Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 12
Efficacy of Ustekinumab Against Spondyloarthritis Associated with Crohn’s Disease: A Case Report and Review of the Literature
Authors Matsumoto S , Matsumoto K, Takaya H, Otake H , Mashima H
Received 18 May 2020
Accepted for publication 14 July 2020
Published 29 July 2020 Volume 2020:12 Pages 133—137
DOI https://doi.org/10.2147/OARRR.S263259
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Chuan-Ju Liu
Satohiro Matsumoto, Keita Matsumoto, Hiromu Takaya, Haruka Otake, Hirosato Mashima
Saitama Medical Center, Jichi Medical University, Saitama, Saitama, Japan
Correspondence: Satohiro Matsumoto Email [email protected]
Abstract: Spondyloarthritis (SpA) is a known extraintestinal complication in inflammatory bowel disease (IBD). However, since the prevalence of SpA is lower in Japan than in Europe, some patients may be inaccurately diagnosed and treated. Although non-steroidal anti-inflammatory drugs (NSAIDs) remain the mainstay treatment for IBD-related SpA, anti-tumor necrosis factor-α antibody and ustekinumab have demonstrated efficacy in patients with SpA refractory to NSAIDs. We report here a case of Crohn’s disease with SpA, as an extraintestinal manifestation, in which ustekinumab proved extremely effective, not only for alleviating the arthritis but also against skin manifestations and scleritis. Only a few studies have documented the therapeutic effects of ustekinumab against SpA associated with IBD; therefore, its efficacy remains unclear.
Keywords: ustekinumab, spondyloarthritis, Crohn’s disease
Introduction
Spondyloarthritis (SpA) causes painful inflammation in the spine and/or the sacroiliac joints and is a family of multiple diseases, including ankylosing spondylitis (AS), psoriatic arthritis, reactive arthritis, uveitis, and inflammatory bowel disease (IBD)-associated spondyloarthropathy.1 SpA is associated with HLA-B27 and the prevalence of HLA-B27 in the Western European population is estimated between 4% and 13%.2,3 However, in Japan, the prevalence of HLA-B27 is extremely low (0.3%) in the general population, with the prevalence of SpA also reportedly low; therefore, some patients may be inaccurately diagnosed or treated as SpA.4
The frequency of AS associated with IBD is 2.1% in Crohn’s disease and 1.9% in ulcerative colitis, while that of peripheral arthritis is considered low at 8% and 6%, respectively.5 Although the frequency of SpA is not high, it is one of the extraintestinal manifestations or complications necessitating close monitoring by gastroenterologists. Non-steroidal anti-inflammatory drugs (NSAIDs) are used as the mainstay treatment for SpA but increase the risk of exacerbation of IBD.6–8 Therefore, the use of NSAIDs in IBD-related SpA (IBD-SpA) should be avoided when possible.9 We also occasionally encounter patients that fail to respond to NSAIDs. The effectiveness of anti-tumor necrosis factor-α antibody and ustekinumab, which is a human monoclonal antibody directed against the shared p40 subunit of interleukin (IL)-12 and IL-23, has been demonstrated in patients refractory to NSAIDs.8,10
Case Presentation
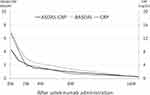
A 77-year-old Japanese woman diagnosed with Crohn’s disease of the small intestine had achieved remission with budesonide and maintained remission with mesalazine and enteral feeding. Six months after the initiation of therapy, she presented with fever, systemic punctate erythema, polyarthralgia, and bilateral coxalgia, with no relapse of gastrointestinal symptoms. Lower gastrointestinal endoscopy revealed that the lower ileal and colonic lesions were in remission. She was admitted to our hospital owing to difficulties in moving her body due to hip pain. On admission, she developed systemic punctate erythema with desquamation, polyarthralgia without redness and swelling, and hyperemia without ocular discharge on both bulbar conjunctiva (Figure 1). The white blood cell count was 2510/μL and the serum C-reactive protein (CRP) level was 13.4 mg/dL. Short tau inversion recovery (STIR)-magnetic resonance imaging (MRI) of the sacroiliac joints revealed hyperintense foci in the bilateral sacroiliac joints, especially on the right side (Figure 2A). She was diagnosed with sacroiliitis, peripheral arthritis, skin rash, and scleritis associated with Crohn’s disease; treatment was initiated with NSAIDs and a topical preparation. However, owing to the poor response of bilateral coxalgia to this treatment, the patient was started on ustekinumab therapy. The Ankylosing Spondylitis Disease Activity Score (ASDAS)-CRP11 