Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 11
Efficacy of bariatric surgery in improving metabolic outcomes in patients with diabetes. A 24-month follow-up study from a single center in the UAE
Authors Alnageeb H, Abdelgadir E, Khalifa A, Suliman M, Gautam S, Layani L, Subramaniam S, Bashier A
Received 9 June 2018
Accepted for publication 25 June 2018
Published 3 September 2018 Volume 2018:11 Pages 459—467
DOI https://doi.org/10.2147/DMSO.S176761
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ming-Hui Zou
Hanadi Alnageeb,1 Elamin Abdelgadir,2 Azza Khalifa,2 Mohamed Suliman,3 Subash Chander Gautam,4 Laurent Layani,4 Sriganesh Subramaniam,4 Alaaeldin Bashier2
1Medical Department, Fujairah Hospital, Fujairah, UAE; 2Endocrine Department, Dubai Hospital, Dubai Health Authority, Dubai, UAE; 3Endocrinology, Imperial College London Diabetes Centre, Al Ain, UAE; 4Surgical Department, Fujairah Hospital, Fujairah, UAE
Background: Owing to its impact on weight loss, remission of diabetes mellitus and metabolic syndrome, bariatric surgery has offered hope for grossly obese individuals. In recent years, obesity has increased in the UAE and the use of bariatric surgery has increased in-line with this trend. However, data regarding bariatric surgery outcomes in diabetic Emirati people is scarce.
Objective: To evaluate the effect of bariatric surgery in patients with diabetes mellitus.
Methods: This is a retrospective analysis of diabetic patients treated with bariatric surgery with a minimal follow-up of 1 year and extended for some patients (21) to 2 years follow up. A total of 80 patients underwent bariatric surgery. Two surgical procedures were used; laparoscopic sleeve gastrectomy (n=53) or mini-gastric bypass between January 1, 2015, and July 20, 2017.
Results: Mean baseline weight was 119.2±31.2 kg, this has significantly dropped to 100.1±23.1, 91.2±22.3, 82.3±17.5, and 81.3±15.3 kg at 3, 6, 12, and 24 months respectively, and this change was statistically significant P<0.001 at each time point. Mean baseline HbA1c was 8.6% ± 2.3% and this dropped significantly to 6.5±1.7, 5.9±1.2, 5.6±0.8, and 5.4±0.7 at 3, 6, 12, and 24 months respectively (P<0.000). In 49 (61.3%) we considered fatty liver based on ultrasound features either with or without elevation in alanine aminotransferase (ALT). We noticed a significant decrease in ALT at 3, 6, and 12 months after surgery. Furthermore, 11 patients (22.4%) showed sonographic features of improvement in fatty liver in addition to normalization of ALT.
Conclusions: Bariatric surgery was effective over a follow-up period of 2 years in achieving significant weight loss as well as resulting in improvements in glycemic control, blood pressure, and fatty liver.
Keywords: sleeve gastrectomy, type 2 diabetes, type 1 diabetes, excess weight loss, HbA1c, weight, bariatric surgery, Middle East, UAE
Introduction
Obesity is gradually becoming a global health concern. According to the World Health Organization (WHO), worldwide prevalence of obesity has tripled since 1975.1 As of 2016, around 39% of adults aged 18 years or older were overweight, and 13% were obese.1 The estimated prevalence in the Middle East does not differ remarkably from international records, as the WHO has reported over 74% and 69% overweight women and men, respectively. The United Arab Emirates (UAE), in particular, is one of six Middle Eastern countries with the highest rates of overweight and obesity.2
Sheikh-Ismail et al3 demonstrated that the prevalence of obesity along with overweight in the seven emirates of UAE was 27% and 16%, respectively. Adult females were prone to be more obese in the UAE than their male counterparts. Similarly, Mahboub et al4 reported the rate of obesity prevalence to be 20.9%. This would make the UAE one of the highest countries in the Middle East in terms of obesity.5
The alarming rise in the prevalence of obesity in UAE has been noted in both adults and children. In a population-based study evaluating the prevalence of overweight and obesity in children, using the CDC method, revealed that 37.2% of the Emiratis between 15 and 18 years were overweight, 22.2% were obese and 8.8% were extremely obese. The highest percentages of overweight adolescents were living in Dubai (52.6%).6
Despite the globally rising prevalence of obesity, few pharmacologic treatment options are currently available for clinical prescription, and even fewer are available in the UAE. This, in addition to patients and physician’s inertia toward medical treatment of obesity, have probably contributed in increasing the demand for weight reduction surgeries in the UAE, and the gulf region in general. Bariatric surgeries are currently being done in many centers across the UAE; however, few outcome reports have been published.7
In this study, we aimed at assessing bariatric surgery outcomes in patients with diabetes mellitus in the UAE. We looked at weight loss and changes in metabolic parameters over a 2-year period. To our knowledge, this is the second study from the UAE to evaluate bariatric surgery outcomes, and the first to assess outcomes specifically in patients with diabetes.
