Back to Journals » Risk Management and Healthcare Policy » Volume 15
Efficacy and Safety of Flexible Laryngeal Mask Ventilation in Otologic Surgery: A Retrospective Analysis
Authors Liu F, Xi C, Cui X, Wang G
Received 15 January 2022
Accepted for publication 26 April 2022
Published 9 May 2022 Volume 2022:15 Pages 945—954
DOI https://doi.org/10.2147/RMHP.S354891
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Mecit Can Emre Simsekler
Feihong Liu, Chunhua Xi, Xu Cui, Guyan Wang
Department of Anesthesiology, Beijing Tongren Hospital, Capital Medical University, Beijing, People’s Republic of China
Correspondence: Guyan Wang, Department of Anesthesiology, Beijing Tongren Hospital, Capital Medical University, Beijing, People’s Republic of China, Tel +86-13910985139, Email [email protected]
Background: Flexible laryngeal mask airways (FLMAs) ventilation have been widely used as airway devices during general anesthesia, especially in otologic surgery. However, the current literature reports that the clinical success and failure rates for FLMA usage are quite different, and there remains a paucity of data regarding factors associated with FLMA failure and complications related to FLMA usage.
Purpose: To evaluate the success and failure rates of FLMA usage in otologic surgery, the factors associated with FLMA failure and complications related to FLMA usage.
Patients and Methods: All patients who underwent otologic surgery, including middle ear and mastoid procedures, under general anesthesia at a large tertiary general hospital from 2015 to 2019 were reviewed. The primary outcome was the FLMA failure rate, defined as any airway event requiring device removal and tracheal intubation, including primary and secondary failure. The secondary outcomes were specific clinical factors, including patient sex, age, weight, American Society of Anesthesiologists (ASA) classification, body mass index (BMI) and duration of surgery, which were analyzed as related risk factors.
Results: Among 5557 patients with planned FLMA use, the final success rate was 98.5%. Sixty-seven percent of the failures occurred during initial introduction of the FLMA, 8% occurred after head and neck rotation, and 25% occurred during the procedures. Two independent clinical factors associated with FLMA failure were male sex and age. Respiratory complications were observed in 0.61% of patients, and the rate of severe nerve and tissue damage associated with FLMA use was 0.05.
Conclusion: This study demonstrates a high success rate of 98.5% for FLMA use in adults undergoing otologic surgery with rare adverse airway events and injuries complications. Two independent risk factors require attention and thorough and accurate management is necessary for every clinician.
Keywords: otologic surgery, flexible laryngeal mask airway, safety, efficacy, airway complications
Introduction
The laryngeal mask airway (LMA) was invented in 1981 by Dr Brain.1 Because of its advantages,1 FLMAs are increasingly used as a substitute for endotracheal tubes in a variety of surgical situations requiring general anesthesia. With the appearance of various new LMAs that address the limitations of the classic model, not only has their use in selective operations increased, but the indications for FLMA have also grown.2 FLMAs can be inserted into the hypopharynx easily without laryngoscopy and neuromuscular blocking agents, and they can also be removed from the patient’s mouth quickly.3 Decreasing airway irritation during surgery results in fewer hemodynamic changes and airway accidents from anesthesia and enables wakeup with less coughing and bucking, which could result in less ossicular replacement prosthesis displacement.4–6 In middle ear/mastoid procedures (MEMs), because the operation involves the temporal bone, including the surrounding normal nerves and blood vessels, improper manipulation can lead to complications such as facial paralysis; therefore, the operation needs to be performed carefully. Compared to endotracheal intubation, FLMAs have little effect on middle ear pressure.7,8 These advantages make anesthesiologists prefer FLMAs during otologic surgery. In addition, since FLMAs can reduce the response to upper airway stimulation, they can be used as an airway device during surgery requiring facial nerve monitoring without the use of muscle relaxants.9
However, the points of contention and primary disadvantages of the use of FLMA are the reduced levels of airway protection, the increased risk of gastric insufflation, the difficulty of insertion, partial upper airway obstruction and the possibility of dislocation during the procedure.10,11 To expose the operative field, otologists usually require the patient’s head be rotated 60°~90° to the healthy side. Some studies have reported that the head and neck position can affect the sealing and ventilation functions of FLMAs and the fiberoptic view.8,12,13 John et al reported that the incidence of regurgitation, which could increase the risk of aspiration with FLMA use, varies from 0% to 23% compared with endotracheal tube (ETT). However, the incidence of regurgitation in the LMA group (20%) was not significantly different from that in the ETT group (18%), as reported by a systematic review. Brodrick et al reported that approximately 10% of the participants in the FLMA group had partial airway obstructions, and the possible cause was the downfolding of the epiglottis. Other complications reported with the use of FLMAs include cranial nerve injury, arytenoid dislocation, mucosal trauma, postoperative sore throat, hoarseness, and respiratory accidents.14,15
Patterns of use in different geographic regions and the reported incidence of failure and complications vary widely. In the adult population, a recent observational study revealed a 1.1% incidence of laryngeal mask failure, with 62% of patients having significant airway complications.14 In this study, we analyzed the independent risk factors for LMA failure, including male sex, poor dentition, increased body mass index (BMI), and operation table rotation. However, very few large sample studies have provided definitive data about FLMA failure and airway complications that occur during otologic surgery.
