Back to Journals » Local and Regional Anesthesia » Volume 9
Efficacy of ultrasound-guided transversus abdominis plane block for postoperative analgesia in patients undergoing inguinal hernia repair
Authors Venkatraman R , Ranganathan Jothi A, Sakthivel A, Sivarajan G
Received 3 August 2015
Accepted for publication 29 October 2015
Published 18 January 2016 Volume 2016:9 Pages 7—12
DOI https://doi.org/10.2147/LRA.S93673
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Stefan Wirz
Rajagopalan Venkatraman, Ranganathan Jothi Abhinaya, Ayyanar Sakthivel, Govindarajan Sivarajan
Department of Anaesthesia, SRM Medical College Hospital and Research Centre, Chennai, Tamil Nadu, India
Background and aim: Transversus abdominis plane block (TAP block) is a novel procedure to provide postoperative analgesia following inguinal hernia surgery. The utilization of ultrasound has greatly augmented the success rate of this block and additionally avoiding complications. The aim of our study was to gauge the analgesic efficacy of ultrasound-guided TAP block in patients undergoing unilateral inguinal hernia repair.
Materials and methods: Sixty patients scheduled for elective inguinal hernia repair were selected for the study. At the end of the surgical procedure, they were randomly divided into two groups. Ultrasound-guided TAP block was performed with 20 mL of ropivacaine 0.2% (group A) or normal saline (group B). Visual analog scale (VAS) scores were used to assess pain. Paracetamol was given if VAS >3 and tramadol was used when VAS >6. Patients were monitored for VAS scores and total analgesic consumption for the 24-hour period.
Results: The TAP block with ropivacaine (group A) reduced VAS scores at 4, 6, and 12 hours. There was no distinction in VAS scores at 0, 2, and 24 hours between the two groups. The duration of analgesia for TAP block with ropivacaine lasted for 390 minutes. Total analgesics consumption was also significantly reduced in group A than group B. No complication was reported to TAP block in both the groups.
Conclusion: The ultrasound-guided TAP block provides good postoperative analgesia, reduces analgesic requirements, and provides good VAS scores with fewer complications following inguinal hernia surgery.
Keywords: inguinal hernia repair, postoperative analgesia, ropivacaine, transversus abdominis block, ultrasound
Introduction
Inguinal hernia surgery is one of the most commonly performed surgical procedures worldwide. Ilioinguinal nerve block provides good postoperative analgesia following inguinal hernia surgery. However, being a blind procedure, the failure rate is high. The transversus abdominis plane (TAP) block is an alternate, easy to perform, and an effective peripheral abdominal field block that blocks the ilioinguinal, hypogastric, and lower intercostal (T7–T11) nerves.1 TAP block is a novel technique for blocking the abdominal wall neural afferents via the lumbar triangle of Petit. The objective of a TAP block is to deposit local anesthetics within the plane between the internal oblique (IO) and transversus abdominis (TA) muscles targeting the spinal nerves in this plane.2 The TAP block has developed from a landmark-guided technique to ultrasound-guided technique. The continuous assessment of the drug injection between IO and TA muscles ensures distribution of the local anesthetics to the nerves lying underneath the fascia of TA muscle.3 TAP block has been utilized as a part of multimodal regime for postoperative analgesia following various surgical procedures such as large bowel resection,4 open appendectomy,5 retropubic prostatectomy,6 nephrectomy,7 hernia repair,8 laparoscopic cholecystectomy,9,10 and cesarean section.11
The objective of this prospective, randomized, double-blinded control study was to evaluate the analgesic efficacy of ultrasound-guided TAP block in patients following unilateral inguinal hernia repair. In this study, we analyzed the visual analog scale (VAS) pain score and total analgesic consumption following TAP block in inguinal hernia surgery.
Materials and methods
After receiving institutional ethical committee approval and written informed consent from patients, American Society of Anesthesiologists (ASA) I–II patients undergoing elective unilateral inguinal hernioplasty were enrolled into the study. Patients in the age group of 18–60 years and weighing between 50 and 80 kg were selected into the study. Patients with scrotal or recurrent hernia, bilateral hernia, irreducible, obstructed and strangulated hernia, hepatic or renal failure, and known allergy or contraindication to study drugs were excluded from the study.