Methodology
Patients and procedures
Subjects
This is a retrospective analysis of outcome data of patients with diabetes (type 1 or type 2) treated by bariatric surgery between January 1, 2015, and July 1, 2017, from a single center in the city of Fujairah, UAE. All included patients were at least 18 years old, non-pregnant and had complete data on demographics, and pre- and post-surgery biometric and biochemical parameters. To be included in the study patients should have completed follow up for at least 6 months after surgery. We excluded patients without diabetes, those who had post-operative follow-up for <6 months, and patients with incomplete data records.
Ethical approvals
The study was part of an MSc thesis that has been approved by the ethical committees of the Ministry of Health (UAE) and by Queen Mary, University of London. Owing to the retrospective nature of the study and in accordance to the ethical committees rules for such study designs, a waiver of informed consent was granted. Patient identity and confidentiality of information have been protected.
Aim of the study
The aim of the study was to assess the efficacy and consistency of metabolic benefits of bariatric surgery in patients with diabetes mellitus.
Outcome measures
Primary outcome
To assess the trend of percentage of excess body weight (EBW) reduction at 3, 6, 12, and 24 months after the bariatric surgery
Secondary outcomes
We aimed to assess the bariatric surgery outcomes in diabetic patients including morbidity, and mortality. We also looked at changes in HbA1c, lipid profile, blood pressure, TSH, and serum transaminases (as indicator for fatty liver status). Furthermore, we aimed at assessing the rates of diabetes, hypertension and dyslipidemia remission following surgery. Moreover, we wished to assess whether there was improvement in osteoarthritis or obstructive sleep apnoea symptoms after surgery using questionnaires.
Data collection
We collected the data from surgical records and selected patients based on pre-determined inclusion and exclusion criteria. We then reviewed medical files as well as an electronic database for completion of data records. Data collected included demographic data of age, sex, and nationality as well as information about patients’ co-morbidities. We also collected anthropometric data that included weight, height, and blood pressure at 3, 6, 12, and 24 months. Laboratory data included HbA1c, lipid profile, creatinine, liver function tests, and thyroid function tests. We also collected data on ultrasound imaging of the liver for evaluation of fatty liver disease. To assess regression of diabetes and hypertension we assessed the use of medications at baseline and then at 3, 6, 12, and 24 months.
As part of hospital protocol direct questions were addressed to all patients in each visit to monitor the status of their osteoarthritis and obstructive sleep apnea if they had these conditions at baseline. This included severity of joints pain, requirement for painkillers, quality of nocturnal sleep, reduction in daytime sleepiness, and discontinuation of long-term oxygen therapy. These questions have been analyzed to get an insight on the degree of improvement in symptoms.
Statistical analysis
All data was then entered in an excel sheet and was prepared for analysis. Paired Student’s t-tests were used to test the significance of differences between values for continuous variables measured at baseline and those at various time points. Independent t-tests, one-way analysis of variance (ANOVA) and Chi squared tests were used to assess the significance of differences between the groups. Continuous data are presented as the mean ± SD, and categorical data are presented as frequencies and percentages. Differences with P-values ≤0.05 were considered to be statistically significant. Analyses were performed using Statistical Package for the Social Sciences (SPSS) version 23 (IBM Corp, New York, NY, USA).
