Back to Journals » Journal of Asthma and Allergy » Volume 15
Efficacy and Safety of Fluticasone Furoate and Oxymetazoline Nasal Spray: A Novel First Fixed Dose Combination for the Management of Allergic Rhinitis with Nasal Congestion
Authors Kumar RS, Jain MK, Kushwaha JS, Patil S, Patil V, Ghatak S, Sanmukhani J , Mittal R
Received 12 March 2022
Accepted for publication 25 April 2022
Published 10 June 2022 Volume 2022:15 Pages 783—792
DOI https://doi.org/10.2147/JAA.S357288
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Luis Garcia-Marcos
RS Kumar,1 Manish Kumar Jain,2 Jitendra Singh Kushwaha,3 Santosh Patil,4 Vasanti Patil,5 Soumya Ghatak,6 Jayesh Sanmukhani,7 Ravindra Mittal7
1Department of Pulmonary Medicine, Government Medical College & Government General Hospital, Srikakulam, India; 2Department of Pulmonary Medicine, Maharaja Agrasen Superspeciality Hospital, Jaipur, India; 3Department of Medicine, Prakhar Hospital Pvt. Ltd, Kanpur, India; 4Department of ENT, Jeevan Rekha Hospital, Belgavi, India; 5Department of ENT, Rajarshi Chhatrapati Shahu Maharaj Government Medical College and CPR Hospital, Kolhapur, India; 6Department of ENT, College of Medicine and Sagore Dutta Hospital, Kolkata, India; 7Department of Clinical Research and Regulatory Affairs, Cadila Healthcare Limited, Ahmedabad, India
Correspondence: Jayesh Sanmukhani, Department of Clinical Research and Regulatory Affairs, Cadila Healthcare Ltd, Ahmedabad, India, Tel +91 76000 12192, Email [email protected]; [email protected]
Objective: To compare the efficacy and safety of a fixed dose combination of Fluticasone Furoate and Oxymetazoline Hydrochloride Nasal Spray 27.5/50 mcg (FDC) with Fluticasone Furoate Nasal Spray 27.5 mcg (Fluticasone) in the management of allergic rhinitis.
Patients and Methods: A prospective, randomized, double-blind, two-arm, active-controlled, parallel, multicenter, comparative clinical study was conducted in patients with allergic rhinitis aged 18 years and above having moderate-to-severe nasal congestion.
Results: A total of 250 patients were randomized (1:1) to receive either the FDC or Fluticasone alone in a dose of two sprays in each nostril once daily at night. There was a significantly (P< 0.001) greater reduction in night-time Total Nasal Symptom Score with the FDC as compared to Fluticasone at all the time points starting from as early as day 3 and sustained till the end of treatment (Day 28) (Day 3: − 3.1 vs − 2.2; Day 7: − 4.0 vs − 3.4; Day 14: − 5.7 vs − 5.0; Day 28: − 7.0 vs − 6.4). A significantly greater number of patients (P< 0.05) had complete relief in Nasal Congestion with the FDC (44.7%) as compared to Fluticasone (26.8%). Both the study medications were well tolerated by all the patients. The proportion of patients showing worsening of symptoms (rebound congestion/rhinitis medicamentosa) after stoppage of medication was similar in both groups (P> 0.05).
Conclusion: The FDC was superior to Fluticasone alone in relieving the nasal congestion and reduction of Total Nasal Symptom Score in allergic rhinitis patients with moderate-to-severe nasal congestion when administered once daily in the evening. Oxymetazoline when used along with the nasal steroid in a once daily dose does not cause rebound congestion and rhinitis medicamentosa even after long-term continuous use of 28 days.
Keywords: Fluticasone Furoate, oxymetazoline, nasal spray, allergic rhinitis, nasal congestion
Introduction
Allergic rhinitis is a common inflammatory disease condition of the upper respiratory tract. The disease is quite prevalent across the world, with reports ranging from 10–40% in various age groups in the western world including the United States and 10–13% in India (Delhi state of North India).1,2 Moreover, its symptoms are often associated with asthmatic children (up to 75%) and adults (up to 80%). The disease has a great impact on various aspects of patient’s quality-of-life (physical, social, and psychological).3,4 It is currently being managed by various non-pharmacological (steam inhalation, etc.) and pharmacological (oral and intranasal) modalities, however, intranasal steroids are considered to be the first line of management for both the nasal and ocular symptoms5 and are preferred over oral H1-antihistamines and leukotriene receptor antagonists and intranasal H1-antihistamines.
