Back to Journals » Journal of Pain Research » Volume 15
Efficacy of Combination Therapy with Pregabalin in Neuropathic Pain: A Preclinical Study in the Rat L5 Spinal Nerve Ligation Model
Authors Nozawa K, Karasawa Y , Shidahara Y, Ushida T
Received 27 July 2022
Accepted for publication 27 October 2022
Published 31 October 2022 Volume 2022:15 Pages 3469—3478
DOI https://doi.org/10.2147/JPR.S383981
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Robert B. Raffa
Kazutaka Nozawa,1 Yusuke Karasawa,1 Yuka Shidahara,2 Takahiro Ushida3
1Medical Affairs, Viatris Pharmaceuticals Japan Inc., Minato-ku, Tokyo, Japan; 2Bioscience Business Division, KAC Co., Ltd, Ritto, Shiga, Japan; 3Multidisciplinary Pain Center, Aichi Medical University, Nagakute, Aichi, Japan
Correspondence: Kazutaka Nozawa, Medical Affairs, Viatris Pharmaceuticals Japan Inc, Minato-ku, Tokyo, Japan, Tel +81 80-5001-3029, Email [email protected]
Purpose: Neuropathic pain is sometimes difficult to manage because of limited efficacy of analgesic monotherapy even at high doses. Combination therapy may help address this issue, but there is little evidence for its effectiveness. Therefore, we evaluated the efficacy of combination therapy with pregabalin, an anchor drug for treating neuropathic pain, using the rat L5 spinal nerve ligation model.
Methods: Experiments were performed on four-week-old L5 spinal nerve ligated male Sprague-Dawley rats. Mechanical allodynia was assessed using the von Frey test, where the 50% withdrawal threshold was evaluated for five drugs: pregabalin, duloxetine, venlafaxine, tramadol, and celecoxib. The single-drug experiment included 112 rats, where each drug was tested independently. Median effective doses (ED50s) were determined. Combinations of pregabalin with each of the other four drugs were tested (n=84). The 50% withdrawal threshold in the von Frey test was evaluated. The ED50 of each combination was determined experimentally. Isobolographic analyses were conducted to assess the synergistic potential of the drug combinations, excluding pregabalin-celecoxib, since the ED50 of celecoxib could not be determined.
Results: In the single-drug experiment, all drugs except celecoxib resulted in a dose-dependent increase in the 50% withdrawal threshold 2 h after administration, with a maximum possible effect ranging from 4.4% to 79.6%. Similarly, all pregabalin combinations demonstrated a dose-dependent increase in the 50% withdrawal threshold, with pregabalin-tramadol showing the greatest increment. Isobolographic analysis of this combination revealed synergistic effects. Specifically, the combination index was γ=0.4 (< 1). Combinations of pregabalin with duloxetine and venlafaxine demonstrated additive (γ=0.9) and antagonistic effects (γ=2.0), respectively.
Conclusion: This study demonstrated that combination of pregabalin with tramadol has synergistic antiallodynic effects, while that with duloxetine has additive effects. Moreover, pregabalin combined with venlafaxine was potentially antagonistic. Pregabalin combined with tramadol may serve as a promising drug combination for the effective management of neuropathic pain.
