Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
Efficacy and safety of paliperidone palmitate 3-month versus 1-month formulation in patients with schizophrenia: comparison between European and non-European population
Authors Savitz AJ, Xu H , Gopal S , Nuamah I, Ravenstijn P, Hough D, Hargarter L
Received 3 October 2018
Accepted for publication 10 January 2019
Published 21 February 2019 Volume 2019:15 Pages 587—602
DOI https://doi.org/10.2147/NDT.S189668
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Adam J Savitz,1 Haiyan Xu,1 Srihari Gopal,1 Isaac Nuamah,1 Paulien Ravenstijn,2 David Hough,1 Ludger Hargarter3
1Janssen Research & Development, LLC, Raritan, NJ, USA; 2Janssen Research & Development, a Division of Janssen Pharmaceutica NV, Beerse, Belgium; 3Medical & Scientific Affairs, Janssen Cilag EMEA, Neuss, Germany
Purpose: This randomized, double-blind (DB), non-inferiority phase 3 study was conducted to assess the efficacy and safety of paliperidone palmitate 3-month (PP3M) vs 1-month formulation (PP1M) in European and non-European patients with schizophrenia.
Patients and methods: In this randomized, DB, parallel-group study, adult patients (18–70 years) with schizophrenia (per DSM-IV-TR) having Positive and Negative Syndrome Scale (PANSS) total score between 70 and 120; previously stabilized on PP1M were enrolled. The study had 4 phases: screening (3 weeks), open-label (OL) stabilization (17 weeks), DB (48 weeks) and follow-up (4–12 weeks) phase. Patients were treated with fixed-dose PP3M (175–525 mg eq deltoid/gluteal) or PP1M (50–150 mg eq deltoid/gluteal) for 48 weeks in DB phase.
Results: In total, 487 European (PP3M, n=242; PP1M, n=245) and 508 non-European patients (PP3M, n=241; PP1M, n=267) entered DB phase (modified intent-to-treat (mITT) [DB] analysis set). Among the 508 non-European patients in mITT set, 67.7% were from Asia (n=344) and 32.3% were from rest of world (ROW, n=164). During the DB phase, similar percentage of Europeans (PP3M: 7%; PP1M: 8%) and non-Europeans (PP3M: 9%; PP1M: 10%) experienced relapse (Kaplan–Meier estimate PP3M–PP1M [95% CI] of percentage of relapse-free patients at the end of DB phase [primary endpoint]: European: 1.0% [-4.3%; 6.2%]; non-European: 1.4% [-4.4%; 7.1%]; Asian: 1.6% [-5.7%; 9.0%]; and ROW: 1.4% [-7.0%, 9.8%], per-protocol analysis set). Incidence of treatment-emergent adverse events (TEAEs) was lower in Europeans (PP3M: 56%, PP1M: 59%) than non-Europeans (PP3M: 80%, PP1M: 73%). The most commonly reported TEAE was weight gain.
Conclusion: PP3M showed similar efficacy to PP1M in Europeans and non-Europeans, consistent with non-inferiority of PP3M to PP1M observed in overall population. Rates of AEs were higher in non-Europeans. However, weight gain was greater in non-Europeans, especially the Asian population.
Keywords: long-acting injectable, non-inferiority, randomized, relapse, tolerability
Introduction
Non-adherence and partial adherence to oral antipsychotic regimens is a common challenge in patients with schizophrenia,1–4 and is often associated with a poor prognosis for recovery,5 a negative impact on families and caretakers, and a significant economic burden to the public.6 Use of long-acting injectable (LAI) antipsychotics has been suggested to support adherence management,7 and ensure reliable and sustained exposure to pharmacologic treatment and reduce the risk of relapse among patients with schizophrenia.8
Paliperidone palmitate 1-month (PP1M) is an LAI formulation approved for the treatment of schizophrenia in several countries, and also for schizoaffective disorder in the USA.9 A more recently introduced LAI, paliperidone palmitate 3-month (PP3M) formulation, is designed to offer a substantially longer dosing interval, and is approved in the USA,10 the European Union,11 and other countries for the maintenance treatment of schizophrenia in patients previously treated with PP1M. Results from two long-term, multicenter phase 3 studies have demonstrated that a larger proportion of patients with schizophrenia, who were stabilized with PP1M for ≥4 months followed by treatment with PP3M (PP1M × 3.5 doses: 175, 263, 350 or 525 mg eq), did not experience relapse vs placebo.12 Additionally, PP3M was non-inferior to PP1M with similarly low relapse rates in both groups.13
Race and ethnic differences as well as differences in healthcare systems may influence treatment response, and safety profiles associated with antipsychotic treatment. Comparison of efficacy across different geographic regions is important because the response rates sometimes differ. The reasons for such differences are not easy to pinpoint, but may be due to culture, differences in medical care and even pharmacogenetic variations (eg, of the cytochrome P450 family of oxidative enzymes, CYP450) leading to differences in metabolism. Hence, we believe it is important to compare the efficacy across regions.14–16 The current study is a subgroup analysis of a long-term, multicenter, phase 3 study that analyzed the non-inferiority of PP3M over PP1M in the treatment of symptoms of schizophrenia.13 The objective of this subgroup analysis was to assess the comparative efficacy of PP3M vs PP1M in European patients with schizophrenia previously stabilized on PP1M, and to compare their efficacy and safety outcomes with non-European populations.