Fluticasone Furoate is an intranasal glucocorticoid with enhanced receptor affinity, potent and long anti-inflammatory activity and low systemic bioavailability in comparison to other glucocorticoids currently in usage. It is one of the most commonly used intranasal steroids for the treatment of allergic rhinitis.4 Fluticasone Furoate nasal spray (27.5 mcg per spray) is already approved for the treatment of symptoms of allergic rhinitis in various countries.
Although intranasal steroids are the first line of treatment, only about 60% of subjects achieve excellent relief with the same in the clinical studies. Also the effect of intranasal steroids takes a few days to reach maximum efficacy (even though the effect starts after 12 hours), thereby suggesting the need for improved treatment modalities.6 As nasal congestion is the most commonly reported and bothersome symptom severely impacting the quality-of-life and productivity of the patients with allergic rhinitis,7 it is prudent to use additional medications for the management of moderate-to-severe nasal congestion to tide over the crisis to such a time that the intranasal steroids reach their maximum efficacy. As per the recommendations of the Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines, intranasal decongestants should be used along with intranasal steroids for the management of patients with allergic rhinitis having moderate-to-severe nasal obstruction.5 Intranasal decongestants are known to have the best effect on nasal obstruction amongst all the pharmacotherapy options approved for the management of allergic rhinitis.8
Oxymetazoline is an adrenomimetic that nonselectively agonizes α1- and α2-adrenergic receptors and endothelial postsynaptic α2 receptors, resulting in vasoconstriction in the nasal vascular beds when applied locally. Oxymetazoline has a nearly instantaneous onset of action (5–10 minutes).6 Oxymetazoline Hydrochloride Nasal Spray 0.05%w/w is approved in various countries and is commonly used over the counter for the relief of stuffy nose.
Considering the limited efficacy of intranasal steroids in patients with allergic rhinitis having moderate-to-severe nasal obstruction and the beneficial effects of oxymetazoline hydrochloride in the management of nasal obstruction, a fixed dose combination of Fluticasone Furoate and Oxymetazoline Hydrochloride Nasal Spray has been developed by M/s Cadila Healthcare Limited (India). The efficacy and safety of the concomitant use of Fluticasone Furoate and Oxymetazoline Hydrochloride Nasal Spray (as separate sprays) has been evaluated in various clinical trials before suggesting that the addition of a nasal decongestant to intranasal steroids adds to the efficacy of steroids alone.7,9 Besides the improvement in efficacy, various studies have also shown that concomitant use of intranasal steroids ameliorates the rebound congestion known to occur with the long-term use of intranasal decongestants.7,9–11 The current Phase III clinical study was conducted to evaluate the efficacy and safety of the fixed dose combination of Fluticasone Furoate and Oxymetazoline Hydrochloride Nasal Spray in patients with allergic rhinitis having moderate-to-severe nasal congestion.
Patients and Methods
This prospective, randomized, double-blind, two-arm, active-controlled, parallel, multicenter, comparative phase III clinical trial was conducted at six tertiary care centers in India from December 2020 to March 2021. The study was conducted by ENT consultants, pulmonologists, and physicians after approval from the Drugs Controller General of India (National Regulatory Authority) and local Institutional Ethics Committees at each center. The study was registered on the Clinical Trials Registry of India (www.ctri.nic.in;CTRI/2020/10/028347) before initiation. Written informed consent was obtained from all the patients prior to initiation of any study-related activity. The study was conducted in compliance with the ‘Guidelines for Clinical Trials on Pharmaceutical Products in India - GCP Guidelines’ and the ethical principles of the Declaration of Helsinki.
Patients
Patients aged 18–65 years of either sex were enrolled in the study. Patients were required to have a documented clinical history of seasonal allergic rhinitis with exacerbation during the study season with a Total Nasal Symptom Score (TNSS) ≥6, a Nasal Congestion Score ≥2, and adequate literacy to complete the diary card.
