Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Efficacy and cardiac safety of the concurrent use of trastuzumab and anthracycline-based neoadjuvant chemotherapy for HER2-positive breast cancer: a systematic review and meta-analysis
Authors Wu Y, Xu Z , Zhang K, Wu J, Li X, Arshad B, Li Y, Wang Z, Li H, Wu K, Kong L
Received 4 June 2018
Accepted for publication 23 July 2018
Published 26 September 2018 Volume 2018:14 Pages 1789—1797
DOI https://doi.org/10.2147/TCRM.S176214
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Yu-Tuan Wu,1,* Zhou Xu,1,* Ke Zhang,2,* Jiu-song Wu,3,* Xin Li,1,* Bilal Arshad,1 Ying-Cun Li,3 Zhong-Liang Wang,2 Hong-Yuan Li,1 Kai-Nan Wu,1 Ling-Quan Kong1
1Department of Endocrine and Breast Surgery, The First Affiliated Hospital of Chongqing Medical University, Chongqing 400016, China; 2Department of Orthopedics, Children’s Hospital of Chongqing Medical University, Chongqing 400020, China; 3Department of General Surgery, Children’s Hospital of Chongqing Medical University, Chongqing 400020, China
*These authors contributed equally to this work
Abstract: The concurrent use of trastuzumab and anthracycline-based neoadjuvant chemotherapy (NAC) has been proposed to improve the pathologic complete response (pCR) rate, although there are conflicting views about its efficacy and safety. The purpose of this study was to evaluate the efficacy and cardiac safety of the concurrent use of trastuzumab and anthracycline-based NAC for human epidermal growth factor receptor 2 (HER2)-positive locally advanced breast cancer. We systematically searched PubMed, Embase, and Cochrane databases from inception until July 1, 2017, for relevant articles. A total of 13 studies were included in the meta-analysis. The results showed that the pCR rate was significantly higher in the concurrent use of trastuzumab and anthracycline group (45%) than that in the nonconcurrent use group (32%) (OR: 2.36, 95% CI: 1.69–3.30, P<0.0001). Besides, the pooled absolute rate of breast conservation surgery (BCS) was 48% (95% CI: 0.35–0.61) and 38% (95% CI: 0.14–0.62) in the experimental and control groups, respectively (OR: 1.10, 95% CI: 0.64–1.90, P=0.73). No significant differences were found in the left ventricular ejection fraction (LVEF), which decreased by >10% (OR: 1.26, 95% CI: 0.55–2.88, P=0.59), and in terms of cardiac failure (OR: 2.17, 95% CI: 0.24–19.84, P=0.49), when comparing the concurrent use of trastuzumab and anthracyclines with their nonconcurrent use. In conclusion, the concurrent use of trastuzumab and anthracycline-based NAC for certain HER2-positive locally advanced breast cancers significantly improves the pCR rates without obvious increases in the cardiotoxicity.
Keywords: breast cancer, HER2, neoadjuvant chemotherapy, trastuzumab, anthracycline
Background
Breast cancer, being the most common malignancy and the second most common cause of cancer death in females, is rising rapidly in recent years.1 Neoadjuvant chemotherapy (NAC) has become a standard treatment for operable breast cancer; patients who are candidates for adjuvant chemotherapy are also candidates for NAC.2 The primary benefit of NAC is response-guided therapy and the potential to predict prognosis by pathologic complete response (pCR); besides, it would downstage the primary tumor in patients to make surgery more practicable. Patients intend to shrink the tumor size and obtain pCR after NAC,2 which would improve the chance for breast-conserving surgery and the rates of disease-free survival (DFS) and overall survival (OS).3,4 According to the molecular classification of breast cancer, about 20%–25% patients with metastatic tumor and 12%–17% patients with primary tumor overexpress the human epidermal growth factor receptor 2 (HER2), which is classified as HER2-positive breast cancer and is associated with more aggressive and dismal prognosis; fortunately, targeted therapy with the anti-HER2 monoclonal antibody trastuzumab seems to improve the prognosis of HER2-positive breast cancer patients.5–8 Thus, targeted therapy with trastuzumab is recommended as an important treatment for HER2-positive breast cancer.6,7 Meanwhile, anthracycline-based chemotherapy is one of the most common regimens in the treatment for breast cancer, also frequently used as a neoadjuvant regimen, and HER2-positive breast cancer is highly sensitive to anthracyclines.2 A meta-analysis reported that the addition of trastuzumab to NAC in HER2-positive breast cancer achieved higher pCR with no additional toxicity.9 However, considering the different active mechanisms and cardiotoxicity of both trastuzumab and anthracyclines, we should further analyze the effect and toxicity of the concurrent use of trastuzumab and anthracycline-based NAC. Recent studies reported that concurrent combination therapy with anthracycline-based chemotherapy and trastuzumab targeted therapy is expected to be a potential standard neoadjuvant treatment for locally advanced HER2-positive breast cancer since a higher pCR rate was achieved despite the potential cardiotoxicity of both trastuzumab and anthracyclines.5,8 However, the efficacy and cardiac safety of the concurrent use of trastuzumab and anthracycline-based NAC are controversial.
