Back to Journals » Neuropsychiatric Disease and Treatment » Volume 14
Efficacy, tolerability, and safety of oral paliperidone extended release in the treatment of schizophrenia: a 24-week, open-label, prospective switch study in different settings in Taiwan
Authors Chen CY, Tang TC, Chen TT, Bai YM, Tsai HH, Chen HL, Huang CJ, Chen CK, Chen CC, Hsiao MC , Liu CY , Yeh HS, Chiu NY, Hsiao CC, Chen CS, Su TP
Received 1 January 2018
Accepted for publication 13 February 2018
Published 8 March 2018 Volume 2018:14 Pages 725—732
DOI https://doi.org/10.2147/NDT.S161186
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Wai Kwong Tang
Ching-Yen Chen,1,2 Tze-Chun Tang,3 Tzu-Ting Chen,4 Ya Mei Bai,5,6 Huei-Huang Tsai,7 Hou-Liang Chen,7 Chun-Jen Huang,8,9 Chih-Ken Chen,1,2 Chun-Chih Chen,10 Mei-Chun Hsiao,11 Chia-Yih Liu,2,12 Hong-Shiow Yeh,13 Nan-Ying Chiu,10 Cheng-Chen Hsiao,14 Cheng-Sheng Chen,8,9 Tung-Ping Su5,15,16
1Department of Psychiatry, Keelung Chang Gung Memorial Hospital, Keelung, Taiwan; 2School of Medicine, Chang Gung University, Taoyuan, Taiwan; 3Dr Tang’s Psychiatric Clinic, Kaohsiung, Taiwan; 4Department of Psychiatry, National Taiwan University Hospital, Yunlin Branch Hospital, Yunlin, Taiwan; 5Department of Psychiatry, Taipei Veterans General Hospital, Taipei, Taiwan; 6Department of Psychiatry, College of Medicine, National Yang-Ming University, Taipei, Taiwan; 7Tsao Tun Psychiatric Center, Ministry of Health and Welfare, Nantou, Taiwan; 8Department of Psychiatry, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan; 9Department of Psychiatry, School of Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan; 10Department of Psychiatry, Changhua Christian Hospital Lukang Branch Hospital, Changhua, Taiwan; 11Yong Mei Psychiatric Clinic, Taoyuan City, Taiwan; 12Department of Psychiatry, Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan; 13Department of Psychiatry, Mackay Memorial Hospital, Taipei, Taiwan; 14Cheng Chen Hsiao Clinic, Chiayi, Taiwan; 15Division of Psychiatry, Faculty of Medicine, National Yang-Ming University, Taipei, Taiwan; 16Department of Psychiatry, Cheng Hsin General Hospital, Taipei, Taiwan
Purpose: Paliperidone extended release (ER) is an oral psychotropic treatment formulated to release paliperidone at a controlled, gradually ascending rate. We evaluated the efficacy and safety of switching to paliperidone ER in Taiwanese patients with schizophrenia who were unresponsive or intolerant to previous antipsychotic therapy.
Patients and methods: This was a 24-week, open-label, single-arm, multicenter, Phase IV trial. Based on consulting psychiatrists’ judgment, patients were deemed eligible for the switch to paliperidone ER; the switch was achieved by cross-tapering, using a recommended starting dose of 6 mg. Eligibility considerations included lack of efficacy, tolerability, and/or adherence to previous oral antipsychotic medication.
Results: Of the 297 enrolled patients, 178 (59.5%) completed the study. The main reasons for discontinuation included insufficient efficacy (8.7%), patient decision (8.4%), and adverse events (AEs; 6.4%). Improvements in the: Positive and Negative Syndrome Scale total score and Clinical Global Impression-Severity score were observed only in patients treated at medical centers and not in those treated at psychiatric hospitals. The most common AEs were insomnia, headache, constipation, and extrapyramidal syndrome. One or more serious AEs were reported in 11 (3.7%) patients; none resulted in death. No significant changes in body weight, plasma glucose, or lipid levels were observed.
Conclusion: Switching to paliperidone ER was effective and well tolerated for up to 24 weeks in patients with schizophrenia who were unresponsive or intolerant to previous antipsychotic therapy. The observed differences in treatment between psychiatric hospitals and medical centers with regard to dosage and titration of paliperidone ER warrant further investigation.