and Bath Ankylosing Spondylitis Disease Activity Index (BASDAI)12 at the start of ustekinumab therapy were 4.3 and 7.0, respectively. Shortly thereafter, arthritis, skin eruptions, and scleritis resolved (Figure 3), and the hip pain gradually improved. Two months after the start of ustekinumab therapy, STIR-MRI of the sacroiliac joints showed improvement in the white matter hyperintensities (Figure 2B), the ASDAS-CRP and BASDAI were significantly improved to 0.98 and 1.4, respectively, and the serum CRP level decreased to 1.39 mg/dL (Figure 4). The patient has continued to receive ustekinumab every 8 weeks, with no relapse of any of the gastrointestinal, skin, and joint symptoms, including coxalgia. The HLA type determination performed later was positive for B52 and B54, but negative for B27.
 |
Figure 3 Complete resolution in the bilateral ocular conjunctiva (A), forearm (B), and abdomen (C) two months after one ustekinumab injection. |
Discussion
In addition to the characteristic intestinal lesions, IBD is also associated with various extraintestinal manifestations. The reported incidence of extraintestinal manifestations in patients with Crohn’s disease ranges from 25% to 46%.13,14 In a study investigating 244 patients with Crohn’s disease in Belgium, 65 (27%) were diagnosed with sacroiliac arthritis using X-ray, with 16 (6%) of these patients reportedly associated with AS.15 In Europe, the prevalence of HLA-B27 in patients with SpA is extremely high,16 and HLA-B27 is included in the classification criteria for axial SpA as proposed by the Assessment of Spondyloarthritis International Society in 2009.17 Conversely, the distribution of HLA-B type among 36 Japanese patients diagnosed with SpA is as follows: B61, 25.0%; B44, 25.0%; B35, 22.2%; B51, 19.4%; B52, 16.7%; B27, 5.6%. The distribution of HLA-B type in Japanese patients with SpA differs from that in Europe, and the frequency of HLA-B27 in Japan is considerably lower than that observed in Europe.1
The most common symptoms of early SpA are low back pain and back pain. The characteristic nature of SpA pain is to worsen in the early morning hours, causing sleep disturbance, and to improve with stretching and physical activity and worsen with prolonged inactivity. These symptoms are key to patient interviewing.18 Early detection, diagnosis, and treatment are required as SpA negatively influences the quality of life. X-ray investigations have been the gold standard for diagnostic imaging of SpA and one of the essential criteria for AS and axial SpA. As an average of 7 years is required for the appearance of characteristic findings on the X-ray,19 the classification criteria for axial SpA also includes MRI for diagnostic imaging.1 MRI is the most powerful tool for early diagnosis of SpA, and MRI findings of sacroiliac arthritis determine whether to initiate the administration of biological agents. Hence, the diagnosis of non-X-ray SpA (non-radiographic axial SpA) by MRI is recognized as a window of opportunity and is utilized to determine the time point at which effects of biological agents can be expected.20
Although the etiology of SpA remains unclear, a complex interaction between genes (HLA–B27) affected by microbiota in the intestinal tract or skin and innate and adaptive immune responses (Th17 pathway) has been implicated.21 The Th17 pathway (particularly IL-23) plays an important role in the pathogenesis of SpA.22 Ustekinumab is a human monoclonal antibody directed against the shared p40 subunit of IL-12 and IL-23, reportedly exerting its anti-inflammatory effects by inhibiting these ILs and their downstream proinflammatory cytokines, namely, interferon (IFN)-γ and IL-17, likely to be efficacious in SpA. Ustekinumab has demonstrated short- and mid-term efficacy in AS,23 and we have previously reported that ustekinumab was effective in patients with peripheral SpA.24 Conversely, the effect of ustekinumab on axial SpA failed to significantly differ from that observed in the placebo group after 24 weeks of therapy.16 Although evaluated using the visual analog scale, ustekinumab was reportedly ineffective in AS associated with Crohn’s disease,25 necessitating further cases for future investigations.26
In our case, ustekinumab was effective not only for SpA but also against scleritis. The efficacy of ustekinumab against extraintestinal manifestations of Crohn’s disease remains relatively unknown. Crohn’s disease with uveitis successfully treated with ustekinumab is reported.27 The efficacy of ustekinumab against ophthalmic disease as extraintestinal manifestations of IBD is expected.