Therefore, we conducted a systematic review and meta-analysis of randomized and nonrandomized studies to compare the effect of concurrent vs nonconcurrent use of trastuzumab and anthracycline-based NAC in HER2-positive locally advanced breast cancer. We first calculated the rate of pCR attained. Furthermore, the cardiac safety of the combination therapy was evaluated. The result of this study would give advice on further clinical research into and application of the concurrent use of trastuzumab and anthracycline-based NAC in HER2-positive locally advanced breast cancer patients.
Methods
The systematic review and meta-analysis were conducted in accordance with the PRISMA guidelines.10 This study was performed in accordance with an established protocol and was prospectively registered in the International Prospective Register of Systematic Reviews (PROSPERO),11 and the registration information is available on https://www.crd.york.ac.uk/PROSPERO/ (registration number: CRD42017071427).
Eligibility criteria
We considered randomized and nonrandomized studies that had investigated the concurrent use of trastuzumab and anthracycline-based regimen NAC (experimental group) with or without a control group for HER2-positive breast cancer. Studies with the concurrent use of trastuzumab and anthracycline-based NAC were eligible for meta-analysis if they reported the data of pCR. Studies were ineligible under the following conditions: 1) they were reviews and case reports; 2) no experimental group was available or relevant data of interesting outcomes could not be extracted; 3) they contained cases with metastasis or coexisting other malignancies; 4) cases were not HER2-positive breast cancer patients; and 5) regimens contained other targeting drugs in addition to trastuzumab. HER2-positive breast cancer is defined as the condition wherein the HER2 immunohistochemistry score of the patient is 3+ or the fluorescence in situ hybridization (FISH) result indicates HER2 gene amplification.
Search strategy
We searched PubMed, Embase, and Cochrane databases from inception until July 1, 2017, for relevant articles in any language. The references were searched using a combination of medical subject heading terms and free text words, such as “breast neoplasm”, “breast cancer”, “breast carcinoma”, “neoadjuvant”, “preoperative”, “anthracycline”, “doxorubicin”, “epirubicin”, “Herceptin”, and “trastuzumab”. Two investigators independently performed the reference searches, and a third investigator was consulted when disagreement arose. More details of the search strategy are available in Supplementary materials.
Outcome measures
The primary outcomes were the absolute rates of pCR and the OR of the pCR, when comparing concurrent use with nonconcurrent use of trastuzumab and anthracycline-based NAC for HER2-positive breast cancer. The pCR is defined as the state in which no residual invasive carcinoma is found in the breast and axillary lymph nodes or the breast. The secondary outcomes were the absolute rates and OR of cardiac ejection fraction decrease (CED), cardiac failure (CF), complete response (CR), partial response (PR), breast conservation surgery (BCS), recurrence-free survival (RFS), and OS.
Study selection
All 1,175 references were identified after databases were searched. After duplicates were removed, two researchers independently assessed the eligible studies by scanning the titles and abstracts of articles. After that, we reviewed the full text of possible articles according to the inclusion and exclusion criteria. Finally, a total of 13 studies5,8,12–22 were included in the meta-analysis (Figure 1).
  | Figure 1 References selection flow diagram. |
Data extraction and quality assessment
Two researchers independently extracted information of the eligible studies using electronic tables. The following items were extracted from eligible articles: basic information, including the year of study publication, country, study design, sample size, age, chemotherapy regimen, type of cancer, and time of follow-up (Table S1); information on outcomes, including data on pCR and secondary outcome measures (Table S2).
We assessed the quality of the included studies using the Newcastle–Ottawa scale (NOS) (Table S3). The NOS has three parameters of quality assessment for prospective or retrospective cohort studies, including selection, comparability, and outcome assessment. The NOS assigns a maximum of four points for selection, two points for comparability, and three points for outcome. NOS scores of ≥7 points were considered to indicate high-quality studies and scores of 5–6 points were considered to indicate moderate quality. A third investigator was consulted when disagreement arose between the prior reviewers.