Keywords: analgesic, animal model, isobologram, synergistic effects
Introduction
Neuropathic pain is defined as pain caused by a lesion or a disease of the somatosensory nervous system,1 which alters sensory signals transmitted to the brain and spinal cord.2 Common characteristics of neuropathic pain include persistent burning and painful sensations, numbness, and increased sensitivity to touch.2 The global prevalence of this condition is estimated to be 7%–10%.2,3 Neuropathic pain is frequently associated with sleep disruption and anxiety, negatively affecting patients’ overall mental well-being and reducing their quality of life.4
Pharmacotherapy is currently the most commonly used treatment to manage neuropathic pain. First-line treatments including gabapentinoids such as gabapentin and pregabalin and serotonin-norepinephrine reuptake inhibitors (SNRIs) such as duloxetine and venlafaxine and second-line treatment including the weak opioid tramadol are recommended by the International Association for the Study of Pain.5 In the clinical setting, nonsteroidal anti-inflammatory drugs (NSAIDs) such as celecoxib are prescribed for mixed pain consisting of nociceptive and neuropathic components. However, their efficacy in treating neuropathic pain is limited.6
Neuropathic pain is associated with the upregulation of voltage-gated calcium channels (VGCCs), specifically the α2-δ-1 subunit, in the dorsal horn and dorsal root ganglion of the spinal cord,7,8 causing increased neural excitation and consequently, neuropathy.8,9 Pregabalin, an anticonvulsant drug, binds to the α2-δ auxiliary subunits to reduce calcium influx, lowering neurotransmitter release and, consequently, overall neuronal excitability.8 Its neuropathic pain–relieving properties have been demonstrated in several preclinical and clinical studies.8 SNRIs are thought to relieve neuropathic pain by improving the impaired descending noradrenergic inhibitory system.10 They have demonstrated efficacy in treating neuropathic pain mainly in patients with diabetic peripheral neuropathy. Among the SNRIs, duloxetine has evidence with moderate quality, whereas venlafaxine has been less evidenced.11,12 Tramadol, a weak opioid, has a unique pharmacological property of exerting not only an opioidergic effect but also noradrenergic and serotonergic effects.13 It has been reported to be effective in patients with several neuropathic pain conditions, although the quality of evidence has been low or very low.14 While several treatment options are available, the overall response rates to analgesic monotherapy in patients with neuropathic pain remain modest.5 Moreover, high-dose analgesic monotherapies may cause adverse effects.15,16 Because neuropathic pain is debilitating, effective pain-management strategies are essential.
Combination therapies using compounds with different modes of action can potentially address the limitations of analgesic monotherapy by providing synergistic effects at lower drug doses. These effects provide an added advantage of potentially fewer treatment-related side effects.17,18 However, there is little concrete evidence to support the efficacy of combination treatments for neuropathic pain. Specifically, clinical trials employing combination therapy with pregabalin have demonstrated varying efficacy.18 In the COMBO-DN clinical trial, pregabalin combined with duloxetine was reported to be noninferior to high-dose monotherapy with either drug.19 On the other hand, preclinical studies have shown that combinations of pregabalin with tapentadol or neurotropin have synergistic effects.20,21 Nevertheless, the use of tapentadol is precluded by limited evidence for treating neuropathic pain,22 and neurotropin has only been approved in Japan.23 Given the paucity of evidence supporting combination therapy, it is imperative to test combinations with widely available and commonly prescribed drugs for the treatment of neuropathic pain.
The aim of this preclinical study was to evaluate the antiallodynic efficacy of pregabalin in combination with other commonly used analgesics in the rat L5 spinal nerve ligation (SNL) model. We assessed the synergistic potential of the combinations to identify candidates for the treatment of neuropathic pain.
Materials and Methods
Animals
A total of 256 four-week-old male Sprague-Dawley rats (Charles River Laboratories, Shiga, Japan), weighing 80–90 g, were used for this study. Animals were housed in a room having temperature between 22.6°C–24.6°C, humidity between 48%–63%, and a light cycle of 12 h per day (0700 to 1900 hours). Rats were housed in polypropylene plastic cages (345 mm × 403 mm × 178 mm; CREA, Tokyo, Japan, Inc.) with not more than two or three rats per cage. The diet included standard rat chow (CRF-1, dry diet; Oriental Yeast Co., Ltd, Tokyo, Japan) and tap water supplemented with hypochlorite (2–10 ppm), available ad libitum. All animals were allowed to acclimatize for five days before commencing experimental procedures.
All rats were euthanized with carbon dioxide after evaluation.
Drugs
Five drugs were tested in this study: duloxetine, celecoxib (Tokyo Chemical Industry Co., Ltd, Tokyo, Japan), pregabalin (ChemFaces, Hubei, China), venlafaxine, and tramadol (Sigma-Aldrich, St. Louis, MO, USA). All drugs were dissolved in distilled water (Otsuka Pharmaceutical Factory Inc, Tokushima, Japan) containing 0.5% w/v methylcellulose 400 solution (Fujifilm Wako Pure Chemical Corporation, Osaka, Japan) and administered orally (5 mL/kg) on Day 7 after SNL.
