Back to Journals » International Journal of General Medicine » Volume 15
Efficacy of Primary Closure Technique in Treatment of Post-Sternotomy Mediastinitis in Paediatric Group: A Randomized Controlled Trial
Authors Fadaly AS, Abdellatif GM, Saeed SE, Brik A, Elsharawy M, Deebis A, Elfwakhry RM, Shemais DS
Received 2 September 2022
Accepted for publication 14 October 2022
Published 25 October 2022 Volume 2022:15 Pages 7929—7939
DOI https://doi.org/10.2147/IJGM.S388446
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Ahmed S Fadaly,1 Ghada Mohammed Abdellatif,2 Sameh E Saeed,1 Alaa Brik,1 Mamdouh Elsharawy,1 Ahmed Deebis,1 Rabab Mahmoud Elfwakhry,3 Dina Said Shemais1
1Department of Cardiothoracic Surgery, Faculty of Human Medicine, Zagazig University, Zagazig, Egypt; 2Department of Pediatric medicine, Faculty of Human Medicine, Zagazig University, Zagazig, Egypt; 3Department of Radiodiagnosis, Faculty of Human Medicine, Zagazig University, Zagazig, Egypt
Correspondence: Dina Said Shemais, Department of cardiothoracic surgery, Zagazig University, Zagazig, 44631, Egypt, Tel +201090726390, Email [email protected]
Purpose: To assess the efficacy of primary sternal closure technique compared to vacuum-assisted closure technique in treatment of post-cardiac surgery mediastinitis in paediatric age group. Additionally, assessed postoperative need for IV drug use, hospital stay length, wound and sternal healing and survival. Hypotheses: primary sternal closure is a reliable technique for treatment of poststernotomy mediastinitis following cardiac surgery in paediatric age group.
Materials and Methods: A prospective randomized controlled trial included 217 pediatric patients developed post-cardiac surgery mediastinitis from 2016 to 2022. They were randomly divided into primary sternal closure group (A) and vacuum-assisted closure group (B) and operated by two cardiothoracic surgeons. Follow-up of the patients was done for 6-months duration following treatment of mediastinitis to assess postoperative need for hospitalization, IV drug use, wound complications, sternal stability and survival.
Results: The final analysis included 101 patients in each group. The chance of survival over 6 months after surgery was more for primary sternal closure group (175.2) days versus (157.6) days for the vacuum-assisted closure group, with significant difference Log Rank test p-value (0.005). Duration for IV antibiotics use in the primary closure group was 8.55± 3.57 and it was 32.61± 8.39 showing high statistically significant difference (p< 0.001). Patients in the primary closure group had earlier discharge from hospital 15.77± 4.18 than vacuum assisted group 42.61± 8.39, with high statistically significant difference (p< 0.001). Primary closure group showed better sternal stability and sternotomy wound healing on clinical follow-up.
Conclusion: Primary sternal closure technique is a favorable technique over vacuum-assisted closure technique for treatment of paediatric mediastinitis following cardiac surgery. The reinforced sternal closure technique is a reliable technique with promising results regarding IV drugs need, hospitalization duration, survival and sternotomy wound healing.
