Back to Journals » Journal of Blood Medicine » Volume 13
Efficacy of Oxymetholone in Severe and Nonsevere Acquired Aplastic Anemia: A Propensity Score Matching Analysis
Authors Pengthina W , Saelue P
Received 10 August 2022
Accepted for publication 18 November 2022
Published 7 December 2022 Volume 2022:13 Pages 753—761
DOI https://doi.org/10.2147/JBM.S383148
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Worachaya Pengthina,1 Pirun Saelue2
1Pharmaceutical Care Training Center, Department of Pharmaceutical Care, Faculty of Pharmacy, Chiang Mai University, Chiang Mai, Thailand; 2Clinical Hematology Unit, Division of Internal Medicine, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand
Correspondence: Pirun Saelue, Clinical Hematology Unit, Division of Internal Medicine, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, 90110, Thailand, Tel +66 7445 1481 ; +66 81543 3031, Fax +66 7428 1457, Email [email protected]
Background: Bone marrow transplantation, antithymocyte globulin/cyclosporine and eltrombopag are recommended as first-line therapy of severe aplastic anemia (SAA). However, androgens could be considered as front-line treatment among any patients ineligible for better methods although unsatisfactory efficacy is presented.
Objective: This retrospective study aimed to evaluate response and survival rate of practical-based treatment with oxymetholone.
Patients and Methods: This constituted an analysis of patients receiving a diagnosis of acquired aplastic anemia (AA) at the age of 15 or over and receiving oxymetholone between January 2004 and December 2018. Propensity Score Analysis (PSA) 1:1 matching was performed, according to sex, age and interval from first symptom to treatment. The primary outcome was one-year overall response (OR).
Results: Seventy-four patients were successfully matched by PSA. The 1-year OR of oxymetholone in the nonsevere AA (nSAA) and SAA/very severe AA (vSAA) groups was 54.1 and 13.5%, respectively (P < 0.001). With median follow-up 2.7 years, the overall survival was 59.5% in nSAA and 37.8% in SAA/vSAA (P = 0.051). Median survival in nSAA and SAA/vSAA were 7.0 years and 1.8 years, respectively (P = 0.045). However, the responders of SAA/vSAA had longer survival than nonresponders of the nSAA group.
Conclusion: These results revealed longer survival among the responders of patients with AA, even in the SAA/vSAA group. However, close monitoring of therapeutic responses is still performed. Switching therapy is necessary when remission is undetected after 6 months of oxymetholone treatment.
Keywords: androgen, hematologic disease, real world practice, survival
Introduction
Aplastic anemia (AA) is a rare, life-threatening hematologic disease characterized by hypocellular bone marrow. Its incidence in Asian populations is 2 to 3 times higher than that of western countries.1 The severity of AA is classified as nonsevere (nSAA), severe (SAA) and very severe (vSAA) based on the peripheral blood and bone marrow of patients at diagnosis. The patients having AA with absolute neutrophil count (ANC) <1000 cells/µL are at increased risk of severe bacterial and fungal infection, leading to high morbidity and mortality. Specific treatments including bone marrow transplantation (BMT), eltrombopag, immunosuppressive therapy (ISTs) and androgen in addition to supportive care play a crucial role in improving their prognosis.2–4 However, the first-line treatment in AA depends on patients’ age, severity, availability of an HLA donor and patients’ decision-making.
Androgens are an alternative treatment option in SAA.4 The possible mechanism of action is enhanced erythropoietin production. One in vitro study showed the telomerase activity stimulation of androgens could result in hematologic improvement.5,6 The overall response rate of androgens was up to 50% among patients with nSAA.7 On the other hand, androgens have still shown a poor response of first-line treatment among patients with SAA/vSAA.7,8
In addition to some limitations of BMT, eltrombopag and ISTs including patients’ characteristics, HLA matching and the high cost of these treatment, oxymetholone is currently used for all AA severities in clinical practice even though the lower response or delay of response was presented in SAA and vSAA groups. Thus, this study was undertaken to evaluate response and survival of practical-based treatment with oxymetholone.