Spinal Nerve Ligation
The SNL model is commonly used to induce neuropathic pain in animals.24 In this study, SNL was performed under inhalation anesthesia (2–4% isoflurane in air). The left L5 spinal nerve was exposed by removing a small segment of both the paravertebral muscle and the left spinous process of the L5 lumbar vertebra. L5 spinal nerves were then ligated with 6–0 silk sutures. The muscle and adjacent fascia were closed with sutures, and the skin was subsequently closed with metal clips.
von Frey Test
The von Frey test is commonly used to measure mechanical allodynia in rodents.25 In this study, the von Frey test was performed on each animal on Day 7 after SNL. Rats were placed in a plastic box having a mesh-wired bottom and allowed 30 minutes to habituate. Tactile stimuli comprising a series of von Frey filaments (0.4, 0.6, 1, 2, 4, 6, 8, and 15 g; North Coast Medical Inc., Morgan Hill, California, USA) were then applied in succession to the middle plantar surface of the paw, starting with the 2-g filament. The “up-down method” was used, and the withdrawal threshold was computed as 50% withdrawal threshold (g)=(10Xf+kd)/10,000, where Xf is the value of the von Frey stimulus last applied (in log units), k is a tabular value for the response pattern, and d is the distance between consecutive filaments applied (in log units).25 Only animals satisfying the criteria for mechanical allodynia (50% withdrawal threshold <4 g) were selected for subsequent experiments. Animals were allocated to groups such that the 50% withdrawal threshold and average body weight on Day 7 did not differ across groups. The von Frey test was conducted before and 2 h after drug administration.
Single-Drug Experiment
The single-drug experiment included 148 rats that had undergone SNL. Of these, 112 animals demonstrated mechanical allodynia and were allocated for drug administration. These rats were divided into the following five drug subgroups: pregabalin, duloxetine, venlafaxine, tramadol, and celecoxib. Of these, 21 animals each were assigned to the pregabalin, duloxetine, tramadol, and celecoxib subgroups, and 28 animals were assigned to the venlafaxine subgroup. Drug doses were determined based on a preliminary study. The doses for the single drugs were set based on previous studies.21,26–28 Pregabalin was administered at concentrations of 10, 20, and 30 mg/kg; duloxetine at 10, 30, and 60 mg/kg; tramadol at 25, 50, and 100 mg/kg; celecoxib at 10, 30, and 100 mg/kg; and venlafaxine at 10, 100, 600, and 800 mg/kg.
The median effective dose (ED50) for each drug was calculated based on a preliminary study and the single-drug experiment group in the current study and was determined experimentally from the log dose-response curves.
Combination-Drug Experiment
In the combination-drug experiment, various combinations of pregabalin with the four remaining analgesic drugs were tested. In total, 108 rats with SNL were tested, and 84 rats demonstrated mechanical allodynia. Overall, 21 rats were assigned to each combination subgroup (pregabalin-duloxetine, pregabalin-tramadol, pregabalin-celecoxib, and pregabalin-venlafaxine). In each subgroup, seven animals each were assigned to receive one of three doses. For every drug combination, each constituent drug was co-administered at a concentration of either 1/8, 1/4, or 1/2 of their respective ED50 values. The ED50 for celecoxib could not be determined. Therefore, for the combination of pregabalin and celecoxib, the concentrations included (pregabalin + celecoxib) 1/8 ED50 mg/kg + 12.5 mg/kg, 1/4 ED50 mg/kg + 25 mg/kg, and 1/2 ED50 mg/kg + 50 mg/kg. The ED50 of the drugs in the combination was determined as described above.
Data Analysis
ED50 Calculation
Log dose-response curves of the antiallodynic effects determined using the von Frey test were constructed by plotting the 50% withdrawal threshold against the logarithm of dose concentrations tested. Experimental ED50s were then calculated from the sigmoid curve fitted to the data.
Isobolographic Analysis
To assess the synergistic effects of combination therapy, isobolograms were constructed based on the ED50 of the constituent drugs.29 Combination effects were evaluated using the combination index γ.30 For any drug combination, a value of γ=1 indicates an additive effect, whereas γ<1 and γ>1 indicate synergistic and antagonistic effects, respectively.30
Statistical Analysis
Descriptive statistics are reported unless otherwise stated. The 50% withdrawal thresholds and ED50 values are reported as mean (standard error [SE]) values. Student’s t-tests were performed to test for significant differences in the 50% withdrawal threshold before and 2 h after drug administration in the combination-drug experiment. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., North Carolina, USA) for Microsoft Windows. ED50 values were computed using the EXSUS statistical analysis system (version 10.1.1; EP Croit Corporation, Tokyo, Japan).
Results
Of the 256 animals included in this study, 196 were assigned to the single- or combination-drug experiment groups. The body weight of all animals increased between Day 0 (day of SNL) and Day 7 (7 days after SNL), indicating that they were in good health. No clinical abnormalities were observed in the animals throughout the study period.