Keywords: pediatric mediastinitis, post-cardiac surgery, primary closure, vacuum-assisted closure, interrupted mattress wires
Introduction
Postcardiac surgery mediastinitis is a serious complication.1 Mediastinitis in pediatric age group is annoying for patients and it is unacceptable by parents.6 It is associated with significant morbidity leading to significant longer hospital stay and higher costs. Mortality may occur in 10% to 25% of the mediastinitis cases.11
Documented risk factors for postoperative mediastinitis in the pediatric group are younger age, preoperative pneumonia and other respiratory tract infections, prolonged surgery duration, malnutrition, longer time on the mechanical ventilator and for and prolonged intensive care stay.5 Additionally, immunity is affected by operative manipulations and used materials like bone wax3 cardiopulmonary bypass, perioperative factors like postoperative bleeding and exploration, blood transfusion and anesthesia.2
Favorable prognosis of mediastinitis is detected in pediatric rather than adult patients.6 Although there are multiple procedures described for mediastinitis treatment, no concurrency about the optimal treatment strategy for pediatric mediastinitis. Protocols should be developed to help surgeons to manage this devastating complication.1
Surgical drainage with debridement8 and appropriate antibiotic regimen are considered as the corner stone for mediastinitis treatment. However, the best treatment strategy to fasten the healing of the wound is still controversial. There are some agreed points: 1) Surgical exploration for debridement of the infected tissues, foreign material removal and curettage of sternal halves edges until normal bleeding are essential; 2) Laboratory microbial tests for the collected purulent fluid and antibiotic susceptibility testing to confirm the diagnosis and antibiotic regimen needed; finally 3) Empirical antibiotics should be injected intravenously before surgery and modified according to microbial testing of the collected fluid. Following surgery, multiple conventional treatments were described like open dressing or closed irrigation, showing good results.6
Currently, the conventional treatments of mediastinitis include a debridement followed by sternotomy closure using vascularized soft tissue (omentum and muscle flaps for example), and a primary closure followed by several days of closed suction drainage, with or without antimicrobial irrigation. However, the details of the surgical treatment are still controversial.1
Vacuum-assisted closure is a technical innovation in wound care. However, the validity of its use for the management of post-sternotomy mediastinitis in pediatrics is unclear.9 Moreover, there is still controversy about the mechanism by which the vacuum technique improves wound healing.3 Negative pressure application shows several advantages: 1) Negative pressure enhances wound drainage; 2) Negative pressure application avoids any mediastinal cavity residual and ensures that the mediastinum contains healthy tissue; 3) Negative pressure aids in approximation of the wound edges and stabilization of the chest; and 4) Favorable improvement in local microcirculation have been described, which stimulates the formation of granulation tissue by maintaining a moist environment.4
A recent approach with early primary closure of post-sternotomy wound over a single chest tube for mediastinal drainage, mostly removed in 1 or 2 days was described. This simple technique offers comfort for the patient with interestingly high rate of success. However, this approach has failed in small number of patients. They needed surgical re-exploration due to prolonged sepsis and suspected ongoing mediastinitis. Moreover, there was a need for long course of intravenous antibiotics.6
We conducted this study to assess the efficacy of primary sternal closure with a modified wiring technique compared with vacuum-assisted sternal closure in the treatment of mediastinitis following cardiac surgery. We assessed postoperative IV drug use duration, hospitalization period, sternotomy wound stability and survival in both groups.
Materials and Methods
Ethical Statement
The Institutional review board of Zagazig University approved the study. The registration number of the study is (ZU-IRB#9859/28-1-2016). A written informed consent was taken from all parents of the patients included in the study. The study was conducted according to the ethical principles of the declaration of Helsinki.
Study Design and Population
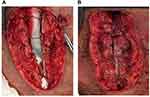
During seven years duration from 2016 to 2022, 4720 pediatric patients were operated by open heart surgery in three tertiary hospital institution (Zagazig University Hospitals, Atfal Misr Hospital and 6th October University Hospital). The study was performed in the aforementioned tertiary hospital institutions, as a prospective randomized controlled trial, to include all pediatric patients complaining from mediastinitis (Figure 1) after open heart surgery. The sample size in our study was calculated using open Epi to be 202 patients, 101 patients in each group. Assuming that difference in mortality rate was 2.4% following primary closure versus 14.3% following vacuum assisted closure, at CI 95% and study power 80%. Patients who developed mediastinitis were 217 patients (4.5%) initially screened for the study.
 |
Figure 1 A case of mediastinitis. It shows necrotic and devitalized soft tissue with involved sternal infection. |
Inclusion criteria were: 1) pediatric age group from 6 months to 14 years old. 2) patients operated for congenital heart lesions through the median sternotomy. 3) patients developed mediastinitis within 60 days post-cardiac surgery. 4) Haemodynamically stable patients.
Exclusion criteria were: 1) adult patients having mediastinitis. 2) pediatric mediastinitis not related to open heart surgery. 3) patients who developed mediastinitis after 60 days post cardiac surgery. 4) patients who had congenital lesion needing surgical intervention in addition to congenital heart lesions.
15 cases were excluded from the study. The final number of studied cases was 202. The studied cases were randomized by serially numbered closed envelopes by one of the authors other than surgeons who operated the cases into 2 equal groups. The envelopes that were serially numbered 1,3,5,…., for primary closure technique. The envelope was delivered to the surgeon at the day of the operation after the patient was in the operating room.
Group A (n=101) had primary closure technique for mediastinitis treatment and Group B (n=101) had vacuum-assisted closure for mediastinitis (Figure 2).
 |
Figure 2 Flow chart of the study (CONSORT flow chart). |
Surgical Technique
Two surgeons with over 10 years experience operated all patients. Complete aseptic precautions were followed in all patients. Debridement of all infected and devitalized bone, cartilage, muscle and soft tissue was done. Irrigation of the pericardial space with warm saline mixed with povidone iodine 7.5% concentration in a ratio of 2:1 was done. Chest tube was added in the mediastinum as a mediastinal drain.