This study aimed to evaluate the failure and success rates of FLMA usage in otologic surgery, the factors associated with FLMA failure and complications related to FLMA usage in a large number of patients who underwent otologic surgery during the period of 2015–2019.
Patients and Methods
Ethical approval for this study (TRECKY2016-020) was provided by the Ethical Committee of Beijing Tongren Hospital, Capital Medical University, Beijing, China. The requirement for written informed consent was waived since this is a retrospective study. The study conformed with the Declaration of Helsinki. We included all adult otitis media patients who underwent MEMs under general anesthesia and positive pressure ventilation from April 1, 2015, to December 31, 2019. Patient information was extracted from an electronic information system (AIMS, Beijing Yifei Huatong Technology Development Company, Beijing, China), which was available on April 1, 2015. The exclusion criteria were patients undergoing emergency surgery, children and adolescents (age under 18), patients undergoing simultaneous laryngeal and neurosurgical procedures requiring tracheal intubation, and patients with other non-MEMs, such as preauricular fistulas.
General anesthesia for otologic surgery is standardized, regardless of special circumstances, in our department. Anesthesia was induced with intravenous (I.V.) propofol/etomidate, analgesics (opioids), sedatives (midazolam) and nondepolarizing neuromuscular blockers. Standard FLMA (Medis, Medical Ltd., Tianjin, China) insertion/endotracheal intubation was performed by skilled anesthetists with more than 3 years of experience in all cases. The laryngeal mask model was selected according to weight-based size recommendations (size 3 for 35–50 kg, size 4 for 50–70 kg and size 5 for 70–100 kg). Oxybuprocaine gel was applied at the tip and back of the cuff, and the operator placed his index finger between the laryngeal capsule and the breathing tube and placed it along the posterior wall of the oropharynx until there was significant pharyngeal resistance. The FLMA cuff pressure reached 60 mmHg (1 mmHg=0.133 kPa). After endotracheal intubation or FLMA placement, an oxygen supply was achieved by intermittent positive pressure and ventilation (IPPV) with a vital volume of 6–8 mL/kg, and the respiratory rate was controlled to maintain the end-tidal carbon dioxide partial pressure (EtCO2) at 35–40 mmHg. Anesthesia was maintained by inhalation agents and incremental doses of opioids, total intravenous anesthesia (TIVA), or a combination of the two methods. Neuromuscular blockers were added according to the duration of the operation.
Methods of assessing the FLMA position during manually controlled ventilation were as follows: First, auscultation was performed to detect whether there were murmurs in the neck and chest and to observe the peak pressure of the airway. If there were no murmurs and the peak pressure < 20 cmH2O (1 cmH2O=0.0098 kPa), the oropharyngeal leak pressure (OLP) continued to be observed; otherwise, the FLMA was reinserted. Second, the OLP was determined: the valve of the anesthesia machine was closed, fresh gas was applied at 5 L/min, and the increase in airway pressure was observed via a pressure-time curve. The OLP is when the peak pressure is no longer rising or there is gas leakage. To ensure the safe use of FLMAs in our clinical practice, FLMA failure was defined as ineffective ventilation or a difference between the OLP and peak inspiratory pressure (PIP) of less than 5 cmH2O. Three failures occurred, and endotracheal intubation was immediately applied.
FLMA failure was defined as incorrect FLMA positioning and tracheal intubation, either on induction (primary failure) or after turning the patient’s head and neck 60°~90° to the healthy side (secondary failure).