Single-Drug Experiment
Mechanical allodynia was assessed in SNL rats assigned to the single-drug treatment group using the von Frey test. Of the five drugs tested, pregabalin, duloxetine, venlafaxine (except at the 10 mg/kg dose), and tramadol caused an increase in the 50% withdrawal threshold of rats 2 h after drug administration compared with that before drug administration. For these four drugs, a dose-dependent increase in the withdrawal threshold was observed (Table 1). Specifically, the maximum possible effect ranged from 27.6–79.6% for pregabalin, 12.0–58.8% for duloxetine, 19.5–49.5% for tramadol, and 4.4–64.1% for venlafaxine (Table 1). At most doses, celecoxib did not demonstrate an antiallodynic effect (Table 1).
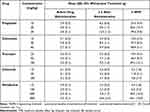 |
Table 1 Withdrawal Threshold in the von Frey Test in the Single-Drug Experiment |
The ED50 of each drug was determined. The mean (SE) ED50s for pregabalin, tramadol, duloxetine, and venlafaxine were 17.1 (3.0) mg/kg, 75.0 (17.2) mg/kg, 26.4 (4.6) mg/kg, and 673.4 (58.5) mg/kg, respectively (Table 2). The ED50 of celecoxib could not be estimated as it did not demonstrate an antiallodynic effect in the von Frey test (Table 1).
 |
Table 2 ED50 for Both Single- and Combination-Drug Experiments |
Combination-Drug Experiment: Isobolographic Analyses
Isobolographic analyses of all drug combinations revealed that the pregabalin-tramadol combination demonstrated synergistic effects (mean [SE] ED50: pregabalin, 3.5 [1.0] mg/kg; tramadol, 15.5 [4.3] mg/kg; Figure 1B), and the corresponding combination index, γ, was 0.4.
None of the pregabalin combinations with SNRIs were synergistic. Specifically, the pregabalin-duloxetine combination demonstrated only an additive effect (γ=0.9; Figure 1A). The mean (SE) experimental ED50 was 7.5 (1.9) mg/kg for pregabalin and 11.6 (2.9) mg/kg for duloxetine. On the contrary, the pregabalin-venlafaxine combination showed a potential antagonistic effect (mean [SE] ED50: pregabalin, 17.2 [14.2] mg/kg; venlafaxine, 663.8 [537.0] mg/kg; γ=2.0; Figure 1C).
As with the single-drug experiment, the von Frey test was used to evaluate mechanical allodynia in SNL rats assigned to the combination-drug treatment groups. All drug combinations demonstrated a dose-dependent increase in the 50% withdrawal threshold 2 h after drug administration (Figure 2). Specifically, the largest difference in mean withdrawal threshold was observed in the pregabalin-tramadol subgroups, while the least difference was observed in the pregabalin-celecoxib subgroups (Figure 2). The ED50s for all pregabalin combinations are presented in Table 2.
Discussion
Neuropathic pain is a debilitating symptom of a range of different etiologies that does not always respond to single pharmacological treatment regimens. Evidence for the efficacy of combination therapy is limited.5 In this study, we demonstrated the antiallodynic efficacy of pregabalin in combination with four other drugs, namely duloxetine, tramadol, celecoxib, and venlafaxine, in the rat L5 SNL neuropathic pain model. The antiallodynic effect was most prominent when pregabalin was combined with tramadol, and the isobolographic analysis of this combination revealed synergistic effects. Additionally, pregabalin combinations with duloxetine and venlafaxine showed additive and antagonistic effects, respectively.