In Group A, the sternum was primarily closed with stainless steel wire over a single chest tube. The technique of stainless steel wires was modified to add more support and reinforcement to the friable sternal halves and guarantee fixed closed sternum, thus preventing mediastinal dehiscence and bacterial tracking into the mediastinum. We used interrupted horizontal mattress sutures overlapped by interrupted simple wires. First we started with the horizontal mattress sutures, the wire was passed from left sternal half, from outside to inside, sliding on the lateral edge of the sternum. Then it was passed in the right sternal half from inside to outside on the same level opposite the left one. Then the wire was passed longitudinally on the right sternal half for about 2 Intercostal spaces and it was inserted from outside to inside to enter the adjacent intercostal space. Then the wire was passed to the left sternal half from inside to outside opposite the same level of the right one. That would result in formation of a horizontal (U) shaped suture with its base at the right of the sternum. Then a simple wire was passed at the middle of the base of (U) shaped suture lateral to from outside to inside. It was then passed from inside to outside at the same level in the right sternal half the opposite half, making sure that it is lateral to the two free arms of the U shaped suture.
This technique was repeated to involve all the sternal length. Then the U shaped sutures were pulled carefully one by one to re-approximate the sternal halves and were cabled on the left sternal half. After that, the simple wires were cabled lateral to the cabled horizontal mattress sutures (Figure 3A and B). Antesternal submuscular silicone suction drain was inserted. Running absorbable suture was used to close the soft tissue of the chest. The skin was closed with interrupted nonabsorbable suture. The mediastinal drain was managed as a routine and was removed when postoperative output had decreased generally after 24–48 hours. Subcutaneous drain It was removed, generally in 5 to 7 days.
Antibiotic Regimen for Primary Closure Group
Sensitive antibiotics were given intravenously for 7 to 12 days. It ranged from 4th generation cephalosporin (cefepime) to vancomycin if there is methicillin-resistant staphylococcus aureus bacteria.
Group B patients had one silicone round drain placed in the mediastinal space for drainage. The skin was reapproximated and covered, then the vacuum was applied. Suction drainage at about –70 mmHg was applied. The drain was followed up daily and repetitive cultures were done. The chest was closed when negative cultures were achieved in the mediastinum.
Antibiotic Regimen for Primary Closure Group
Sensitive antibiotics were given to patients, during vacuum as well as 2 to 4 weeks after closure of the chest. It ranged from 4th generation cephalosporin (cefepime) to vancomycin if there is methicillin-resistant staphylococcus aureus bacteria.
Nutrition of the Patients
Patients were appropriately fed either enterally or orally as much as possible according to age, weight and general condition.
Postoperative Follow Up of the Patients
During hospital stay, patients were followed up clinically and by laboratory investigation in the form of WBCS, ESR, CRP, and procalcitonin was done every 3 days to follow up the infection and detect sepsis early if present. Cultures were done from the drainage if present.
Plain CXR (anteroposterior and lateral views) was done for each patient before discharge and after 3 months of discharge. Plain CXR was assessed by a radiologist with over 5 years experience in cardiac and thoracic imaging. All images were processed and interpretation was carried out on the picture archiving and communication system (PACS) to detect if there is sternal gapping, antesternal and retrosternal collection if present.
The patients were followed up after they were discharged from hospital for 6 months in our outpatient clinic to record postoperative sternal stability, sternotomy wound infection and survival.
Statistical Analysis
Microsoft Excel was used to code, enter, and interpret the data. The data were then analyzed using the SPSS version 20.0. Data represent number and percentages of patients. Other data represent the mean ± standard deviation and range in parenthesis. The Chi-square test was applied to compare between the two studied groups. The correlation was done by the Pearson correlation test.