Statistical analyses
We pooled the absolute rates of pCR and secondary outcomes in the experimental and control groups, as well as the ORs with the 95% CIs of pCR and secondary outcomes, and compared the concurrent use with nonconcurrent use of trastuzumab and anthracycline-based NAC for HER2-positive breast cancer. The meta-analysis was carried out using the Cochrane Collaboration’s Review Manager Software (RevMan, version 5.3; Cochrane Collaboration, Oxford, UK) and R software (version 3.3.2; R Foundation for Statistical Computing, Vienna, Austria). Probability values were two-sided, and P<0.05 was considered of statistical significance. Statistical heterogeneity was evaluated using the I-squared (I2) and chi-squared (χ2) tests. I2 values of 25%, 50%, and 75% indicated low, moderate, and high levels of heterogeneity, respectively. A P-value of <0.1 for χ2 was defined to indicate the presence of heterogeneity. Results were pooled using the maximum likelihood estimation. A random-effects model was used for analysis if heterogeneity existed; otherwise, a fixed-effect model was used. Besides, sensitivity analysis was performed by excluding the heterogeneity study or the study of the least sample size depending on the presence or absence of significant heterogeneity. Funnel plots and the Egger’s test of funnel plot asymmetry were used to evaluate publication bias.
Results
Description of included studies
Overall, 13 studies were included in this meta-analysis after ineligible studies were excluded from the 1,175 identified references (Figure 1), and 1,391 HER2-positive breast cancer patients were analyzed for the concurrent use of trastuzumab and anthracycline-based NAC.
We have summarized the baseline characteristics in Table S1 and the extracted data in Table S2. Of the 13 studies, four studies were randomized trials, six studies were prospective cohorts, and three studies were retrospective cohorts. Five studies had two arms; meanwhile, eight studies in the meta-analysis were single-armed ones (experimental arm), of which three studies’ control groups were abandoned because the patients were not HER2 positive or because the treatment regimen was not suitable for comparing with the experimental group.
We evaluated the quality of the included studies using the NOS (Table S3). We found that all of the included studies were of moderate or high quality, and hence the included studies were reliable. Besides, we assessed the publication bias of the included studies using symmetrical funnel plot analysis and Egger’s tests, and the result showed no significant publication bias. Meanwhile, we found significant between-study heterogeneity, and the random-effects model was used.
The pCR rate of concurrent vs nonconcurrent use of trastuzumab and anthracycline-based NAC in HER2-positive breast cancer patients
All 13 studies, which included 1,391 patients, were analyzed for the pCR rate after concurrent use of trastuzumab and anthracycline-based NAC in HER2-positive breast cancer patients. The pCR rate ranged from 7% to 65% in the 13 studies, and the pooled absolute rate of pCR was 45% (95% CI: 0.36–0.54) (Figure 2A).
Meanwhile, all four studies, including 248 patients, reported the pCR rate of nonconcurrent use of trastuzumab and anthracycline-based NAC in HER2-positive breast cancer patients. There were two studies using the same control group; thus, we excluded one study for control group analysis. The pCR rate ranged from 22% to 40% in the four studies, and the pooled absolute rate of pCR was 32% (95% CI: 0.21–0.42) (Figure 2B).
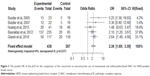
In total, five studies had compared the pCR rate of concurrent vs nonconcurrent use of trastuzumab and anthracycline-based NAC in HER2-positive breast cancer patients. The meta-analysis of the five studies showed that patients with concurrent use of trastuzumab and anthracycline-based NAC had a substantially higher pCR rate, and the OR was 2.36 (95% CI: 1.69–3.30, P<0.0001) (Figure 3). No significant between-study heterogeneity was found, and the fixed-effect model was used. Sensitivity analysis showed that no single study could significantly alter the overall pooled effect.
The CR rate of concurrent vs nonconcurrent use of trastuzumab and anthracycline-based NAC in HER2-positive breast cancer patients
Seven studies reported the CR rate of concurrent use of trastuzumab and anthracycline-based NAC in HER2-positive breast cancer patients. Meanwhile, three studies reported the CR rate of nonconcurrent use of trastuzumab and anthracycline-based NAC in HER2-positive breast cancer patients. The pooled absolute rate of CR was 51% (95% CI: 0.34–0.68) and 37% (95% CI: 0.11–0.63) in the experimental group and the control group, respectively (Figure S1), and the OR was 3.03 (95% CI: 1.50–6.13, P=0.002) (Figure 4).