Definitions
Percentage of excess weight loss (%EWL) was calculated by dividing the weight loss in kilograms after surgery by the pre-surgery excess body weight (calculated as the excess weight in kilograms to yield a BMI of 25 kg/m2) and multiplied by 100.
Type 2 diabetes was defined using the American Diabetes Association definition of type 2 diabetes (HbA1c>6.5%) or fasting blood glucose 7 mmol/L (126 mg/dL). Type 1 diabetes was diagnosed based on the same criteria, in addition, the patient should either have positive antibodies or documented on hospital records as type 1 diabetes. Complete remission of type 2 diabetes was defined using SOARD-ASMBS (Surgery for Obesity and Related Diseases-American Society for Metabolic Surgery and Obesity) standardized reporting outcomes 2015 as: “HbA1c<6% range and fasting blood glucose <100 mg/dL in the absence of active pharmacological agent.” Partial response was defined based on the same criteria as: Sub-diabetic hyperglycaemia (HbA1c 6%–6.4%, FBG 100–125 mg/dL) in the absence of antidiabetic medications.8 Fat free mass (kg) was calculated by subtracting fat mass (kg) from total weight (kg)
Patients’ pathway
Preoperative care
All patients received detailed information and extensive counseling regarding the surgical procedures and expected complications. Screening for potential candidates was based on the American Society for Metabolic and Bariatric Surgery (ASMBS) guidelines, which recommend surgery if the BMI is >40 kgm2 in patients with no comorbidities, and in patients with a BMI of >35 kgm2 if they had obesity associated comorbidities, including diabetes, hypertension, hyperlipidaemia, obstructive sleep apnoea, and non-alcoholic fatty liver disease.9
Surgical procedures
A range of bariatric surgical procedures were provided, however, laparoscopic mini gastric bypass (MGB) and laparoscopic sleeve gastrectomy were the most commonly chosen procedures. All procedures were done by a single bariatric surgeon.
Postoperative care
The bariatric nurse contacted patients usually on day 5 after surgery and appointed them to visit the clinic on the 10th post-operative day for a suture removal. Patients were given free access to nutrition services in the center to receive personalized dietary advice, however, the general rule was gradual re-introduction of solid foods, avoidance of high glycemic index foods, and more consumption of high fiber diets. Patients were also given follow-up appointments with the clinician, and psychologist at 1, 3, 6, 12, 18, and 24 months.
Results
Baseline characteristics
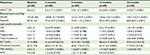
A total of 80 patients fulfilled the inclusion criteria and were included in the study, 51% (n=41) were females and the mean age was 37.4±10.2 years. The Emirati nationals contributed 92.5% (74) of the cohort, while 2.5% (n=2) were other Arab nationalities and 5% (n=4) were non-Arabs. All patients were known to have diabetes with type 2 diabetes constituting 86% (n=69) of patients while 14% (n=11) had type 1 diabetes. A total of 56.3% (n=45) had hypertension, 22.5% (n=18) were diagnosed with dyslipidemia and 65% (n=52) were diagnosed with non-alcoholic fatty liver (Table 1). Most patients underwent sleeve gastrectomy 66.2% (n=53), while 25% (n=20) underwent bypass surgery, the rest underwent other forms of surgery (laparoscopic gastric banding) 8.8% (n=7).
  | Table 1 Characteristics of patients at baseline |
As per our inclusion criteria, all the 80 patients have been followed up for at least 6 months, 69 patients (86%) were followed up for at least 1 year while 20 patients (25%) were followed up for at least 2 years. Figure 1 shows the flow chart for the patients at the various time points of the follow-up.