Results
Patients Characteristics
Our study enrolled 204 patients from the pediatric group complaining from mediastinitis after cardiac surgery. 2 cases lost to follow up, one patient in each group. Then the final analysis enrolled 202 patients, divided equally and randomly into 2 group; the primary closure group A and the vacuum-assisted closure group B. The flow chart of the studied patients is clarified in (Figure 2). The general characteristics of the studied patients in both groups are described in Table 1. There was no significant difference (P>0.05) between both groups regarding age and weight.
 |
Table 1 Patients Charcteristics |
Operative and Postoperative Data Following the Cardiac Surgery
Operative data are described in Tables 2 and 3. There was no significant difference (p>0.05) between both groups regarding surgical procedure, use of prosthetic material, Cardiopulmonary bypass time, ischemic time, need for re-exploration and ICU stay duration. All the above mentioned data are considered as risk factors for mediastinitis.
 |
Table 2 Surgical Procedures Performed for the Studied Groups Before Occurring of Mediastinitis |
 |
Table 3 Operative Data for the Studied Groups Following the Cardiac Surgery |
Postoperative Data Following Mediastinitis Treatment
These results are illustrated in Table 4. We noted a high statistically significant increase (P <0.001) in the time of intravenous antibiotics use and hospitalization period in the vacuum-assisted group compared to the primary closure group.
 |
Table 4 Postoperative Data After Treatment of Mediastinitis in the Studied Groups |
Postoperative Survival and Mortality
We found that the mean time of survival over 6 months duration for patients operated with primary closure was 175.2 days, versus 157.6 days for patients operated with vacuum assisted closure (Table 5). This means that the chance of survival is more for patients in the primary closure group, showing a significant difference Log Rank test p-value (0.005), clarified in Kaplan-Meier survival analysis (Figure 4). In the primary closure group, there were 3 cases of mortality (3%). One patient died before discharge due to aspiration pneumonia that needed mechanical ventilation followed by septic shock. Mortality occurred in another 1 patient 20 days after discharge from hospital due to pneumonia. The patient had aspiration pneumonia that needed mechanical ventilation and resulting septic shock. One patient died due cachexia, however, sternotomy wound cultures were negative. It is important to mention that the sternum was clinically stable, sternotomy wound showed no discharge, CXR showed no collection and negative laboratory results were confirmed before discharge.
 |
Table 5 Estimated Survival and Mortality of the Patients of Both Group |
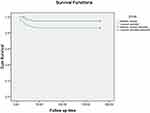 |
Figure 4 Kaplan-Meier survival analysis of studied cases according to type of intervention (n=202) over six months duration (180 days). |
In the vacuum-assisted closure group, there was 14 cases of mortality (13.9%). Seven patients died early within 15 days after surgical debridement and application of vacuum system due to septic shock. Four patients died within 35 days due to resultant haemodynamic unstability due to prolonged duration of vacuum-assisted use. Two patients died due to ventilator associated pneumonia (VAP) and septic shock. One patient died after he was discharged from hospital and negative cultures due to cachexia and poor general condition.
Discussion
Surgical site infections following cardiac surgeries result in increased morbidity, prolonged ICU and hospital stay as well as an increase in the cost of care on health institutions. Although there are multiple studies had evaluated the incidence and risk factors of sternotomy wound infections in the pediatric population, the optimum treatment of such infections is not documented yet.10,12
This study compared the postoperative outcome of primary closure of sternum with vacuum-assisted closure in pediatric mediastinitis following open heart surgery.
Primary sternal closure following debridement of the necrotic tissue had gained interest by cardiothoracic surgeons. This technique could overcome the need for plastic reconstructive surgery with acceptable results.7 Ohye et al found that primary closure is a simple and effective treatment for mediastinitis in children. It is appropriate for the majority of cases, more comfortable for the patient and achieves a high rate of success. They used simple stainless steel wires.13
We improved the simple sternal wiring technique to the reinforced wiring technique. In adults, reinforced sternal closure by different techniques by Robicsek, Daugherty, and Cook, titanium plates; stainless steel coils; or cables were suggested to be used in high-risk patients for wound complications and mediastinitis to minimize the incidence of sternal dehiscence and thus prevents bacterial tracking to the mediastinum.4,18 We supposed that reinforced wiring technique used in our study has the following advantages: 1) the transverse mattress sutures add more support to the devitalized friable sternum. 2) the added simple wires guarantee tight approximation of both sternal halves. 3) stable sternum prevents bacterial tracking into the mediastinum and recurrence of mediastinitis. 4) the interrupted sutures were intended to preserve the vascular blood supply of the sternum to allow fast, stable and appropriate sternal healing in the pediatric age group.
Plain CXR (posteroanterior and lateral views) was done before discharge (Figure 5A and B) and after 3 months (Figure 6A and B) on follow-up in our outpatient clinic. There was no sternal gapping, no retrosternal nor antesternal collections on serial follow-up of the patients included in primary closure group.
