severity of mental symptoms at the time of assessment relative to the clinician’s past experience with patients who have the same diagnosis. CGI – improvement (CGI-I) is a 7-point scale where the clinician assesses the evolution of the symptoms: either improvement or worsening compared to a baseline state at the beginning of the intervention.
The patient had been treated by his psychiatrist for 2 years. Previously, he had been taking venlafaxine 150 mg/day, vortioxetine 5 mg/day, mianserine 15 mg/day, mirtazapine 30 mg/day, citalopram 20 mg/day, agomelatine 25 mg/day, flupentixol 1 mg/day, and more recently clomipramine 75 mg/day, olanzapine 2.5 mg/day, and alprazolam 1 mg/day, without any clinical improvement. In the interview, the patient reported deterioration of his psychic state in the last 6 months. At that time, a cardiac pacemaker had been implanted for symptomatic sinus-node dysfunction. The type of pacemaker was a DDDR (Vitatron E60A1, electrodes 5,076 [58 cm] and 5,076 [52 cm]; Medtronic, Dublin, Ireland). Additionally, the patient was suffering from prostatic hyperplasia, arterial hypertension, and mixed hyperlipidemia. A computed tomography scan of his head was performed, where a radiologist described moderate cortical atrophy of the brain hemispheres and a small lacuna in the basal ganglia on the left side.
When we introduced ECT, it was the patient’s first psychiatric hospitalization. At the beginning, clomipramine and benzodiazepine were reduced. Trazodone was added and the dose increased gradually to 150 mg/day. Because of the productive symptoms mentioned earlier, as well as to activate the patient, sulpiride was included at a dose of 200 mg/day. Venlafaxine at a dose of 150 mg/day was prescribed as the main antidepressant. Before we started ECT, we had discontinued venlafaxine, and both trazodone and sulpiride treatments were maintained.
Due to the lack of expected improvement, the doctors decided to conduct a series of ECT after 30 days’ stay in the psychiatric ward. Because of this, the patient was consulted by a neurologist, anesthesiologist, and electrocardiologist. Before the first ECT treatment, the pacemaker was checked. Before starting the first ECT, the following results were obtained: 44 points on the BDI, 28 on the HRSD, 6 on the CGI-S, and 4 on the CGI-I (Table 1). Nine ECTs with maximum load of 432 mC were conducted twice a week. In anesthesia, the patient always received propofol at a maximum dose of 180 mg/day and suxamethonium at a maximum of 80 mg/day. The electrodes were placed bitemporally, and the longest sending of an electrical impulse was 3 seconds. Periodically, the pacemaker was examined at the electrocardiology ward. After each ECT routine, a 12-lead electrocardiography procedure was performed. If necessary, it was possible to consult an electrocardiologist urgently. The pacemaker’s functions remained normal during the entire hospitalization.
After the fourth ECT treatment, some improvements in psychic status were objectively observed. The patient was less preoccupied with the state of his health and mistakes he had committed in the past. Subjectively, the patient did not feel the change. ECT was continued. The patient increased his purposeful activity, and he was able to focus his attention on reading. Also, the patient’s family noticed a significant improvement in his mental status: he expressed interest in the world around him and his family home. After the sixth ECT treatment, the following results were obtained: BDI 30 points, HRSD 14 points, CGI-S 3 points, and CGI-I 2 points. After the eighth treatment, the patient began to declare a subjective improvement in his well-being. Gradually, he began to go for walks and do things that pleased him. He got a pass to the house. Due to the improvement in the patient’s mental state, ECT was ended after nine treatments. He was discharged in a balanced mood and psychomotor drive, with no signs of psychotic production or suicidal thoughts, with the following results: BDI 28 points, HRSD 10 points, CGI-S 3 points, and CGI-I 1 point.
Discussion
A wide range of pacemakers are currently used. A DDDR pacemaker, pacing and sensing both chambers of the heart and adjusting automatically, was implanted in our patient.10 During the hospitalization, the algorithm of the pacemaker was not modified. Although ECT is known to be a safe treatment, there are some concerns that an electrical impulse will impact pacemakers, especially older ones.3,11 On the other hand, pacemakers are sensitive on demand to myopotentials generated by clonic skeletal muscle contractions or suxamethonium-induced muscle fasciculations, which may lead to their malfunction. Therefore, during ECT these pacemakers should be temporarily reprogrammed to an asynchronous mode. However, in most cases, the pacemaker mode was not converted. The synchronous mode was preserved to minimize the risk of VT/VF episodes, which are the most serious side effects occurring in the asynchronous mode.4
Moreover, newer pacemakers are rarely disturbed by muscle-relaxant medicines. As such, taking into account other case reports, staying with the synchronous mode might be preferable.4 Dolenc et al reported that anticholinergic agents used immediately before ECT might be used to prevent the patient from developing bradycardia or asystolia.3 Atropine should protect the patient from bradycardia connected with activating the parasympathetic nervous system, especially in patients with primary bradyarrhythmia or heart block.2 However, the use of anticholinergics has been criticized.4 The anesthesiologist should always be prepared for pacemaker-malfunction episodes.
