Back to Journals » Research and Reports in Urology » Volume 8
Efficacy and safety evaluation of pentoxifylline associated with other antioxidants in medical treatment of Peyronie's disease: a case-control study
Authors Paulis G , Barletta D, Turchi P, Vitarelli A, Dachille G, Fabiani A, Romano G
Received 26 September 2015
Accepted for publication 10 November 2015
Published 31 December 2015 Volume 2016:8 Pages 1—10
DOI https://doi.org/10.2147/RRU.S97194
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jan Colli
Gianni Paulis,1,2 Davide Barletta,3 Paolo Turchi,4 Antonio Vitarelli,5 Giuseppe Dachille,6 Andrea Fabiani,7 Romano Gennaro8
1Regina Apostolorum Hospital, Andrology Center, Albano L, 2Castelfidardo Medical Team, Peyronie's Disease Care Center, Rome, 3Department of Urology, Andrology Center, San Matteo Hospital, Pavia, 4Azienda ASL 4 Prato – Andrology Service, Prato, 5Department of Urology, University of Bari, 6Department of Urology, S Giacomo Hospital, Monopoli, Bari, 7Department of Surgery, Section of Urology and Andrology, Macerata, 8Department of Urologic Oncology, Section of Avellino, Italian League Against Cancer, Avellino, Italy
Abstract: Peyronie's disease (PD) is a chronic disorder involving the tunica albuginea surrounding the corpora cavernosa of the penis. A conservative treatment is indicated in the first stage of disease. The aim of this study was to assess the therapeutic impact and possible side effects of treatment with pentoxifylline (PTX) in combination with other antioxidants in 307 patients with early-stage PD. Patients were subdivided into three groups: A, B, and C. Both groups, A and B, comprising of 206 patients, underwent treatment, whereas Group C was the control group (n=101). Treatment lasted 6 months and included the following: Group A: PTX 400 mg twice a day + propolis 600 mg/d + blueberry 160 mg/d + vitamin E 600 mg/d + diclofenac 4% gel twice/a day + PTX 100 mg via perilesional penile injection/every other week (12 injections in all); Group B: the same treatment as Group A except for the penile PTX injections. After the 6-month treatment course, we obtained the following results: actual mean decrease in plaque volume -46.9% and -24.8% in Group A and B, respectively (P<0.0001); mean curvature reduction -10.1° and -4.8°, respectively (P<0.0001); resolution of pain in 67.6% and 67.2% of cases, respectively (P=0.961); recovery of normal penile rigidity in 56.09% and 23.5% of cases, respectively (P=0.005). After 6 months, progression of disease was observed in all patients belonging to Group C: plaque volume +123.3%; curvature +15.7°; no recovery of penile rigidity. The statistically significant results of our study show that multimodal treatment with PTX in association with other antioxidants and topical diclofenac is efficacious in treating early-stage PD. Furthermore, treatment proved to be more effective when PTX was administered both orally and by penile injection. No serious adverse effects occurred.
Keywords: multimodal treatment, penile curvature, penile injections, antioxidant supplementation
Introduction
Peyronie’s disease (PD) is a chronic inflammatory disease involving the tunica albuginea surrounding the corpora cavernosa of the penis. Prevalence of this disease varies between 3.6% and 13% as reported by various epidemiological studies.1–4 It is, therefore, not as rare a disease as is generally believed; in fact, PD prevalence is much higher than that of diabetes mellitus, which was 2.8% in 2000 (the estimated prevalence for 2030 is 4.4%).5
PD affects male subjects with a mean age of 50–55 years. PD is at times a treacherous disease, which unfortunately can affect even young men under 40 years of age, and in these cases, its evolution has been shown to be more rapid and its symptoms more evident.6–8
No clear understanding of the etiology of PD has been reached so far; however, there is general consensus that the major pathogenic mechanism arises as a consequence of penile trauma.9–11 The chronic inflammatory process is thus thought to occur in genetically predisposed male subjects after penile trauma or microtrauma.12,13
Following trauma and the related accumulation of fibrin, insufficient activation of the fibrinolytic process triggers the pathological mechanism that causes formation of plaque due to excessive production of collagen by fibroblasts and myofibroblasts.14–18 At the disease site, there is consistent production of reactive oxygen species (ROS) and proinflammatory cytokines, among which the most important is the transforming growth factor beta-1, largely responsible for the production of collagen in the disease site.18–22 The presence of oxidative stress leads to activation of the nuclear factor kappa-light-chain-enhancer of activated B-cells, which in turn causes further gene expression of proinflammatory cytokines, as well as gene expression of collagen, fibrin, and inducible nitric oxide synthase.18,23 The gradual local overproduction of collagen, associated with degradation–destruction of the elastic fibers of the tunica albuginea,24,25 gradually leads to a sectoral reduction in elasticity, which in turn causes inevitable morphological changes in the penis, ie, curvature, hourglass deformity, divots, and shortening. Besides penile curvature and the other possible morphological changes, the most frequent symptoms of PD are pain and erectile dysfunction.
