Back to Journals » Cancer Management and Research » Volume 14
Efficacy of Osimertinib After Progression of First-Generation Epidermal Growth Factor Receptor-Tyrosine Kinase Inhibitor (EGFR-TKI) in EGFR-Mutated Lung Adenocarcinoma: A Real-World Study in Chinese Patients
Authors Xu Z , Hao X, Wang Q, Wang J, Yang K, Wang S, Teng F, Li J, Xing P
Received 25 October 2021
Accepted for publication 14 January 2022
Published 1 March 2022 Volume 2022:14 Pages 863—873
DOI https://doi.org/10.2147/CMAR.S346173
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sanjeev K. Srivastava
Ziyi Xu,1,* Xuezhi Hao,1,* Qi Wang,2 Jing Wang,2 Ke Yang,3 Shouzheng Wang,1 Fei Teng,1 Junling Li,1 Puyuan Xing1
1Department of Medical Oncology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, 100021, People’s Republic of China; 2Department of Medical Oncology, Beijing Chaoyang Sanhuan Hospital, Beijing, 100021, People’s Republic of China; 3Department of Medical Oncology, Cancer Hospital of Huanxing, Beijing, 100021, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Junling Li; Puyuan Xing, Department of Medical Oncology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, 100021, People’s Republic of China, Email [email protected]; [email protected]
Objective: Osimertinib is the standard targeted strategy for lung adenocarcinoma patients harboring epidermal growth factor receptor (EGFR)-activating mutation who have achieved acquired mutation T790M beyond progression of first-line EGFR-tyrosine kinase inhibitor (TKI). In a real world setting, the efficacy for osimertinib as a subsequent treatment beyond first-generation EGFR-TKI progression under complex circumstances such as different T790M mutation status is still worth exploring.
Methods: Records of 84 lung adenocarcinoma patients with an EGFR sensitive mutation who received first-generation EGFR-TKI as first-line therapy and sequenced by osimertinib after progression were retrospectively reviewed in this study. The assessment of efficacy of subsequent osimertinib treatment was evaluated by progression free survival (PFS), objective response rate (ORR), complete response (CR), partial response (PR), disease control rate (DCR) and stable disease (SD) rates. Relationship between PFS and clinicopathological characteristics was analyzed using univariate analysis.
Results: Until the median follow-up time of 23.7 months (IQR 10.8– 29.0 months), the median PFS (mPFS) of subsequent osimertinib was 17.0 months (HR 1.744, 95% CI, 13.547– 20.382). Among 60 patients who had at least one measurable lesion, 35.0% of patients (21/60) had PR to osimertinib, and 63.3% patients (38/60) had SD during osimertinib treatment. The ORR was 35.0%, and the DCR was 98.3%. Patients with acquired T790M mutation which was detected by NGS or ddPCR assay had an mPFS of 17.0 months (HR = 1.032, 95% CI, 14.941– 18.987), while the remaining 17 patients who had negative or unknown T790M mutation status had an mPFS of 23.5 months (HR = 9.404, 95% CI, 5.068– 41.932). No significant difference was observed in those with and without T790M mutation (P = 0.704).
Conclusion: Osimertinib may serve as an alternative subsequent choice after progression of first-generation EGFR-TKI in EGFR-mutated lung adenocarcinoma and may represent a potential treatment option for selected T790M-negative patients.