Materials and Methods
Study Design and Population
This retrospective cohort study enrolled patients receiving a diagnosis of acquired AA at the age of 15 or over and receiving oxymetholone between January 2004 and December 2018. AA severity was defined according to the Camitta Criteria.2 SAA was defined as bone marrow cellularity <25% (or 25 to 50% with <30% residual hematopoietic cells), plus at least two criteria of ANC <0.5 x 109/L, platelets <20 x 109/L and reticulocyte count <20 x 109/L. Very severe AA was defined similar to severe AA but ANC <0.2 x 109/L. Patients treated with antithymocyte globulin (ATG) or other androgens within three months before or after oxymetholone initiation were excluded. The eligible patients were followed until the end of study. When they died, were lost to follow-up or discontinue treatment, they were censored.
Response Assessment
Responding to treatment was divided in complete response (CR) and partial response (PR). CR was assessed by blood transfusion independent with all of the following conditions: hemoglobin >10 g/dL, platelet >100 x 109/L and ANC >1 x 109/L at least four weeks apart.9 PR was described as blood transfusion independent and no longer meeting the SAA criteria. The primary outcome was overall response rate (OR), which defined as a CR or PR, of oxymetholone at 12 months. The secondary outcomes included OR at 1, 3 and 6 months of treatment, relapse, 1-year overall survival (OS) and adverse events.
Statistical Analysis
In retrospective study, the possibility of selection bias due to confounding variables could occur in an estimate of treatment effects. Therefore, we performed propensity score matching to balance the distribution of covariates between nSAA and SAA/vSAA groups. The estimated propensity scores were calculated to predict the probability for each patient who received oxymetholone via a logistic regression using baseline variables including sex, age, and interval from first symptom to treatment. Patients with nSAA and SAA/vSAA were matched with one-to-one ratio.
Results were shown as frequency counts and percentages for categorical data while median and range were presented as continuous data. OR was shown as percent of responders and Fisher’s exact test was used to compare response rate between severity groups. The OS was analyzed using the Kaplan-Meier method and compared by the Log rank test. Factors associated with OS were determined using Cox proportional hazard models. P-value less than 0.05 was considered statistically significant.
Ethical Consideration
This study was approved by the Human Research Ethics Committee of Songklanagarind Hospital, Prince of Songkla University, as well as the hospital director. The research protocol followed in this retrospective study used an electronic medical records and hospital databases that were collected for routine medical care. We requested a waiver of informed consent for this study. All data will be anonymized to ensure privacy and confidentiality of patients’ personal information, with each participant assigned a unique identifier. This study is in line with the Declaration of Helsinki.
Results
One hundred and three patients were included in this study. Before matching, 59 patients were nSAA and 44 patients were SAA/vSAA (Figure 1). Fifty-five patients (53.4%) were male. The median age was 52.9 years, while nSAA group had a significantly higher median age (P = 0.015). The patients with SAA/vSAA had shorter duration from first symptom to treatment than those with nSAA (2.5 months vs 4.9 months, P = 0.034). The median dose of oxymetholone in the SAA/vSAA and nSAA groups was 150 mg/day and 100 mg/day, respectively (P = 0.009).
 |
Figure 1 Flow diagram of patient selection and study design. |
After propensity score analysis was performed, 74 patients were successfully matched. All imbalanced characteristics became well balanced without statistical differences. Baseline characteristics are shown in Table 1.
 |
Table 1 Baseline Characteristics of Patients |
The 1-Year Response Outcome
The 1-year OR of oxymetholone in the nSAA and SAA/vSAA groups were 54.1 and 13.5%, respectively (P < 0.001). The CR achievement was 13.5% for the nSAA group. Only one patient (2.7%) with SAA/vSAA achieved CR at eleventh month. However, this patient finally relapsed within six months after CR. Consequently, there was no CR reported at 1-year visit.
The 1-, 3-, and 6-Month Response Outcome
The percentage of responders at 1-, 3- and 6-month follow-up are shown in Figure 2. The response of oxymetholone was found within one month after treatment initiation for the nSAA group and after three months of treatment for the SAA/vSAA group. The median response time was 1.9 months and 5.8 months for nSAA and SAA/vSAA, respectively.
 |
Figure 2 The percentage of responders at 1-month, 3-month, 6-month and 12-month follow-up. |
The Relapse Rate and Factors Associated with Response
For a total of 40 responders, relapse was observed among 16 patients. Based on the number of responders in each group, the relapse rates were 45.5% (5/11) in SAA/vSAA group and 37.9% (11/29) in nSAA group. The median duration of relapse was 5.6 and 15.6 months for the SAA/vSAA and nSAA groups, respectively. Of a total of 16 relapsing patients, 13 died (4 patients in the SAA/vSAA group and 9 patients in the nSAA group).