Patients were excluded from the study if they had allergic rhinitis with little or no seasonal exacerbations or nonallergic rhinitis or had a documented evidence of acute or chronic sinusitis, chronic purulent postnasal drip, rhinitis sicca, atrophic rhinitis, or rhinitis medicamentosa, nasal structure abnormalities, including nasal ulceration, nasal mucosal erosion, large nasal polyps, marked septal deviations, or recent nasal surgery that would have significantly interfered with nasal air flow; had hypersensitivity to Oxymetazoline, Fluticasone, and/or any other drug of same class. The other key exclusion criteria were patients with an active pulmonary disorder including asthma, upper respiratory tract or sinus infection that required antibiotic therapy within 14 days of the screening visit or an upper respiratory infection/ocular infection within 7 days of the screening visit; patients with history of narrow-angle glaucoma, increased intraocular pressure, and posterior subcapsular cataract; patients with abnormal laboratory values, ie, RBS >140 mg/dL, serum transaminases ≥3x Upper Normal Limit, serum bilirubin ≥2.0 mg/dL, and serum creatinine ≥2.5 mg/dL; patients with clinically significant uncontrolled systemic diseases such as gastrointestinal, cardiovascular, renal, neurological, psychiatric, endocrine, immunological, or hematological disorders or malignancy; pregnant or lactating females and females of child bearing age not willing to use double methods of contraception during the study period; patients who have received the following medications in the given time frame: nasal or oral decongestants, nasal or oral antihistamines: 72 hours; nasal or inhaled corticosteroids, leukotriene receptor antagonists, 5-lipoxygenase inhibitors, methylxanthines, non-prescription drugs: 7 days; MAO inhibitors: 14 days; oral corticosteroids: 12 weeks.
Patients were permitted to use any medication for the treatment of concomitant diseases or adverse events during the study period that were not known to interact with the study medication. However, a record of the same was maintained in the Case Record Form. Patients were not allowed to use the following medications during the study period: any other anti-allergic medication (systemic/topical), any other nasal spray preparation; any other medication for the treatment of allergic rhinitis; ocular preparations like artificial tears /eye wash, etc.; Monoamine Oxidase Inhibitors (MAOI), tri-cyclic and tetra-cyclic antidepressants and CYP3A inhibitors.
Study Procedures and Drugs
Patients satisfying the eligibility criteria were randomized in a 1:1 ratio, as per the centralized computer-generated randomization schedule to receive either the Test (Fluticasone Furoate and Oxymetazoline Hydrochloride Nasal Spray 27.5/50 mcg manufactured by M/s Cadila Healthcare Limited, India [FDC group]) or Reference (Fluticasone Furoate Nasal Spray 27.5 mcg manufactured and marketed by M/s Cadila Healthcare Limited, India [Fluticasone group]) drugs, in a double blind fashion. Both the study drugs, ie, Fluticasone Furoate and Oxymetazoline Hydrochloride Nasal Spray 27.5/50 mcg and Fluticasone Furoate Nasal Spray 27.5 mcg, were supplied in identical bottles with a similar looking pump and actuator. Both the formulations were similar in color and appearance to maintain double blinding in the study.
After randomization, patients were followed up on an outpatient basis with scheduled visits at Day 7, Day 14, Day 28, and Day 30 (visit 6). Patients were instructed to take two sprays of the study drug (nasal spray) in each nostril once daily every day at night before sleeping for 28 days, starting from the day of randomization. After 4 weeks of active treatment (day 28), the study drugs were withdrawn and all the patients were followed up again 2 days after the discontinuation of treatment to evaluate the incidence of rebound congestion/rhinitis medicamentosa or aggravation of other symptoms.
Efficacy and Safety Assessments
The efficacy of the study drugs was evaluated by using the Total Symptom Score (TSS). This is a validated scale comprising of four nasal (Congestion, Sneezing, Itching, and Rhinorrhoea) and three ocular (Itching/Burning, Tearing/Watering, and Redness) symptoms used for assessing the treatment outcomes in patients with allergic rhinitis. Each of the seven symptoms were rated on a 4-point scale ranging from 0–3, defined as 0 = none/no symptoms; 1 = mild symptoms, but not affecting any activities during the day/sleep at night; 2 = moderate symptoms affecting at least one activity or disturbing sleep; and 3 = severe symptoms affecting >2 daily activities or disturbing sleep all night or most of the night. The TSS (TSS) ranges from 0–21. Total Nasal Symptom Score (TNSS) has been calculated by adding the scores of the four nasal symptoms (range = 0−12) while the Total Ocular Symptom Score (TOSS) has been calculated by adding the scores of the three ocular symptoms (range = 0–9). The symptom scoring was done in the diary card twice daily (once in the morning assessing the night time symptoms and once in the evening assessing the day time symptoms) by the patients everyday starting from the day of screening to record baseline scores till the end of the study period, ie, post-treatment follow-up, to record rebound score after stopping the treatment.