Weight changes
The obesity measures assessed were weight, BMI and percentage loss of excess weight. The mean baseline weight was 119.2±31.2 kg, this had significantly dropped to 100.1±23.1, 91.2±22.3, 82.3±17.5, and 81.3±15.3 kgs at 3, 6, 12 and 24 months respectively, this change was statistically significant P<0.001 at each time point. Patients had lost an average of their excess body weight (EBW) of 34.5%, 55.4%, 71% and 71.7% at 3, 6, 12 and 24 months respectively, P<0.001, Table 2. The BMI had dropped significantly from 46.5±13.1 kg/m2 at the baseline to 38.3±8.6, 34.5±8.0, 31.3±7.1, 30.9±5.5 kg/m2 at 3, 6, 12 and 24 months respectively, P<0.001 (Table 2).
  | Table 2 Changes in obesity measures Note: *Highly significant P-value <0.001. |
Males’ weights were statistically significantly higher than females’ weights at the baseline and each of the follow-up time points, with P-values of 0.017, 0.003, 0.006, 0.016, and 0.04 at 3, 6, 12, and 24 months respectively. There were no statistically significant differences by gender in terms of EBW% loss and BMI (Table 3). Furthermore, we did not find any significant differences between age groups nor between type 1 and type 2 diabetes patients in obesity measures at the baseline and follow-up periods.
  | Table 3 Changes in obesity measures after surgery by gender Note: *Significantly different (P≤0.05). Abbreviation: BMI, body mass index. |
Metabolic parameters
Baseline HbA1c was 8.6% ± 2.3% and this dropped significantly to 6.5±1.7, 5.9±1.2, 5.6±0.8, and 5.4±0.7 at 3, 6, 12 and 24 months respectively (P<0.000), Table 4. Similar improvements were seen with blood pressure, the systolic blood pressure at baseline was 135.8±18.0 mmHg and dropped significantly to 124.8±15.1, 121.6±19.3, 120.6±12.6, and 120.1+10.2 at 3, 6, 12, and 24 months respectively (Table 4).
Total cholesterol and low-density lipoprotein (LDL) were significantly reduced by bariatric surgery, The LDL was reduced from 2.8±1.5 at baseline to 2.3±1.0 and 1.6±1.0 mmol/L at 12 and 24 months, respectively (P<0.05). Similar changes were seen with total cholesterol as it dropped from a baseline of 4.6±1.3 mmol/L to reach 4.05±0.8 mmol/L at follow-up visits (Table 4). There were no significant changes in serum creatinine throughout the follow-up period.
Medications
At baseline 51.3% (n=41) were using one drug to treat their diabetes, 26.3% (n=21) were using two drugs, 17.5 (n=14) were on three drugs, and 5% (n=4) were on four drugs. At 24 months 80% (n=16) stopped all medications while 15% (n=3) were using a single medicine to control their diabetes and only 5% (n=1) were using two medications (P<0.05). A larger percentage (72.5%) of patients have stopped using any kind of anti-diabetes medication after 3 months of the surgery and the percentage increased to 80% (16 out of 20 patients who completed 2 years of follow up), Figure 2. According to these results, diabetes had regressed in 72.5% at 3 months and in 80% of patients followed at 2 years. Patients using insulin at 12 and 24 were mostly type 1 diabetes, while only two patients with type 2 diabetes were using insulin at 12 months and a single patient at 24 months.
  | Figure 2 The use of medications over the study period. |
The use of statins and calcium channel blockers was decreased from 21.3% and 12.5% before surgery to 10% and 0%, respectively, after surgery, P≤0.05.
Other parameters
Despite being prescribed multivitamins postoperatively, few of our patients developed vitamin D deficiency after bariatric surgery (31.6% [n=6] patients), and 15.8% (n=3) patients developed vitamin B12 deficiency, 10.5% (n=2) patients developed iron deficiency anemia, and one patient developed folate deficiency. These vitamin deficiencies might reflect lack of compliance to prescribed treatment.
Comorbidities
Almost 61.3% (n=49) patients were considered to have fatty liver based on ultrasound features ± elevated alanine aminotransferase (ALT). We noticed a significant decrease in ALT at 3, 6 and 12 months after surgery. Furthermore, 11 (22.4%) showed sonographic features of improvement in fatty liver in addition to normalization of ALT.
Thyroid-stimulating hormone (TSH) levels decreased significantly from baseline at 3, 6 and 12 months after surgery, P≤0.05, but increased again after 24 months of follow-up, P>0.05. This was reflected as well in a reduction in thyroxine dose in the hypothyroid cohort (Table 4).