Conservative medical treatment is indicated in the first stage of the disease, when there is still pain and penile curvature, and erectile dysfunction, if present, does not yet prevent complete sexual intercourse. Current medical-conservative therapies include oral substances (Potaba, tamoxifen, colchicine, carnitine, vitamin E, pentoxifylline [PTX], phosphodiesterase 5 inhibitors, flavonoids/propolis, blueberries), intralesional treatments (verapamil, collagenase clostridium histolyticum, interferon, iloprost, hyaluronic acid, steroids), topical treatments (diclofenac 4% gel, verapamil hydrochloride 15% gel, liposomal recombinant human superoxide dismutase gel), and local physical treatment (iontophoresis, extracorporeal shock wave therapy [ESWT], Capacitive Resistive Energy Transfer/TECAR therapy, traction, and vacuum devices).26–44 Our study consists uses a multimodal therapeutic approach to PD using antioxidant substances. We already had experience in using a combined therapy with antioxidants such as propolis, blueberries, and vitamin E associated with local treatment consisting of penile perilesional injections with verapamil.38–40 In this study, we decided to continue our positive experience with multimodal PD therapy, and thus, for the second time with a larger sample, we found an association between oral antioxidants and local perilesional injections, replacing verapamil with PTX, and administering it both orally and via injection.33 The reason behind this choice is that, in addition to its strong antioxidant effect, PTX also has antifibrogenic activity.45–48
Besides evaluating the efficacy of PTX, we aimed at making a more in-depth assessment regarding the tolerability of this interesting compound with antioxidant, antifibrogenic properties.
Materials and methods
We conducted this controlled study to analyze and learn more about the therapeutic effects and possible side effects of multimodal treatment with PTX associated with other antioxidant substances in subjects affected by PD in whom conservative management of the disease was indicated. For all patients, the fundamental inclusion criterion was therefore the presence of PD in an active, as yet unstabilized, stage.
The total number of patients who presented to our outpatient clinic between May 2, 2012 and December 31, 2014 with symptoms that were without doubt referable to PD was 381. However, 26 of them were excluded from the study because their clinical situation met one or more of the following exclusion criteria:
- any medical therapy for sexual dysfunction both prior to and during the study;
- PD in a stabilized phase;
- previous therapy for PD;
- severe erectile dysfunction;
- significant penile curvature preventing complete sexual intercourse;
- patients with allergy or intolerance to one or more of the substances used in the study;
- low blood pressure;
- patients receiving concomitant theophylline;
- patients receiving concomitant anticoagulant drugs (dicumarol, heparin, etc);
- presence of risk factors for hemorrhage;
- recent retinal or cerebral hemorrhage.
Exclusion criteria from number 7 to number 11 are exclusively relevant to contraindications to the use of PTX. Therefore, 355 patients affected by PD in its active, unstabilized stage were selected and enrolled. Before any treatment was administered, every patient was informed that one of the therapeutic options for PD was surgical treatment. All patients refused the surgical option a priori, and 101 of them preferred not to be treated even with conservative medical therapy due to various reasons: lack of trust in the type of therapy, fear of its side effects, hope of spontaneous resolution, underestimation of the disease, and overall costs of care.
We therefore divided patients into three groups, A, B, and C. Both treatment groups, A and B, received a 6-month combined therapy with various antioxidant substances and differed only in that Group A received penile injections with PTX, whereas Group B did not. However, both groups received oral PTX. Group C represents the control group, made up of patients who did not undergo any therapy. The detailed characteristics of the three groups are as follows:
- Group A: Oral therapy: PTX 400 mg twice a day + propolis 600 mg/d (on an empty stomach) + blueberry (vaccinium myrtillus) 160 mg/d + vitamin E 600 mg/d for 6 months. Diclofenac sodium 4% gel twice a day, applied as topical treatment to the dorsal and lateral surfaces of the penis (excluding the glans) for 6 months. PTX 100 mg was given as a perilesional injection in the penis using a thin 30-gauge needle, approximately every other week (twice a month) for 6 months and for a total number of 12 penile injections.
- Group B: Oral therapy: PTX 400 mg twice a day + propolis 600 mg daily (on an empty stomach) + blueberry (vaccinium myrtillus) 160 mg/d + vitamin E 600 mg/d for 6 months. Diclofenac sodium 4% gel twice a day, applied as topical treatment to the dorsal and lateral surfaces of the penis (excluding the glans) for 6 months.
- Group C: This was the control group and included all patients who opted not to undergo any treatment.
Unlike other authors, for several years we have preferred to administer penile injections close to the plaque and not within the plaque itself. In fact, since peyronie’s plaque is a densified zone with reduced or null stretchability-elasticity, we believe that an injection of a substance directly into the plaque may produce a strong pressure increase, thus causing further penile trauma. Furthermore, the perilesional injection, as it is not an intraplaque injection, does not require any previous local anesthesia.
Out of the 355 patients originally selected for the study, we had to exclude 48 further patients due to the following reasons:
- thirty-one cases were excluded because of various reasons (degree of penile curvature, plaque volume, plaque echogenicity, comorbidity, presence of erectile dysfunction), as they disrupted the necessary statistic homogeneity between the three groups;
- ten cases of patients who were treated for a few days but had to discontinue treatment early because they immediately presented uncomfortable side effects after administration of oral PTX (tachycardia, rash, low blood pressure, dizziness);
- seven cases who developed severe skin irritation after topical administration of diclofenac gel.