Consistent with the findings reported in the literature regarding the use of pregabalin (anticonvulsant), duloxetine and venlafaxine (SNRIs), and tramadol (weak opioid) for neuropathic pain,2 the results from our single-drug experiment indicated antiallodynic effects of each of these drugs. Celecoxib, however, did not have any impact on the SNL rats. Celecoxib is an NSAID (cyclooxygenase-2 inhibitor) typically prescribed to treat nociceptive pain and is frequently combined with pregabalin in clinical practice for pain relief when neuropathic pain is present as a symptom.31
The von Frey test showed reduced mechanical allodynia in most combination subgroups. Across all the different combinations with pregabalin, the subgroup receiving the combination of pregabalin and tramadol experienced the greatest increase in withdrawal threshold after drug administration. This finding was supported further by isobolographic analyses, which demonstrated the synergistic effects of the combination. The synergism could be attributed to the distinct mechanisms of action of tramadol and pregabalin. Tramadol binds to the µ-opioid receptors in the brain and inhibits serotonin and norepinephrine reuptake.2 On the other hand, pregabalin has several possible mechanisms of action. It primarily targets the α2-δ-1 subunit of VGCCs to reduce overall neural excitability.8 Other mechanisms include the inhibition of N-methyl D-aspartate (NMDA) receptors and sodium currents and reduced VGCC trafficking via the β4a subunit.32
Analgesic effects of the combinations of pregabalin or tramadol with other drugs have been previously reported. Studies have indicated the synergistic benefits of tramadol when combined with acetaminophen for treating nociceptive pain.33 This combination is currently approved by the Food and Drug Administration34 to treat nociceptive pain, such as chronic lower back pain35 and dental pain.36 In contrast, pregabalin has a synergistic antiallodynic effect for neuropathic pain when combined with tapentadol.20 Tapentadol is a drug that combines μ-opioid agonism, indirectly modulating the descending pain pathways involving the brain and spinal cord, with the action of noradrenaline reuptake inhibition by delaying the release of noradrenaline into the synaptic cleft, thereby having high analgesic efficacy.20 Since tapentadol is a derivative of tramadol, the results of this study are consistent with the synergistic effects observed with the pregabalin-tapentadol combination.20 Moreover, synergistic effects with opioids have also been observed with other anticonvulsants such as gabapentin, the same gamma-aminobutyric acid (GABA) derivative as pregabalin.32 Gabapentin, when combined with opioids such as morphine, not only reduced pain scores in patients with neuropathic pain but also enhanced the analgesic effects of morphine by increasing pain tolerance.37 Furthermore, gabapentin-opioid combinations have demonstrated greater efficacy than opioid monotherapy in treating cancer-related neuropathic pain. The current study provides evidence supporting combination therapy with pregabalin and tramadol to treat neuropathic pain, consistent with previous reports of synergistic effects with pregabalin-tapentadol20 and gabapentin-opioid combinations.37 However, the concomitant use of opioids and gabapentinoids must be considered with caution due to the reported risk of respiratory depression.38
Several clinical studies have previously investigated the combinations of pregabalin with other classes of analgesics as well. Romanò et al demonstrated that pregabalin combined with celecoxib has greater efficacy in treating chronic lower back pain having both nociceptive and neuropathic components than individual monotherapies;39 The results of the von Frey test demonstrate that pregabalin combined with celecoxib showed limited efficacy in alleviating mechanical allodynia, suggesting that this combination may not be an appropriate choice for neuropathic pain. Nevertheless, for mixed pain, such as those having both neuropathic and nociceptive characteristics, a combination of drugs independently targeting each pain may be clinically meaningful. The additive effect observed with the pregabalin-duloxetine combination in this study supports the findings of the COMBO-DN clinical study, which demonstrated the nonsuperiority of this combination over high-dose monotherapy for treating peripheral neuropathic pain in diabetes, with no significant differences in treatment-emergent adverse events (TEAEs) in both groups.19 This result also suggests that the pregabalin-duloxetine combination may not demonstrate synergistic effects, consistent with the additive effects observed in the present study, and that low-dose combination therapy may not aid in reducing TEAEs.
Interestingly, our results indicated potential antagonistic effects when pregabalin was combined with venlafaxine. Venlafaxine functions as a selective serotonin reuptake inhibitor at low doses and as an SNRI at high doses.40 Compared with high-dose venlafaxine, the efficacy of low-dose venlafaxine is limited, and it is therefore not recommended.11 Consistent with this finding, our results demonstrate that venlafaxine in combination therapy, when lower doses are used, may not be effective in managing neuropathic pain. Although duloxetine and venlafaxine belong to the same class of drugs (SNRIs) and have been strongly recommended,5 we observe different combination effects with each. However, it is not clear if the antagonism with venlafaxine is true antagonism or a spurious finding. The ED50 of venlafaxine in the combination is much greater and lies beyond the dose range of the single agents tested, and this could be a potential reason for its observed variability. Therefore, this combination must be investigated further.