The hospital survival rates in Group A and Group B were 97% and was 86.1%, respectively. Patients were followed up after they were discharged from hospital for six months. The mean time of survival for cases operated with primary closure was 172.2 days, versus 157.6 days for the cases who had vacuum assisted closure. This means that the chance of survival was likely better for the primary closure group than vacuum-assisted group, with a significant difference Log Rank test p-value (0.02). Mortality was 3% in Group A and 13.9% in Group B.
Ohye et al found that hospital survival for the group of patients undergoing primary closure for mediastinitis was 97%.15 However, the patients require prolonged intravenous antibiotics course. The disadvantage of six weeks intravenous antibiotic treatment is the necessity of presence of a central venous line, because of small-sized patients and the poor peripheral venous tolerance to antibiotics.13 In our study, patients in the primary closure group had shorter duration of hospitalization (10–20 days) and shorter duration of IV antibiotics (7 to 12 days) guided by laboratory results and cultures. Moreover, the sternum was stable on clinical examination and there was no discharge in the mediastinal and antesternal drains. It was well tolerated by the patients, allows early mobilization of the patients and earlier discharge from the hospital.
The newly emerging vacuum-assisted closure technique showed success in small cohorts of pediatric patients.2,7 During the follow-up in the postoperative period of VAC group in our study, we found that there are constraints for the patient and medical team: 1) the vacuum-assisted closure system must be changed every 2 or 3 days, 2)repetitive cultures from the drains and laboratory indicators of infection were needed that remained positive for long time up to 45 days, 3) It was not tolerated by the patient, delayed patient mobilization, 4) Need for delayed closure after negative culture results was worrying to the parents, 5) Haemodynamics should be carefully monitored, 6) Additionally, prolonged ICU stay pre and post surgery was needed.
Durandy described limitations to the patients treated by vacuum-assisted closure that minimizes its efficacy.3 On the contrary, Onan et al found that vacuum systems ensure prevention of wound contamination, while the negative pressure applied prevents fluid retention in the mediastinum and prevents tissue edema. It also allows simultaneous stabilization of the chest. The overall mortality rate was 14.2% in their study.14 Additionally, patients can be mobilized early and can receive physiotherapy to minimize further complications.4
Ugaki et al suggest that there were limitations for VAC use. It should be preferably used when negative pressure has little effect on cardiac function like localized mediastinitis or steady circulation after recovery from a severe infection. Strong negative pressure in the mediastinum can be a risk for direct compression of cardiac cavities, causing decreased cardiac output, especially in cases of severe mediastinitis and/or marginal cardiac function resulting in deterioration of the circulatory system.17
During negative pressure application in adults, cardiac ruptures were described by the authors. The optimum negative pressure applied in pediatric patients is not determined yet. The risk of hemodynamic instability during negative pressure application is really worrying, especially in patients with Fontan- or Rastelli-type procedures; experimental data remains conflicting, and the best site for foam placement should be importantly localized.1,15,16
It is important to mention that the prevention of poststernotomy mediastinitis is the corner stone in all cardiac surgery operations. Strict follow-up to the guidelines and appropriate timing and dosage of prophylactic antibiotics should be considered.
Conclusion
Primary sternal closure technique is the favorable technique over vacuum-assisted closure technique for treatment of pediatric mediastinitis following cardiac surgery. The reinforced wiring technique using interrupted mattress sutures with added interrupted simple wires is a reliable wiring technique for sternal closure with promising results regarding the need of IV drugs and hospitalization need, wound and sternal healing and survival.
Abbreviations
CXR, chest x-ray; ICU, intensive care unit; IV, intravenous; VAC, vacuum-assisted closure.
Ethical Approval
Institutional review boards’ approval was obtained.
Informed Consent
Written informed consent was obtained from all patients.
Acknowledgment
The authors thank all staff members and colleagues in the Cardiothoracic, Pediatric and Radiology and Surgery Departments, Zagazig University, for their helpful cooperation.
Funding
The authors state that this work has not received any funding.
Disclosure
The authors of this manuscript declare no relevant conflicts of interest in this work.