Keywords: osimertinib, progression, subsequent therapy, lung adenocarcinoma, T790M mutation
Introduction
Epidermal growth factor receptor (EGFR)-activating mutations, including mainly in exon 19 (19del) and exon 21 (L858R) mutations, have been confirmed as the main predictors of clinical outcome with targeted therapy in non-small cell lung cancer (NSCLC).1,2 EGFR-tyrosine kinase inhibitors (TKIs) are now a standard first-line therapy for NSCLC patients harboring EGFR-activating mutations, resulting in a 70% response rate and a prolonged progression-free survival (PFS).3 However, the majority of patients would develop acquired resistance to EGFR-TKIs,4 with the mean duration of initial response being 3 to 7 months.5,6 The mechanism of resistance is complex, and a threonine-to-methionine mutation at codon 790 (T790M) of the EGFR gene accounts for approximately 50% of acquired resistance to the first-generation EGFR-TKI gefitinib.4 Some patients would acquire MET amplification or EGFR amplification, and even mutations in PIK3CA.7
Osimertinib is a third-generation EGFR-TKI, known to be effective both as first-line therapy in NSCLC patients harboring the sensitive EGFR mutations,8 and in patients with the T790M resistant mutation after failure of prior TKIs, significantly prolonging progression free survival (PFS) compared to platinum and pemetrexed chemotherapy (10.1 months vs 4.4 months, P < 0.001).9 Osimertinib also has similar efficacy in the Asia-Pacific patient population harboring the EGFR T790M mutation, with a median PFS (mPFS) of 9.7 months (95% CI, 7.0–11.1).10 However, in patients who have not acquired the EGFR T790M mutation beyond the progression of first-generation EGFR-TKI, chemotherapy is still a recommended strategy by the National Comprehensive Cancer Network (NCCN) Guidelines. Continuation of EGFR-TKI combined with chemotherapy is not recommended, according to the results in the IMPRESS study, showing that continuation of gefitinib after progression on first-line gefitinib did not prolong PFS (5.4 months vs 5.4 months) in patients who received chemotherapy as subsequent therapy,11 and has even been detrimental to overall survival compared to chemotherapy plus placebo (13.4 months vs 19.5 months, P=0.016).12
In clinical practice, however, some patients could not tolerate chemotherapy after progression of first-line EGFR-TKIs, and thus received osimertinib even without detection of EGFR-T790M. Furthermore, the clinical utility of tissue rebiopsy has usually been limited by the lack of available tissue, costs, risk of complications, and turnaround times.13 Plasma circulating tumor DNA (ctDNA) has advantages over tissue biopsy in the perspectives mentioned above, and is recommended not only for EGFR sensitive mutations14 but also for acquired T790M mutation.15 The Cobas test, droplet digital polymerase digital chain reaction (ddPCR), and next generation sequencing (NGS) could be used in the detection of the T790M mutation in tumor DNA derived from ctDNA to identify patients for osimertinib treatment.16 In a real world setting, the efficacy of osimertinib as a subsequent treatment beyond first-generation EGFR-TKI progression under complex circumstances such as the combination of bevacizumab, with or without the T790M mutation, is still worth exploring.
Methods
Study Design
We retrospectively reviewed the records of advanced lung adenocarcinoma patients diagnosed by pathology and radiological results at the Cancer Hospital Chinese Academy of Medical Sciences (CAMS). Patients with EGFR sensitive mutations who received first-generation EGFR-TKIs as first-line therapy followed by osimertinib after progression were included. Inclusion criteria included the following: 1. Pathologically diagnosed as recurrent/metastatic lung adenocarcinoma; 2. Harboring typical EGFR 19del or 21L858R point mutation assessed by amplification refractory mutation system (ARMS)-PCR or NGS assay; 3. Progression after first-generation EGFR-TKIs as first-line therapy; 4. With or without EGFR exon 20 T790M mutation alone or co-occurring with other EGFR mutations confirmed by NGS or ddPCR with tissue or liquid biopsy after progression of prior TKI; 5. Patients who received osimertinib combined with or without bevacizumab as subsequent therapy prior to TKI, regardless of whether they had received chemotherapy or not. Having received local therapy such as palliative surgery, radiotherapy, radiofrequency ablation, intrathecal injection or intrapleural chemotherapy together with targeted therapy were allowed for inclusion. Patients who had other kinds of EGFR-TKIs or chemotherapy between first- and third-generation EGFR-TKIs were also included. Those who had no complete records or follow-up data were excluded from the analysis.
The present study was approved by the ethics committee of Cancer Hospital, CAMS and Peking Union Medical College (approval No. 21/245-2916). Informed consent was waived by the ethics committee.
Clinical Assessment
The assessment of efficacy of subsequent osimertinib treatment was based on the RECIST version 1.1.17 The indices of efficacy assessment were evaluated by progression free survival (PFS), overall survival (OS), objective response rate (ORR), complete response (CR), partial response (PR), disease control rate (DCR) and stable disease (SD) rates. PFS was defined as the period between the initiation of osimertinib to progression or death from any cause, and OS was defined as the period from the initiation of osimertinib treatment to death from any cause or the last follow-up. ORR was defined as the sum of CR and PR rates, and DCR was defined as the sum of the CR, PR and SD rates.
The relationship between PFS and clinicopathological characteristics was analyzed using univariate analysis, including age, gender, smoking history, tumor stage, brain metastases, best response to prior EGFR-TKIs, the presence of the T790M mutation, and the line of osimertinib. EGFR mutation status at diagnosis was also analyzed as a factor.
Gene Tests
EGFR sensitive mutations were detected by ARMS-PCR or NGS at baseline, with either tissue or cytohistology samples. The EGFR exon 20 T790M mutation was confirmed by plasma ctDNA or tissue biopsy when first-line EGFR-TKIs progressed. Most patients underwent NGS texting with another tissue or liquid biopsy, while some patients also had their plasma samples tested by ddPCR assay. The T790M mutation detected by either NGS or ddPCR was deemed positive in this study. After the progression of osimertinib, some patients underwent extra gene testing with tissue or ctDNA.