Across all tested combinations, pregabalin combined with tramadol demonstrated more than a two-fold increase in withdrawal threshold in the von Frey test. However, it must be noted that mechanical allodynia, the condition investigated in this study, is not always observed in every case of neuropathic pain in clinical practice. Therefore, these results must be interpreted with caution since combination therapy may not necessarily lead to analgesia in all forms of neuropathic pain. The increased withdrawal threshold was observed when the dose concentrations of both pregabalin and tramadol in the combination were lower than their respective concentrations when used individually. Pregabalin is commonly associated with unfavorable side effects such as somnolence, dizziness, and weight gain,41,42 causing patients to discontinue treatment,42 whereas tramadol is associated with nausea, dizziness, and sometimes constipation.14 Therefore, the observed synergistic effect of the pregabalin-tramadol combination permits a reduction in both pregabalin and tramadol dosage, which may be beneficial for mitigating TEAEs. However, the safety of individual drugs and drug combinations was not assessed as this was a preclinical study, and it could not be determined whether lowering the drug dosage would reduce TEAEs. These aspects must be evaluated in future clinical studies.
Conclusions
This study demonstrated that pregabalin combined with tramadol has synergistic effects and may be a promising treatment for neuropathic pain. This combination strategy enables the use of lower doses of each constituent drug to provide a therapeutic benefit similar to that achieved using high-dose monotherapy but with possibly fewer adverse effects. Our findings lay the foundation for assessing combination therapy in real-world clinical practice to determine the optimal dose and confirm the efficacy and safety of this drug combination for the effective management of neuropathic pain.
Abbreviations
ED50, Median effective dose; GABA, Gamma-aminobutyric acid; NMDA, N-methyl D-aspartate; NSAID, Nonsteroidal anti-inflammatory drug; SE, Standard error; SNL, Spinal nerve ligation; SNRI, Serotonin-norepinephrine reuptake inhibitor; TEAE, Treatment-emergent adverse event; VGCC, Voltage-gated calcium channel.
Data Sharing Statement
Data supporting the findings of this study are available from the corresponding author on request.
Acknowledgments
Editorial support in the form of medical writing, assembling tables, creating high-resolution images based on authors’ detailed directions, collating author comments, copyediting, fact checking, and referencing was provided by Varsha Sreenivasan, PhD, of Cactus Life Sciences (part of Cactus Communications) and funded by Viatris Pharmaceuticals Japan Inc.
Ethics Approval
All experimental procedures were conducted by KAC Co. Ltd. The research facility has been accredited by the Japanese Society for Laboratory Animal Resources. All procedures were conducted in compliance with the Animal Experiment Regulations of KAC Co. Ltd., the Animal Experiment Committee Regulations, and the Animal Experiment Approval Provisions (approval nos. 19-0705 and 20-0710 [additional preliminary tests]).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave approval to the final version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was sponsored by Viatris Pharmaceuticals Japan Inc.
Disclosure
KN and YK are employees of Viatris Pharmaceuticals Japan Inc. YS is an employee of KAC Co., Lt., Japan. TU declares no competing interests in this work.
References
1. International Association for the Study of Pain (IASP). Terminology; 2017. Available from: https://www.iasp-pain.org/resources/terminology/.
2. Colloca L, Ludman T, Bouhassira D, et al. Neuropathic pain. Nat Rev Dis Primers. 2017;3(1):17002. doi:10.1038/nrdp.2017.2
3. van Hecke O, Austin SK, Khan RA, Smith BH, Torrance N. Neuropathic pain in the general population: a systematic review of epidemiological studies. Pain. 2014;155(4):654–662. doi:10.1016/j.pain.2013.11.013
4. Inoue S, Taguchi T, Yamashita T, Nakamura M, Ushida T. The prevalence and impact of chronic neuropathic pain on daily and social life: a nationwide study in a Japanese population. Eur J Pain. 2017;21(4):727–737. doi:10.1002/ejp.977
5. Finnerup NB, Attal N, Haroutounian S, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162–173. doi:10.1016/S1474-4422(14)70251-0
6. Sumitani M, Sakai T, Matsuda Y, et al. Executive summary of the clinical guidelines of pharmacotherapy for neuropathic pain: second edition by the Japanese society of pain clinicians. J Anesth. 2018;32(3):463–478. doi:10.1007/s00540-018-2501-0
7. Bauer CS, Nieto-Rostro M, Rahman W, et al. The increased trafficking of the calcium channel subunit α2δ-1 to presynaptic terminals in neuropathic pain is inhibited by the α2δ ligand pregabalin. J Neurosci. 2009;29(13):4076–4088. doi:10.1523/JNEUROSCI.0356-09.2009
8. Verma V, Singh N, Singh Jaggi A. Pregabalin in neuropathic pain: evidences and possible mechanisms. Curr Neuropharmacol. 2014;12(1):44–56. doi:10.2174/1570159X1201140117162802
9. Li CY, Song YH, Higuera ES, Luo ZD. Spinal dorsal horn calcium channel alpha2delta-1 subunit upregulation contributes to peripheral nerve injury-induced tactile allodynia. J Neurosci. 2004;24(39):8494–8499. doi:10.1523/JNEUROSCI.2982-04.2004
10. Obata H. Analgesic mechanisms of antidepressants for neuropathic pain. Int J Mol Sci. 2017;18(11):2483. doi:10.3390/ijms18112483
11. Gallagher HC, Gallagher RM, Butler M, Buggy DJ, Henman MC. Venlafaxine for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;2015(8):CD011091.