Patients and methods
Study population
This subgroup analysis was based on data from a phase 3, double-blind (DB), parallel-group, non-inferiority study. (EudraCT Number: 2011-004889-15) conducted at 199 sites across 26 countries from April 2012 to March 2015 (16 countries in Europe). The primary study is published elsewhere.13 In brief, this randomized study enrolled adult (18–70 years old) patients of either sex, with schizophrenia (Diagnostic and Statistical Manual of Mental Disorders, fourth-Edition [DSM-IV-TR]), having a screening and baseline Positive and Negative Syndrome Scale (PANSS) total score between 70 and 120, and with deterioration of schizophrenia symptoms. Patients who stopped other antipsychotics because they preferred injectables or as a result of insufficient efficacy or safety or tolerability concerns with the existing therapy were included in the present study.
The key exclusion criteria were: patients with active DSM-IV diagnoses besides schizophrenia, significant suicidal behavior risk substance dependence 6 months before screening, tardive dyskinesia, neuroleptic malignant syndrome, significant medical or neurological illness, mental retardation, morbid obesity (BMI >40 kg/m2), prolonged QT interval risk factors, torsades de pointes, or sudden death. Other exclusion criteria were: no response, or history of intolerability, or hypersensitivity to risperidone or paliperidone.
The study protocol and amendments were reviewed and approved by each site’s Independent Ethics Committee or Institutional Review Board (Supplementary material). The study was conducted in compliance with the Declaration of Helsinki and applicable regulatory requirements. All patients provided written informed consent prior to study enrollment.
Study design
The study was divided into 4 phases: up to 3 weeks screening, 17 weeks open-label (OL) stabilization (flexible doses), 48 weeks DB (fixed doses) and 4–12 weeks follow-up. Oral tolerability testing was performed during screening (paliperidone extended release 6 mg/day for 4–6 consecutive days) in patients who were not previously exposed to oral or injectable risperidone or paliperidone. After completing the screening phase and meeting all eligibility criteria, patients entered the OL stabilization phase where they received PP1M as follows: 150 mg eq (deltoid) on day 1; 100 mg eq (deltoid) on day 8; flexibly dosed 50, 75, 100, or 150 mg eq (deltoid or gluteal) at weeks 5 and 9; and same PP1M dose as week 9 maintained at week 13. Clinically stable patients (defined as patients with <70 PANSS total score with ≤4 PANSS item [P1, P2, P3, P6, P7, G8, G14] scores and ≥1 reduction at weeks 14 and 17 from OL baseline in CGI-S score) then began the DB phase of 48 weeks. In the DB phase, patients were randomized (1:1) to fixed doses of 175, 263, 350, or 525 mg eq PP3M at weeks 17, 29, 41 and 53; or 50, 75, 100, or 150 mg eq PP1M every month.13 Blinding was maintained in the PP3M group with monthly matched placebo injections (20% Intralipid®) as a substitute for active medication.