Statistical Analysis
Clinical characteristics and responses to therapy of patients were analyzed with descriptive statistics. The continuous and categorical data were presented as medians [quartile 1 (Q1) and quartile 3 (Q3)] and numbers (percentages), respectively. Continuous variables were compared by t-tests, and categorical variables were analyzed by χ2 tests. All statistical analysis was performed by utilizing SPSS version 26.0 (IBM Corp., Armonk, NY, USA), and a P value <0.05 was considered to be significant. Median PFS was calculated by the Kaplan-Meier product limit method. Hazard ratios (HR) and 95% CI were calculated using the Cox proportional hazards model. Risk factors for PFS were analyzed with the univariate Cox proportional hazards regression model, using the following covariates: age, gender, smoking history, tumor stage, brain metastases, best response to prior EGFR-TKI, the presence of T790M mutation, line of targeted therapy, and EGFR mutation status at diagnosis.
Results
Characteristics
From February 2017 to June 2021, 84 eligible patients were included in the study. Clinicopathological features of all enrolled patients are shown in Table 1. Most enrolled patients were females who never-smoked with a good performance status of 0–1. The median age of diagnosis of recurrent or metastatic disease was 56 years old (IQR 49–64 years old). In total, 59 patients (70.2%) had stage IIIB/IV disease when first diagnosed, while 25 patients (29.8%) had recurrence after resection, with or without adjuvant chemotherapy or adjuvant radiotherapy. Seventeen patients (20.2%) underwent rebiopsy on tissue to detect T790M using NGS assay. Four patients (4.8%) who had pleural effusion or leptomeningeal metastasis (LM) received thoracocentesis or rachicentesis to undergo NGS tests on pleural fluid or cerebrospinal fluid (CSF). The remaining 58 patients (69.0%) received NGS tests on ctDNA only. Among patients who received plasma gene tests, 42 patients (72.4%) were positive, 7 patients (12.1%) who were negative on NGS tests received further plasma tests using ddPCR assays and had positive results for the T790M mutation, and the remaining 9 patients (15.5%) had negative results on NGS tests or both. Twenty patients (23.8%) had been diagnosed with lung adenocarcinoma with brain metastases (BM) at baseline of first-generation EGFR-TKIs, including a limited number of LM. As for progression pattern of first-line EGFR-TKIs, 13 patients (15.5%) had intracranial progression or new lesions in the CNS, while the remaining 71 patients (84.5%) had non-CNS metastases. Therefore, a total of 26 patients (31.0%) had BM or LM prior to osimertinib.
Treatment
All enrolled patients were pathologically diagnosed with recurrent/metastatic NSCLC harboring sensitive EGFR exon 19 deletion or exon 21 L858R mutation and progressed after first-line EGFR-TKI icotinib, gefitinib, or erlotinib. Most patients (94.0%) underwent secondary tissue or liquid biopsy to detect the T790M mutation beyond progression. Two patients (2.4%) received one to two cycles of chemotherapy while awaiting NGS or ddPCR testing.
All patients then received osimertinib as subsequent therapy until progression or death, with no intolerable adverse events occurred. In total, 42 patients (50.0%) had received icotinib, 29 patients (34.5%) had received gefitinib, and the remaining 13 patients (15.5%) had received erlotinib as their first-line therapy. Fifteen patients (17.9%) had received a combination of first-generation EGFR-TKIs and the anti-angiogenic agent bevacizumab concurrently or when gradual progression occurred, with progression in no more than two nontargeted lesions, and with an asymptomatic status or stability of pre-existing symptoms.18 In total, 73.8% of patients (62/84) received osimertinib as second-line therapy, while the remaining 26.2% of patients (22/84) had subsequent chemotherapy or other EGFR-TKIs until they received osimertinib as third-line therapy. Thirty-eight patients (45.2%) underwent local therapy including palliative surgery, radiotherapy (RT), radiofrequency ablation (RTA) for regional lesions, intrathecal injection for LM, and intrapleural chemotherapy for pleural effusion, in addition to systemic treatment. The treatment strategy has been shown in Table 2.