Keywords: prospective, switch study, open-label, paliperidone extended release, schizophrenia, settings
Introduction
Schizophrenia is a chronic illness that typically requires long-term treatment, with the primary goal of disease management being optimal control of symptoms. Unfortunately, ~40% of patients with schizophrenia do not adhere to their medication regimen at any given time.1 Factors contributing to nonadherence include poor symptom control, patients’ belief that medical therapy is unnecessary, and dissatisfaction due to adverse effects.2–4 Sustained symptom control with acceptable tolerability is critical for patients with schizophrenia to be able to engage in meaningful activities requiring adequate functioning, such as employment and education. Indeed, improved patient functioning has been shown to have a significant impact on long-term prognosis in patients with schizophrenia.5
Paliperidone extended release (ER; paliperidone ER; INVEGA®; Janssen, LP, Titusville, NJ, USA) is a once-daily oral psychotropic medication that is delivered via an osmotic controlled-release oral delivery system (OROS®; Alza Pharmaceuticals, Palo Alto, CA, USA) and approved for the treatment of schizophrenia by the US Food and Drug Administration and the European Agency for the Evaluation of Medicinal Products. The unique formulation allows for a controlled, gradually ascending release of paliperidone over a 24-hour period, thereby allowing treatment initiation at an effective dose without the need for dose titration to avoid tolerability issues.6 At steady state, minimal 24-hour peak-to-trough fluctuations in paliperidone plasma concentrations are observed with this formulation; minimal fluctuations may be associated with reduced side effects.7 In addition, paliperidone undergoes limited hepatic metabolism,8 which minimizes the risk of hepatic drug–drug or drug–disease interactions.
Paliperidone ER has been shown to be effective and is well tolerated in the treatment of acute schizophrenia in the the Western population.9,10 A recently published 24-week open-label extension study has confirmed the sustained efficacy and tolerability of paliperidone ER in Chinese patients with schizophrenia.11 However, data regarding its use in East Asian populations are still limited, particularly as a switch therapy. In this study, we assessed the efficacy and safety of paliperidone ER in patients with schizophrenia who were managed in non-acute settings in Taiwan and were unresponsive or intolerant to previous therapy. The primary objective was to assess the long-term efficacy, safety, and tolerability of paliperidone ER in this population.
Patients and methods
Subjects and treatment
This was a 24-week, multicenter, open-label, single-arm, Phase IV study of patients with schizophrenia who were managed in non-acute settings either at medical centers or psychiatric hospitals. Patients aged 18 years or older who had a diagnosis of schizophrenia according to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) criteria for at least 1 year were eligible for the study. Suitability for switching to paliperidone ER owing to lack of efficacy, tolerability, and/or adherence to previous oral atypical antipsychotic medication was judged and determined by each patient’s consulting psychiatrist. Exclusion criteria included a diagnosis of substance dependence within the past 6 months; medical conditions potentially affecting the absorption, metabolism, or excretion of the study drug; a history of neuroleptic malignant syndrome; a significant risk for suicide or violent behavior; pregnancy or lactation; treatment with clozapine; treatment with any long-acting injectable antipsychotic agent during the previous 3 months; and treatment with paliperidone palmitate as part of a clinical trial within the previous 10 months. The study was conducted in accordance with the Declaration of Helsinki and was approved by the local ethics committee or institutional review board at each center. Written informed consent was obtained from all patients before inclusion.
Switching of treatment was achieved by cross-tapering. Although dosing was based on the consulting psychiatrist’s discretion along with consideration of individual patients’ clinical characteristics, a starting dose of 6 mg was recommended. A higher initial dose could be considered by the investigators if the patient had uncontrolled symptoms; doses lower than those recommended could be considered for patients intolerant to previous therapy. The dose was titrated stepwise at increments of 3 mg, and a period of at least 1 week was required between dose adjustments. In general, the switching period was not allowed to exceed 4 weeks.
Efficacy and safety assessments
The visits were conducted at 2 weeks (visit 2), 4 weeks (visit 3), 12 weeks (visit 4), and 24 weeks (visit 5). Efficacy was determined based on changes from baseline in the following scores at each visit and at the end of the study using the last observation carried forward (LOCF) approach: Positive and Negative Syndrome Scale (PANSS) total score12 and PANSS Marder factor,13 Global Assessment of Functioning (GAF) scale,14 and Clinical Global Impression-Severity (CGI-S)15 score. The percentage of patients achieving a clinical response, defined as an improvement in the PANSS total score of 20% or more, was determined. Personal and social functioning were assessed using the Personal and Social Performance (PSP) scale, which has been validated in acutely ill and stable patients with schizophrenia.16,17 The PSP scale is a clinician-rated scale of personal and social functioning, with a score of 1 to 10 (on a 100-point scale) representing lack of autonomy in basic functioning and a score of 91 to 100 reflecting excellent functioning.18 The scale evaluates 4 domains of behavior: socially useful activities, including work and study; personal and social relationships; self-care; and disturbing and aggressive behaviors. In patients with acute schizophrenia, an improvement of at least one 10-point category represents a clinically meaningful difference.17 All efficacy outcomes were analyzed for patients overall and as grouped according to the type of facility at which they were treated (medical center or psychiatric hospital).