The safety of the study medication was assessed by recording the adverse events occurring during the course of the study. Routine hematological and biochemical laboratory investigations were done at screening and at the end of treatment. All abnormalities found in the physical examination (including vitals) and laboratory investigations were dealt with as adverse events. A urine pregnancy test was done for females of child bearing potential at screening and at the end of treatment.
Statistical Analysis
The primary end point of the study was the reduction in TNSS (night time) in the two groups at end of 3 days, 7 days, 14 days, and 28 days. The secondary efficacy endpoints were reduction in TNSS (day time) in the two groups; reduction in nasal congestion (individual symptom score) in the two groups; proportion of patients achieving complete relief of nasal congestion (both day time and night time scores to be 0), and reduction in TSS and TOSS in the two groups. All the end points were evaluated at end of 3 days, 7 days, 14 days, and 28 days of study.
The sample size of the study was based on the primary efficacy endpoint (reduction in TNSS (night time)). A total of 224 patients (Test: 112, Reference: 112) were required to achieve 90% power with a 5.0% two-sided level of significance, considering mean reduction in night time TNSS of 8.0 in the test group and 7.0 in the control group, assuming a common standard deviation of 2.3.4 Considering atreatment allocation ratio of 1:1 and drop-out rate of 10%, a total of 250 patients were enrolled in the study.
For primary and secondary efficacy analysis, the reductions in various scores in the two groups at the end of 3 days, 7 days, 14 days, and 28 days were calculated and compared using an un-paired t-test for each time point separately. Chi-square/Fisher's Exact test was used for categorical variables. P-values less than 0.05 were considered as significant. Data of all the randomized patients, including patients with protocol deviations, who had completed at least one (01) post-randomization visit with efficacy variable assessment have been considered for Intention to Treat analysis in the study. Last Observation Carried Forward (LOCF) method has been used to impute the missing data in patients who were lost to follow-up or drop outs.
Results
Two hundred and fifty patients of allergic rhinitis with nasal congestion were enrolled in this randomized, double-blind, active-controlled, multicentre phase III clinical trial. One hundred and twenty-three patients were assigned to the FDC group (received the Fixed dose combination of Fluticasone Furoate and Oxymetazoline Hydrochloride Nasal Spray 27.5/50 mcg) and 127 patients were assigned to the Fluticasone group (received the Fluticasone Furoate Nasal Spray 27.5 mcg). The flow of patients in the study is shown in Figure 1. All the enrolled patients were considered for intention to treat efficacy and safety analysis. The demographic profile and baseline characteristics of patients enrolled in the study are given in Table 1. All the patients enrolled in the study had a prior history of allergic rhinitis and had an exacerbation of symptoms with moderate-to-severe nasal congestion. The mean TNSS, TOSS, and TSS scores were similar at baseline in the two groups.
 |
Table 1 Demographic and Baseline Characteristics of All Enrolled Patients |
 |
Figure 1 Flow of patients in the study. |
Efficacy
Total Nasal Symptom Score (TNSS)
The primary efficacy variable of the study was reduction in TNSS (night time) in the two groups at the end of 3 days, 7 days, 14 days, and 28 days. The night time TNSS started decreasing in both the groups as early as 3 days after the start of treatment. The reduction in night time TNSS score was significantly greater in the FDC group as compared to that in the Fluticasone group at all the time points in the study, starting from as early as day 3 itself. The significantly greater effect of the Fixed Dose Combination was sustained even till the end of the treatment period, ie, day 28. A similar statistically superior reduction in day time TNSS scores was also noted in patients in the FDC group as compared to that in the Fluticasone group at the end of 3 days, 7 days, and 14 days. There was a greater reduction in day time TNSS at day 28 in the FDC group, but it did not reach statistical significance levels. The results of night time and day time TNSS are shown in Figure 2.