The patient’s sex, age, weight, American Society of Anesthesiologists (ASA) classification, BMI, duration of surgery, airway management and adverse events associated with the use of FLMA were recorded. Primary failure and secondary failure were manually reviewed, as were all common indicators of failure of FLMA placement (eg, air leakage, inadequate ventilation, airway obstruction). Adverse incidents, such as laryngospasm, desaturation (SPO2<90% over 60s), postoperative pulmonary edema, hoarseness, sore throat and nerve and tissue damage, were collected from the AIMS.
Statistical Analysis
Statistical analyses were carried out with IBM SPSS 24 software (SPSS Inc., Chicago, IL, USA). Qualitative data are presented as numbers and percentages. Demographic data were evaluated for normality with the Kolmogorov–Smirnov test. Patients with and without FLMAs were compared according to demographic and clinical characteristics with the chi-square test for categorical variables and with t-tests (normally distributed) or Mann–Whitney U-tests (nonnormally distributed) for continuous variables. Univariate logistic regressions were performed to identify potentially significant factors. Variables considered to be significant with a P-value less than 0.05 in the univariate analysis were entered into the multiple logistic regression analysis. For the purposes of multivariate analysis, patients were classified according to BMI into underweight (<18.5 kg/m2), normal (18.5–22. 9 kg/m2), overweight (23–27.4 kg/m2) and obese (≥27.5 kg/m2) groups according to the WHO recommendations for Chinese people; according to age in 10-year epochs; and according to ASA classification as either low-grade ASA (ASA I) or high-grade ASA (ASA II and ASA III). Because BMI can be considered representative of weight, we excluded weight from the regression model. The adjusted odds ratio (OR) with 95% confidence interval (95% CI) was used to describe the effect of each independent variable on the risk of FLMA failure.
Sample size estimation was performed to define the power of the data analysis as previously described. Based on an expected FLMA failure rate of 1.5%, a sample size of 5557 would allow the evaluation of at least 7 covariates (six were included in our study).
Results
A total of 5583 FLMA patients were identified, and 5582 patients were finally included in the analysis. One was excluded as the surgery was cancelled because of a severe arrhythmia attack before induction. A total of 5557 patients had planned FLMA use, and 26 were scheduled for ETT. Among the ETT patients, 5 needed emergency hemostasis surgery, 4 had cleft lip and/or palate, 3 required pharynx surgery and 1 required intracranial surgery simultaneously, 2 had combined severe pulmonary disease requiring possible postoperative ventilation support, 1 had nasopharyngeal cancer after radiotherapy, and 1 had yellow oral discharge after anesthesia induction for mask ventilation; no detailed reason was provided for the remaining 8. Total FLMA failure occurred in nearly 1.5% of FLMA patients. Primary failure occurred in 1% (57/5557) of patients, with murmurs in the neck and chest in 16/57 (28.1%) patients, airway obstruction in 21/57 (36.8%) patients and no detailed reasons in 20/57 (35.1%) patients. Secondary failure occurred in 28/5557 (0.5%) patients, after head and neck rotation in 7 (0.1%) patients and during surgery in 21 (0.5%) patients. Final FLMA success was achieved in 5472 (98.5%) (Figure 1) patients. In all failed FLMA cases, endotracheal intubation was successfully performed.
Patient demographic and clinical data, including sex, age, weight, ASA classification, BMI, and duration of surgery, are recorded in Table 1. In the univariate analysis, we found that male sex and age were highly correlated with FLMA failure. The two variables were included in the logistic regression analysis, and both were independent predictors of FLMA failure (male sex (OR 1.66, 95% CI 1.07–2.56) and age (OR 1.21, 95% CI 1.03–1.41) (Table 2).
 |
Table 1 Patient Demographics in Successful and Failed LMA |
 |
Table 2 Independent Risk Factors for FLMA Failure |
Related complications occurred in 5472 FLMA patients (Table 3), of which 953 (17.41%) had sore throat. Most patients had a visual analog scale (VAS) score of less than 3 and recovered the day after surgery. Other patients with nerve and tissue damage had hoarseness (1 patient, 0.01%), arytenoid dislocation (2 patients, 0.02%), and postpharyngeal bleeding (1 patient, 0.01%). All of these patients were well treated and recovered well after surgery. Of the FLMA patients, 34 (0.61%) had respiratory complications. Desaturation occurred before, during and after the surgery in 3 (0.05%), 4 (0.07%), and 7 (0.13%) patients, respectively. Laryngospasm occurred in 18 (0.33%), and in these patients, two suffered negative pressure pulmonary edema (NPPE). Both of these patients required immediate tracheal intubation and intensive care management. There was no regurgitation during the use of the FLMAs. Only one patient experienced regurgitation during induction and mask ventilation.