The sample size was calculated on the basis of the 24-hour paracetamol requirement of patients undergoing inguinal hernia repair. For the purposes of sample size calculation, we believed that a clinically important reduction in 24-hour paracetamol consumption would be a 25% absolute reduction. This was a conservative assumption based on our pilot data. On the basis of initial pilot studies, we projected a 24-hour paracetamol requirement of 4 g, with a standard deviation of 1 g in the control group. We calculated that 25 patients per group would be required for an experimental design incorporating two equal sized groups, using an α;=0.05 and β=0.2. To minimize any effect of data loss, we elected to recruit 30 patients per group into the study.
All patients were premedicated with alprazolam 0.5 mg orally 2 hours before surgery. Heart rate, noninvasive blood pressure, and peripheral O2 saturation were continuously monitored during surgery and in the postoperative period. Spinal anesthesia was administered in all patients with 15 mg of heavy bupivacaine in the L3–L4 subarachnoid space. The surgery was started after checking the level of the blockade. All the surgeries were performed by three different surgeons available in our institute. They were explained of the study before the study was started. They all agreed that they will perform Lichtenstein tension-free meshplasty, which is the routine method in our hospital for open hernia repair. An anesthesiologist prepared 20 mL of either ropivacaine 0.2% or normal saline in a 20 mL syringe and he did not take further part in the study. At the end of surgery, after two segment regression of the level, ultrasound-guided TAP block was performed by second anesthesiologist who was blinded to the drug taken. The patients were randomly assigned to two groups with group A patients receiving 20 mL of ropivacaine 0.2% and group B patients receiving 20 mL of normal saline.
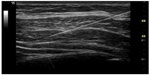
The abdominal wall was scanned using a high-frequency linear array transducer probe (6–13 MHz) in the multibeam mode, connected to a portable ultrasound unit. The ultrasound probe is positioned laterally toward the anterolateral part of the abdominal wall between the iliac crest and the subcostal margin. The orientation of the probe was perpendicular to a line joining the anterior superior iliac spine and the inferior rib to obtain a transverse view of the abdominal layers (respectively, from superficial to the depth, external oblique (EO), IO, TA, and, most deeply, peritoneal cavity). Following infiltration with lignocaine 1% (2 mL), an 80 mm, 22 G short-bevel needle was advanced using the in-plane insertion with ultrasound real-time assessment. The injection site was defined between aponeurosis of IO and TA muscles. When the tip was correctly located in the targeted plane, 20 mL of drug was injected with intermittent aspiration and correct placement of the needle was confirmed by expansion of the local anesthetic solution as a dark shadow between aponeurosis of the IO that moved anteriorly and the TA muscles pushing the muscle deeper.
Pain assessments were scored for all patients at rest and with coughing at 2, 4, 6, 12, and 24 hours after surgery by an anesthesiologist (independent observer) who did not know the group assignment. To assess pain, VAS was utilized and instructions were given for all patients prior to surgery.12 Patients were called upon to mark a point in the 10 point VAS scale according to the intensity of pain as shown in Figure 1.
  | Figure 1 Visual analog scale. |
Patients were given intravenous paracetamol if VAS >3, maximally four times a day at 6-hour intervals. At any time, if pain relief was inadequate (VAS >6), tramadol was given in a dose of 1.5 mg/kg intravenously. Total analgesic consumption in the 24-hour postoperative period was also recorded. Any complications related to interventions were noted as well.
Statistical analysis was performed using a standard statistical program, The Statistical Package for Social Sciences version 17.0 software (IBM Corporation, Armonk, NY, USA). Demographic data were analyzed using Student’s t-test. Measurements of pain scores were analyzed at each time interval performed using the unpaired t-test. Baseline variables were expressed as mean ± standard deviation, while pain scores were expressed as mean ± standard deviation and categorical data are presented as raw data and as frequencies. The level for all analyses was set at P=0.05 and a P-value less than 0.05 were considered statistically significant.
Results
Seventy-two patients were recruited into the study and a Consolidated Standards of Reporting Trials flow diagram depicting the passage of participants through the trial has been provided in Figure 2.
  | Figure 2 CONSORT flow chart. |
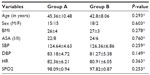
The two groups were comparable in terms of the basic demographic profiles (age, sex, weight, vital parameters, and ASA physical status) and given in Table 1. There was no statistical significance on the three surgeons operating in both the groups and given in Table 2.