Safety was assessed based on the occurrence of treatment-emergent adverse events (AEs) reported by patients. The Extrapyramidal Symptom Rating Scale (ESRS) was used to assess 4 types of drug-induced movement disorders: parkinsonism, akathisia, dystonia, and tardive dyskinesia.19 Six ESRS factors were analyzed: hypokinetic parkinsonism, orofacial dyskinesia, trunk/limb dyskinesia, akathisia, tremor, and tardive dystonia.
Clinical and laboratory evaluations were performed at baseline and at 24 weeks and included blood pressure, pulse, body weight, body mass index, electrocardiography, hematology, and blood chemistry.
Statistical analyses
Efficacy variables were analyzed for the intent-to-treat population, which included patients who had received 1 or more doses of the study medication and had 1 or more post-baseline efficacy measurements. The safety analysis population included all patients who had received 1 or more doses of the study medication.
Descriptive statistics were used for all efficacy (using the LOCF approach) and safety parameters. Frequency distributions were generated for CGI-S, ESRS, PANSS, and PSP scale scores. For efficacy assessments, changes from baseline to each visit were tested for differences using the Wilcoxon signed-rank test (for ordinal/continuous data) and the Fisher’s exact test (for categorical data). Statistical tests for differences between end point (or visits) and baseline scores were interpreted at the 5% significance level (2-tailed). No adjustment was made for multiplicity. The p-value was set at 0.05 for all statistical tests.
Results
Baseline characteristics and disposition of patients
Of the 297 patients who were enrolled in the study from 9 centers (7 medical centers and 2 psychiatric hospitals), 178 (59.5%) completed the 24-week treatment. Reasons for discontinuation included insufficient efficacy (8.7%), patient decision (8.4%), AEs (6.4%), and loss to follow-up (5.4%). Demographic and baseline characteristics are summarized in Table 1. Overall, 46.1% of patients were male, and the mean age ± standard deviation (SD) was 40.1 ± 10.9 years. The mean age at the first onset of psychotic symptoms, at the first initiation of antipsychotic therapy, and at diagnosis of schizophrenia were 25.0, 27.1, and 27.9 years, respectively. A majority of patients (73.1%) had a DSM-IV diagnosis of paranoid schizophrenia. Reasons for switching from previous antipsychotic drugs to paliperidone ER included insufficient efficacy (74.1%), AEs (22.2%), and nonadherence to treatment (6.1%). A total of 136 patients (45.8%) switched to paliperidone ER from risperidone, 37 (12.5%) from olanzapine, and 27 (9.1%) from quetiapine. The percentage of patients starting treatment with paliperidone ER at 3, 6, and 9 mg was 40.8%, 53.1%, and 5.0%, respectively. The mean ± SD daily dose was 10.0 ± 2.38 mg over the entire treatment period.
  | Table 1 Patient demographics and baseline characteristics |
Efficacy
The Positive and Negative Syndrome Scale
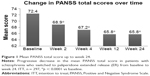
At the end of the treatment period (LOCF analysis), the mean ± SD PANSS total score improved from baseline by 6.9 ± 17.2 points (n = 297). The mean ± SD PANSS positive, negative, disorganized, and uncontrolled scores improved from baseline by 2.2 ± 5.6, 1.7 ± 4.4, 1.4 ± 4.4, and 0.5 ± 3.9 points, respectively (all p < 0.001). A decrease in mean PANSS total score of more than 5 points was noted after only 4 weeks of treatment (Figure 1). From visits 2 to 5, the proportion of patients achieving clinical response, defined as patients who achieved 20% or more improvement in the PANSS total score versus baseline, increased from 16.7% to 31.3%.
PANSS Marder factor scores
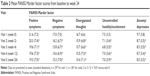
Mean PANSS Marder factor scores at all the visits were significantly lower than those at baseline (Table 2).