Efficacy
The percentage of patients who remained relapse-free (based on the Kaplan–Meier cumulative estimate of survival) by the end of DB phase (48 weeks) was the endpoint for primary efficacy. Relapse was defined as one or more of the following: 1) hospitalization for symptoms of schizophrenia (involuntary or voluntary admission); 2) for patients scoring >40 at randomization, an increase of 25% in PANSS total score from randomization for two consecutive assessments (3–7 days apart) or an increase in 10 points for patients who scored ≤40 at randomization; 3) increase in distinct PANSS item scores (P1, P2, P3, P6, P7, or G8) for two consecutive assessments (3–7 days apart; increase defined as PANSS item scores ≥5 after randomization for 2 consecutive assessments separated by 3–7 days if the maximum score for the above PANSS items was ≥3 at randomization, or ≥6 after randomization if the maximum score for the above PANSS items was 4 at randomization); 4) deliberate self-injury or violent behavior that was clinically significant; and 5) suicidal or homicidal ideation and aggressive behavior. Based on PANSS ratings, the occurrence of relapse was ascertained when the increased symptoms were first presented and a second assessment (within 3–7 days post first assessment) further confirmed it.
The secondary efficacy endpoints included changes from baseline (DB phase) to DB endpoint in PANSS total score, Clinical Global Impressions of Severity (CGI-S) scale, Personal and Social Performance (PSP) scale, proportion of patients who achieved symptomatic remission during the last 6 months before the end of DB phase (defined as meeting the Andreasen et al17 remission criteria during the 6 months prior to end of DB phase, with no excursion allowed), and proportion of patients who achieved both symptomatic and functional remission. Criterion for symptomatic remission was defined as having a simultaneous score of mild or less on all selected PANSS items (P1, P2, P3, N1, N4, N6, G5, and G9). Functional remission criterion was defined as having PSP score >70.
Safety
Safety evaluations included assessment of incidence of treatment-emergent adverse events (TEAEs), changes in extrapyramidal symptoms (EPS) scales18 (Abnormal Involuntary Movement Scale [AIMS], Barnes Akathisia Rating Scale [BARS], and Simpson and Angus Rating Scale [SARS]), suicidal ideation and behavior using Columbia Suicide Severity Rating Scale (C-SSRS), clinical laboratory tests (prolactin levels and glucose levels), vital signs measurements and body weight, electrocardiograms, and injection site evaluations.
Statistical analysis
Sample size determination
The target overall sample size of the global study was 1,388 patients. Assuming a relapse-free rate of 70% for PP1M, a true difference of 4% in relapse-free survival favoring PP1M vs PP3M, and a 1-sided significance level of 2.5%, 380 patients per treatment group were required to demonstrate with 90% power that PP3M was similar to PP1M by a non-inferiority margin of 15% in relapse-free survival rates. Although the subgroup analysis part of the study was not powered, the global study was designed to have a sufficiently large European population to show consistency of results between the global population and the European population.
Statistical analyses
The Kaplan–Meier method was used to derive the 48-week cumulative estimate of relapse-free survival. Greenwood’s formula was used to compute the standard error (SE) estimates. Treatment comparisons during the DB phase between PP3M and PP1M for the changes from baseline for PANSS total score, PSP, and CGI-S were performed by an analysis of covariance (ANCOVA) model where treatment and country were factors and baseline (DB phase) value was a covariate. Proportion of patients who achieved symptomatic remission17 was evaluated using the Cochran–Mantel–Haenszel test controlling for country. The point estimate and 95% CI for the relative risk of remission were presented. Safety results were analyzed descriptively.
The intent-to-treat (ITT) OL analysis set was used for all efficacy and safety analyses for the OL phase and included all patients who had received at least 1 dose of study drug during the OL phase. The primary efficacy analysis was performed by using the per-protocol (PP) analysis set, which included all randomized patients who received at least 1 dose of study drug during the DB phase and did not have major protocol violations (eg, violations of intended study population treatment assignment errors or excluded medication use). For all secondary efficacy analyses for the DB phase, the modified ITT-DB analysis set (mITT-DB, defined as all patients who received at least 1 dose of study drug during the DB phase, with no errors in the delivery of active treatment due to manufacturing of the investigational product) was used. DB phase safety analyses were performed using the safety analysis set (defined as all patients who received at least 1 dose of study drug during the DB phase). Since about two-thirds of non-Europeans in this study were from Asia, we have also provided limited data on patients from Asia and rest of the world (ROW). Complete details on efficacy and safety of PP1M and PP3M in Asian sub-analyses are provided elsewhere.19
Results
Patient demographics
Overall, 647 European patients were enrolled in the study and were treated in the OL phase (ITT [OL] analysis set) (Table 1), and 498 (77% of those enrolled in the OL phase) European patients (PP3M: n=253; PP1M: n=245) were randomized to the DB phase (Table 1). In the OL phase, the most common reasons for discontinuation were lack of efficacy (8%, n=54) and withdrawal of consent (6%, n=42; Figure 1). The PP-analysis set included 467/498 randomized patients, (PP3M: n=229; PP1M: n=238), while the mITT (DB) analysis set included 487/498 patients (PP3M: n=242; PP1M: n=245). In total, 414 (85%) patients completed the DB phase (inclusive of relapsed patients, mITT [DB] analysis set; in both the treatment arms, the proportion was similar for completion (PP3M, 86% and PP1M, 84%) and for completion without a relapse (PP3M: n=189, 78%; PP1M: n=187, 76%). In the DB phase, most patients discontinued as they withdrew consent (Figure 1).