 |
Figure 2 Reduction in night time and day time TNSS in the two groups at end of 3 days, 7 days, 14 days, and 28 days. (A) night time TNSS Score; (B) day time TNSS Score. |
Nasal Congestion
All the patients reported an improvement in nasal congestion after the start of treatment, however the reduction in nasal congestion score was significantly more in the patients treated with the FDC of Fluticasone and Oxymetazoline as compared to those being treated with Fluticasone alone (P<0.05 at all time-points for both night time and day time nasal congestion score). The reduction in night time and day time nasal congestion scores in the two groups is shown in Figure 3. The proportion of patients with complete relief of nasal congestion throughout the day (both day time and night time) was also significantly greater in the FDC group as compared to that in the Fluticasone group (Day 3: 9.8% vs 1.6%; Day 7: 20.3% vs 4.7%; Day 14: 29.3% vs 7.9%; Day 28: 44.7% vs 26.8%; P<0.05 at all the time-points).
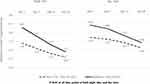 |
Figure 3 Reduction in night time and day time Nasal Congestion Score in the two groups at end of 3 days, 7 days, 14 days, and 28 days. |
Total Symptom Score (TSS) and Total Ocular Symptom Score (TOSS)
The reduction in night time TSS in the two groups, ie, FDC group vs Fluticasone group at various time points were as follows: Day 3: −4.4±2.7 vs −3.4±2.7; Day 7: −5.8±2.7 vs −5.1±2.6; Day 14: −8.2±2.9 vs −7.3±3.0; Day 28: −10.0±2.6 vs −9.2±3.1. This reduction in night time TSS was statistically superior in the FDC group as compared to that in the Fluticasone group throughout the study period. The reduction in day time TSS in the two groups were as follows:- Day 3: −3.9±2.7 vs −2.7±2.4; Day 7: −4.9±3.0 vs −4.4±2.6; Day 14: −6.9±3.7 vs −6.0±3.3; Day 28: −8.5±4.0 vs −8.5±4.0. There was no difference in the reduction of night time or day time ocular score in the two groups.
Safety
Both the study drugs were well tolerated by all the patients in the study. A total of six adverse events were reported in six patients in the FDC group (adverse event rate 5.9%) and 11 adverse events were reported in 10 patients in the Fluticasone group (adverse event rate 7.9%) during the 28 days treatment period. All the adverse events reported in the study were “mild” in severity. No severe or serious adverse event was reported by any of the patients enrolled in the study. All the reported adverse events resolved completely with/without symptomatic treatment during the study period. None of the adverse events required any change in the dosing or discontinuation of the study medication during the entire course of the study. The most common adverse event reported during the study was local application site discomfort/irritation in both the Fluti-oxy group (3.3%) and the Fluticasone group (3.9%). The most common systemic event reported was Headache in both the groups with an incidence of 3.2% in the FDC group and 0.8% in the Fluticasone group. The other adverse events reported included dryness in the nose (one patient in the FDC group) and redness in the nose and fever (one patient each in the Fluticasone group). There was no difference in the adverse event profile of the FDC group as compared to the Fluticasone group at the end of the study (P>0.05). On overall assessment of tolerability, 95.1% patients in the FDC group and 92.1% in the Fluticasone group were rated to have an “Excellent” tolerability to the study medication.
Rebound Congestion
All the subjects were followed up 2 days after stopping the treatment to evaluate for any worsening of symptoms or development of rebound congestion. The subjects were also asked to enter the daily symptoms in the diary card even after stopping the treatment. The proportion of patients showing worsening of symptoms after stoppage of medication was similar in the two groups (P>0.05). In total, 11.4% of patients in the FDC group and 16.5% of patients in the Fluticasone group reported an increase in nasal congestion score (P=0.47), while 25.2% of patients in the FDC group and 28.4% of patients in the Fluticasone group had an increase in the TNSS 2 days after stopping the treatment (P=0.27). Also, 13.2% (7 out of 53) patients who had complete relief of nasal congestion at day 28 in the FDC group reported some nasal congestion after stopping the drug, while this number was 26.5% (9 out of 34) in the Fluticasone group (P=0.16).