PSP scale, GAF scale, and CGI-S scores
Statistically significant improvements in mean PSP scale, GAF scale, and CGI-S scores from baseline were observed at all study visits (Table 3). From baseline to week 24, the median CGI-S score decreased from 4.3 to 3.9 (LOCF analysis), and the percentage of patients scoring as markedly ill, severely ill, or extremely severely ill decreased from 45.5% to 19.0%.
Medical centers versus psychiatric hospitals
Of the 297 patients, 215 (72.4%) and 82 (27.6%) received treatment at medical centers and psychiatric hospitals, respectively. Compared with patients treated at medical centers, those treated at psychiatric hospitals were older and had disease of longer duration and greater severity (Table 4). Both the PANSS total score and the CGI-S score improved statistically significantly only in patients treated at medical centers (Figure 2).
During the 24-week treatment period, 218 (73.4%) patients experienced at least 1 AE of any severity. Of the 857 total events, 339 (39.6%) were drug-related AEs, 11 (1.3%) were serious AEs (SAEs), and 2 (0.2%) were drug-related SAEs. Overall, 10 (3.4%) patients had SAEs.
Of the drug-related AEs, the most common were nervous system disorders (23.9%) and psychiatric disorders (18.2%). The former included extrapyramidal symptoms (8.8%), tremor (4.7%), and akathisia (5.7%), and the latter included insomnia (9.1%), anxiety (5.1%), and depression (3.0%; Table 5). The 2 drug-related SAEs were intracranial hemorrhage and auditory hallucination, which were reported separately in 2 patients. Quality of sleep did not improve significantly during the study period; however, a significant improvement in daytime drowsiness was reported (p < 0.05).
With regard to extrapyramidal symptoms, the mean ± SD ESRS total score significantly improved from 9.31 ± 11.7 at baseline to 8.17 ± 12.0 at the last visit (p < 0.005), mainly attributable to improvements in parkinsonism and akathisia. Body weight decreased from 66.2 ± 14.7 to 65.5 ± 14.5 kg (mean ± SD), and the decrease was nonsignificant. No clinically significant changes were noted in hematology profile, blood chemistry, or blood pressure.
Discussion
This is the first study conducted in Taiwan to evaluate the use of paliperidone ER in patients with schizophrenia. The switch to paliperidone ER therapy was associated with statistically significant improvements in symptom control, as reflected by changes in the PANSS total score as well as subscale scores. The efficacy of paliperidone ER as a switch therapy was demonstrated by a decrease of more than 5 points in the PANSS total score after 4 weeks of treatment. The proportion of patients achieving a clinical response increased from 16.7% at visit 2 to 31.3% at visit 5. In addition, improvements in the PANSS Marder factor scores demonstrate the broad spectrum of antipsychotic effects of paliperidone ER on different domains of schizophrenia, including positive symptoms, negative symptoms, uncontrolled hostility/excitement, and anxiety/depression.
Improving personal and social functioning is an essential component of optimizing long-term outcomes for patients with schizophrenia and is paramount to improving the prognosis.20 The results of this study show that paliperidone ER was effective in terms of improving patients’ daily functioning, as reflected by significant improvements in the PSP scale and GAF scores. Although a significant increase in the mean PSP scale score was observed within as early as 4 weeks of initiating treatment, a clinically relevant improvement was not achieved by the end of the study period; a longer duration of treatment may be required to achieve further improvements in personal and social functioning.
The participants in this study represented a heterogeneous group of patients who were managed in medical centers and psychiatric hospitals. Patients treated at psychiatric hospitals may be resistant to the therapeutic effects of a given drug owing to the longer duration and greater severity of their illness, and as such, prolonged duration of treatment and/or higher than normal doses may be required. On the contrary, as shown in Figure 3, the daily dose of paliperidone ER used to treat patients at psychiatric hospitals in this study was maintained between 3 and 6 mg throughout the study. However, for patients treated at medical centers, therapy was initiated at a dose of 3 to 6 mg, with subsequent up-titration to 9 to 12 mg. Analysis showed that in patients achieving a clinical response, the average doses of paliperidone ER used in medical centers and psychiatric hospitals were 7.0 and 5.4 mg, respectively. Considering that improvements in the mean PANSS total score and CGI-S score were observed only in patients treated at medical centers but not in those at psychiatric hospitals, it is possible that the greater efficacy observed in patients in medical centers was due to the shorter duration of their illness and timely titration of antipsychotics to their optimal doses. In fact, improvements in symptoms and functioning after 1 year of treatment with paliperidone ER have been observed to be greater in patients with recently diagnosed schizophrenia than in those with long-standing schizophrenia.21 Further studies are required to verify these results and to investigate the probable reasons for prescription of lower doses of antipsychotics in psychiatric hospitals in Taiwan, which may include local health insurance policies, physicians’ attitudes, and factors intrinsic to the institutions (medical centers vs psychiatric hospitals). Nevertheless, in other countries also, paliperidone was used at doses lower than those recommended by official guidelines, although the patients’ diseases were severe and chronic.