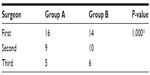  | Table 2 Number of patients operated by three surgeons |
There was no statistically significant difference in VAS scores at 0, 2, and 24 hours. But VAS scores were significantly less in group B at 4, 6, and 12 hours and given in Table 3. The time at which paracetamol was required was substantially longer in group A (439.50 minutes) than group B (233.50 minutes). The total paracetamol requirement in the first 24 hours were considerably less in group A (1.27±0.64 doses) than group B (2.53±0.68 doses). Similarly the tramadol requirement was more in group B (1.47±0.78 doses) than group A (0.6±0.49 doses).
  | Table 3 VAS score and analgesic consumption |
There were no significant variations in heart rate, blood pressure, and oxygen saturation in both the groups. No complication was reported in both the groups.
Discussion
The benefits of good postoperative analgesia include a reduction in the postoperative stress response and morbidity, better patient satisfaction and improved outcome.4 TAP block has gained acceptance in the recent years after Rafi13 initially described it in 2001 using the traditional anatomical landmarks. The TAP block is performed in the iliolumbar triangle of Petit, which is bounded superiorly by the lower coastal margins, inferiorly by the iliac crest, anteriorly by the EO and posteriorly by the latissimus dorsi muscles (Figure 3). The blunt technique utilizes a double-loss of resistance as the needle is advanced through the EO and IO fascia layers.14 The aim of TAP block is to place the tip of the needle between the IO and the TA muscles (Figure 4). The advantages of TAP block include simple and effective analgesic technique, appropriate for surgical procedures where parietal peritoneum is a significant component of postoperative pain, very minimal complication rate and can be performed even if neuraxial techniques are contraindicated.3 In surgeries where TAP block alone may not be adequate, it may be used as part of a multimodal pain regime. One major disadvantage of blind TAP block is the higher incidence of failure rate. The use of ultrasound has circumvented this problem and with experience, the success rate increases. With ultrasound, the spread of local anesthetic in the correct plane can be confirmed. The presence of ultrasound also allows us to use catheters thereby prolonging the duration of analgesia to as much duration as needed.
  | Figure 3 Ultrasound view. |
  | Figure 4 Needle placement in TAP block. |
In our study, the duration of postoperative analgesia with TAP block lasted for 440 minutes and there was a significant reduction in the consumption of other analgesics. The superiority of TAP block was also proved by the lower VAS score in group A than group B. Paracetamol was needed only after 440 minutes when VAS was more than 3. The most important finding from our study was the significant reduction in the consumption of other analgesics. Two patients did not receive any rescue analgesics for 24 hours. The prolonged duration of analgesia following TAP block may be because of its poor vascularity thereby causing delayed absorption. Bhattacharjee et al15 reported duration of postoperative analgesia to be 290 minutes following TAP block with bupivacaine, which are similar to our study. They also reported that four patients did not receive any rescue analgesia for 24 hours. There was no difference in pain scores in the first 2 hours in both the groups. This was explained by the postoperative analgesia offered by spinal bupivacaine in both the groups for the first 2 hours. There was also no difference in pain scores at 24 hours. This was because TAP block has regressed and patient had pain similar to control group.
Mukhtar and Khattak16 reported a significant reduction in the intraoperative morphine consumption following preincisional TAP block for renal transplant recipients. Tammam17 performed a study on TAP block for inguinal hernia through a catheter placed by ultrasound-guided Seldinger catheter insertion approach. The mean cumulative morphine requirement over the first 48 hours postoperative period was significantly less in the block group. In spite of the presence of the catheter, this study has examined only a single dose of 20 mL 0.25% bupivacaine with which they could demonstrate reduced analgesic requirement for 48 hours.
Sharma et al18 evaluated analgesic efficacy of TAP block after abdominal surgery. TAP block reduced VAS pain scores for up to 24 hours and not beyond that. Patients undergoing TAP block had reduced tramadol requirement for up to 48 hours. These findings correlate with our study. McDonnell et al4 performed a study on the analgesic efficacy of TAP block for patients undergoing large bowel resection. TAP block reduced VAS pain scores on emergence and at all postoperative time points, including at 24 hours. Morphine requirements in the first 24 hours were also reduced.
We did not encounter any complication in our study. Most of the other studies have also not reported any complication with TAP block. The advantage of TAP block is the safety profile of the block. However, the incidence of colon and liver injury has been reported with TAP block.17 Chandon et al19 performed a randomized trial on ultrasound-guided TAP block versus continuous wound infusion for postcesarean analgesia. The postoperative analgesia was randomized to either a bilateral TAP block (levobupivacaine 150 mg) or a continuous wound infusion. The study was prematurely terminated due to the occurrence of generalized seizures in one patient within the TAP group. This may have been because of the higher dose in a parturient or an accidental intravascular injection.