The PR rate of concurrent vs nonconcurrent use of trastuzumab and anthracycline-based NAC in HER2-positive breast cancer patients
Ten studies analyzed the PR rate for the concurrent combination therapy, and three studies reported the PR rate for nonconcurrent use of trastuzumab and anthracycline-based NAC. The pooled absolute rate of PR was 49% (95% CI: 0.31–0.68) and 47% (95% CI: 0.04–0.91) in the experimental group and the control group, respectively (Figure S2), and the OR was 0.32 (95% CI: 0.11–0.92, P=0.03) (Figure 4).
The BCS rate of concurrent vs nonconcurrent use of trastuzumab and anthracycline-based NAC in HER2-positive breast cancer patients
Usually, surgery of breast cancer was planned after NAC, and BCS was one of the favorable choices. However, the choice of BCS was partly dependent on the efficacy of NAC. Totally, nine studies reported the BCS rate of the concurrent combination therapy, and two studies reported the BCS rate of nonconcurrent use of trastuzumab and anthracycline-based NAC. The pooled absolute rate of BCS was 48% (95% CI: 0.35–0.61) and 38% (95% CI: 0.14–0.62) in the experimental and control groups, respectively (Figure S3). The concurrent use of trastuzumab and anthracycline-based NAC did not result in significantly increased BCS rate compared to the results from nonconcurrent use of trastuzumab and anthracycline-based NAC; the OR was 1.10 (95% CI: 0.64–1.90, P=0.73) (Figure 4).
The CED rate of concurrent vs nonconcurrent use of trastuzumab and anthracycline-based NAC in HER2-positive breast cancer patients
Cardiotoxicity is a common side effect when resorting to treatment with trastuzumab and anthracyclines, and CED is a sign of cardiotoxicity. Usually, the left ventricular ejection fraction (LVEF) is calculated to represent the CED. Eleven studies calculated the LVEF decrease with concurrent combination therapy, and four studies reported the LVEF decrease on nonconcurrent use of trastuzumab and anthracycline-based NAC. After excluding an obvious heterogeneous study,14 the pooled absolute rate of >10% LVEF decrease was 8% (95% CI: 0.04–0.16) and 14% (95% CI: 0.05–0.23) in experimental and control groups, respectively (Figure S4), and the OR was 1.26 (95% CI: 0.55–2.88, P=0.59) (Figure 4).
CF is a fatal outcome of cardiotoxicity caused by trastuzumab and anthracyclines. Four studies reported on patients with apparent cardiac dysfunction; totally, five patients showed CF in the experimental group, but no one was dead from CF. When comparing the CF rate between the experimental and the control groups, the OR was 2.17 (95% CI: 0.24–19.84, P=0.49) (Figure 4).
Survival benefits
During the period of follow-up in the individual study (the maximum and minimum durations of follow-up were 46.0 months and 16.2 months), the pooled absolute rate of RFS was 86% (95% CI: 0.78–0.94) and 76% (95% CI: 0.58–0.95) in the experimental and control groups, respectively (Figure S5). When comparing the RFS rate between the experimental and the control groups, the OR was 3.34 (95% CI: 1.32–8.43, P=0.01) (Figure 4). Meanwhile, the absolute rate of OS was 96% (95% CI: 0.94–0.99) and 90% (95% CI: 0.79–1.00) in the experimental and control groups, respectively (Figure S6), and the OR was 2.30 (95% CI: 1.13–4.66, P=0.02) (Figure 4).
Discussion
Recently, NAC has become a general approach in the treatment of locally advanced breast cancer, which mainly aims to reduce the size of the tumor and even obtain pCR, eventually allowing radical surgery or more BCS.2 The pCR after NAC is reported to be a valuable surrogate of long-term DFS. It is hypothesized that higher rates of pCR would also result in higher rates of long-term survival.8,23 The concurrent use of trastuzumab with multiple chemotherapy agents, used as the neoadjuvant therapy for locally advanced HER2-positive breast cancer, has been reported to have better efficacy compared with chemotherapy alone.9,24,25 Meanwhile, several studies have reported conflicting results about the efficacy and safety of the concurrent use of trastuzumab and anthracycline-based NAC for HER2-positive locally advanced breast cancer. As reported by Buzdar et al,8 26% in the chemotherapy-alone arm achieved pCR; meanwhile, 65.2% in the trastuzumab-plus-anthracycline-based NAC arm achieved pCR, with no clinical congestive CF being observed. Here, our meta-analysis evaluated the efficacy and safety of the concurrent use of trastuzumab and anthracycline-based NAC for HER2-positive locally advanced breast cancer.