The implementation of a hospital-based global budget program in Taiwan significantly reduced expenditures on second-generation antipsychotics (SGA), with the extent of influence varying among institutions – global budgeting had less impact on SGA expenditures in psychiatric hospitals compared with medical centers.22 In addition, financial incentives derived from the program and compensation schemes were found to influence the adaptive behavior of hospitals and individual physicians. The reasons for the use of lower doses of paliperidone ER in psychiatric hospitals compared with medical centers observed in our study require further investigation, with additional factors such as therapeutic inertia being taken into consideration.
Paliperidone ER was generally well tolerated during the 24-week treatment period, and the findings are consistent with the known pharmacologic profile of paliperidone and comparable with those seen in completed Phase III studies.11,23 Most AEs related to paliperidone ER were tolerable and did not result in treatment discontinuation. Of note, switching to paliperidone ER did not exacerbate extrapyramidal symptoms and was shown to improve parkinsonism and akathisia.
Although considered superior to conventional agents in terms of safety profile, atypical antipsychotic agents have been associated with specific concerns related to adverse metabolic effects.24,25 Throughout the paliperidone ER treatment period, no clinically significant changes were observed in body weight, metabolic parameters, and blood pressure. These findings support the favorable metabolic profile of paliperidone ER observed in a previous 24-week double-blind trial.26 The efficacy and safety of paliperidone ER for the treatment of schizophrenia, including the use of a flexible dose regimen, have also been confirmed in the Chinese population.27,28
Limitations of this study include, but are not limited to, the open-label trial design and the lack of a comparator arm. A double-blind randomized controlled trial design is necessary to evaluate the effects of paliperidone ER as an initial or switch therapy in the management of schizophrenia in Taiwan. Another limitation is the lack of prolactin monitoring. Moreover, the effects of therapy should be analyzed separately for medical centers and psychiatric hospitals in future studies.
Conclusion
This 24-week study showed that paliperidone ER was effective and well tolerated as a switch therapy for patients with schizophrenia in Taiwan. The results suggest that higher doses (9 to 12 mg/day) are preferred for maintenance therapy in these patients. Further studies are needed to explore the effects of paliperidone ER in different settings.
Acknowledgments
The authors thank Susan Shu-Chuan Ho (Janssen Taiwan, Johnson and Johnson) for providing coordination and administrative assistance with the manuscript. Cactus Communications Pvt. Ltd. provided editorial assistance with the manuscript. This study was funded by Janssen Taiwan, Johnson and Johnson. Janssen Taiwan was involved in the study design, collection and analysis of data, and review of the manuscript.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Valenstein M, Ganoczy D, McCarthy JF, Myra Kim H, Lee TA, Blow FC. Antipsychotic adherence over time among patients receiving treatment for schizophrenia: a retrospective review. J Clin Psychiatry. 2006;67:1542–1550. | ||
Liu-Seifert H, Adams DH, Kinon BJ. Discontinuation of treatment of schizophrenic patients is driven by poor symptom response: a pooled post-hoc analysis of four atypical antipsychotic drugs. BMC Med. 2005;3:21. | ||
Yamada K, Watanabe K, Nemoto N, et al. Prediction of medication noncompliance in outpatients with schizophrenia: 2-year follow-up study. Psychiatry Res. 2006;141:61–69. | ||
Cooper C, Bebbington P, King M, et al. Why people do not take their psychotropic drugs as prescribed: results of the 2000 National Psychiatric Morbidity Survey. Acta Psychiatr Scand. 2007;116:47–53. | ||
Nasrallah HA, Targum SD, Tandon R, McCombs JS, Ross R. Defining and measuring clinical effectiveness in the treatment of schizophrenia. Psychiatr Serv. 2005;56:273–282. | ||
Kane J, Canas F, Kramer M, et al. Treatment of schizophrenia with paliperidone extended-release tablets: a 6-week placebo-controlled trial. Schizophr Res. 2007;90:147–161. | ||