For non-European regions, 782 patients were enrolled and received treatment in the OL phase (ITT [OL] analysis set; patients from Asia: 510 and patients from ROW: 272); of these, 518 patients (66% of patients enrolled in OL) were randomized in the DB phase (PP3M: n=251; PP1M: n=267) (Table 1). In total 481/518 randomized patients were included in the PP-analysis set (Asia: n=335; ROW: n=146), while 508 patients were included in the mITT (DB) analysis set (PP3M: n=241; PP1M: n=267; Asia: 344 patients [PP3M: n=170; PP1M: n=174]; ROW: n=164 [PP3M: n=71; PP1M: n=93]; mITT [DB] analysis set).
In total, 410 (81%) non-European patients completed the DB phase (including patients with relapse, mITT [DB] analysis set); similar percentages of patients in both treatment groups completed the DB phase (mITT [DB] analysis set, PP3M: 82%; PP1M: 80%; Asia: n=285, 83%; ROW: n=125, 76%). Furthermore, similar percentages of patients completed the DB phase without a relapse (PP3M: n=177, 73%; PP1M: n=186, 70%; Asia: n=248, 72%; ROW: n=115, 70%), although the number of patients in ROW subgroup was slightly lower than in the Asian and European subgroups. Similar to the European patients, withdrawal of consent was the most common reason for discontinuation for both treatment groups in the DB phase (mITT [DB] analysis set, overall: n=48, 9%; PP3M: n=26, 11%, PP1M: n=22, 8%; Asia: n=36, 10% [PP3M: n=19, 11%; PP1M: n=17, 10%]; ROW: n=12, 7% [PP3M: n=7, 10%; PP1M: n=5, 5%]).
Baseline (OL) characteristics were similar across both European and non-European patients except that most patients in the European subgroup were white (97%) while a majority of patients in the non-European subgroup were Asians (65%). Current nicotine usage was higher in the European (53%) vs non-European subgroup (35%) (Table 2). Among the 508 non-European patients in mITT (DB) set, 67.7% were from Asia (n=344) and 32.3% were from rest of world (ROW, n=164) (Table 2).
Prior and concomitant medications
Before entry into the study, similar percentage of patients in the European (92%) and non-European subgroups (89%) received ≥1 psychotropic medications (Table 2). During the DB phase, a higher percentage of patients in the non-European subgroup received benzodiazepines (safety analysis set, n=145, 28%; lorazepam: n=102, 20%) than European subgroup (safety analysis set, n=97, 19%; lorazepam: n=34, 7%). However, within the subgroups, similar percentage of patients treated with PP3M and PP1M received benzodiazepines during the DB phase (European subgroup, PP3M: n=46, 18%; PP1M: n=51, 21%; non-European subgroup, PP3M: n=74, 29%; PP1M: n=71, 27%) with lorazepam overall being the most common (>10% patients) benzodiazepine (European subgroup, PP3M: n=15, 6%; PP1M: n=19, 8%; non-European subgroup, PP3M: n=51, 20%; PP1M: n=51, 19%).
Extent of exposure
Similar exposure was observed in all three subgroups (European, Asian and ROW) between patients from both treatment groups (Table 3). Patients in European, Asian and ROW subgroup received similar mean (SD) PP3M dose and PP1M dose.