After accurate selection, 307 patients were finally enrolled and divided into three groups:
- Group A – 112 patients
- Group B – 94 patients
- Group C – 101 patients.
Patients assigned to Group C, although they refused to undergo any treatment, consented to be followed up after 6 months.
Propolis and blueberry were administered combined in a single tablet of Propolberry-3P® – Brea Srl, Grosseto, Italy (one tablet of Propolberry contains propolis – 600 mg and blueberry – 160 mg).
All 307 patients who took part in the study, besides undergoing a physical examination and careful collection of their clinical history, performed the following tests before and after the 6-month treatment period: dynamic penile color Doppler ultrasound with photographic documentation of the penis at maximum erection,49 IIEF questionnaire for the evaluation of erectile function,50 and pain rating questionnaire (pain intensity numeric rating scale/PI-NRS).51
The color Doppler ultrasound, besides assessing the plaque’s echogenicity, also included measurement of its three dimensions (length, width, and thickness),52 and imaging of the penis at maximum erection with photographic poses according to Kelâmi,49 for goniometric measurement of the curvature of the penis.
Plaque volume was measured in cm3 using the ellipsoid formula.53,54
To assess erectile function, we used the IIEF questionnaire,50 taking into consideration the answers that refer specifically to the evaluation of penile rigidity (IIEF-Erectile Function), ie, answers to questions 1–5 and question 15 (IIEF-EF normal score: 26–30). Patients with a score below 26 were identified as suffering from erectile dysfunction.
The questionnaire used to assess pain is based on analogical measurement of pain intensity on a scale with 11 points, going from 0 to 10 (PI-NRS), where 0= no pain and 10= worst possible pain.51
After the approval of the Institutional (LILT) ethics committee, specific written informed consents were obtained from 307 patients.
Our study was conducted according to the Declaration of Helsinki of 1975, 1983, and subsequent revisions.
Statistical analysis
Statistical comparison between the baseline and follow-up categorical variables was calculated using the chi-square (χ2) test. Statistical comparison between the baseline and follow-up continuous variables was calculated using Student’s t-test. A value of P<0.05 was considered statistically significant. To calculate statistics, we used the Primer of Biostatistics software package (Version 7.0, McGraw-Hill Global Education Holdings, LLC, NY, USA).
Results
The number of patients enrolled in the study was 307, with a mean age =53.6±11.1 (standard deviation, SD). Age varied between 22 and 73 years. Most subjects (255/307 cases =83.06%) presented penile curvature, with a mean curvature of 26.7°±12.6°.
Penile pain was present in 57.9% of patients (178 out of 307 cases), and their mean score on the PI-NRS was 4.8±2.7 SD. Erectile dysfunction was present in 36.1% of subjects (111 out of 307 cases), and their mean erectile function (IIEF-EF) score was 19.79±4.91 SD. In all cases presenting calcification, it was never present in the totality of the plaque, but only in a small percentage of the area affected by the disease, confirming that in all cases examined PD was still in an active, progressive stage.
Statistical comparison of the baseline clinical and demographic features of the three groups did not reveal any significant statistical differences, thus confirming a substantial homogeneity for subsequent statistical analysis (Table 1).
Evaluation of the therapeutic efficacy of the administered substances
Results after 6 months of treatment
Statistical analysis allowed us to find statistically significant differences between the two treatment groups (A and B) and the control group (C) in terms of the following: actual reduction in penile plaque volume and calcification volume, improvement in penile curvature, pain, and erectile function (Table 2).
At 6 months from study entry, a reduction in plaque volume was seen in all cases in Group A, in 79.7% of cases in Group B, and never in Group C (P<0.0001).
Specifically in Group A, an average of 46.9% reduction in plaque volume was observed; in Group B, the mean reduction was 24.8% (P<0.0001); and in Group C, an average 123.3% increase in plaque volume occurred (P<0.0001).
It must be specified that in Group A no increase in plaque volume was observed after the 6-month treatment, while an increase occurred in 5.3% of cases in Group B, and 98.01% of cases in Group C (P<0.0001).
After 6 months, when present, penile pain resolved in 67.6% of cases in Group A, 67.2% of cases in Group B, and 6.8% of cases in Group C (P<0.0001).
In Groups A and B, there was no progression of penile curvature after treatment, whereas in Group C curvature progressed in 80.7% of cases (P<0.0001).
After 6 months, a reduction in curvature occurred in Group A, B, and C in 96.8%, 56.4%, and 3.6% of cases, respectively. Actual measure of the decrease in curvature was, on average, −10.1° for Group A and −4.8° for Group B (P<0.0001), while in Group C curvature increased, on average, by 15.7° (P<0.0001).
With respect to penile rigidity in patients with ED, recovery of regular erections occurred in 56.09% of cases in Group A and 23.5% of cases in Group B (P=0.0052), whereas, on the contrary, no recovery occurred in Group C (A versus C: P<0.0001; B versus C: P=0.0019). It is important to stress the fact that at 6 months from study entry, no onset of ED occurred in patients belonging to Groups A and B who had no problems of rigidity, while in the control group (Group C) ED appeared at 6-month follow-up in 48% of patients who initially did not suffer from it (P<0.0001).
Evaluation of the tolerability of the substances used
Overall, our multimodal therapy was well tolerated.
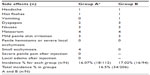
Tables 3 and 4 list side effects by substance and treatment group.