 |
Table 2 Treatment Strategy of 84 EGFR-Mutated Lung Adenocarcinoma Patients Who Received Osimertinib After Progression of First-Generation EGFR-TKI |
Efficacy and Response to Osimertinib
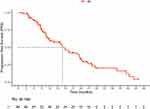
Until 8th October 2021, the median time of follow-up was 23.7 months (IQR 10.8–29.0 months). When 51 progression events (60.7%) and 22 survival events (26.2%) had occurred, the PFS of subsequent osimertinib was mature, while the OS was not. The median PFS1 of first-generation EGFR-TKIs was 17.9 months (HR 2.333, 95% CI, 13.287–22.433). The median PFS of subsequent osimertinib was 17.0 months (HR 1.744, 95% CI, 13.547–20.382), as shown in Figure 1. Eleven patients out of 51 patients (21.6%) who had progressed after osimertinib treatment had intracranial progression or new lesions in the CNS, while the remaining 40 patients (78.4%) had non-CNS metastases. Fourteen patients (27.5%) who had progression then underwent another gene test, among whom 35.7% patients (5/14) had the C797S acquired mutation. Among 60 patients who had at least one measurable lesion, only one patient (1.7%) had progressive disease at the first evaluation after osimertinib therapy (Table 3). Among these patients, 35.0% of patients (21/60) had a partial response to osimertinib, and 63.3% of patients (38/60) had stable disease during osimertinib treatment. The ORR was 35.0%, and the DCR was 98.3%.
 |
Table 3 Best Response to Osimertinib After Progression of First-Generation EGFR-TKI in 60 Advanced Lung Adenocarcinoma Patients Harboring EGFR-Activating Mutations with at Least One Measurable Lesion |
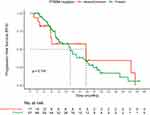
Risk Factors for PFS of Osimertinib
The PFS of osimertinib as a subsequent therapy for female patients and male patients was 17.9 months vs 16.5 months, respectively, with no significant difference observed (P = 0.231, HR = 1.442, 95% CI, 0.789–2.637). Patients harboring EGFR exon 19 deletion had similar mPFS to those with EGFR exon 21 L858R mutation (17.0 months vs 18.0 months), with no significant difference observed (P = 0.143, HR = 1.517, 95% CI, 0.865–2.661). Patients with acquired T790M mutation which was detected by NGS or ddPCR assay had a mPFS of 17.0 months (HR = 1.032, 95% CI, 14.941–18.987), while the remaining 17 patients who had negative or unknown T790M mutation status had a mPFS of 23.5 months (HR=9.404, 95% CI, 5.068–41.932). No significant difference was observed in those with and without the T790M mutation (P = 0.704), as was shown in Figure 2. The hazard ratio of PFS in patients with different characteristics using univariate analysis is shown in Figure 3.
Discussion
Osimertinib is a standard treatment for lung adenocarcinoma patients who have progressed after first-generation EGFR-TKIs with acquired T790M mutations, improving survival and response compared to traditional chemotherapy.9 Patients who have progression after first-line EGFR-TKIs are recommended to undergo a secondary biopsy to detect the T790M mutation, which accounts for only approximately 50% of this subpopulation.4 Systemic chemotherapy is recommended for patients who progress during or after first-line EGFR-TKIs without the T790M mutation by the NCCN guidelines, yet a better subsequent regimen is still under exploration. In clinical practice, obtaining tumor tissue is always difficult and costly, especially in patients with relapsed or metastatic disease, which makes liquid biopsy an alternative to detect acquired resistance mutations. There are still a group of T790M-negative patients who do not tolerate to cytotoxic agents or are unwilling to receive chemotherapy, and thus receive third-generation EGFR-TKIs as a subsequent choice, or after failure of second-line systemic chemotherapy. Some patients are even unaware of their gene status before making treatment decisions. Therefore, it is worthwhile to explore the efficacy of osimertinib under such complex situations, so as to determine more options and optimal strategies for lung adenocarcinoma patients harboring EGFR sensitive mutations who progress beyond first-line EGFR-TKIs.
Previously in a global real-world study, osimertinib demonstrated a similar clinical efficacy to clinical trials, with a mPFS of 11.1 months (95% CI, 11.0–12.0) observed in 3015 T790M-positive NSCLC patients.19 In our previous study that explored the efficacy of osimertinib in 94 NSCLC patients as subsequent therapy, the mPFS was 8.6 months (8.5 months as second-line therapy, 9.1 months as ≥3rd line therapy).20 For patients with detectable T790M mutation, the DCR and median PFS were 91.9% and 8.6 months (95% CI, 7.2 to 10.0), respectively, and were 80.0% and 3.2 months (95% CI, 0.5 to 5.9) for those without T790M mutations.20 In this real-world study, the efficacy of osimertinib in NSCLC patients harboring EGFR exon 19 deletion or exon 21 L858R mutation who had progression after first-generation EGFR-TKI, with or without T790M mutation detected by NGS or ddPCR was retrospectively analyzed. The mPFS of osimertinib in all patients enrolled was 17.0 months (HR 1.744, 95% CI, 13.534–20.382), comparably longer than previous studies,9 with 26.2% of patients who received osimertinib as third-line therapy after chemotherapy or other kinds of EGFR-TKIs. Among 60 patients who had at least one measurable lesion, the ORR was 35.0%, and the DCR was 98.3%. Although the ORR rate seemed poorer than that in the AURA3 study (71%),9 this study included not only patients harboring the T790M mutation but also those who had negative results or even unknown status in the real-world setting, and also those who received osimertinib as third-line therapy, which may influence the response rate.