Efficacy
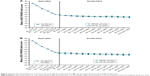
In the European subgroup, a similar proportion of patients in both treatment groups (PP-analysis set, PP3M: 7%, n=17; PP1M: 8%, n=20) relapsed during the DB phase. Results were consistent in the non-European subgroup (PP-analysis set, PP3M: 9%, n=20; PP1M: 10%, n=25; Asia: n=37, 11% [PP3M: n=17, 10%; PP1M: n=20, 12%]; ROW: n=8, 5% [PP3M: n=3, 5%; PP1M: n=5, 6%]). The Kaplan–Meier estimates of the difference (95% CI) between PP3M and PP1M treatment groups in patients who remained relapse-free were similar between European subgroup (1.0% [-4.3%; 6.2%]) and non-European subgroup (1.4% [-4.4%; 7.1%]; Asia: 1.6% [-5.7%; 9.0%]; ROW: 1.4% [-7.0%; 9.8%]), and global population (1.2% [-2.7%; 5.1%]); the lower bound of the 95% CI was larger than the pre-specified non-inferiority margin of -15% in both subgroups as well as in the global population. Additionally, the estimate based on the mITT (DB) analysis set was consistent with the PP-analysis set in both European as well as non-European subgroups (difference PP3M-PP1M, [95% CI]: European subgroup: 0.8% [-4.3%, 5.9%]; non-European subgroup: 2.1% [-3.4%, 7.7%]; Asia: 1.7% [-5.5%; 8.9%]; ROW: 3.5% [-4.5%; 11.6%]). Due to the low number of relapses, the median time-to-relapse was not estimable in both European and non-European subgroups for patients in both treatment groups (Figure 2).
The secondary efficacy endpoints (PANSS total score, CGI-S and PSP scores) also showed similar improvements in both treatment groups from DB baseline to DB endpoint in European and non-European patients (Table 4 and Figure 3). In both treatment groups of European patients, a similar percentage (52% in each group) showed symptomatic remission with 0.98 (95% CI: 0.83, 1.15) relative risk of remission for PP3M vs PP1M. Similar percentage of European patients in both PP3M and PP1M achieved symptomatic remission as well as both the symptomatic and functional remission at different timepoints during the DB phase (Figure 4).
Safety
Overall, 308 (ITT [OL] analysis set) patients in the European subgroup (48%) experienced ≥1 TEAE, 40 patients (6%) experienced ≥1 serious TEAE, and 24 patients (4%) had a TEAE leading to study drug discontinuation during the OL phase (Table 5). In contrast, higher percentage of patients (ITT [OL] analysis set) in the Asian and ROW subgroups (Asia: 71%, ROW: 64%) experienced ≥1 TEAE during the OL phase; <10% of patients experienced ≥1 serious TEAEs (Asia: n=43 [8%], ROW: n=18 [7%]) and TEAE leading to discontinuation of study drug (Asia: 25 [5%], ROW: n=11 [4%]) in the OL phase. The most common TEAEs (≥5% patients) reported in the European subgroup during the OL phase were injection site pain (11%) while those experienced by patients in the non-European subgroup (≥10% in either Asian or ROW subgroup) during the OL phase included insomnia (Asia: 11%; ROW: 4%), akathisia (Asia: 10%; ROW: 5%) and increased weight (Asia: 6%; ROW: 11%).
Higher percentage of patients (76%) in the non-European subgroup experienced ≥1 TEAE than the European subgroup (58%) during the DB phase. However, within the subgroups, similar percentages of patients in both treatment groups experienced ≥1 TEAE (safety analysis set, European subgroup, PP3M: n=142 [56%]; PP1M: n=145 [59%]; Asia: PP3M: n=138 [81%]; PP1M: n=132 [76%]; ROW: PP3M: n=62 [77%]; PP1M: n=63 [68%]) during the DB phase. The most common (≥5% patients) TEAEs occurring in patients of both European and non-European subgroups following either PP1M or PP3M treatments during the DB phase included increased weight, followed by nasopharyngitis, and anxiety (Table 5).
There were 2 deaths in the European subgroup (DB phase: PP1M-treated, one due to suicide and the other due to bacterial meningitis) vs 4 deaths in the non-European subgroup (OL phase: n=2 [arteriosclerosis and cardiac arrest, n=1 each]; DB phase: n=2; PP3M: n=1 [hepatocellular carcinoma]; PP1M: n=1 [toxicity to various agents]) during the study. Most common serious TEAEs in the European and non-European patients were psychiatric-related generally indicating worsening of the underlying disease (Table 5). Incidence of EPS-related TEAEs was similar between PP3M and PP1M treated patients of European and non-European subgroups; however, the incidence was slightly more in the non-European subgroup than the European subgroup (Table 5).