Conclusion
We encountered a case of Crohn’s disease, in which ustekinumab was effective against SpA associated with Crohn’s disease, and additionally alleviated skin lesions and scleritis. Thus, ustekinumab can be effective against not only Crohn’s enteritis but also SpA and extraintestinal manifestations of Crohn’s disease.
Institutional Approval
No institutional approval was required for the publication of this manuscript.
Abbreviations
SpA, spondyloarthritis; AS, ankylosing spondylitis; IBD, inflammatory bowel disease; NSAIDs, non-steroidal anti-inflammatory drugs; IL, interleukin; CRP, C-reactive protein; STIR, short tau inversion recovery; MRI, magnetic resonance imaging; ASDAS, Ankylosing Spondylitis Disease Activity Score; BASDAI, Bath Ankylosing Spondylitis Disease Activity Index; IFN, interferon.
Ethical Considerations
Written informed consent was obtained from the patient for publication of this Case Report and the accompanying images.
Disclosure
All authors report no conflict of interest in this work.
References
1. Rudwaleit M, van der Heijde D, Landewé R, et al. The development of Assessment of Spondylo Arthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68(6):777–783. doi:10.1136/ard.2009.108233
2. Gill T, Asquith M, Rosenbaum JT, Colbert RA. The intestinal microbiome in spondyloarthritis. Curr Opin Rheumatol. 2015;27(4):319–325. doi:10.1097/BOR.0000000000000187
3. Mustafa KN, Hammoudeh M, Khan MA. HLA-B27 prevalence in Arab populations and among patients with ankylosing spondylitis. J Rheumatol. 2012;39(8):1675–1677. doi:10.3899/jrheum.120403
4. Tanaka H, Akaza T, Juji T. Report of the Japanese central bone marrow data center. Clin Transpl. 1996;139–144.
5. Malaty HM, Lo GH, Hou JK. Characterization and prevalence of spondyloarthritis and peripheral arthritis among patients with inflammatory bowel disease. Clin Exp Gastroenterol. 2017;10:259–263. doi:10.2147/CEG.S136383
6. Forrest K, Symmons D, Foster P. Systematic review: is ingestion of paracetamol or non-steroidal anti-inflammatory drugs associated with exacerbations of inflammatory bowel disease? Aliment Pharmacol Ther. 2004;20(10):1035–1043. doi:10.1111/j.1365-2036.2004.02270.x
7. Takeuchi K, Smale S, Premchand P, et al. Prevalence and mechanism of nonsteroidal anti-inflammatory drug-induced clinical relapse in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2006;4(2):196–202. doi:10.1016/S1542-3565(05)00980-8
8. Taurog JD, Chhabra A, Colbert RA. Ankylosing spondylitis and axial spondyloarthritis. N Engl J Med. 2016;374(26):2563–2574. doi:10.1056/NEJMra1406182
9. Pouillon L, Bossuyt P, Vanderstukken J, et al. Management of patients with inflammatory bowel disease and spondyloarthritis. Expert Rev Clin Pharmacol. 2017;10(12):1363–1374. doi:10.1080/17512433.2017.1377609
10. Torgutalp M, Poddubnyy D. Emerging treatment options for spondyloarthritis. Best Pract Res Clin Rheumatol. 2018;32(3):472–484. doi:10.1016/j.berh.2019.01.014
11. Lukas C, Landewé R, Sieper J, et al. Development of an ASAS-endorsed disease activity score (ASDAS) in patients with ankylosing spondylitis. Ann Rheum Dis. 2009;68(1):18–24. doi:10.1136/ard.2008.094870
12. Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol. 1994;21(12):2286–2291.