In the dose-escalation cohorts of a study in which patients with activating EGFR mutations advanced NSCLC who developed resistance to first- or second-generation EGFR-TKI treatments received osimertinib at doses of 20 to 240 mg once daily, the response rate was 21%, and the median PFS was 2.8 months for those without centrally detectable T790M mutation, suggesting that osimertinib might also have moderate efficacy for such patients.21 In the Phase 2 TREM study in which NSCLC patients with progression on at least one previous EGFR-TKI received osimertinib regardless of the presence of T790M mutation, 120 (60%) were T790M-positive, 52 (26%) were T790M-negative and 27 (14%) had unknown T790M-status in 199 included patients.22 The ORR was 60% (51–69%) for T790M-positive patients and 28% (15–41%) for T790M-negative patients (p < 0.001); the median PFS were 10.8 months and 5.1 months for T790M-positive and T790M–negative patients, respectively (HR 0.62, p = 0.007); the median OS were 22.5 months and 13.4 months for T790M-positive and T790M–negative patients, respectively (HR 0.55, p = 0.002).22 This study has also indicated the clinically significant activity of osimertinib in a proportion of T790M-negative NSCLC patients. A Phase II study has recently been designed to assess the efficacy of osimertinib in patients with EGFR-mutated NSCLC who developed isolated CNS progression (T790M-negative or unknown) or systemic disease progression (T790M-negative) during first- or second-generation EGFR-TKIs or systemic disease progression with the background above.23 Notably, several patients in our study achieved a fine response to osimertinib even as third-line therapy, with 5 out of 17 patients (29.4%) with at least one measurable lesion having a partial response to third-line osimertinib and the other 12 patients (70.6%) having a stable disease, indicating that a broader population may benefit from osimertinib in later line. No significant difference was observed in those with and without the T790M mutation (P = 0.704) in our study, with the mPFS being 17.0 months (HR = 1.032, 95% CI, 14.941–18.987) for those with detectable T790M mutation, and 23.5 months (HR = 9.404, 95% CI, 5.068–41.932) for those with negative or unknown T790M mutation status. The reason for the observed activity of osimertinib in patients without the T790M-mutation in our study remains unclear, and might in part be due to false negative biopsies because of tumor heterogeneity. Moreover, the combination of localized therapy or anti-angiogenic agents might also contribute to the benefit in PFS. Based on our results, osimertinib might represent a potential treatment option for selected T790M-negative patients. Nevertheless, the long-term survival still requires a follow up.
Regarding the resistance mechanism, the most common EGFR tertiary mutation was EGFR C797S (14–24%), identified in EGFR T790M-preserved patients who progressed from osimertinib, and BRAF fusion or mutation accounted for 1–7% of resistance mechanisms, according to previous studies.24 In our previous study, that explored the resistance mechanisms of resistance to osimertinib, around 50% of patients maintained T790M mutations and 55.1% of patients experienced molecular modifications including EGFR acquired mutations such as C797S and C796S non-EGFR-dependent mutations such as PIK3CA and BRAF, EGFR amplification and MET amplification.25 In our current study, 14 patients underwent liquid biopsy after progression of osimertinib, among whom 8 patients (57.1%) had preserved EGFR T790M mutations, 5 patients (35.7%) had EGFR C797S mutations, and 1 patient (7.1%) acquired BRAF mutation beyond progressions. The results are comparable to previous reports and further investigation on mechanisms underlying resistance to osimertinib is still required in future studies.