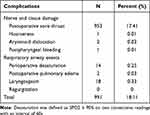 |
Table 3 Incidence of Complications Associated the Use of FLMA |
Discussion
In this retrospective study, we demonstrate that FLMAs can be effectively and safely used in patients undergoing otitis media surgery after prudent preoperative evaluation. Among 5557 patients with planned FLMA use, the final success rate was 98.5%, and the incidence of FLMA failure was 1.5%. The total FLMA failure rate is slightly higher than the LMA failure rates of 0.86–1.1% from large observational non-ENT studies16,17 and significantly lower than the 7.4% FLMA failure rate previously reported for ENT surgery.18 The relatively low failure rate in our study supports the safety of FLMA use for intraoperative airway management during otologic surgery. 67% of the failures occurred during initial introduction of the FLMA, 8% occurred after head and neck rotation, and 25% occurred during the procedures. Presenting features of primary FLMA failure included leakage (28.1%, with murmurs in the neck and chest) and upper airway obstruction (36.8%); detailed reasons for primary failure were not recorded for some patients (35.1%). Two independent clinical factors were associated with FLMA failure: male sex and age. Respiratory complications were observed in 0.61% of patients, and the rate of severe nerve and tissue damage associated with FLMA was 0.05.
The primary disadvantage and greatest concern with the use of LMAs is the inability to isolate the airway and protect against the risk of aspiration. The sealing mechanism of the laryngeal mask is affected by the following: the shape of the laryngeal mask cuff being consistent with the pharyngeal anatomy (ie, the position and size of the laryngeal mask) and whether the resultant force forming the end-to-end seal can maintain equilibrium (ie, the volume of air bag). Current studies on the effect of airway sealing mainly focus on the influence of the OLP. OLP mainly depends on the following factors: mucous membrane stress; oropharyngeal anatomy; scuff volume, pressure, throat mask size; head and neck position; anesthetic; demographic factor; pathological change; and airway technique. It is generally believed that effective positive pressure ventilation can be achieved when the OLP is greater than 20 cmH2O. The difference between the OLP and PIP should also be considered, and a higher differential pressure may be considered to reduce airway sealing. Based on years of clinical experience and related clinical research reports, we routinely ensure that the difference between the OLP and PIP is more than 5 cmH2O. In our study, no severe respiratory event was associated with FLMA failure related to airway protection. Usually, in our clinical practice, to avoid gastric insufflation, auscultation over the epigastrium was performed before OLP was achieved when the FLMA inserted,19 however, it is not continuously monitored, thus, asymptomatic gastric insufflation might be underestimated in our study. All these findings support that the conventional method of using FLMAs in ear surgery can basically meet the need for intraoperative airway sealing and maintain safe and effective ventilation in the volume-controlled ventilation mode. Because there are many factors affecting OLP, which may affect the value of the critical pressure difference, the optimal critical pressure difference still needs to be further studied in clinical trials with large sample sizes.
Otologic surgery involves turning the head to the healthy side. Changes in the position of the head and neck, such as flexion, extension and rotation, alter the geometric structure of the pharyngeal cavity, and might affect the sealing effectiveness of the laryngeal mask accordingly. When the head and neck are in the flexed position, the laryngeal mask is closely attached to the laryngopharynx due to compression of the pharyngeal cavity, and the OLP is increased.20 When the head and neck are in extension, the laryngeal mask and laryngopharynx are not close enough because of the enlargement of the pharyngeal cavity, and the OLP is decreased. In the study conducted by Keller and Brimacombe, patients were mechanically ventilated with a laryngeal mask and placed in four head and neck positions: median, anterior flexion, extension, and rotation. OLP was measured, and the anatomical position of the cuff was graded by fibrobronchoscopy. The results showed that the OLPs of the four head and neck positions were ranked as flexion >midline >extension, and there was no significant difference between the rotation position and midline position. The results of a study in our department showed that in the case of good ventilation in the midline position, turning the head laterally 60~90° can improve the placement of the FLMA in otologic surgery but has no significant effect on the ventilation of the laryngeal mask. In this study, there were only 7 cases where the laryngeal mask failed due to head and neck rotation. The exact reason for this is unknown, but one possible reason is that the FLMA may not have been in good alignment when the head was in the midline right position. Another reason may be that the change in head and neck position caused the FLMA to rotate in the oropharyngeal cavity, resulting in increased inspiratory pressure and decreased airtightness. This is also an area that we need to pay more attention to in the future. In clinical work, at the end of ear surgery, increased inspiratory pressure and poor ventilation may occur, which may be due to the reduced anteroposterior diameter of the pharyngeal cavity caused by head and neck flexion, the compression of perilaryngeal tissues against the mask body, resulting in partial airway obstruction, and even a shallower depth of insertion and displacement of the inserted mask.