Ereshefsky L, Mascarenas CA. Comparison of the effects of different routes of antipsychotic administration on pharmacokinetics and pharmaco-dynamics. J Clin Psychiatry. 2003;64:18–23. | ||
Vermeir M, Boom S, Naessens I, Talluri K, Eerdekens M, Hargarter L. Absorption, metabolism and excretion of a single oral dose of 14C-paliperidone 1 mg in healthy subjects. Eur Neuropsychopharmacol. 2005;15:S648–S649. | ||
Marder SR, Kramer M, Ford L, et al. Efficacy and safety of paliperidone extended-release tablets: results of a 6-week, randomized, placebo-controlled study. Biol Psychiatry. 2007;62:1363–1370. | ||
Meltzer HY, Bobo WV, Nuamah IF, et al. Efficacy and tolerability of oral paliperidone extended-release tablets in the treatment of acute schizophrenia: pooled data from three 6-week placebo-controlled studies. J Clin Psychiatry. 2008;69:817–829. | ||
Zhang H, Li H, Liu Y, et al. Safety and efficacy of paliperidone extended-release in Chinese patients with schizophrenia: a 24-week, open-label extension of a randomized, double-blind, placebo-controlled study. Neuropsychiatr Dis Treat. 2016;12:69–77. | ||
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. | ||
Marder SR, Davis JM, Chouinard G. The effects of risperidone on the five dimensions of schizophrenia derived by factor analysis: combined results of the North American trials. J Clin Psychiatry. 1997;58:538–546. | ||
Endicott J, Spitzer RL, Fleiss JL, Cohen J. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33:766–771. | ||
Guy W. ECDEU Assessment Manual for Psychopharmacology. Rockville, MD: U.S. Dept. of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976. | ||
Gagnon DD, Adriaenssen I, Nasrallah H, Morosini PL. Reliability, validity and sensitivity to change of the Personal and Social Performance scale in patients with stable schizophrenia. Int J Neuropsychopharmacol. 2006;9:S288. | ||
Patrick D, Adriaenssen I, Morosini PL, Rothman M. Reliability, validity and sensitivity to change of the Personal and Social Performance scale in patients with acute schizophrenia. Int J Neuropsychopharmacol. 2006;9:S287–S288. | ||
Morosini PL, Magliano L, Brambilla L, Ugolini S, Pioli R. Development, reliability and acceptability of a new version of the DSM-IV social and occupational social functioning assessment scale (SOFAS) to assess routine social functioning. Acta Psychiatr Scand. 2000;101:323–329. | ||
Chouinard G, Margolese HC. Manual for the Extrapyramidal Symptom Rating Scale (ESRS). Schizophr Res. 2005;76:247–265. | ||
Lambert E, Naber D. Current issues in schizophrenia: overview of patient acceptability, functioning capacity and quality of life. CNS Drugs. 2004;18:5–17. | ||
Canuso CM, Bossie CA, Amatniek J, Turkoz I, Pandina G, Cornblatt B. Paliperidone extended-release tablets in patients with recently diagnosed schizophrenia. Early Interv Psychiatry. 2010;4:64–78. | ||
Chiu HJ, Chou PH, Loh el-W, et al. Changes in the prescription pattern of antipsychotics for schizophrenic outpatients after the implementation of a global budgeting program. J Chin Med Assoc. 2014;77:325–332. | ||
Kramer M, Simpson G, Maciulis V, et al. One-year open-label safety and efficacy study of paliperidone extended-release tablets in patients with schizophrenia. CNS Spectr. 2010;15:506–514. | ||
Casey DE. Metabolic issues and cardiovascular disease in patients with psychiatric disorders. Am J Med. 2005;118:S15–S22. | ||
American Diabetes Association; American Psychiatric Association; American Association of Clinical Endocrinologists; North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. J Clin Psychiatry. 2004;65:267–272. | ||
Kramer M, Simpson G, Maciulis V, et al. Paliperidone extended-release tablets for prevention of symptom recurrence in patients with schizophrenia: a randomized, double-blind, placebo-controlled study. J Clin Psychopharmacol. 2007;27:6–14. | ||
Zhang L, Li J, Zhao Y, Su Y, Si T. Critical evaluation of paliperidone in the treatment of schizophrenia in Chinese patients: a systematic literature review. Neuropsychiatr Dis Treat. 2016;12:113–131. | ||
Zhang H, Li H, Liu Y, et al. Safety and efficacy of paliperidone extended-release in Chinese patients with schizophrenia: a 24-week, open-label extension of a randomized, double-blind, placebo-controlled study. Neuropsychiatr Dis Treat. 2016;12:69–77. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.