At baseline, 31.3% (n=25) patients gave a history of osteoarthritis and other joint problems; 14 of them reported significant improvement in their symptoms. Another 15% (n=12) patients were diagnosed preoperatively with obstructive sleep apnea, 11 of them (91.7%) reported improvement in the quality of their sleep, reduced daytime sleepiness, and discontinuation of long-term oxygen therapy.
Males had significantly higher levels of triglycerides, ALT and creatinine than females before surgery, P≤0.05. However, those differences disappeared at the subsequent follow-up periods as shown in Table 4.
Outcomes per type of surgery
Laparoscopic sleeve gastrectomy (LSG) outcome measures
Of all 53 patients who underwent LSG, only 19 (35.8%) had complete profiles at 24 months. Table 5 shows weight changes in those who underwent LSG. Forty-eight patients (97.9%) of type 2 diabetes mellitus patients who underwent sleeve gastrectomy stopped using both insulin and oral hypoglycemic agents. Four patients with type 1 diabetes mellitus continued on insulin at lower doses. Figure 3 shows changes in body composition after LSG. All patients (n=31) with hypertension stopped their antihypertensive treatment, except for one patient who continued using two antihypertensive drugs.
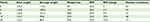  | Table 5 Weight outcomes for LSG presented as mean data Abbreviation: LSG, laparoscopic sleeve gastrectomy. |
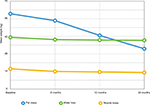  | Figure 3 Changes in body composition post LSG. Abbreviation: LSG, laparoscopic sleeve gastrectomy. |
No major complications (leakages, bleeding) were observed after surgery. The average length of stay in the hospital was 2–3 days. No deaths occurred postoperatively or even in the period of follow up.
Outcomes following mini-gastric bypass (MGB)
At 24 months after surgery, fat, muscle, and water mass decreased by 49.36% and 9.8%, respectively. Twenty patients out of 27 who underwent MGB were diagnosed with type 2 diabetes and were on antidiabetic medications. Sixteen out of the 20 patients stopped their antihyperglycemic medications at 12 months. Seven out of the 27 patients had type 1 diabetes and continued on their insulin at a lower dose.
Discussion
In the UAE, the prevalence of obesity in patients with diabetes is >30% and overweight is 43%.2 While type 2 diabetes affects nearly a fifth of the population according to the latest estimate of the IDF.10 Bariatric surgery is widely performed in the UAE and the Middle East in general, however, very few studies have assessed the outcomes of those procedures.7,11 Our study looked specifically at the outcomes of surgery in patients with diabetes.
Weight changes
Weight reduction after bariatric surgery is attributed to different mechanisms including the minimization of the absorption surface area, modulation of eating behavior either due to limited gastric space or due to higher brain centers remodeling after surgery leading to healthier meals preferences, and the satiety set point.7,12 Moreover, alterations of the systemic neuro-hormones (eg, ghrelin, glucose-dependent insulin-tropic peptide, GLP-1, and peptide YY) may also contribute to the weight loss.13,14 Glycemic improvement in patients with diabetes is widely considered to be attributable to weight reduction but the neurohormonal changes are also an important factor.15–17
At the time of writing of this paper, there have been only a handful of studies in the UAE that looked into the bariatric surgery outcomes. In a study by Abusnana et al,7 an assessment was made of the outcomes in 95 bariatric surgeries in Emirati patients, only a third of these patients had diabetes while our cohort was solely patients with diabetes. Another difference between the two studies is that sleeve gastrectomy was performed in 66.2% (n=53) of our cohort compared to 90% (n=86) in Abusnana’s cohort. Moreover, our study analyzed the observed the outcome until 24 months after surgery, while in the other study it was only 12 months.7
Despite these differences, we observed comparable weight reduction between our cohort and that of Abusnana et al7 at 12 months (119.2±31.2– 82.3±17.5, and 123.67±18.03– 74.3±15.18, respectively). Similarly, the EBWL was 71.0±31.5 and 67.88, respectively.7 There was no statistically significant difference between patients with or without diabetes in Abusnana’s study from a weight point of view. The weight and BMI reduction were maintained in our cohort for up to 24 months, this is the trend of many of the previous bariatric surgery outcome studies.18–20
In the systemic review by Gill et al21 in which they analyzed 28 studies, the mean percentage of excess weight loss was 47.3% (range 6.3%–74.6%) after a mean follow-up period of 13 months (range 3–36).