Brain metastases (BMs) are one of the most common distant metastases in advanced lung cancer patients26 and have an unsatisfactory prognosis.27 It has been suggested that the incidence of BM increases over time in NSCLC patients harboring EGFR mutations during targeted treatment.28 Studies have shown that early-generation EGFR-TKIs show better CNS efficacy than chemotherapy, however, the high frequency of intracranial progression is still irresistible.29,30 Third-generation EGFR-TKIs have shown improved penetration and superior efficacy in the central nervous system (CNS) compared to first-generation EGFR-TKIs.31,32 In a real-world study from ASTRIS Korean Subset, the intracranial ORR and intracranial DCR were 62.5% and 93.8%, respectively, and the median intracranial PFS was 13.0 months (95% CI, 7.21–18.8).33 The study has indicated the potential role of osimertinib in T790M-positive NSCLC with BM or LM in the real-world setting. In our previous study, osimertinib achieved an intracranial ORR of 53.3% and an intracranial DCR of 80%, in 15 NSCLC patients with evaluable CNS metastasis sites after progression of early-generation EGFR-TKIs.34 Treatment options for BM also included surgery, radiotherapy (RT), and whole-brain radiotherapy (WBRT).35 However, the relapse rate in the CNS is still high, and local therapies are sometimes limited by their adverse events.36 There is still an urgent need for more alternative strategies beyond osimertinib. In our study, with 20 patients (23.8%) diagnosed as BM at baseline, and 6 patients (7.1%) progressed with new metastases in CNS after first-generation EGFR-TKI, a total of 26 patients (31.0%) were confirmed to have metastases in CNS (including 4 patients with LM) prior to osimertinib treatment. No significant difference in mPFS has been observed for patients with or without BM prior to osimertinib (P = 0.995). Median PFS for patients who have undergone RT or WBRT (10/26, 38.5%) was not significantly different from those who have not (P = 0.767). Similarly, mPFS for patients who have combined EGFR-TKI and bevacizumab (11/26, 42.3%) was not significantly different from those who have not (P = 0.781), probably due to the limitation of sample size in each subgroup.
Our study has several strengths. As it was designed in a real-world setting, the complex circumstances were taken into consideration so as to study the efficacy of subsequent osimertinib in the real-world, and to provide more information for a larger population. There are still several limitations in this study. First, the OS data were not mature by the date cutoff and needed further follow-up to explore long-term survival. Second, since a higher ratio of T790M may correlate with the osimertinib response,37 and because the detection of T790M using ddPCR may have different sensitivities compared to the NGS assay,16 it is assumed that the results from different assays indicated that the different ratios of T790M may differ in response to osimertinib. However, due to the limited sample size of patients who further received ddPCR when tested negative by NGS, the difference made by gene testing remained unknown in this retrospective study. Therefore, we are carrying out a prospective trial, studying the efficacy of osimertinib in patients who progressed beyond first- and second-generation EGFR-TKIs and who were T790M positive via ddPCR test but negative via NGS assay, to further explore this issue. Other limitations included the failure to demonstrate whether the presence of concomitant genes would influence the efficacy of subsequent osimertinib and survival in patients who received the regimen. According to previous studies, EGFR-mutant NSCLC patients with concomitant mutations at baseline were more likely to have shorter PFS than with those without a concomitant mutation (6.20 months vs 18.77 months),38 and that a dual blockade of EGFR and VEGFR pathways may improve survival in those with concomitant mutations.39 Due to limited genomic detection information offered in this study, we failed to determine the relationship between concomitant genes and the efficacy of subsequent osimertinib, and whether the combination of bevacizumab would improve the survival of such patients. It is still essential to obtain more genomic detection information and to design further prospective studies to further elucidate the relationship of genetic alternatives and survival. Further investigation on the resistance mechanism of osimertinib is still required, too.
Conclusion
Osimertinib may serve as an alternative subsequent choice after progression of first-generation EGFR-TKIs in EGFR-mutated lung adenocarcinoma, and may represent a potential treatment option for selected T790M-negative patients.