Univariable and multivariable analysis showed that SAA/vSAA was associated with a lower response rate (OR=0.12, 95% CI: 0.02–0.61, P = 0.011). Baseline ANC ≥ 0.5 x109/L was associated with increased one-year response by univariable analysis (OR=3.94, 95% CI: 1.17–13.20, P = 0.026). However, we found no statistically significant association between baseline ANC and response in multivariable analysis (P = 0.845).
The One-Year Overall Survival
During median follow up of 2.7 years, the OS was 48.6% with median survival of 4.8 years. The survival rate was 59.5% for the nSAA group and 37.8% for the SAA/vSAA group (P = 0.051). The median survival for nSAA and SAA/vSAA were 7.0 years and 1.8 years, respectively (P = 0.045). However, in the response subgroup, median survival for nSAA was 13.0 years compared with 11.8 years for SAA/vSAA (P = 0.956) (Figure 3).
 |
Figure 3 Kaplan–Meier survival curves of overall survival analysis (A). Overall survival in patients with different severity and response (B). |
Factors Associated with Overall Survival
Univariable analysis showed the patients’ baseline characteristics that were significantly related to OS included baseline ANC <0.5x109/L (HR=2.23, 95% CI: 1.16–4.28, P = 0.016) and SAA/vSAA (HR=2.25, 95% CI: 1.17–4.33, P = 0.049). However, the multivariable analysis did not show any association of those variables and OS (P = 0.478 and P = 0.157, respectively). The univariable and multivariable analysis of factors associated with OS is provided in Table 2.
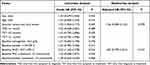 |
Table 2 Univariable and Multivariable Analysis for Overall Survival Among Acquired AA Patients |
Regarding subgroup analysis by severity, among patients with SAA/vSAA, univariable analysis demonstrated that time from first symptoms to treatment (TST) ≤3 months (HR=1.41, 95% CI 1.007–5.761, P = 0.048) and time from diagnosis to treatment (TDT) ≤1 month (HR=2.54, 95% CI 1.059–6.101, P = 0.037) were associated with higher OS (Table 3). However, significance was not found using multivariable analysis.
 |
Table 3 Univariable Analysis for Overall Survival in Acquired AA with nSAA and SAA/vSAA |
Survival Curves According to Time to Treatment Initiation
For nSAA group, the patients with early treatment had a longer median survival time (13.0 vs 6.7 years for TST ≤3 months and >3 months, respectively, P = 0.461 and median not reached vs 6.7 years for TDT ≤1 month and >1 month, respectively, P = 0.811).
On the other hand, for the SAA/vSAA group, the median survival time was significant greater in the longer TST group (0.6 vs 4.8 years for TST ≤3 months and >3 months, respectively, P = 0.042). The same value of median survival was presented in the longer TDT group (0.6 vs 4.8 years for TDT ≤1 month and >1 month, respectively, P = 0.031) (Figure 4).
Safety Outcomes
The most common adverse effect (AE) of oxymetholone was infection (64.8%), follow by impaired liver function (40.5%), bleeding (13.5%), virilization (12.1%) and other AEs (8.1%). Moderate to severe impaired liver function was a leading cause of treatment discontinuation (62.5%). Moreover, one patient wanted to discontinue oxymetholone because of increased appetite and weight gain although most patients could continue treatment after virilization was observed.
A total of 38 patients (51.4%) died during the study period. The most common cause of death was infection complications (42.1%). The other causes of death were malignancy (5.3%), bleeding (5.3%), nonAA-related causes (13.1%) and unknown (34.2%).
Discussion
Aplastic anemia is a serious hematologic disease. The mortality rate of disease improved dramatically after the era of BMT, eltrombopag and ISTs with ATG.9–12 Although ATG combined with and cyclosporine or eltrombopag is recommended as first-line treatment among patients with SAA ineligible for BMT,2,13 androgens are currently used for all AA severities in our setting due to financial barriers or lacking HSCT donors. This constitutes a retrospective study evaluating the efficacy of oxymetholone, one of androgens. The nSAA group showed higher one-year OR than that of the SAA/vSAA group (P < 0.001), as well as higher OS (P = 0.051). However, life expectancy could be prolonged among patients with SAA/vSAA responding to oxymetholone.