References
1. Abu-Omar Y, Naik MJ, Catarino PA, Ratnatunga C. Right ventricular rupture during use of high-pressure suction drainage in the management of poststernotomy mediastinitis. Ann Thorac Surg. 2003;76:974. doi:10.1016/S0003-4975(03)00180-2
2. Al-Sehly A, Robinson J, Lee B, et al. Pediatric poststernotomy mediastinitis. Ann Thorac Surg. 2005;80:2314–2320. doi:10.1016/j.athoracsur.2005.05.035
3. Basha M, Shemais D, Abdelwahed E, et al. Computed tomography imaging assessment of the effect of vancomycin paste on poststernotomy healing. Int J Gen Med. 2021;14:9287–9296. doi:10.2147/IJGM.S343124
4. Cicco G, Tosi D, Crisci R, et al. Use of new cannulated screws for primary sternal closure in high risk patients for sternal dehiscence. J Thorac Dis. 2019;11(11):4538–4543. doi:10.21037/jtd.2019.10.79
5. Copeland H, Newcombe J, Yamin F, et al. Role of negative pressure wound care and hyperbaric oxygen therapy for sternal wound infections after pediatric cardiac surgery. World J Pediatr Congenit Heart Surg. 2018;9(4):440–445. doi:10.1177/2150135118772494
6. Durandy Y, Mediastinitis in pediatric cardiac surgery. Prevention, diagnosis and treatment. World J Cardiol. 2010;11:391–398. doi:10.4330/wjc.v2.i11.391
7. Fleck T, Simon P, Burda G, Wolner E, Wollenek G. Vacuum assisted closure therapy for the treatment of sternal wound infections in neonates and small infants. Interact Cardiovasc Thorac Surg. 2006;5:285–288. doi:10.1510/icvts.2005.122424
8. Hiramatsu T, Okamura Y, Komori S, Nishimura Y, Suzuki H, Takeuchi T. Vacuum-assisted closure for mediastinitis after pediatric cardiac surgery. Asian Cardiovasc Thorac Ann. 2008;16:e45–e46. doi:10.1177/021849230801600524
9. Kadohama T, Akasaka N, Nagamine A, et al. Vacuum-assisted closure for pediatric post-sternotomy mediastinitis: are low negative pressures sufficient? Ann Thorac Surg. 2008;85:1094–1096. doi:10.1016/j.athoracsur.2007.09.004
10. Levy I, Ovadia B, Erez E, et al. Nosocomial infections after cardiac surgery in infants and children: incidence and risk factors. J Hosp Inf. 2003;53:111–116. doi:10.1053/jhin.2002.1359
11. Mangukia C, Agarwal S, Satyarthy S, Datt V, Satsangi YD. Mediastinitis following pediatric cardiac surgery. J CARD SURG. 2014;29:74–82. doi:10.1111/jocs.12243
12. Nateghian A, Taylor G, Robinson JL. Risk factors for surgical site infections following open heart surgery in a Canadian pediatric population. Am J Infect Control. 2004;32:397–401. doi:10.1016/j.ajic.2004.03.004
13. Ohye R, Manike R, Graves H, Devaney E, Bove E. Primary closure for postoperative mediastinitis in children. J Thorac Cardiovasc Surg. 2004;128:480–486. doi:10.1016/j.jtcvs.2004.04.023
14. Onan I, Yildiz O, Tüzün B, Timur B, Haydin S. Vacuum‐assisted closure for mediastinitis in pediatric cardiac surgery: a single‐center experience. Artif Organs. 2019;43(2):119–124. doi:10.1111/aor.13321
15. Sartipy U, Lockowandt U, Gäbel J, Jidéus L, Dellgren G. Cardiac rupture during vacuum-assisted closure therapy. Ann Thorac Surg. 2006;82:1110–1111. doi:10.1016/j.athoracsur.2006.01.060
16. Steigelman MB, Norbury KC, Kilpadi DV, McNeil JD. Cardiopulmonary effects of continuous negative pressure wound therapy in swine. Ann Thorac Surg. 2009;88:1277–1283. doi:10.1016/j.athoracsur.2009.06.027
17. Ugaki S, Kasahara S, Arai S, Takagaki M, Sano S. Combination of continuous irrigation and vacuum-assisted closure is effective for mediastinitis after cardiac surgery in small children. Interact Cardiovasc Thorac Surg. 2010;11:247–251. doi:10.1510/icvts.2010.235903
18. Zeitani J, Peppo A, Moscarelli M, et al. Influence of sternal size and inadvertent paramedian sternotomy on stability of the closure site: a clinical and mechanical study. J Thorac Cardiovasc Surg. 2006;132(1):38–42. doi:10.1016/j.jtcvs.2006.03.015
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.