The mean (SD) weight change from OL baseline to DB endpoint was similar between PP3M and PP1M treated patients of both European as well as non-European subgroups, though weight gain was overall less in the European population (Europe, PP3M: 1.3 [6.52] kg, PP1M: 2.3 [6.13] kg; Non-Europe, PP3M: 3.1 [7.30] kg, PP1M: 3.8 [7.14] kg) (Table 6). Diabetes mellitus and hyperglycemia-related TEAEs were low and similar between PP3M and PP1M-treated patients in the European, Asian and ROW subgroups (Table 5). Incidence of injection site-related TEAEs was similar between PP3M and PP1M-treated patients of the European, Asian and ROW subgroups during the DB phase (Table 5). The local injection site tolerability was good in European, Asian and ROW subgroups.
Discussion
The results of the current subgroup analysis demonstrated the non-inferiority of PP3M to PP1M; primary efficacy results (ie, relapse-free rates at end of 48-week DB phase) in European and non-European (which had a significant proportion of Asian population [65%]) subgroups are similar and consistent with that observed in the global population.13 Most patients in both subgroups (>70%) on both treatments completed the 48-week DB phase without a relapse. These findings are consistent with the results of the global study.13
The secondary efficacy endpoint results also suggested that PP3M showed similar efficacy to PP1M in the maintenance treatment of European patients with schizophrenia. Symptomatic remission was achieved in the majority of European and non-European patients in both treatment groups throughout the last 6 months of DB treatment. These results are in agreement with the findings of similar relapse-prevention studies assessing the efficacy of PP1M in maintaining symptomatic control in patients with schizophrenia,20–25 and the long-term maintenance study using PP3M.12
Comparable safety and tolerability profiles were noted for PP3M and PP1M during the DB phase in the European patients. Incidence of TEAEs was lower in the European patients compared with the non-European patients. It should be noted that the majority of patients in the non-European subgroup were Asians and Asian patients have been shown to be somewhat more susceptible to adverse events.19 Low discontinuations due to TEAEs were comparable for PP1M and PP3M treatments in European and non-European subgroups. Serious TEAEs were similar between both treatment groups in European and non-European patients and were mostly psychiatric-related. Weight gain and nasopharyngitis were the most common TEAEs observed in both treatment groups. A higher incidence of akathisia, and increased glucose levels were observed in the non-European population compared with the European population. Weight gain was less in European patients compared with non-European patients; this may be due to higher baseline BMI in European patients compared with the ROW which were majority Asian.26–28 Evidence also suggests that baseline BMI differs between Asians and Europeans.29 A subgroup analysis of the same study comparing the Asian and global populations demonstrated that incidence of weight gain was greater in the Asian subgroup (31% in both groups) compared with the global population (21% in both groups).19 The extent of weight gain in the Asian subgroup (<2 kg) was comparable with the global population (~1.5 kg)19 and was consistent with earlier studies.22,23,25 Previous studies also reported similar weight gain in Asian patients treated with PP1M.30,31 No new safety signals emerged.
This study, as a post hoc study, was not powered to show statistical significance for a subgroup analysis. However, the primary study was a fully powered non-inferiority study and enrolled a sufficient number of patients to derive meaningful conclusions from this subgroup analysis. Unlike real life practice, PP3M-treated patients in both European and non-European subgroups had only 2 opportunities for dose adjustments. Further, all patients received monthly injections to maintain the blind. The high completion rates, low relapse rates and low discontinuations due to TEAEs can be attributed to the fact that patients who entered the DB phase were already able to tolerate and respond to PP1M. Some varied responses observed in the study may be attributed to the occurrence of different ethnicities as well as differences in healthcare delivery within the European populations. PP3M could offer advantages by enhancing the number of available treatment options and potentially offering improved outcomes for European patients with schizophrenia.
Conclusion
The efficacy findings of this subgroup analysis (between European and non-European patients) corroborate those of the primary study in PP3M- and PP1M-treatment groups. A greater percentage of non-Europeans, especially Asian population, had weight gain compared to Europeans. No new safety signals were noted during the course of this study. Therefore, PP3M could be considered as a useful treatment option to prevent relapse in schizophrenia in European patients.