All adverse effects, except for those strictly localized to the penis, occurred exclusively after PTX was taken orally and never after penile injection with PTX or topical application of diclofenac gel. As already mentioned in the “Material and methods” section, a number of adverse effects, although not severe, were very bothersome and thus forced us to discontinue therapy.
Specifically, in ten cases oral treatment with PTX was discontinued after a few days because patients, after taking it a few times, presented uncomfortable side effects such as tachycardia, skin rashes, dizziness, or drop in blood pressure; in seven cases topical treatment with diclofenac gel was discontinued after a few days after onset of severe, widespread penile skin irritation.
Although these 17 cases were obviously excluded from subsequent treatment and thus from the study of clinical efficacy, nevertheless, to provide comprehensive information, we decided to report the adverse effects in Table 3 (first and last column).
In the other 24 cases, the adverse effects after administration of oral PTX (gastrointestinal problems and headache: 11.65%) were mild and short lasting and gradually disappeared over the course of treatment.
Overall, incidence of side effects after oral administration of PTX was 15.74% (34 cases out of 216).
Adverse effects after penile injection with PTX occurred in only four cases (3.57%) and consisted, in all cases, of a small ecchymosis, which never exceeded 1 cm in diameter.
The incidence of side effects after topical diclofenac application was, overall, 6.1% (13 cases out of 213), and consisted always in more or less widespread local skin irritation. As previously mentioned, in seven cases treatment was discontinued due to severe, widespread local irritation, while in six other cases the irritation on the skin of the penis was mild and temporary and regressed without discontinuing the medication.
Taking into consideration exclusively the 206 patients comprising treatment Groups A and B, the total incidence of adverse effects was 16.5% (34 cases out of 206; Table 4), while the incidence per group was 16.07% in Group A and 17.02% in Group B.
In our study, no severe adverse effects occurred.
Discussion
As other authors previously reported, we decided to use PTX to treat PD in its initial, not yet stabilized phase,31,32 intrigued by the interesting properties of PTX, which has been used since 1976 and is commonly employed to treat circulatory disorders, in particular in chronic peripheral artery disease.55,56
With its various properties, PTX acts on various crucial issues of PD, as our study results seem to confirm that besides reducing the production of ROS and protecting against damage to the tissue, it proved to have an anti-inflammatory and especially fibrinogen-reducing action, as it is an antagonist to fibrogenic cytokine TGF-β1.45–48,57
The anti-inflammatory action of PTX also derives from its inhibition of the transcription action of NF-κB and the release of proinflammatory cytokine TNF-α.58,59 PTX has also shown nonspecific inhibition of phosphodiesterase through the cyclic AMP pathway,60–62 and therefore, besides facilitating vasodilation and oxygenation of tissues, it promotes further antifibrogenic activity by stimulating apoptosis of the fibroblasts in the tunica albuginea of the corpora cavernosa.62
Our study joins that of other authors who, in their articles, confirmed the efficacy of PTX in the treatment of PD.31,32,63–66 In our study, however, we used the substance not only orally, but also via penile injection. We also used other antioxidant substances, ie, vitamin E, propolis, and blueberry, as part of our multimodal therapeutic approach. Vitamin E has antioxidant, anti-inflammatory, and antifibrogenic properties.39,67–69 Propolis, besides being an antioxidant, also contains caffeic acid phenethyl ester and terpenoids, which can hinder production of proinflammatory cytokines.70,71 Blueberries contain not only anthocyanins that have an antioxidant, anti-inflammatory action72 but also catechins, which are able to inhibit the production of platelet-derived growth factor and fibroblast growth factor – cytokines known to play a role in the physiopathological mechanisms of PD – through inhibition of tyrosine kinase receptors.73–76 The properties of nonsteroid anti-inflammatory drugs are known, including the action of diclofenac, which, in any case, we had already used previously in multimodal management of PD.38–40
The results of our study are interesting, as significant improvements were achieved in both A and B treatment groups in the most important parameters, such as degree of curvature, plaque volume, pain intensity, and penile rigidity.
It must also be noted that, contrary to general opinion, a reduction in the calcification component of plaque (where present) was obtained after treatment in both groups, while even complete resolution was observed in some cases (9.6% in Group A; 8.3% in Group B).
Although after 6 months, the results of Group A were, for the most part, better than those of Group B, the improvements in Group B were clearly significant in comparison with the results of control Group C.
Nevertheless, our study proved that PTX had greater efficacy when it was administered both orally and via perilesional injection (Group A), as clearly evident from the main study endpoints: reduction in plaque volume (P<0.0001), reduction in angle of curvature (P<0.0001), and improvement in erectile function (P=0.0016). Results of the follow-up of the patients in Group C showed a significant progression of disease in all study endpoints.
Comparison with the results of other treatment plans that call for intraplaque penile injections (interferon, verapamil, and collagenase) further persuades us of the efficacy of multimodal therapy, especially when PTX is used, not only because of the brilliant results achieved in the main endpoints, but also especially for the total absence of severe adverse effects such as penile hematomas or rupture of the corpora cavernosa.29
Although our study recorded an absence of severe side effects, the possibility of developing both general and gastrointestinal side effects after use of oral PTX is already known;77,78 in our study, side effects occurred in 15.74% of patients.