Discussion
This study presents the efficacy and safety of a novel fixed dose combination of Fluticasone Furoate and Oxymetazoline Hydrochloride Nasal Spray 27.5/50 mcg developed by M/s Cadila Healthcare Limited (India) compared to Fluticasone Furoate Nasal Spray 27.5 mcg in a randomized, double blind, prospective, multicenter Phase III study conducted in patients of allergic rhinitis with moderate-to-severe nasal congestion. The study demonstrated statistical superiority of the fixed dose combination of Fluticasone Furoate and Oxymetazoline Hydrochloride Nasal Spray 27.5/50 mcg when used in a dose of two nasal sprays administered in each nostril once daily at night in relieving the nasal symptoms of allergic rhinitis as early as 3 days after initiation of treatment and sustenance of the superior effect on nasal congestion and night time TNSS till the end of the treatment period without leading to development of rebound congestion or rhinitis medicamentosa after withdrawal of the treatment.
The results of our Phase III study support the previous publications establishing the pharmacokinetic and pharmacodynamic compatibility of simultaneous use of a steroid and a nasal decongestant in patients with allergic rhinitis. Fluticasone nasal spray is recommended to be used in a dose of two sprays to be administered in each nostril once every day;12 however, the recommended dosing regimen of Oxymetazoline Hydrochloride Nasal Spray 0.05%w/w ranges from one spray in each nostril once daily to up to two sprays in each nostril every 6 hours. As Oxymetazoline provide symptomatic treatment only, it has been shown to be effective even in a single dose and repeat doses are used as and when needed only.13 Various publications have shown that Oxymetazoline is effective in controlling nasal congestion throughout the day even when used in a once daily dosing regimen at night along with steroids.6,14,15 Moreover these studies have also demonstrated that, when used in a once daily dosing regimen, Oxymetazoline is safer and can be used for a longer period of time without any AEs and chances of rhinitis medicamentosa.
Based on the once daily recommended dose of Fluticasone nasal spray and the various studies showing round the clock effectiveness of Oxymetazoline when used in a once daily evening dosing regimen with steroids, we had used the fixed dose combination of Fluticasone Furoate and Oxymetazoline Hydrochloride Nasal Spray 27.5/50 mcg in a once daily evening dosing regimen only. The results from our study also support the hypothesis that when given along with intra-nasal steroid, the duration of action of Oxymetazoline increases and it shows good efficacy even in a once daily dosing regimen. We have shown in our study that even when the fixed dose combination is given as a single night time dose only, there is significantly more reduction in day time nasal congestion and TNSS as compared to fluticasone alone. Also there are a significantly greater number of patients having complete relief in Nasal Congestion (no nasal congestion throughout the day) in the FDC group as compared to the Fluticasone group, indicating that the duration of action of Oxymetazoline is prolonged and the effect remains throughout the day when given along with a steroid.
Besides the pharmacokinetic compatibility, the simultaneous use of steroid and nasal decongestants have shown synergistic pharmacodynamics effects. Addition of Oxymetazoline to steroid leads to improved efficacy of steroids6,15 and also ensures faster onset of action of the steroid.14,15 This is possibly due to a reduction of edema of nasal mucosa by the alpha adrenergic agonist action of Oxymetazoline, thereby facilitating the access of topical steroids.16 This is also supported by the data in our phase III study. The patients in the FDC group showed a significant rapid reduction of TNSS as early as 3 days after the start of treatment, and the superior effect of FDC as compared to fluticasone alone continued till the end of the study, thereby establishing the synergetic effect of adding Oxymetazoline to the steroid.