13. Ephgrave K. Extra-intestinal manifestations of Crohn’s disease. Surg Clin North Am. 2007;87(3):673–680. doi:10.1016/j.suc.2007.03.003
14. Shorbagi A, Bayraktar Y. Primary sclerosing cholangitis–what is the difference between east and west? World J Gastroenterol. 2008;14(25):3974–3981. doi:10.3748/wjg.14.3974
15. Peeters H, Vander Cruyssen B, Mielants H, et al. Clinical and genetic factors associated with sacroiliitis in Crohn’s disease. J Gastroenterol Hepatol. 2008;23(1):132–137. doi:10.1111/j.1440-1746.2007.05108.x
16. Deodhar A, Gensler LS, Sieper J, et al. Three multicenter, randomized, double-blind, placebo-controlled studies evaluating the efficacy and safety of ustekinumab in axial spondyloarthritis. Arthritis Rheumatol. 2019;71(2):258–270. doi:10.1002/art.40728
17. Otsuka A, Morita M, Yamada H. Clinical characteristics of Japanese patients with axial spondyloarthritis, and short-term efficacy of adalimumab. J Orthop Sci. 2015;20(6):1070–1077. doi:10.1007/s00776-015-0755-z
18. Dougados M, van der Linden S, Juhlin R, et al. The European spondylarthropathy study group preliminary criteria for the classification of spondylarthropathy. Arthritis Rheum. 1991;34(10):1218–1227. doi:10.1002/art.1780341003
19. Nakashima Y, Ohishi M, Okazaki K, et al. Delayed diagnosis of ankylosing spondylitis in a Japanese population. Mod Rheumatol. 2016;26(3):421–425. doi:10.3109/14397595.2015.1088679
20. Goh L, Samansa A. Update on biologic therapies in ankylosing spondylitis: a literature review. Int J Rheum Dis. 2012;15(5):445–454. doi:10.1111/j.1756-185X.2012.01765.x
21. Ranganathan V, Gracey E, Brown MA, Inman RD, Haroon N. Pathogenesis of ankylosing spondylitis - recent advances and future directions. Nat Rev Rheumatol. 2017;13(6):359–367. doi:10.1038/nrrheum.2017.56
22. Sherlock JP, Joyce-Shaikh B, Turner SP, et al. IL-23 induces spondyloarthropathy by acting on ROR-γt+CD3+CD4-CD8- entheseal resident T cells. Nat Med. 2012;18(7):1069–1076. doi:10.1038/nm.2817
23. Poddubnyy D, Hermann KG, Callhoff J, Listing J, Sieper J. Ustekinumab for the treatment of patients with active ankylosing spondylitis results of a 28-week, prospective, open-label, proof-of-concept study (TOPAS). Ann Rheum Dis. 2014;73(5):817–823. doi:10.1136/annrheumdis-2013-204248
24. Matsumoto S, Mashima H. Efficacy of ustekinumab against infliximab-induced psoriasis and arthritis associated with Crohn’s disease. Biologics. 2018;12:69–73. doi:10.2147/BTT.S169326
25. Liefferinckx C, Verstockt B, Gils A, et al. Long-term clinical effectiveness of ustekinumab in patients with Crohn’s disease who failed biologic therapies: a national cohort study. J Crohns Colitis. 2019;13(11):1401–1409. doi:10.1093/ecco-jcc/jjz080
26. Mease P. Ustekinumab fails to show efficacy in a phase III axial spondyloarthritis program: the importance of negative results. Arthritis Rheumatol. 2019;71(2):179–181. doi:10.1002/art.40759
27. Chateau T, Angioi K, Peyrin-Biroulet L. Two cases of successful ustekinumab treatment for non-infectious uveitis associated with Crohn’s disease. J Crohns Colitis. 2020;14(4):571. doi:10.1093/ecco-jcc/jjz167
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.