This is currently leading us to investigate how to avoid such effects, for instance, by associating transdermal administration of PTX (with iontophoresis or hydrophoresis replacing oral therapy) to the perilesional injections of PTX, or simply replacing oral PTX with Tradamixina.
Conclusion
Our study outcomes show that combined treatment with PTX associated with other minor antioxidants (propolis, blueberries, and vitamin E) and topical diclofenac is efficacious in treating PD. The study also demonstrated that clinical efficacy of PTX is greater when its oral administration is coupled with local administration via perilesional injection.
Our research confirms that in this disease long-term treatment yields the best results; in consideration of the fact that the first stage of PD has a duration of approximately 6–18 months, short-term therapies should thus certainly be avoided.23,26,79,80
Once again, multimodal therapy has been proven to be the best approach for conservative management of PD, as it makes it possible to achieve better results than those obtained with any single drug.28,64,81–90
Although our study achieved results that are extremely significant statistically, further randomized controlled trials are necessary to confirm the efficacy of PTX in the treatment of PD.
Acknowledgments
We are deeply grateful to Prof Furio Pirozzi Farina, President of the Società Italiana di Andrologia-S.I.A. and Prof Alessandro Palmieri, Secretary of the same Society (both in office in the period 2010–2013), for their exemplary leadership and constant encouragement throughout our study.
Disclosure
The authors report no conflicts of interest in this work.
References
Schwarzer U, Sommer F, Klotz T, Braun M, Reifenrath B, Engelmann U. The prevalence of Peyronie’s disease: results of a large survey. BJU Int. 2001;88:727–730. | |
Mulhall JP, Creech SD, Boorjian SA, et al. Subjective and objective analysis of the prevalence of Peyronie’s disease in a population of men presenting for prostate cancer screening. J Urol. 2004;171:2350–2353. | |
Dibenedetti DB, Nguyen D, Zografos L, Ziemiecki R, Zhou XA. Population-based study of Peyronie’s disease: prevalence and treatment patterns in the United States. Adv Urol. 2011;2011:282503. doi: 10.1155/2011/282503. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3202120/pdf/AU2011-282503.pdf. Accessed November 18, 2015. | |
Yafi FA, Pinsky MR, Sangkum P, Hellstrom WJ. Therapeutic advances in the treatment of Peyronie’s disease. Andrology. 2015;3(4):650–660. | |
Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–1053. | |
Tefekli A, Kandirali E, Erol H, Alp T, Köksal T, Kadioglu A. Peyronie’s disease in men under age 40: characteristics and outcome. Int J Impot Res. 2001;13(1):18–23. | |
Levine LA, Estrada CR, Storm DW, Matkov TG. Peyronie disease in younger men: characteristics and treatment results. J Androl. 2003;24(1):27–32. | |
Paulis G, Cavallini G, Barletta D, Turchi P, Vitarelli A, Fabiani A. Clinical and epidemiological characteristics of young patients with Peyronie’s disease: a retrospective study. Res Rep Urol. 2015;9(7):107–111. | |
Devine CJ Jr, Somers KD, Jordan GH, Schlossberg SM. Proposal: trauma as the cause of the Peyronie’s lesion. J Urol. 1997;157:285–290. | |
Jarow JP, Lowe FC. Penile trauma: an etiologic factor in Peyronie’s disease and erectile dysfunction. J Urol. 1997;158:1388–1390. | |
Zargooshi J. Trauma as the cause of Peyronie’s disease: penile fracture as a model of trauma. J Urol. 2004;172:186–188. | |
Rompel R, Weidner W, Mueller-Eckhardt G. HLA association of idiopathic Peyronie’s disease: an indication of autoimmune phenomena in etiopathogenesis? Tissue Antigens. 1991;38(3):104–106. | |
Dolmans GH, Werker PM, de Jong IJ, Nijman RJ; LifeLines Cohort Study, Wijmenga C, Ophoff RA. WNT2 locus is involved in genetic susceptibility of Peyronie’s disease. J Sex Med. 2012;9(5):1430–1434. | |
Diegelmann RF. Cellular and biochemical aspects of normal and abnormal wound healing: an overview. J Urol. 1997;157:298–302. | |
Somers KD, Dawson DM. Fibrin deposition in Peyronie’s disease plaque. J Urol. 1997;157:311–315. | |
Van de Water L. Mechanisms by which fibrin and fibronectin appear in healing wounds: implications for Peyronie’s disease. J Urol. 1997;157:306–310. | |
Gonzalez-Cadavid NF. Mechanisms of penile fibrosis. J Sex Med. 2009; 6(Suppl 3):353–362. | |
Paulis G, Brancato T. Inflammatory mechanisms and oxidative stress in Peyronie’s disease. Therapeutic “rationale” and related emerging treatment strategies. Inflamm Allergy Drug Targets. 2012;11:48–57. | |