We identified two independent clinical factors associated with FLMA failure: male sex and age. This finding is consistent with the increased incidence of increased upper airway resistance in men. Men had a higher prevalence of obstructive sleep apnea (OSA) syndrome than women (an estimated 10% vs 3%).21 This leads to a higher rate of upper airway narrowing and obstruction in men.22,23 Age was identified as an independent predictor of FLMA failure. A possible reason is that tooth loss in elderly individuals affects the structure of the oropharyngeal cavity, and the muscles and tissues in the oropharyngeal cavity become looser with age, resulting in a relatively narrow throat. These two independent factors are consistent with the results of previous studies. Despite previous studies showing that a high BMI is associated with laryngeal mask failure, however, such a conclusion could not be drawn in this study, possibly because the basic condition of ear patients in the study was relatively good, and there were relatively few obese patients, which was also reflected in the ASA classification.
With regard to secondary failure, in addition to the reasons for head and neck rotation, operation table rotation during surgery and the disappearance of muscle relaxation may lead to a change in the laryngeal mask position, resulting in increased PIP, air leakage or even ventilation failure. Once this happens, we first quickly change the ventilation mode to manual and check the entire respiratory line to rule out changes in the position of the laryngeal mask caused by impingement, twisting and stretching of the respiratory loop due to rotation of the operation table If not, muscle relaxations are added, and breathing parameters are adjusted to determine if mechanical ventilation can be achieved. If there is no improvement after the above treatment, we may request the deferment of surgery, adjustment or replacement of the laryngeal mask, or even change to endotracheal intubation.
In the 5557 FLMA patients, 34 (0.61%) had respiratory complications. Desaturation occurred before, during and after the surgery in 3 (0.05%), 4 (0.07%), and 7 (0.13%) patients, respectively. The causes included insufficient ventilation due to leakage of the laryngeal mask, obstruction of the upper airway due to poor alignment of the laryngeal mask, and laryngospasm or bronchospasm, which usually occurs during induction or recovery. Laryngospasm occurred in 18 (0.33%), and in these patients, two suffered NPPE. Both of these patients required immediate tracheal intubation and intensive care management, and the clinical manifestations and X-ray findings improved within 12 to 24 hours. Historically, the incidence of laryngospasm has been 0.78%-0.94%.24 With refinements in anesthesia and surgical techniques, the rate of laryngospasm has decreased to 0.48%-0.1%.25 In our study, the incidence of laryngeal spasms was also low, supporting this view. A meta-analysis showed that there were no statistically significant differences between the FLMA and ETT groups in laryngospasm following the removal of the airway in either the adult or pediatric subgroups during adenotonsillectomy.14 However, Seung H Yu reported that the incidence of laryngospasm during emergence was greater in the LMA group (1.7%) than in the ETT group (7.5%).26 The incidence of laryngospasm associated with FLMAs also remains controversial. The laryngeal mask can induce severe laryngospasm when the anesthesia is too light. Stimulation, such as surgery or sputum suction, causes a laryngeal reflex, which can cause laryngospasm. Controlling the depth of anesthesia and the use of muscle relaxants can reduce or prevent laryngospasm. In this study, two patients with planned FLMA use experienced serious laryngospasm and hypoxemia; with the application of succinylcholine, laryngospasm relieved, and the patients immediately underwent endotracheal intubation and mechanical ventilation for respiratory support. However, blood flowed from the endotracheal tube intraoperatively, and after pink foam was secreted, bronchial vascular rupture was determined to be the cause of the hemorrhaging; it was thought to be associated with severe laryngospasm caused by forced inspiration due to the negative pressure, leading to NPPE. In healthy adults undergoing general anesthesia, the incidence of NPPE is 0.05 to 0.1%. It is even less common with the use of LMAs.27 In this study, which collected cases for five years, the incidence of NPPE was 0.03%. The direct cause of NPPE is upper airway obstruction, which usually occurs immediately after tracheal catheter removal in patients under general anesthesia but can also occur several hours after extubation. The favorable outcome was likely due to early recognition and appropriate NPPE-specific therapy. Although the incidence of NPPE reported to be associated with LMA use in the current study was low, the increasing use of LMAs in the administration of anesthetics will provide more scenarios where NPPE can manifest. We encourage our colleagues to be vigilant in the recognition of NPPE when using LMAs and to be aware of the diagnosis and treatment of NPPE. In particular, the timing of removal should be carefully selected, and symptomatic treatment should be conducted in a timely manner once NPPE appears. There was no visible regurgitation during or after surgery. Only one patient experienced regurgitation during induction and mask ventilation, because of Insufficient time of fasting water. These findings again demonstrate the safety of laryngeal mask use. However, the guideline of laryngeal masks usage should be strictly regulated. For example, a laryngeal mask should not be used in patients with a full stomach.