Metabolic parameters
Achieving remission of type 2 diabetes is a difficult target to achieve except by bariatric surgery. In our cohort, all patients with type 2 diabetes who were on hypoglycaemic medications, managed to stop all diabetes treatments after surgery with the exception of two patients who needed to be re-started on metformin because of a marginal increase in HbA1c. We report in our patients an overall remission rate of 78.3% at 12 months, which remained stable at 80% of the patients followed up to 24 months. The rates of emission of type 2 diabetes varied from one study to another. Gill et al21 reviewed the remission rate in the studies between 2000 and 2010 and reported a remission rate of 66.2% in these patients, improvement in glycemic control in 26.9%, and stabilization in 13.1%. The mean decreases in FBG and HbA1c levels after LSG were 88.2 mg/dL and 1.7%, respectively.21 All patients with type 1 diabetes continued their insulin but even in these patients we noticed significant reductions in total daily insulin doses.
Blood pressure changes
Weight loss is well-known to result in reduction in blood pressure in many studies.18–21 In our study we found a very significant reduction in both systolic and diastolic blood pressure at the end of the study, which was maintained up to 24 months. These findings indicate that the benefit from LSG regarding blood pressure is more significant for those with clinically diagnosed hypertension. Another study was conducted retrospectively on 100 patients who underwent LSG, reported a complete resolution of 60% of the total number of those labelled as hypertensives before surgery. This was attained at 1 year postoperatively.22
Other effects
The effect of metabolic surgery on thyroid function tests has been evaluated in a few studies. Zendel et al23 have shown that metabolic surgery resulted in favorable effects in hypothyroid patients, as it is associated with improvements in thyroid function tests, and a reduction in thyroxine dose.23 Interestingly, Neves et al24 concluded that metabolic surgery results in significant reductions in TSH levels independent of EBWL in patients with normal thyroid function tests. Our patients showed similar results with significant reductions in TSH levels over a 12-month period.
Strengths and limitations
One of the major limitations of the trial is the retrospective nature of the trial, however, it is considered to be the first trial in the region that evaluated the effects of metabolic surgery in patients with diabetes exclusively. Unlike many other trials we have also looked at the effects of metabolic surgery in both type 1 and type 2 diabetes. Furthermore, we evaluated many other parameters including effect on TSH levels.
Conclusions
Bariatric surgery in obese patients with diabetes is effective in producing significant weight loss, HbA1c blood pressure, and LDL reduction. More importantly, bariatric surgery results in a very high rate of diabetes and hypertension remission rates. We recommend bariatric surgery as an integral part of diabetes management in obese patients with diabetes. Further studies are required to evaluate the effects of metabolic surgery in patients with diabetes, and specifically type 1 diabetes.
Disclosure
The authors report no conflicts of interest in this work.