Davila HH, Magee TR, Vernet D, Rajfer J, Gonzalez-Cadavid NF. Gene transfer of inducible nitric oxide synthase complementary DNA regresses the fibrotic plaque in an animal model of Peyronie’s disease. Biol Reprod. 2004;71(5):1568–1577. | |
Gonzalez-Cadavid NF, Magee TR, Ferrini M, Qian A, Vernet D, Rajfer J. Gene expression in Peyronie’s disease. Int J Impot Res. 2002;14(5):361–374. | |
El-Sakka AI, Hassoba HM, Pillarisetty RJ, Dahiya R, Lue TF. Peyronie’s disease is associated with an increase in transforming growth factor-beta protein expression. J Urol. 1997;158(4):1391–1394. | |
Zimmermann RP, Feil G, Bock C, Hoeltl L, Stenzl A. Significant alterations of serum cytokine levels in patients with Peyronie’s disease. Int Braz J Urol. 2008;34(4):457–466. | |
Sikka SC, Hellstrom WJG. Role of oxidative stress and antioxidants in Peyronie’s disease. Int J Impot Res. 2002;14:353–360. | |
Bichler KH, Lahme S, Mattauch W, Petri E. Collagen metabolism in induratio penis plastica (IPP). Urologe A. 1998;37(3):306–311. | |
Magee TR, Qian A, Rajfer J, Sander FC, Levine LA, Gonzalez-Cadavid NF. Gene expression profiles in the Peyronie’s disease plaque. Urology. 2002;59(3):451–457. | |
Hauck EW, Diemer T, Schmelz HU, Weidner W. A critical analysis of nonsurgical treatment of Peyronie’s disease. Eur Urol. 2006;49:987–997. | |
Levine LA, Estrada CR. Intralesional verapamil for the treatment of Peyronie’s disease: a review. Int J Impot Res. 2002;14(5):324–328. | |
Cavallini G, Biagiotti G, Koverech A, Vitali G. Oral propionyl-l-carnitine and intraplaque verapamil in the therapy of advanced and resistant Peyronie’s disease. BJU Int. 2002;89(9):895–900. | |
Gelbard M, Goldstein I, Hellstrom WJ, et al. Clinical efficacy, safety and tolerability of collagenase clostridium histolyticum for the treatment of peyronie disease in 2 large double-blind, randomized, placebo controlled phase 3 studies. J Urol. 2013;190(1):199–207. | |
Safarinejad MR, Hosseini SY, Kolahi AA. Comparison of vitamin E and propionyl-L-carnitine, separately or in combination, in patients with early chronic Peyronie’s disease: a double-blind, placebo controlled, randomized study. J Urol. 2007;178:1398–1403. | |
Brant WO, Dean RC, Lue TF. Treatment of Peyronie’s disease with oral pentoxifylline. Nat Clin Pract Urol. 2006;3(2):111–115. | |
Alizadeh M, Karimi F, Fallah MR. Evaluation of verapamil efficacy in Peyronie’s disease comparing with pentoxifylline. Glob J Health Sci. 2014;6(7 Spec No):23–30. | |
Paulis G, Pirozzi Farina F, Cavallini G, et al. Pentoxifylline associated with other antioxidants (multimodal therapy) on patients with Peyronie’s disease. Results of a controlled study. Andrology (Los Angel). 2014;3:123. doi: 10.4172/2167-0250.1000123. | |
Palmieri A, Imbimbo C, Creta M, Verze P, Fusco F, Mirone V. Tadalafil once daily and extracorporeal shock wave therapy in the management of patients with Peyronie’s disease and erectile dysfunction: results from a prospective randomized trial. Int J Androl. 2012;35(2):190–195. | |
Pavone C, Napoli G, Caruana G, Alonge V, Usala M, Abbadessa D. Safety and tolerability of local treatment with iloprost, a prostacyclin analogue, in patients with Peyronie’s disease: a phase I study. BJU Int. 2012;110(1):117–121. | |
Pavone C, Castrianni D, Romeo S, et al. TECAR therapy for Peyronie’s disease: a phase-one prospective study. Great evidence in patients with erectile dysfunction. Urologia. 2013;80(2):148–153. | |
Gennaro R, Barletta D, Paulis G. Intralesional hyaluronic acid: an innovative treatment for Peyronie’s disease. Int Urol Nephrol. 2015;47(10):1595–1602. doi: 10.1007/s11255-015-1074-1. | |
Paulis G, D’Ascenzo R, Nupieri P, et al. Effectiveness of antioxidants (propolis, blueberry, vitamin E) associated with verapamil in the medical management of Peyronie’s disease: a study of 151 cases. Int J Androl. 2012;35(4):521–527. | |
Paulis G, Cavallini G, Giorgio GD, Quattrocchi S, Brancato T, Alvaro R. Long-term multimodal therapy (verapamil associated with propolis, blueberry, vitamin E and local diclofenac) on patients with Peyronie’s disease (chronic inflammation of the tunica albuginea). Results of a controlled study. Inflamm Allergy Drug Targets. 2013;12(6):403–409. | |
Fitch WP 3rd, Easterling WJ, Talbert RL, Bordovsky MJ, Mosier M. Topical verapamil HCl, topical trifluoperazine, and topical magnesium sulfate for the treatment of Peyronie’s disease – a placebo-controlled pilot study. J Sex Med. 2007;4(2):477–484. | |