For this study, we also assessed the complications related to nerve and tissue damage. The incidence of sore throat (17.4%) was consistent with that of the P P Higgins study (17.5%), lower than that of the endotracheal intubation group (45.4%) and higher than that of the mask ventilation group (3.3%).28 Most patients had a VAS score of less than 3 and recovered the day after surgery. Many factors including the intracuff pressure, the methods and times of laryngeal mask placement, the material of the laryngeal mask and whether the surface is coated with lubricant may also impact the incidence of sore throat.29,30 Increased awareness of these factors can help to avoid this complication and improve patient satisfaction. Other complications included hoarseness in 1 patient (0.01%), arytenoid dislocation in 2 patients (0.02%), and postpharyngeal bleeding in 1 patient (0.01%). All of these patients were well treated and recovered well after surgery. Generally, laryngeal mask placement does not require the use of a laryngoscope and does not involve entering the glottis. Correct laryngeal mask placement can reduce and avoid the stimulation of pharyngeal soft tissue, and postoperative complications such as sore throat, laryngeal edema, hoarseness, vocal cord injury, recurrent laryngeal nerve palsy and soft tissue injury are less likely to occur. However, forcibly or incorrectly repeated and overinflated placement can cause soft tissue swelling or even damage; pressure on nerves in the laryngeal wall can also cause hoarseness. Therefore, we must master correct use of laryngeal masks and be alert to the occurrence of related complications.
This study has several limitations. First, this study was a retrospective observational study with the inherent limitations of retrospective studies, such as the lack of control for random and undetermined confounding factors. However, our data provide meaningful insights into the safety of FLMA use in otitis media surgery because airway management during surgical anesthesia is fairly standardized at our institution and we reviewed our experience over many years; in addition, the clinical outcomes of this study rely on objective measurements. Second, our statistical results were mainly dependent on the clinical judgment of the anesthesiologist at the time. In the search strategy, cases in which the laryngeal mask involved subsequent endotracheal intubation and cases in which the unstable laryngeal mask was adequately addressed by other anesthesia interventions were not considered to represent failure of the laryngeal mask. Third, patients selected for this study included those who underwent middle ear surgery only and had an FLMA applied. The study did not include data on laryngeal mask type and did not analyze the relationship between mask failure rate and mask type. Fourth, our data are all derived from electronic records, whose accuracy and comprehensiveness affect the statistical results. Fifth, for the determination of the position of the laryngeal mask, we did not obtain fiberoptic and ultrasound scores. However, several studies have demonstrated that the laryngeal mask position can achieve ventilation in some cases, but there are relatively high fiberoptic bronchoscopy and ultrasound scores indicating suboptimal LMA positioning that may indicate an increased risk for further displacement during surgery, including head and neck transposition, recovery of muscle relaxation, or changes in operation table rotation. The literature reports that the frequency of suboptimal LMA positioning was 12.8% to 49% despite clinically successful ventilation.31,32 This condition increases the secondary failure rate. In the future, we can use fiberoptic bronchoscopy and ultrasound to locate the position of the laryngeal mask, assist in appropriate repositioning of the device and increase the success rate of the laryngeal mask. Finally, otorhinolaryngology is a key discipline in our hospital, both the surgeon and the anaesthesiologist are familiar with FLMA and each other’s surgical approaches. Differences in anaesthetic and surgical techniques should be considered when interpreting our results. Despite these limitations, our results provide evidence for the safety and effectiveness of laryngeal masks used by anesthesiologists during middle ear surgery.
Conclusion
In conclusion, this retrospective study demonstrates a high success rate of 98.5% for FLMA use in adults undergoing otologic surgery with rare adverse airway events and injuries complications. Two independent risk factors require attention. To avoid serious complications, thorough and accurate management can enable early detection33 and diagnosis of problems so that they can be actively addressed. In the future, with the help of fiberoptic bronchoscopy and ultrasound, laryngeal masks could be used more widely and safely.