Furthermore, while ECT is being conducted, a special magnet should be easily available to reprogram the pacemaker immediately. Response of the pacemaker to the magnet may be varied, eg, a transient or continuous dysfunction, turning into asynchronous mode or null response. It depends on the model or even its battery level. Therefore, the clinician should know the technical data of the device before the ECT procedure.11
There have been no large, randomized clinical studies of ECT treatment on patients with implanted pacemakers. Recommendations, which cover additional procedures before, during, and after ECT, were proposed by Kokras et al.4 According to these, before each ECT, the physician is supposed to check the parameters of the pacemaker and ensure that the electrodes are correctly placed. Proper cooperation between the ordering psychiatrist, anesthetist, and cardiologist is required. Although presence of the cardiologist is not routinely necessary, a competent authority on pacemakers should be available during the treatment. The asynchronous mode should be temporarily disabled if recommended by the manufacturer. Anticholinergics should be avoided, as they increase the workload of the heart during ECT, but at the same time they decrease the risk of bradycardia. After each ECT procedure, the physician should check the pacemaker.4
Similar recommendations were introduced in 2004. Moreover, they necessitated the use of a magnet for changing the mode of a pacemaker.3 Cardiological side effects after ECT include heart infarction with or without elevated ST segment, congestive heart failure, or atrial fibrillation. Different arrhythmias are the most common side effects. They are connected with activating the autonomous nervous system during seizures.2 At first, the parasympathetic system prevails, which is responsible for slowing down the rhythm of the heart and decreasing blood pressure, resulting in bradyarrhythmia. Next, the sympathetic system is activated, which accelerates the pulse, increases blood pressure, and may result in tachyarrhythmia. MacPherson et al even formulated the theory that having a pacemaker can protect against significant bradyarrhythmia or asystole caused by a cholinergic surge connected with ECT.11
Conclusion
The description herein of this clinical case confirms once again that the use of ECT is safe, even in patients with an implanted cardiostimulator. It is not necessary to program a pacemaker for asynchronous mode. However, it is important to provide appropriate care for a patient from a person who can operate pacemakers. At least periodic interrogation of a pacemaker is required. In some cases, it was conducted only after the first and last ECT session.12 Our patient had his pacemaker checked five times in total. Every time, the stimulator was functioning properly. In this patient, no cardiac complications were noted after ECT. Also, Dolenc et al did not describe any arrhythmia connected with ECT or with the use of suxamethonium.3 There have been no reports of pacemaker dysfunction related to ECT.11 Moreover, the risk of anesthetic complications or cardiac dysfunction does not increase after the cardiac stimulator is implanted.11
Disclosure
The authors report no conflicts of interest in this work.
References
Fink M. Convulsive therapy: a review of the first 55 years. J Affect Disord. 2001;63:1–15. | ||
Yu SW, Vallurupalli S, Arnoldi J, Holloway R. Atrioventricular dissociation after electroconvulsive therapy. Cardiol Res Pract. 2011;2011:746373. | ||
Dolenc TJ, Barnes RD, Hayes DL, Rasmussen KG. Electroconvulsive therapy in patients with cardiac pacemakers and implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2004;27:1257–1263. | ||
Kokras N, Politis AM, Zervas IM, et al. Cardiac rhythm management devices and electroconvulsive therapy: a critical review apropos of a depressed patient with a pacemaker. J ECT. 2011;27:214–220. | ||
Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease study. Lancet. 1997;349:1498–1504. | ||
Geduldig ET, Kellner CH. Electroconvulsive therapy in the elderly: new findings in geriatric depression. Curr Psychiatry Rep. 2016;18:40. | ||
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. | ||
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. | ||
Guy W. ECDEU Assessment Manual for Psychopharmacology. Rockville (MD): Alcohol, Drug Abuse, and Mental Health Administration; 1976. | ||
Klaudel J. Pacjent z rozrusznikiem serca. Chor Serca Naczyn. 2004;1:51–71. | ||
MacPherson RD, Loo CK, Barrett N. Electroconvulsive therapy in patients with cardiac pacemakers. Anaesth Intensive Care. 2006;34:470–474. | ||
Gosselink MJ, Schenkeveld KW, Trines SA, van Vliet IM. Successful electroconvulsive therapy in a 95-year-old man with a cardiac pacemaker: a case report. Am J Geriatr Psychiatry. 2011;19:678–679. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.