While on the one hand, addition of Oxymetazoline enhances the efficacy of steroids, addition of steroids to Oxymetazoline enhances the long-term safety and tolerability of Oxymetazoline. As per convention, Oxymetazoline is not recommended to be used for more than 4–5 days continuously for the fear of developing rhinitis medicamentosa. However, various publications6,14–17 and the results of our Phase III study have shown that using steroid along with Oxymetazoline ameliorates the chances of developing rebound congestion and rhinitis medicamentosa even with long-term continuous use of the nasal decongestant. As seen in our study, the FDC was effective in reducing the nasal congestion throughout the study period without development of tachyphylaxis/loss of effect. Moreover, the proportion of patients showing worsening of symptoms after stoppage of medication was similar in the two groups (P>0.05), indicating that there was no rebound congestion and rhinitis medicamentosa in the patients in the FDC group even after stopping the treatment. Previous studies have demonstrated that frequent (3–4 times a day) long-term use of Oxymetazoline leads to rapid internalization and uncoupling of α-receptors in the nasal mucosa thereby leading to dilatation of deep venous sinusoids (rebound congestion) in resting phase and loss of efficacy of Oxymetazoline (tachyphylaxis). Addition of a steroid to Oxymetazoline prevents development of rhinitis medicamentosa (rebound congestion and tachyphylaxis) by two postulated mechanisms: directly by acting through glucocorticoid response elements thereby restoring the G-protein–adrenoceptor coupling, increasing the cell surface receptor numbers, and reversing the adrenoceptor down-regulation; and indirectly by increasing the duration of action of Oxymetazoline thereby requiring once daily dosing only.16,17
The results of our study are also comparable to the results of the only other published, double-blind, double-dummy, randomized, placebo-controlled parallel study evaluating the treatment with Fluticasone Furoate/Oxymetazoline hydrochloride administered concomitantly but not as FDC in the treatment of perennial allergic rhinitis. The study showed that there was an overall significant difference among treatments (P=0.04) with concomitant Fluticasone and Oxymetazoline resulting in lower total nasal symptoms than did placebo (P=0.014) or Fluticasone alone (P=0.02). These data also suggested that the addition of Oxymetazoline to Fluticasone Furoate results in faster onset of symptom relief than does Fluticasone Furoate alone and Oxymetazoline adds to the overall effectiveness of Fluticasone Furoate in the treatment of perennial allergic rhinitis. Also, there was no incidence of development of rhinitis medicamentosa even with long-term use of Oxymetazoline.6
One of the limitations of the study was the use of only subjective parameters for evaluation of the efficacy of the study drugs. However as this was a double blind study with both the study drugs having exactly the same appearance, there would not have been any bias in efficacy evaluation. We recommend to conduct further studies with objective parameters to evaluate the efficacy and safety of the fixed dose combination of Fluticasone and Oxymetazoline in long-term use.
Conclusion
The results of our above prospective, randomized, double-blind, two-arm, active controlled, parallel, multicenter phase III clinical trial demonstrate that the fixed dose combination of Fluticasone Furoate and Oxymetazoline Hydrochloride Nasal Spray 27.5/50 mcg is superior to Fluticasone Furoate Aqueous Nasal Spray 27.5 mcg given alone as once daily evening dose in relieving the Nasal Congestion and reduction of Total Nasal Symptom Score in patients suffering from Allergic Rhinitis with moderate-to-severe nasal congestion. The superior beneficial effect of the FDC starts as early as 3 days after initiation of therapy and continues till the end of the treatment. The safety profile of Fluticasone Furoate and Oxymetazoline Hydrochloride Nasal Spray 27.5/50 mcg is similar to Fluticasone Furoate Nasal Spray 27.5 mcg. Oxymetazoline when used along with the nasal steroid in a once daily dose does not cause rebound congestion and rhinitis medicamentosa even after long-term continuous use of 28 days.
Clinical Implications
Fixed dose combination of Oxymetazoline with Fluticasone as nasal spray is superior to Fluticasone Nasal Spray for management of allergic rhinitis with nasal congestion. The FDC is safe and does not cause rebound congestion and rhinitis medicamentosa even after long-term continuous use of 28 days when used in once daily dosing regimen.
Data Sharing Statement
The whole deidentified data and other study documents will be made available by the corresponding author upon reasonable request up to 5 years after the end of the study.
Funding
The study was sponsored by Cadila Healthcare Limited, India.
Disclosure
Authors JS and RM are full time employees of Cadila Healthcare Limited and authors RSK, MKJ, JSK, SP, VP, and SG received honorarium for conduct of the study. RSK, MKJ, JSK, and VP report personal fees from Cadila Healthcare Limited, during the conduct of the study. The authors report no other potential conflicts of interest in relation to this work.