Riedl CR, Sternig P, Gallé G, et al. Liposomal recombinant human superoxide dismutase for the treatment of Peyronie’s disease: a randomized placebo-controlled double-blind prospective clinical study. Eur Urol. 2005;48(4):656–661. | |
Paulis G, Brancato T, D’Ascenzo R, et al. Efficacy of vitamin E in the conservative treatment of Peyronie’s disease: legend or reality? A controlled study of 70 cases. Andrology. 2013;1:120–128. | |
Martínez-Salamanca JI, Egui A, Moncada I, et al. Acute phase Peyronie’s disease management with traction device: a nonrandomized prospective controlled trial with ultrasound correlation. J Sex Med. 2014;11(2):506–515. | |
Raheem AA, Garaffa G, Raheem TA, et al. The role of vacuum pump therapy to mechanically straighten the penis in Peyronie’s disease. BJU Int. 2010;106(8):1178–1180. | |
Lin G, Shindel AW, Banie L, et al. Pentoxifylline attenuates transforming growth factor-beta1-stimulated elastogenesis in human tunica albuginea-derived fibroblasts part 2: interference in a TGF-beta1/Smad-dependent mechanism and downregulation of AAT1. J Sex Med. 2010;7(5):1787–1797. | |
Shindel AW, Lin G, Ning H, et al. Pentoxifylline attenuates transforming growth factor-beta1-stimulated collagen deposition and elastogenesis in human tunica albuginea-derived fibroblasts part 1: impact on extracellular matrix. J Sex Med. 2010;7(6):2077–2085. | |
Berman B, Duncan MR. Pentoxifylline inhibits normal human dermal fibroblast in vitroproliferation, collagen, glycosaminoglycan, and fibronectin production, and increases collagenase activity. J Invest Dermatol. 1989;92(4):605–610. | |
Berman B, Duncan MR. Pentoxifylline inhibits the proliferation of human fibroblasts derived from keloid, scleroderma and morphoea skin and their production of collagen, glycosaminoglycans and fibronectin. Br J Dermatol. 1990;123(3):339–346. | |
Kelâmi A. Autophotography in evaluation of functional penile disorders. Urology. 1983;21:628–629. | |
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishrs A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. | |
Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–158. | |
Prando D. New sonographic aspects of peyronie disease. J Ultrasound Med. 2009;28:217–232. | |
Behre HM, Zitzmann M. Imaging diagnostics. In: Nieschlag E, Behre HM, Nieschlag S, editors. Andrology: Male Reproductive Health and Dysfunction. Berlin: Springer-Verlag; 2010:101–108. | |
Kim CK, Cho JY. Prostate. In: Kim SH, editor. Radiology Illustrated: Uroradiology. Berlin: Springer-Verlag; 2012:826. | |
Ehrly AM. Improvement of the flow properties of blood: a new therapeutical approach in occlusive arterial disease. Angiology. 1976;27(3):188–196. | |
Kellner H. Treatment of chronic arterial circulatory disorders. Double blind trial with Trental 400. MMW Munch Med Wochenschr. 1976;118(43):1399–1402. | |
Taha H, Grochot-Przeczek A, Was H, et al. Modulation of inflammatory response by pentoxifylline is independent of heme oxygenase-1 pathway. J Physiol Pharmacol. 2009;60(2):3–12. | |
Shamsara J, Behravan J, Falsoleiman H, Mohammadpour AH, Ramezani M. The effects of pentoxifylline administration on NFKB P50 transcription factor expression. ARYA Atheroscler. 2012;7(4):133–137. | |
González-Espinoza L, Rojas-Campos E, Medina-Pérez M, Peña-Quintero P, Gómez-Navarro B, Cueto-Manzano AM. Pentoxifylline decreases serum levels of tumor necrosis factor alpha, interleukin 6 and C-reactive protein in hemodialysis patients: results of a randomized double-blind, controlled clinical trial. Nephrol Dial Transplant. 2012;27(5):2023–2028. | |
Tsutsumimoto T, Wakabayashi S, Kinoshita T, Horiuchi H, Takaoka K. A phosphodiesterase inhibitor, pentoxifylline, enhances the bone morphogenetic protein-4 (BMP-4)-dependent differentiation of osteoprogenitor cells. Bone. 2002;31(3):396–401. | |
Deree J, Martins JO, Melbostad H, Loomis WH, Coimbra R. Insights into the regulation of TNF-alpha production in human mononuclear cells: the effects of non-specific phosphodiesterase inhibition. Clinics (Sao Paulo). 2008;63(3):321–328. | |
Valente EG, Vernet D, Ferrini MG, Qian A, Rajfer J, Gonzalez- Cadavid NF. L-arginine and phosphodiesterase (PDE) inhibitors counteract fibrosis in the Peyronie’s fibrotic plaque and related fibroblast cultures. Nitric Oxide. 2003;9(4):229–244. | |
Smith JF, Shindel AW, Huang YC, et al. Pentoxifylline treatment and penile calcifications in men with Peyronie’s disease. Asian J Androl. 2011;13(2):322–325. | |
Abern MR, Larsen S, Levine LA. Combination of penile traction, intralesional verapamil, and oral therapies for Peyronie’s disease. J Sex Med. 2012;9(1):288–295. | |
Ciociola F, Colpi GM. Peyronie’s disease: a “triple oxygenant therapy”. Arch Ital Urol Androl. 2013;85(1):36–40. | |