Acknowledgments
I would like to thank Dr. Sun Yanxia who have helped me during the subject research. I shall extend my thanks to Dr. Lei Guiyu for her kindness and help. We thank the editors at American Journal Experts for their assistance in improving the English language herein.
Funding
Beijing Hospitals Authority Clinical Medicine Development of Special Funding Support, code: ZYLX202103.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Brain AI. The laryngeal mask–a new concept in airway management. Br J Anaesth. 1983;55(8):801–805. doi:10.1093/bja/55.8.801
2. White PF. Ambulatory anesthesia advances into the new millennium. Anesth Analg. 2000;90(5):1234–1235. doi:10.1097/00000539-200005000-00047
3. Jannu A, Shekar A, Balakrishna R, Sudarshan H, Veena GC, Bhuvaneshwari S. Advantages, disadvantages, indications, contraindications and surgical technique of laryngeal airway mask. Arch Craniofac Surg. 2017;18(4):223–229. doi:10.7181/acfs.2017.18.4.223
4. Duff BE. Use of the laryngeal mask airway in otologic surgery. Laryngoscope. 1999;109(7 Pt 1):1033–1036. doi:10.1097/00005537-199907000-00004
5. Ayala MA, Sanderson A, Marks R, Hoffer M, Balough B. Laryngeal mask airway use in otologic surgery. Otol Neurotol. 2009;30(5):599–601. doi:10.1097/MAO.0b013e3181ab8de2
6. van Esch BF, Stegeman I, Smit AL. Comparison of laryngeal mask airway vs tracheal intubation: a systematic review on airway complications. J Clin Anesth. 2017;36:142–150. doi:10.1016/j.jclinane.2016.10.004
7. Torun MT, Kuşderci HS, Öterkuş M. Do intubation devices affect middle ear pressure dynamics? J Craniofac Surg. 2019;30(4):1187–1190. doi:10.1097/SCS.0000000000005258
8. Watts P, Lim MK, Gandhewar R, et al. The effect of laryngeal mask airway insertion on intraocular pressure measurement in children receiving general anesthesia. Am J Ophthalmol. 2007;144(4):507–510. doi:10.1016/j.ajo.2007.06.010
9. Jarineshin H, Kashani S, Vatankhah M, Abdulahzade Baghaee A, Sattari S, Fekrat F. Better hemodynamic profile of laryngeal mask airway insertion compared to laryngoscopy and tracheal intubation. Iran Red Crescent Med J. 2015;17(8):e28615. doi:10.5812/ircmj.28615
10. Webster AC, Morley-Forster PK, Janzen V, et al. Anesthesia for intranasal surgery: a comparison between tracheal intubation and the flexible reinforced laryngeal mask airway. Anesth Analg. 1999;88(2):421–425. doi:10.1097/00000539-199902000-00037
11. Doksrød S, Løfgren B, Nordhammer A, Svendsen MV, Gisselsson L, Raeder J. Reinforced laryngeal mask airway compared with endotracheal tube for adenotonsillectomies. Eur J Anaesthesiol. 2010;27(11):941–946. doi:10.1097/EJA.0b013e32833d69c6
12. Somri M, Vaida S, Garcia Fornari G, et al. A randomized prospective controlled trial comparing the laryngeal tube suction disposable and the supreme laryngeal mask airway: the influence of head and neck position on oropharyngeal seal pressure. BMC Anesthesiol. 2016;16(1):87. doi:10.1186/s12871-016-0237-7
13. Okuda K, Inagawa G, Miwa T, Hiroki K. Influence of head and neck position on cuff position and oropharyngeal sealing pressure with the laryngeal mask airway in children. Br J Anaesth. 2001;86(1):122–124. doi:10.1093/bja/86.1.122
14. Xu R, Lian Y, Li WX, Wei H. Airway complications during and after general anesthesia: a comparison, systematic review and meta-analysis of using flexible laryngeal mask airways and endotracheal tubes. PLoS One. 2016;11(7):e0158137. doi:10.1371/journal.pone.0158137
15. Safaeian R, Hassani V, Movasaghi G, Alimian M, Faiz HR. Postoperative respiratory complications of laryngeal mask airway and tracheal tube in ear, nose and throat operations. Anesthesiol Pain Med. 2015;5(4):e25111. doi:10.5812/aapm.25111