References
1. Dykewicz MS, Fineman S. Executive summary of joint task force practice parameters on diagnosis and management of rhinitis. Ann Allergy Asthma Immunol. 1998;81:463–468. doi:10.1016/S1081-1206(10)63152-3
2. Gaur SN, Gupta K, Rajpal S, Singh AB, Rohtagi A. Prevalence of bronchial asthma and allergic rhinitis among urban and rural adult population of Delhi. Indian J Allergy Asthma Immunol. 2006;20:90–97.
3. Shah A, Pawankar R. Allergic rhinitis and co-morbid asthma: perspective from India - ARIA Asia- Pacific Workshop report. Asian Pac J Allergy Immunol. 2009;27:71–77.
4. Kubavat AH, Pawar P, Mittal R, et al. An open label, active controlled, multicentric clinical trial to assess the efficacy and safety of fluticasone furoate nasal spray in adult Indian patients suffering from allergic rhinitis. J Assoc Physicians India. 2011;59:424–428.
5. Brozek JL, Bousquet J, Baena-Cagnani CE, et al. Global allergy and asthma European network; grading of recommendations assessment, development and evaluation working group. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010;126(3):466–476. doi:10.1016/j.jaci.2010.06.047
6. Baroody FM, Brown D, Gavanescu L, DeTineo M, Naclerio RM. Oxymetazoline adds to the effectiveness of fluticasone furoate in the treatment of perennial allergic rhinitis. J Allergy Clin Immunol. 2011;127(4):927–934. doi:10.1016/j.jaci.2011.01.037
7. Stewart M, Ferguson B, Fromer L. Epidemiology and burden of nasal congestion. Int J Gen Med. 2010;8(3):37–45. doi:10.2147/IJGM.S8077
8. Scadding GK, Kariyawasam HH, Scadding G, et al. BSACI guideline for the diagnosis and management of allergic and non-allergic rhinitis.. Clin Exp Allergy. 2017;47(7):856–889. doi:10.1111/cea.12953
9. Matreja PS, Gupta V, Kaur J, Singh S. Efficacy of fluticasone and oxymetazoline as the treatment for allergic rhinitis [internet].2012. J Clin Diagn Res. 2019;6(1):85–88.
10. Ferguson BJ, Paramaesvaran S, Rubinstein E. A study of the effect of nasal steroid sprays in perennial allergic rhinitis patients with rhinitis medicamentosa. Otolaryngol Head Neck Surg. 2001;125(3):253–260. doi:10.1067/mhn.2001.117717
11. Inanh S, Öztürk Ö, Korkmaz M, Tutkun A. The effects of the topical agents of fluticasone propionate, oxymetazoline, and 3% and 0.9% sodium chloride solutions on mucociliary clearance in the therapy of acute bacterial rhinosinusitis in vivo. Laryngoscope. 2002;112:320–325. doi:10.1097/00005537-200202000-00022
12. Summary of Product Characteristics. Avamys. GlaxoSmithKline UK; 2018.
13. Product information leaflet. Otrivin Oxy. glaxosmithkline consumer private limited, India; 2019.
14. Liu W, Zhou L, Zeng Q, Luo R. Combination of mometasone furoate and oxymetazoline for the treatment of adenoid hypertrophy concomitant with allergic rhinitis: a randomized controlled trial. Sci Rep. 2017;7:40425. doi:10.1038/srep40425
15. Meltzer EO, Bernstein DI, Prenner BM, Berger WE, Shekar T, Teper AA. Mometasone furoate nasal spray plus oxymetazoline nasal spray: short-term efficacy and safety in seasonal allergic rhinitis. Am J Rhinol Allergy. 2013;27(2):102–108. PMID: 23562197. doi:10.2500/ajra.2013.27.3864
16. Thongngarm T, Assanasen P, Pradubpongsa P, Tantilipikorn P. The effectiveness of oxymetazoline plus intranasal steroid in the treatment of chronic rhinitis: a randomised controlled trial. Asian Pac J Allergy Immunol. 2016;34(1):30–37. PMID: 26994623. doi:10.12932/AP0649.34.1.2016
17. Vaidyanathan S, Williamson P, Clearie K, Khan F, Lipworth B. Fluticasone reverses oxymetazoline-induced tachyphylaxis of response and rebound congestion. Am J Respir Crit Care Med. 2010;182(1):19–24. PMID: 20203244. doi:10.1164/rccm.200911-1701OC
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