Data sharing statement
Acknowledgments
Dr Shruti Shah and Dr Himabindu Gutha (both SIRO Clinpharm Pvt. Ltd) provided writing assistance and Dr Ellen Baum (Janssen Research & Development, LLC) provided additional editorial support for this manuscript. Authors thank Dr Wolfgang Fleischhacker for scientific advice. The authors also thank the study participants, without whom this study would never have been accomplished, and all the investigators for their participation in this study. Portions of this work were previously presented as a poster at ‘29th ECNP congress’, Vienna, Austria, September 17–20, 2016; DGPPN Congress, City Cube Berlin, Germany, November 23–26, 2016; Society of Biological Psychiatry (SOBP) 72nd Annual Scientific Convention, May 18–20, 2017, San Diego, California and poster abstract was published in European Neuropsychopharmacology; 26:S548–S549: DOI: https://doi.org/10.1016/S0924-977X(16)31592-9; and in Biological Psychiatry; 81:S211: DOI: https://doi.org/10.1016/j.biopsych.2017.02.1127.
Author contributions
Drs Savitz, Gopal, Hargarter, and Hough were involved in study design, data collection, analysis and interpretation. Drs Xu and Nuamah were responsible for the statistical analyses and design/interpretation of study results. Dr Ravenstijn was involved in pharmacokinetic analysis. All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors meet ICMJE criteria and all those who fulfilled those criteria are listed as authors. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
All authors except for Dr Hargarter are employees of Janssen Research & Development; Dr Hargarter is a former employee of Janssen Cilag EMEA. All authors own stock in Johnson & Johnson the parent company of the Janssen companies. The authors report no other conflicts of interest in this work.
References
Bhanji NH, Chouinard G, Margolese HC. A review of compliance, depot intramuscular antipsychotics and the new long-acting injectable atypical antipsychotic risperidone in schizophrenia. Eur Neuropsychopharmacol. 2004;14(2):87–92. | ||
Lieberman JA, Stroup TS, Mcevoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–1223. | ||
Valenstein M, Ganoczy D, Mccarthy JF, Myra Kim H, Lee TA, Blow FC. Antipsychotic adherence over time among patients receiving treatment for schizophrenia: a retrospective review. J Clin Psychiatry. 2006;67(10):1542–1550. | ||
Weiden PJ, Kozma C, Grogg A, Locklear J. Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. PS. 2004;55(8):886–891. | ||
Doering S, Müller E, Köpcke W, et al. Predictors of relapse and rehospitalization in schizophrenia and schizoaffective disorder. Schizophr Bull. 1998;24(1):87–98. | ||
Knapp M, King D, Pugner K, Lapuerta P. Non-adherence to antipsychotic medication regimens: associations with resource use and costs. Br J Psychiatry. 2004;184(06):509–516. | ||
Rauch AS, Fleischhacker WW. Long-acting injectable formulations of new-generation antipsychotics: a review from a clinical perspective. CNS Drugs. 2013;27(8):637–652. | ||
Emsley R, Oosthuizen P, Koen L, Niehaus DJ, Medori R, Rabinowitz J. Oral versus injectable antipsychotic treatment in early psychosis: post hoc comparison of two studies. Clin Ther. 2008;30(12):2378–2386. | ||
Invega Sustenna® (paliperidone palmitate) extended-release injectable suspension, for intramuscular use [prescribing information]. USA: Janseen Pharmaceutical Companies; 2015. | ||
Invega Trinza® (paliperidone palmitate) extended-release injectable suspension, for intramuscular use [prescribing information]. USA: Janseen Pharmaceutical Companies; 2015. | ||
TREVICTA (paliperidone palmitate) [summary of product characteristics]. Belgium: Janseen Pharmaceutica NV; 2014. | ||
Berwaerts J, Liu Y, Gopal S, et al. Efficacy and safety of the 3-month formulation of paliperidone palmitate vs placebo for relapse prevention of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2015;72(8):830–839. | ||