12. Lunn MP, Hughes RA, Wiffen PJ, Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. Cochrane Database Syst Rev. 2014;1:CD007115. doi:10.1002/14651858.CD007115.pub3
13. Barakat A. Revisiting tramadol: a multi-modal agent for pain management. CNS Drugs. 2019;33(5):481–501. doi:10.1007/s40263-019-00623-5
14. Duehmke RM, Derry S, Wiffen PJ, Bell RF, Aldington D, Moore RA. Tramadol for neuropathic pain in adults. Cochrane Database Syst Rev. 2017;6(6):CD003726. doi:10.1002/14651858.CD003726.pub4
15. Freeman R, Durso-Decruz E, Emir B. Efficacy, safety, and tolerability of pregabalin treatment for painful diabetic peripheral neuropathy: findings from seven randomized, controlled trials across a range of doses. Diabetes Care. 2008;31(7):1448–1454. doi:10.2337/dc07-2105
16. Holbech JV, Jung A, Jonsson T, Wanning M, Bredahl C, Bach FW. Combination treatment of neuropathic pain: Danish expert recommendations based on a Delphi process. J Pain Res. 2017;10:1467–1475. doi:10.2147/JPR.S138099
17. Gilron I, Watson CP, Cahill CM, Moulin DE. Neuropathic pain: a practical guide for the clinician. CMAJ. 2006;175(3):265–275. doi:10.1503/cmaj.060146
18. Vorobeychik Y, Gordin V, Mao J, Chen L. Combination therapy for neuropathic pain: a review of current evidence. CNS Drugs. 2011;25(12):1023–1034. doi:10.2165/11596280-000000000-00000
19. Tesfaye S, Wilhelm S, Lledo A, et al. Duloxetine and pregabalin: high-dose monotherapy or their combination? The “COMBO-DN study”--a multinational, randomized, double-blind, parallel-group study in patients with diabetic peripheral neuropathic pain. Pain. 2013;154(12):2616–2625. doi:10.1016/j.pain.2013.05.043
20. Christoph T, De Vry J, Schiene K, Tallarida RJ, Tzschentke TM. Synergistic antihypersensitive effects of pregabalin and tapentadol in a rat model of neuropathic pain. Eur J Pharmacol. 2011;666(1–3):72–79. doi:10.1016/j.ejphar.2011.05.029
21. Okazaki R, Namba H, Yoshida H, Okai H, Taguchi K, Kawamura M. Combined antiallodynic effect of Neurotropin(R) and pregabalin in rats with L5-spinal nerve ligation. Life Sci. 2013;92(4–5):259–265. doi:10.1016/j.lfs.2012.12.009
22. Freo U, Romualdi P, Kress HG. Tapentadol for neuropathic pain: a review of clinical studies. J Pain Res. 2019;12:1537–1551. doi:10.2147/JPR.S190162
23. Nippon Zoki. Neurotropin® tab. 4N.U; 2020. Available from: https://www.nippon-zoki.co.jp/mtassets/files/4370c62cc9c95817d1824958f350923ee030fc0a.pdf.