Androgens were forced to be used as monotherapy in limited resources countries and the efficacy of these agents was evaluated among patients with AA.8, 14–16 The response of oxymetholone was reported as 10% and 56% for SAA/vSAA and nSAA, respectively.8 Among responders, most patients responded to oxymetholone after six months of treatment.8 Furthermore, the median time to initial response was three months with danazol treatment.15 Similarly, this study revealed one-year ORs with 13.5% for SAA/vSAA and 54% for nSAA. The majority of our patients achieved response in six months after the beginning of treatment with the median time to response of 2.7 months. However, in comparison with one related study,14 the median time to PR and CR in this study was shorter (14.8 vs 3.0 months for PR, and 25.58 vs 10.0 months for CR). This difference could be affected by the severity proportion. As we know, SAA/vSAA has a longer median time response than nSAA. Accordingly, the longer median time to PR or CR was shown in the related study exhibiting the greater proportion of severe cases.
Many studies have presented OS ranging from 41 to 65% over two to five years.14–16 In this study, with the median follow up time of 2.7 years, 48.6% OS was observed. The SAA/vSAA group had a lower OS, and shorter median time as well. However, the responders of this group could prolong the median survival close to that of the responders of the nSAA group (11.8 years and 13.0 years, respectively). It revealed that oxymetholone could be considered for SAA on condition that BMT, ATG or eltrombopag was unaffordable. Nonetheless, the median survival time from the beginning of oxymetholone was about six months in both nSAA and SAA/vSAA groups. As a result, regimen should be changed if the response was not found within six months after initial treatment to prolong life and delay death.
Although the median survival in non-responders were 1.5 years and 0.7 years for nSAA and SAA/vSAA group, respectively. The prognosis was likely to be worse in nSAA group (Figure 3B). This finding might be a result of compliance and out-of-hospital treatment. However, this study could not evaluate these factors. Moreover, among eight non-responders in nSAA group, two of them were censored due to discontinue treatment from developing transaminitis.
Because of the high mortality among patients with SAA/vSAA receiving supportive care alone,17 the specific treatment should be started. Early treatment of AA has been associated with decreased risk of mortality. However, in the SAA/vSAA group, our study showed higher death among patients presenting shorter TST and TDT. This was probably the result of the reimbursement problem in our country. In the past, oxymetholone was considered as front-line therapy for SAA/vSAA even though poor efficacy was shown. As a result, although oxymetholone was initiated rapidly, the mortality rate remained high. In the delayed treatment group, any patients not responding to prior rabbit ATG/cyclosporine (CsA) was switched to oxymetholone. Although the study had a washout period of around three months, the survival effect of oxymetholone might also be influenced by the effects of rATG/CsA in that group. In addition to the benefit of rATG/CsA, because the rATG/CsA nonresponders died earlier, the remaining patients in the delayed-treatment group were those with better prognosis. Accordingly, lower mortality could be presented among those patients with delayed oxymetholone treatment.
The higher risk of infections, and main cause of death were related to the lower ANC of patients.13 ANC <5 x 109/L was presented as a factor influencing mortality.16 On multivariable analysis, we did not find significant differences between ANC <5 x 109/L and ANC ≥5 x 109/L. Undetectable association between neutrophil count and mortality could have been affected by the small sample size which was one of our limitations. The increasing number of samples might show the obvious relation of influencing factors. To confirm this finding, further study with a large sample size is required. Nevertheless, patients with lower ANC, particularly <5 x 109/L, should be focused on to prevent infection and reduce mortality.
In addition to the small sample size, the retrospective design was another limitation of our study. Nevertheless, we performed propensity score analysis to balance baseline characteristics and decrease confounding effects. Lastly, compliance and out-of-hospital treatment such as supportive treatments could not be collected. The prospective study should be done to confirm the results of our study.
Conclusion
This study revealed that oxymetholone showed a better response rate among patients with nSAA. However, with the lower mortality and longer survival time among the responders of the SAA/vSAA group, it could indicate these patients were ineligible for BMT, eltrombopag or ATG/CsA. Response of treatment should be monitored and switching therapy is necessary when the occurrence of remission is undetected within six months after the beginning of treatment.
Data Sharing Statement
Data available upon reasonable request to the corresponding author.