Ethics
The present study was approved by the ethics committee of Cancer Hospital, CAMS and Peking Union Medical College (approval No. 21/245-2916). Informed consent was waived by the ethics committee due to the retrospective nature of review. As patient consent to review their medical records was not required by the ethics committee, the data was maintained with confidentiality and this study was performed in compliance with the Declaration of Helsinki.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362:2380–2388. doi:10.1056/NEJMoa0909530
2. Mitsudomi T, Morita S, Yatabe Y, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010;11:121–128. doi:10.1016/S1470-2045(09)70364-X
3. Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947–957. doi:10.1056/NEJMoa0810699
4. Kobayashi S, Boggon TJ, Dayaram T, et al. EGFR mutation and resistance of non-small-cell lung cancer to gefitinib. N Engl J Med. 2005;352:786–792. doi:10.1056/NEJMoa044238
5. Kris MG, Natale RB, Herbst RS, et al. Efficacy of gefitinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in symptomatic patients with non-small cell lung cancer: a randomized trial. JAMA. 2003;290:2149–2158. doi:10.1001/jama.290.16.2149
6. Fukuoka M, Yano S, Giaccone G, et al. Multi-institutional randomized phase II trial of gefitinib for previously treated patients with advanced non-small-cell lung cancer (the IDEAL 1 trial) [corrected]. J Clin Oncol. 2003;21:2237–2246. doi:10.1200/JCO.2003.10.038
7. Sequist LV, Waltman BA, Dias-Santagata D, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med. 2011;3:75ra26. doi:10.1126/scitranslmed.3002003
8. Soria JC, Ohe Y, Vansteenkiste J, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2018;378:113–125. doi:10.1056/NEJMoa1713137
9. Mok TS, Wu YL, Ahn MJ, et al. Osimertinib or platinum-pemetrexed in EGFR T790M-positive lung cancer. N Engl J Med. 2017;376:629–640. doi:10.1056/NEJMoa1612674
10. Zhou C, Wang M, Cheng Y, et al. P3. 02b-096 osimertinib (AZD9291) in Asia-Pacific patients with T790M mutation-positive advanced NSCLC: open-label phase II study results: topic: EGFR RES. Thorac Oncol. 2017;12:S1250. doi:10.1016/j.jtho.2016.11.1763
11. Soria JC, Wu YL, Nakagawa K, et al. Gefitinib plus chemotherapy versus placebo plus chemotherapy in EGFR-mutation-positive non-small-cell lung cancer after progression on first-line gefitinib (IMPRESS): a phase 3 randomised trial. Lancet Oncol. 2015;16:990–998. doi:10.1016/S1470-2045(15)00121-7
12. Mok TSK, Kim SW, Wu YL, et al. Gefitinib plus chemotherapy versus chemotherapy in epidermal growth factor receptor mutation-positive non-small-cell lung cancer resistant to first-line gefitinib (IMPRESS): overall survival and biomarker analyses. J Clin Oncol. 2017;35:4027–4034. doi:10.1200/JCO.2017.73.9250
13. Goldman JW, Noor ZS, Remon J, Besse B, Rosenfield N. Are liquid biopsies a surrogate for tissue EGFR testing? Ann Oncol. 2018;29:i38–i46. doi:10.1093/annonc/mdx706
14. Gray J, Okamoto I, Sriuranpong V, et al. OA 05.02 osimertinib vs SoC EGFR-TKI as first-line treatment in patients with EGFRm advanced NSCLC (FLAURA): plasma ctDNA analysis. Thorac Oncol. 2017;12:S1754–S1755. doi:10.1016/j.jtho.2017.09.348
15. Wang Z, Chen R, Wang S, et al. Quantification and dynamic monitoring of EGFR T790M in plasma cell-free DNA by digital PCR for prognosis of EGFR-TKI treatment in advanced NSCLC. PLoS One. 2014;9:e110780. doi:10.1371/journal.pone.0110780
16. Papadimitrakopoulou VA, Han JY, Ahn MJ, et al. Epidermal growth factor receptor mutation analysis in tissue and plasma from the AURA3 trial: osimertinib versus platinum-pemetrexed for T790M mutation-positive advanced non-small cell lung cancer. Cancer. 2020;126:373–380. doi:10.1002/cncr.32503
17. Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000;92:205–216. doi:10.1093/jnci/92.3.205
18. Chaft JE, Oxnard GR, Sima CS, Kris MG, Miller VA, Riely GJ. Disease flare after tyrosine kinase inhibitor discontinuation in patients with EGFR-mutant lung cancer and acquired resistance to erlotinib or gefitinib: implications for clinical trial design. Clin Cancer Res. 2011;17:6298–6303. doi:10.1158/1078-0432.CCR-11-1468
19. Marinis F, Wu YL, de Castro G
20. Mu Y, Xing P, Hao X, Wang Y, Li J. Real-world data of osimertinib in patients with pretreated non-small cell lung cancer: a retrospective study. Cancer Manag Res. 2019;11:9243–9251. doi:10.2147/CMAR.S221434
21. Jänne PA, Yang JC, Kim DW, et al. AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med. 2015;372:1689–1699. doi:10.1056/NEJMoa1411817