Dell’Atti L, Ughi G. Efficacy of pentoxifylline in Peyronie’s disease: clinical case of a young man. Arch Ital Urol Androl. 2014;86(3):237–238. | |
O’Leary KA, de Pascual-Teresa S, Needs PW, Bao YP, O’Brien NM, Williamson G. Effect of flavonoids and vitamin E on cyclooxygenase-2 (COX-2) transcription. Mutat Res. 2004;551(1–2):245–254. | |
Parola M, Muraca R, Dianzani I, et al. Vitamin E dietary supplementation inhibits transforming growth factor beta 1 gene expression in the rat liver. FEBS Lett. 1992;308(3):267–270. | |
Alcalá M, Sánchez-Vera I, Sevillano J, et al. Vitamin E reduces adipose tissue fibrosis, inflammation, and oxidative stress and improves metabolic profile in obesity. Obesity (Silver Spring). 2015;23(8):1598–1606. | |
Márquez N, Sancho R, Macho A, Calzado MA, Fiebich BL, Muñoz E. Caffeic acid phenethyl ester inhibits T-cell activation by targeting both nuclear factor of activated T-cells and NF-kappaB transcription factors. J Pharmacol Exp Ther. 2004;308(3):993–1001. | |
de las Heras B, Hortelano S. Molecular basis of the anti-inflammatory effects of terpenoids. Inflamm Allergy Drug Targets. 2009;8:28–39. | |
Wang Q, Xia M, Liu C, et al. Cyanidin-3-O-beta-glucoside inhibits iNOS and COX-2 expression by inducing liver X receptor alpha activation in THP-1 macrophages. Life Sci. 2008;83(5–6):176–184. | |
Mulhall JP, Thom J, Lubrano T, Shankey TV. Basic fibroblast growth factor expression in Peyronie’s disease. J Urol. 2001;165(2):419–423. | |
Gentile V, Modesti A, La Pera G, et al. Ultrastructural and immunohistochemical characterization of the tunica albuginea in Peyronie’s disease and veno-occlusive dysfunction. J Androl. 1996;17(2):96–103. | |
Gouni-Berthold I, Sachinidis A. Molecular mechanisms explaining the preventive effects of catechins on the development of proliferative diseases. Curr Pharm Des. 2004;10(11):1261–1271. | |
Takai S, Matsushima-Nishiwaki R, Adachi S, et al. (-)-Epigallocatechin gallate reduces platelet-derived growth factor-BB-stimulated interleukin-6 synthesis in osteoblasts: suppression of SAPK/JNK. Mediators Inflamm. 2008;2008:291808. doi: 10.1155/2008/291808. | |
Escolar DM, Zimmerman A, Bertorini T, et al. Pentoxifylline as a rescue treatment for DMD: a randomized double-blind clinical trial. Neurology. 2012;78(12):904–913. | |
Tian ML, Shen Y, Sun ZL, Zha Y. Efficacy and safety of combining pentoxifylline with angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker in diabetic nephropathy: a meta-analysis. Int Urol Nephrol. 2015;47(5):815–822. | |
Hellstrom WJ. Medical management of Peyronie’s disease. J Androl. 2009;30(4):397–405. | |
Mulhall JP, Schiff J, Guhring P. An analysis of the natural history of Peyronie’s disease. J Urol. 2006;175:2115–2118. | |
Lamprakopoulos A, Zorzos I, Lykourinas M. The use of betamethasone and yaluronidase injections in the treatment of Peyronie’s disease. Scand J Urol Nephrol. 2000;34(6):355–360. | |
Prieto Castro RM, Leva Vallejo ME, Regueiro Lopez JC, Anglada Curado FJ, Alvarez Kindelan J, Requena Tapia MJ. Combined treatment with vitamin E and colchicine in the early stages of Peyronie’s disease. BJU Int. 2003;91(6):522–524. | |
Candebat Montero LH, Miranda Reyes PL, Díaz García F, González Ferro I, Barbosa Ramos F, Codorniu Furet J. Peyronie’s disease: treatment with interferon and laser. Arch Esp Urol. 2008;61(3):413–423. | |
Taylor FL, Levine LA. Non-surgical therapy of Peyronie’s disease. Asian J Androl. 2008;10(1):79–87. | |
Kuehhas FE, Weibl P, Georgi T, Djakovic N, Herwig R. Peyronie’s disease: nonsurgical therapy options. Rev Urol. 2011;13(3):139–146. | |
Larsen SM, Levine LA. Review of non-surgical treatment options for Peyronie’s disease. Int J Impot Res. 2012;24(1):1–10. | |
Halal AA, Geavlete P, Ceban E. Pharmacological therapy in patients diagnosed with Peyronie’s disease. J Med Life. 2012;5(2):192–195. | |
Levine LA. Peyronie’s disease: contemporary review of non-surgical treatment. Translational Androl Urol. 2013;2(1). Available from: http://www.amepc.org/tau/article/view/1461. Accessed November 18, 2015. | |
Favilla V, Russo GI, Privitera S, et al. Combination of intralesional verapamil and oral antioxidants for Peyronie’s disease: a prospective, randomised controlled study. Andrologia. 2014;46(8):936–942. | |
Paulis G. Combination therapy (in the treatment of Peyronie’s disease). In: Cavallini G, Paulis G, editors. Peyronie’s Disease. A Comprehensive Guide. Switzerland: Springer International Publishing; 2015:97–105. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.