Savitz AJ, Xu H, Gopal S, et al. Efficacy and safety of paliperidone palmitate 3-month formulation for patients with schizophrenia: a randomized, multicenter, double-blind, Noninferiority study. Int J Neuropsychopharmacol. 2016;19(7):pii:pyw018. | ||
Banerjee AA. Cross-cultural variance of schizophrenia in symptoms diagnosis and treatment. The Georgetown Undergrad J Health Sci. 2012;6(2):18–24. | ||
Bauer SM, Schanda H, Karakula H, et al. Culture and the prevalence of hallucinations in schizophrenia. Compr Psychiatry. 2011;52(3):319–325. | ||
Stauffer VL, Sniadecki JL, Piezer KW, et al. Impact of race on efficacy and safety during treatment with olanzapine in schizophrenia, schizophreniform or schizoaffective disorder. BMC Psychiatry. 2010;10(1):89. | ||
Andreasen NC, Carpenter WT, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162(3):441–449. | ||
Guy W. ECDEU assessment manual for psychopharmacology. U S Department of Health, and Welfare. 1976:534–537. | ||
Savitz AJ, Xu H, Gopal S, et al. Efficacy and safety of paliperidone palmitate three-monthly formulation in East Asian patients with schizophrenia: Subgroup analysis of a global, randomized, double-blind, phase III, noninferiority study. Neuropsychiatr Dis Treat. 2017;13:2193–2207. | ||
Coppola D, Liu Y, Gopal S, et al. A one-year prospective study of the safety, tolerability and pharmacokinetics of the highest available dose of paliperidone palmitate in patients with schizophrenia. BMC Psychiatry. 2012;12(1):26. | ||
Gopal S, Vijapurkar U, Lim P, Morozova M, Eerdekens M, Hough D. A 52-week open-label study of the safety and tolerability of paliperidone palmitate in patients with schizophrenia. J Psychopharmacol. 2011;25(5):685–697. | ||
Hough D, Gopal S, Vijapurkar U, Lim P, Morozova M, Eerdekens M. Paliperidone palmitate maintenance treatment in delaying the time-to-relapse in patients with schizophrenia: a randomized, double-blind, placebo-controlled study. Schizophr Res. 2010;116(2–3):107–117. | ||
Kramer M, Litman R, Hough D, et al. Paliperidone palmitate, a potential long-acting treatment for patients with schizophrenia. Results of a randomized, double-blind, placebo-controlled efficacy and safety study. Int J Neuropsychopharmacol. 2010;13(5):635–647. | ||
Nasrallah HA, Gopal S, Gassmann-Mayer C, et al. A controlled, evidence-based trial of paliperidone palmitate, a long-acting injectable antipsychotic, in schizophrenia. Neuropsychopharmacology. 2010;35(10):2072–2082. | ||
Pandina GJ, Lindenmayer JP, Lull J, et al. A randomized, placebo-controlled study to assess the efficacy and safety of 3 doses of paliperidone palmitate in adults with acutely exacerbated schizophrenia. J Clin Psychopharmacol. 2010;30(3):235–244. | ||
Dayabandara M, Hanwella R, Ratnatunga S, Seneviratne S, Suraweera C, de Silva VA. Antipsychotic-associated weight gain: management strategies and impact on treatment adherence. Neuropsychiatr Dis Treat. 2017;13:2231–2241. | ||
Vandenberghe F, Gholam-Rezaee M, Saigí-Morgui N, et al. Importance of early weight changes to predict long-term weight gain during psychotropic drug treatment. J Clin Psychiatry. 2015;76(11):e1417–e1423. | ||
Bushe CJ, Slooff CJ, Haddad PM, Karagianis JL. Weight change by baseline BMI from three-year observational data: findings from the worldwide schizophrenia outpatient health outcomes database. J Psychopharmacol. 2013;27(4):358–365. | ||
Bailey SD, Xie C, Paré G, et al. Variation at the DPP4 locus influences apolipoprotein B levels in South Asians and exhibits heterogeneity in Europeans related to BMI. Diabetologia. 2014;57(4):738–745. | ||
Li H, Rui Q, Ning X, Xu H, Gu N. A comparative study of paliperidone palmitate and risperidone long-acting injectable therapy in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(4):1002–1008. | ||
Takahashi N, Takahashi M, Saito T, et al. Randomized, placebo-controlled, double-blind study assessing the efficacy and safety of paliperidone palmitate in Asian patients with schizophrenia. Neuropsychiatr Dis Treat. 2013;9:1889–1898. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.