22. Eide IJZ, Helland Å, Ekman S, et al. Osimertinib in T790M-positive and -negative patients with EGFR-mutated advanced non-small cell lung cancer (the TREM-study). Lung Cancer. 2020;143:27–35. doi:10.1016/j.lungcan.2020.03.009
23. Takeda M, Shimokawa M, Nakamura A, et al. A phase II study to assess the efficacy of osimertinib in patients with EGFR mutation-positive NSCLC who developed isolated CNS progression (T790M-negative or unknown) during first- or second-generation EGFR-TKI or systemic disease progression (T790M-negative) after treatment with first- or second-generation EGFR-TKI and platinum-based chemotherapy (WJOG12819L). Clin Lung Cancer. 2021;22:376–380. doi:10.1016/j.cllc.2020.12.009
24. Zhang YC, Zhou Q, Wu YL. Clinical management of third-generation EGFR inhibitor-resistant patients with advanced non-small cell lung cancer: current status and future perspectives. Cancer Lett. 2019;459:240–247. doi:10.1016/j.canlet.2019.05.044
25. Mu Y, Hao X, Xing P, et al. Acquired resistance to osimertinib in patients with non-small-cell lung cancer: mechanisms and clinical outcomes. J Cancer Res Clin Oncol. 2020;146:2427–2433. doi:10.1007/s00432-020-03239-1
26. Riihimäki M, Hemminki A, Fallah M, et al. Metastatic sites and survival in lung cancer. Lung Cancer. 2014;86:78–84. doi:10.1016/j.lungcan.2014.07.020
27. Ulahannan D, Khalifa J, Faivre-Finn C, Lee SM. Emerging treatment paradigms for brain metastasis in non-small-cell lung cancer: an overview of the current landscape and challenges ahead. Ann Oncol. 2017;28:2923–2931. doi:10.1093/annonc/mdx481
28. Rangachari D, Yamaguchi N, VanderLaan PA, et al. Brain metastases in patients with EGFR-mutated or ALK-rearranged non-small-cell lung cancers. Lung Cancer. 2015;88:108–111. doi:10.1016/j.lungcan.2015.01.020
29. Heon S, Yeap BY, Lindeman NI, et al. The impact of initial gefitinib or erlotinib versus chemotherapy on central nervous system progression in advanced non-small cell lung cancer with EGFR mutations. Clin Cancer Res. 2012;18:4406–4414. doi:10.1158/1078-0432.CCR-12-0357
30. Park SJ, Kim HT, Lee DH, et al. Efficacy of epidermal growth factor receptor tyrosine kinase inhibitors for brain metastasis in non-small cell lung cancer patients harboring either exon 19 or 21 mutation. Lung Cancer. 2012;77:556–560. doi:10.1016/j.lungcan.2012.05.092
31. Wu YL, Ahn MJ, Garassino MC, et al. CNS efficacy of osimertinib in patients with T790M-positive advanced non-small-cell lung cancer: data from a randomized phase III trial (AURA3). J Clin Oncol. 2018;36:2702–2709. doi:10.1200/JCO.2018.77.9363
32. Reungwetwattana T, Nakagawa K, Cho BC, et al. CNS response to osimertinib versus standard epidermal growth factor receptor tyrosine kinase inhibitors in patients with untreated EGFR-mutated advanced non-small-cell lung cancer. J Clin Oncol. 2018;36:3290–3297. doi:10.1200/JCO.2018.78.3118
33. Ahn BC, Kim JH, Pyo KH, et al. Analyses of CNS response to osimertinib in patients with T790M-positive advanced NSCLC from ASTRIS Korean subset, open-label real-world study. Cancers. 2021;13. doi:10.3390/cancers13153681
34. Xing P, Mu Y, Hao X, Wang Y, Li J. Data from real world to evaluate the efficacy of osimertinib in non-small cell lung cancer patients with central nervous system metastasis. Clin Transl Oncol. 2019;21:1424–1431. doi:10.1007/s12094-019-02071-5
35. Kim SY, Hong CK, Kim TH, et al. Efficacy of surgical treatment for brain metastasis in patients with non-small cell lung cancer. Yonsei Med J. 2015;56:103–111. doi:10.3349/ymj.2015.56.1.103
36. Zheng MH, Sun HT, Xu JG, et al. Combining whole-brain radiotherapy with gefitinib/erlotinib for brain metastases from non-small-cell lung cancer: a meta-analysis. Biomed Res Int. 2016;2016:5807346. doi:10.1155/2016/5807346
37. Ariyasu R, Nishikawa S, Uchibori K, et al. High ratio of T790M to EGFR activating mutations correlate with the osimertinib response in non-small-cell lung cancer. Lung Cancer. 2018;117:1–6. doi:10.1016/j.lungcan.2017.12.018
38. Hong S, Gao F, Fu S, et al. Concomitant genetic alterations with response to treatment and epidermal growth factor receptor tyrosine kinase inhibitors in patients with EGFR-mutant advanced non-small cell lung cancer. JAMA Oncol. 2018;4:739–742. doi:10.1001/jamaoncol.2018.0049
39. Zhang Z, Zhang Y, Luo F, et al. Dual blockade of EGFR and VEGFR pathways: results from a pilot study evaluating apatinib plus gefitinib as a first-line treatment for advanced EGFR-mutant non-small cell lung cancer. Clin Transl Med. 2020;10:e33. doi:10.1186/1479-5876-10-S2-A33
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.