Ethics Approval
This study was approved by the Human Research Ethics Committee of Songklanagarind Hospital, Prince of Songkla University (approval number: REC.63-226-14-1).
Acknowledgments
We also thank to the officers of the division of Information Technology, Songklanagarind Hospital, Prince of Songkla University.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Disclosure
The authors declare that there are no conflicts of interest in this work.
References
1. Issaragrisil S, Kaufman DW, Anderson T, et al. The epidemiology of aplastic anemia in Thailand. Blood. 2006;107(4):1299–1307. doi:10.1182/blood-2005-01-0161
2. Killick SB, Bown N, Cavenagh J, et al. Guidelines for the diagnosis and management of adult aplastic anaemia. Br J Haematol. 2016;172(2):187–207. doi:10.1111/bjh.13853
3. Townsley DM, Scheinberg P, Winkler T, et al. Eltrombopag added to standard immunosuppression for aplastic anemia. N Engl J Med. 2017;376(16):1540–1550. doi:10.1056/NEJMoa1613878
4. Uaprasert N, Chansung K, Pongtanakul B, et al. Guideline for diagnosis and management of aplastic anemia in Thailand 2020. J Hematol Transfus Med. 2020;30(4):405–414.
5. Bär C, Huber N, Beier F, et al. Therapeutic effect of androgen therapy in a mouse model of aplastic anemia produced by short telomeres. Haematologica. 2015;100(10):1267–1274. doi:10.3324/haematol.2015.129239
6. Calado RT, Yewdell WT, Wilkerson KL, et al. Sex hormones, acting on the TERT gene, increase telomerase activity in human primary hematopoietic cells. Blood. 2009;114(11):2236–2243. doi:10.1182/blood-2008-09-178871
7. Gutiérrez-Serdán R, López-Karpovitch X. Acquired aplastic anemia: a demographic, clinical, and therapeutic survey of a single institution in Mexico City. Rev Hematol Mex. 2016;17(2):81–89.
8. Pizzuto J, Conte G, Sinco A, et al. Use of androgens in acquired aplastic anaemia. Relation of response to aetiology and severity. Acta Haematol. 1980;64(1):18–24. doi:10.1159/000207205
9. Gafter-Gvili A, Ram R, Gurion R, et al. ATG plus cyclosporine reduces all-cause mortality in patients with severe aplastic anemia-systematic review and meta-analysis. Acta Haematol. 2008;120(4):237–243. doi:10.1159/000203403
10. Ellis RJ, Kahn Q, Skikne BS, et al. A retrospective analysis of long-term survival in severe aplastic anemia patients treated with allogeneic bone marrow transplantation or immunosuppressive therapy with antithymocyte globulin and cyclosporin A at a single institution. Mil Med. 2002;167(7):541–545.
11. Paquette RL, Tebyni N, Frane M. Long-term outcome of aplastic anemia in adults treated with antithymocyte globulin: comparison with bone marrow transplantation. Blood. 1995;85(1):283–290. doi:10.1182/blood.V85.1.283.bloodjournal851283
12. Passweg JR, Marsh JC. Aplastic anemia: first-line treatment by immunosuppression and sibling marrow transplantation. Hematology Am Soc Hematol Educ Program. 2010;2010:36–42. doi:10.1182/asheducation-2010.1.36
13. Valdez JM, Scheinberg P, Nunez O, et al. Decreased infection-related mortality and improved survival in severe aplastic anemia in the past two decades. Clin Infect Dis. 2011;52(6):726–735. doi:10.1093/cid/ciq245
14. Argote VEF, Peñafiel COR, Sánchez M, et al. Androgen treatment for acquired aplastic anemia in Mexican adults. Blood. 2008;112(11):1046. doi:10.1182/blood.V112.11.1046.1046
15. Jaime-Perez JC, Colunga-Pedraza PR, Gomez-Ramirez CD, et al. Danazol as first-line therapy for aplastic anemia. Ann Hematol. 2011;90(5):523–527. doi:10.1007/s00277-011-1163-x
16. Mir MA, Delamore IW. Oxymetholone in aplastic anaemia. Postgrad Med J. 1974;50(581):166–171. doi:10.1136/pgmj.50.581.166
17. Dezern AE, Brodsky RA. Clinical management of aplastic anemia. Expert Rev Hematol. 2011;4(2):221–230. doi:10.1586/ehm.11.11
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