The major limitation of our study was that the duration of analgesia lasted no more than 24 hours. The catheter can be used to prolong the duration of analgesia. If we had calculated morphine requirement by patient-controlled analgesia, it would have given better results. Since we are not practicing it routinely in our hospital, we did not include it in our study.
Conclusion
TAP block significantly reduces the VAS pain score and analgesic requirement for up to 24 hours without any complications. The ultrasound has made the block easier to perform with a higher success rate. TAP block can safely be used as part of the multimodal pain regime for abdominal surgeries.
Disclosure
The authors report no conflicts of interest in this work.
References
Salman AE, Yetişir F, Yurekli B, Aksoy M, Yildirim M, Kilic M. The efficacy of the semi-blind approach of transversus abdominis plane block on postoperative analgesia in patients undergoing inguinal hernia repair: a prospective randomized double-blind study. Local Reg Anesth. 2013;6:1–7. | |
McDonnell JG, O’Donnell BD, Farrell T, et al. Transversus abdominis plane block: a cadaveric and radiological evaluation. Reg Anesth Pain Med. 2007;32:399–404. | |
Bonnet F, Berger J, Aveline C. Transversus abdominis plane block: what is its role in postoperative analgesia? Br J Anaesth. 2009; 103(4):468–470. | |
McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007;104:193–197. | |
Carney J, Finnerty O, Rauf J, Curley G, McDonnell JG, Laffey JG. Ipsilateral transversus abdominis plane block provides effective analgesia after appendectomy in children: a randomized controlled trial. Anesth Analg. 2010;111:998–1003. | |
O’Donnell BD, McDonnell JG, McShane AJ. The transversus abdominis plane (TAP) block in open retropubic prostatectomy. Reg Anesth Pain Med. 2006;31:91. | |
Hosgood SA, Thiyagarajan UM, Nicholson HF, Jeyapalan I, Nicholson ML. Randomized clinical trial of transversus abdominis plane block versus placebo control in live-donor nephrectomy. Transplantation. 2012;94:520–525. | |
Aveline C, Le Hetet H, Le Roux A, et al. Comparison between ultrasound-guided transversus abdominis plane and conventional ilioinguinal/iliohypogastric nerve blocks for day-case open inguinal hernia repair. Br J Anaesth. 2011;106:380–386. | |
El-Dawlatly AA, Turkistani A, Kettner SC, et al. Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth. 2009;102:763–767. | |
Petersen PL, Stjernholm P, Kristiansen VB, et al. The beneficial effect of transversus abdominis plane block after laparoscopic cholecystectomy in day-case surgery: a randomized clinical trial. Anesth Analg. 2012;115:527–533. | |
McDonnell JG, Curley G, Carney J, et al. The analgesic efficacy of transversus abdominis plane block after cesarean delivery: a randomized controlled trial. Anesth Analg. 2008;106:186–191. | |
Venkatraman R, Sandhiya R. Evaluation of efficacy of epidural butorphanol tartrate for postoperative analgesia. Int J Pharm Pharm Sci. 2015;7(2):52–54. | |
Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–1026. | |
Mukhtar K. Transversus abdominis plane (TAP) block. J N Y School Reg Anesth. 2009;12:28–33. | |
Bhattacharjee S, Ray M, Ghose T, Maitra S, Layek A. Analgesic efficacy of transversus abdominis plane block in providing effective perioperative analgesia in patients undergoing total abdominal hysterectomy: a randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2014;30:391–396. | |
Mukhtar K, Khattak I. Transversus abdominis plane block for renal transplant recipients. Br J Anaesth. 2010;104:663–664. | |
Tammam TF. Transversus abdominis plane block: the analgesic efficacy of a new block catheter insertion method. Egypt J Anaesth. 2014;30:39–45. | |
Sharma P, Chand T, Saxena A, Bansal R, Mittal A, Shrivastava U. Evaluation of postoperative analgesic efficacy of transversus abdominis plane block after abdominal surgery: a comparative study. J Nat Sci Biol Med. 2013;4:177–180. | |
Chandon M, Bonnet A, Burg Y, et al. Ultrasound-guided transversus abdominis plane block versus continuous wound infusion for post-caesarean analgesia: a randomized trial. PLoS One. 2014;9(8):1–6. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.