24. Ho Kim S, Mo Chung J. An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat. Pain. 1992;50(3):355–363. doi:10.1016/0304-3959(92)90041-9
25. Deuis JR, Dvorakova LS, Vetter I. Methods used to evaluate pain behaviors in rodents. Front Mol Neurosci. 2017;10:284. doi:10.3389/fnmol.2017.00284
26. Hahm TS, Ahn HJ, Ryu S, et al. Combined carbamazepine and pregabalin therapy in a rat model of neuropathic pain. Br J Anaesth. 2012;109(6):968–974. doi:10.1093/bja/aes306
27. Nakagawa T. Pharmacological properties of tramadol and tapentadol. Jpn J Pharm Palliat Care Sci. 2013;6:11–22. Japanese.
28. Iyengar S, Webster AA, Hemrick-Luecke SK, Xu JY, Simmons RM. Efficacy of duloxetine, a potent and balanced serotonin-norepinephrine reuptake inhibitor in persistent pain models in rats. J Pharmacol Exp Ther. 2004;311(2):576–584. doi:10.1124/jpet.104.070656
29. Tallarida RJ, Raffa RB. Testing for synergism over a range of fixed ratio drug combinations: replacing the isobologram. Life Sci. 1996;58(2):PL23–PL28.
30. Chou TC. Theoretical basis, experimental design, and computerized simulation of synergism and antagonism in drug combination studies. Pharmacol Rev. 2006;58(3):621–681. doi:10.1124/pr.58.3.10
31. Ushida T, Matsui D, Inoue T, et al. Recent prescription status of oral analgesics in Japan in real-world clinical settings: retrospective study using a large-scale prescription database. Expert Opin Pharmacother. 2019;20(16):2041–2052. doi:10.1080/14656566.2019.1651840
32. Patel R, Dickenson AH. Mechanisms of the gabapentinoids and α 2 δ-1 calcium channel subunit in neuropathic pain. Pharmacol Res Perspect. 2016;4(2):e00205. doi:10.1002/prp2.205
33. Yoshizawa K, Arai N, Suzuki Y, et al. Synergistic antinociceptive activity of tramadol/Acetaminophen combination mediated by μ-opioid receptors. Biol Pharm Bull. 2020;43(7):1128–1134. doi:10.1248/bpb.b20-00230
34. U.S. Food and Drug Administration. Ultracet (325 mg Acetaminophen/37.5 mg tramadol hydrochloride) tablets; 2001. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2001/21123_Ultracet.cfm.
35. Peloso PM, Fortin L, Beaulieu A, Kamin M, Rosenthal N. For Protocol TRP-CAN-1 Study Group. Analgesic efficacy and safety of tramadol Acetaminophen combination tablets (Ultracet) in treatment of chronic low back pain: a multicenter, outpatient, randomized, double blind, placebo controlled trial. J Rheumatol. 2004;31(12):2454–2463.
36. Medve RA, Wang J, Karim R. Tramadol and Acetaminophen tablets for dental pain. Anesth Prog. 2001;48(3):79–81.
37. Eckhardt K, Ammon S, Hofmann U, Riebe A, Gugeler N, Mikus G. Gabapentin enhances the analgesic effect of morphine in healthy volunteers. Anesth Analg. 2000;91(1):185–191. doi:10.1213/00000539-200007000-00035
38. Food and Drug Administration. FDA warns about serious breathing problems with seizure and nerve pain medicines gabapentin (Neurontin, Gralise, Horizant) and pregabalin (Lyrica, Lyrica CR); 2019. Available from: https://www.fda.gov/drugs/drug-safety-and-availability/fda-warns-about-serious-breathing-problems-seizure-and-nerve-pain-medicines-gabapentin-neurontin.
39. Romano CL, Romano D, Bonora C, Mineo G. Pregabalin, celecoxib, and their combination for treatment of chronic low-back pain. J Orthop Traumatol. 2009;10(4):185–191. doi:10.1007/s10195-009-0077-z
40. Debonnel G, Saint-Andre E, Hebert C, de Montigny C, Lavoie N, Blier P. Differential physiological effects of a low dose and high doses of venlafaxine in major depression. Int J Neuropsychopharmacol. 2007;10(1):51–61. doi:10.1017/S1461145705006413
41. Kato H, Miyazaki M, Takeuchi M, et al. A retrospective study to identify risk factors for somnolence and dizziness in patients treated with pregabalin. J Pharm Health Care Sci. 2015;1(1):22. doi:10.1186/s40780-015-0022-7
42. Toth C. Pregabalin: latest safety evidence and clinical implications for the management of neuropathic pain. Ther Adv Drug Saf. 2014;5(1):38–56. doi:10.1177/2042098613505614
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