16. Ramachandran SK, Mathis MR, Tremper KK, Shanks AM, Kheterpal S. Predictors and clinical outcomes from failed Laryngeal Mask Airway Unique™: a study of 15,795 patients. Anesthesiology. 2012;116(6):1217–1226. doi:10.1097/ALN.0b013e318255e6ab
17. Mathis MR, Haydar B, Taylor EL, et al. Failure of the Laryngeal Mask Airway Unique™ and Classic™ in the pediatric surgical patient: a study of clinical predictors and outcomes. Anesthesiology. 2013;119(6):1284–1295. doi:10.1097/ALN.0000000000000015
18. Nekhendzy V, Ramaiah VK, Collins J, Lemmens HJ, Most SP. The safety and efficacy of the use of the flexible laryngeal mask airway with positive pressure ventilation in elective ENT surgery: a 15-year retrospective single-center study. Minerva Anestesiol. 2017;83(9):947–955. doi:10.23736/S0375-9393.17.11403-3
19. Lee JS, Kim DH, Choi SH, Ha SH, Kim S, Kim MS. Prospective, randomized comparison of the i-gel and the self-pressurized air-Q intubating laryngeal airway in elderly anesthetized patients. Anesth Analg. 2020;130(2):480–487. doi:10.1213/ANE.0000000000003849
20. Kim HJ, Lee K, Bai S, Kim MH, Oh E, Yoo YC. Influence of head and neck position on ventilation using the air-Q® SP airway in anaesthetized paralysed patients: a prospective randomized crossover study. Br J Anaesth. 2017;118(3):452–457. doi:10.1093/bja/aew448
21. Fietze I, Laharnar N, Obst A, et al. Prevalence and association analysis of obstructive sleep apnea with gender and age differences - results of SHIP-Trend. J Sleep Res. 2019;28(5):e12770. doi:10.1111/jsr.12770
22. Mohsenin V. Gender differences in the expression of sleep-disordered breathing: role of upper airway dimensions. Chest. 2001;120(5):1442–1447. doi:10.1378/chest.120.5.1442
23. Mohsenin V. Effects of gender on upper airway collapsibility and severity of obstructive sleep apnea. Sleep Med. 2003;4(6):523–529. doi:10.1016/S1389-9457(03)00168-0
24. Runciman WB, Webb RK, Klepper ID, Lee R, Williamson JA, Barker L. The Australian Incident Monitoring Study. Crisis management–validation of an algorithm by analysis of 2000 incident reports. Anaesth Intensive Care. 1993;21(5):579–592. doi:10.1177/0310057X9302100515
25. Burgoyne LL, Anghelescu DL. Intervention steps for treating laryngospasm in pediatric patients. Paediatr Anaesth. 2008;18(4):297–302. doi:10.1111/j.1460-9592.2008.02445.x
26. Yu SH, Beirne OR. Laryngeal mask airways have a lower risk of airway complications compared with endotracheal intubation: a systematic review. J Oral Maxillofac Surg. 2010;68(10):2359–2376. doi:10.1016/j.joms.2010.04.017
27. Vandse R, Kothari DS, Tripathi RS, Lopez L, Stawicki SP, Papadimos TJ. Negative pressure pulmonary edema with laryngeal mask airway use: recognition, pathophysiology and treatment modalities. Int J Crit Illn Inj Sci. 2012;2(2):98–103. doi:10.4103/2229-5151.97275
28. Higgins PP, Chung F, Mezei G. Postoperative sore throat after ambulatory surgery. Br J Anaesth. 2002;88(4):582–584. doi:10.1093/bja/88.4.582
29. El-Boghdadly K, Bailey CR, Wiles MD. Postoperative sore throat: a systematic review. Anaesthesia. 2016;71(6):706–717. doi:10.1111/anae.13438
30. McHardy FE, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia. 1999;54(5):444–453. doi:10.1046/j.1365-2044.1999.00780.x
31. Von Ungern-sternberg BS, Wallace CJ, Sticks S, Erb TO, Chambers NA. Fibreoptic assessment of paediatric sized laryngeal mask airways. Anaesth Intensive Care. 2010;38(1):50–54. doi:10.1177/0310057X1003800110
32. Kim J, Kim JY, Kim WO, Kil HK. An ultrasound evaluation of laryngeal mask airway position in pediatric patients: an observational study. Anesth Analg. 2015;120(2):427–432. doi:10.1213/ANE.0000000000000551
33. Figueiredo AA, Sales T, Nicolau LAD, et al. Laryngeal mucosa alterations in mice model of gastroesophageal reflux: effects of topical protection. Laryngoscope. 2020;130(12):E889–E895. doi:10.1002/lary.28597
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