References
WHO. Obesity and overweight. Available from: http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed May 26, 2018. | ||
Sulaiman N, Elbadawi S, Hussein A, et al. Prevalence of overweight and obesity in United Arab Emirates expatriates: the UAE National Diabetes and Lifestyle Study. Diabetol Metab Syndr. 2017;9:88. | ||
Sheikh-Ismail LI, Henry CJK, Lightowler HJ, Aldhaheri AS, Masuadi E, Al Hourani HM. Prevalence of overweight and obesity among adult females in the United Arab Emirates. Int J Food Sci Nutr. 2009;60(Suppl 3):26–33. | ||
Mahboub B, Afzal S, Alhariri H, Alzaabi A, Vats M, Soans A. Prevalence of symptoms and risk of sleep apnea in Dubai, UAE. Int J Gen Med. 2013;6:109–114. | ||
EMRO WHO Int [Internet]. Obesity. Cairo, Egypt: World Health Organization Regional Office for the Eastern Mediterranean; 2014. | ||
Alblooshi A, Shaban S, Altunaiji M, et al. Increasing obesity rates in school children in United Arab Emirates. Obes Sci Pract. 2016;2(2):196–202. | ||
Abusnana S, Abdi S, Tagure B, Elbagir M, Maleckas A. Bariatric surgery outcomes: a single-center study in the United Arab Emirates. Diabetes Metab Syndr Obes. 2015;8:461–471. | ||
Brethauer SA, Kim J, El Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11(3):489–506. | ||
AACE/TOS/ASMBS Guidelines. Perioperative bariatric guidelines. Available from: http://www.sunut.org.uy/wp-content/uploads/2012/11/guias-AACE-TOS-ASMBS-BARIATRICA.pdf. Accessed May 26, 2018. | ||
International Diabetes Federation (IDF). Diabetes Atlas, 8th edition. Available from: http://www.diabetesatlas.org/across-the-globe.html. Accessed May 27, 2018. | ||
Nimeri A, Mohamed A, El Hassan E, et al. Are results of bariatric surgery different in the Middle East? Early experience of an international bariatric surgery program and an ACS NSQIP outcomes comparison. J Am Coll Surg. 2013;216(6):1082–1088. | ||
Quercia I, Dutia R, Kotler DP, Belsley S, Laferrère B. Gastrointestinal changes after bariatric surgery. Diabetes Metab. 2014;40(2):87–94. | ||
Beckman LM, Beckman TR, Earthman CP. Changes in gastrointestinal hormones and leptin after Roux-en-Y gastric bypass procedure: a review. J Am Diet Assoc. 2010;110(4):571–584. | ||
Sala PC, Torrinhas RS, Giannella-Neto D, Waitzberg DL. Relationship between gut hormones and glucose homeostasis after bariatric surgery. Diabetol Metab Syndr. 2014;6(1):87. | ||
Elder KA, Wolfe BM. Bariatric surgery: a review of procedures and outcomes. Gastroenterology. 2007;132(6):2253–2271. | ||
Rubino F. Is type 2 diabetes an operable intestinal disease? A provocative yet reasonable hypothesis. Diabetes Care. 2008;31(Suppl 2):S290–S296. | ||
Rubino F, R’bibo SL, del Genio F, Mazumdar M, McGraw TE. Metabolic surgery: the role of the gastrointestinal tract in diabetes mellitus. Nat Rev Endocrinol. 2010;6(2):102–109. | ||
Zhang F, Strain GW, Lei W, et al. Changes in lipid profiles in morbidly obese patients after laparoscopic sleeve gastrectomy (LSG). Obes Surg. 2011;21(3):305–309. | ||
Sampalis JS, Liberman M, Auger S, Christou NV. The impact of weight reduction surgery on health-care costs in morbidly obese patients. Obes Surg. 2004;14(7):939–947. | ||
Berry M, Fajardo M, Villagran R, Lamoza P, Urrutia L. P-113: Laparoscopic sleeve gastrectomy (LSG) impact in diabetic (T2DM) obese patients. Surg Obes Relat Dis. 2010;6(3):S64–S65. | ||
Gill RS, Birch DW, Shi X, Sharma AM, Karmali S. Sleeve gastrectomy and type 2 diabetes mellitus: a systematic review. Surg Obes Relat Dis. 2010;6(6):707–713. | ||
Sammour T, Hill A, Singh P, Ranasingghe S, Babor R. Rahman H. Laparoscopic sleeve gastrectomy as a single stage bariatric procedure. Obes Surg. 2009;20:1442–1450. | ||
Zendel A, Abu-Ghanem Y, Dux J, Mor E, Zippel D, Goitein D. The impact of bariatric surgery on thyroid function and medication use in patients with hypothyroidism. Obes Surg. 2017;27(8):2000–2004. | ||
Neves JS, Castro Oliveira S, Souteiro P, et al. Effect of weight loss after bariatric surgery on thyroid-stimulating hormone levels in patients with morbid obesity and normal thyroid function. Obes Surg. 2018;28(1):97–103. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.