Our study shows a higher pCR rate in the concurrent use of trastuzumab and anthracycline-based NAC (45%) compared to the rate (32%) with nonconcurrent use of trastuzumab and anthracycline-based NAC. Meanwhile, the rate of CR was higher in the group with concurrent use of trastuzumab and anthracycline-based NAC, but a similar result was not observed in terms of PR, which may due to the limitation of eligible data. Interestingly, the BCS rate was not significantly higher when comparing the concurrent vs nonconcurrent use of trastuzumab and anthracycline-based NAC despite the higher rate of pCR in the concurrent use of trastuzumab-and-anthracycline group. It is a reasonable result when considering the fact that BCS is affected by various factors, such as patients’ will, iatrogenic factors, and economic factors, in addition to the pCR obtained. However, the absolute rate of BCS was higher in the concurrent use of trastuzumab and anthracyclines group (48%) compared with the result in the nonconcurrent use of trastuzumab and anthracyclines group (38%). BCS patients were reported to obtain long-term survival equivalent to that for patients of mastectomy; meanwhile, BCS provides better cosmetic effects and improves the quality of life.26,27 Furthermore, our result shows superior survival benefits in terms of RFS and OS in the group with concurrent use of trastuzumab and anthracycline-based NAC. It seems that the better efficacy of the concurrent use of trastuzumab and anthracycline-based NAC had translated into better long-term tumor control by reducing the chance of proliferation and metastasis of tumor cells.
Cardiotoxicity is one of the most closely observed concerns in the use of trastuzumab and anthracyclines for HER2-positive locally advanced breast cancer, especially with concurrent use of trastuzumab and anthracyclines. It was reported that the concurrent use of trastuzumab plus anthracyclines would result in a high rate of cardiotoxicity.28 Therefore, many clinical research works and practices had avoided the concurrent use of trastuzumab and anthracyclines. In this meta-analysis, we evaluated the cardiotoxicity of the concurrent use of trastuzumab plus anthracycline-based NAC for HER2-positive locally advanced breast cancer. Interestingly, our results indicate that the concurrent use of trastuzumab and anthracyclines resulted in less risk of cardiotoxicity than the nonconcurrent use of trastuzumab and anthracycline-based NAC, and this result was coincidentally in accordance with a meta-analysis that reported that patients treated with trastuzumab and anthracyclines had a lower rate of cardiotoxicity (16%) than those treated with anthracyclines alone (20%).29 The rate of >10% LVEF decrease was lower despite the concurrent use of trastuzumab and anthracyclines, and this may be due to the fact that patients with younger age and better basic cardiac function were more likely to receive the concurrent use of trastuzumab and anthracyclines. Meanwhile, the CF event was rare and did not show any significant difference between the two groups. Therefore, the results of our meta-analysis are in accordance with previous studies in which low cardiotoxicity was observed in the concurrent use of trastuzumab and anthracyclines during chemotherapy.29 In conclusion, the concurrent use of trastuzumab plus anthracycline-based NAC for HER2-positive locally advanced breast cancer is suggested to be safe in terms of cardiotoxicity. However, the patients should be carefully and closely evaluated for cardiac function before and during the concurrent use of trastuzumab plus anthracyclines.
Trastuzumab, a chimeric humanized monoclonal antibody to the extracellular region of the HER2 protein that reduces the proliferation of tumor cells, is confirmed to be good for the prognosis of HER2-positive breast cancer. However, trastuzumab alone has modest antitumor activity.8,30 Anthracycline-based regimens are recommended as one of the standard NAC regimens in breast cancer patients, and a previous study has demonstrated that anthracycline-containing regimens were superior to non-anthracycline-containing regimens in HER2-positive breast cancer patients.31 It was hypothesized that a significantly better curative effect would be obtained when trastuzumab and anthracyclines were combined since they have different mechanisms of action. Bayraktar et al14 reported that neoadjuvant therapy with trastuzumab concurrent with anthracycline-based regimens achieved a higher rate of pCR and RFS for HER2-positive breast cancer, and no significant adverse events were observed. Two previous meta-analyses showed that trastuzumab combined with NAC significantly increases the rate of pCR without increasing additional toxicity.9,24 However, these two studies had small sample sizes and did not analyze the subgroup of concurrent use of trastuzumab and anthracycline-based regimens. Therefore, our study seems to provide unique and more powerful evidence.
To our knowledge, this is the first meta-analysis to evaluate the efficacy and cardiac safety of the concurrent use of trastuzumab plus anthracycline-based NAC for HER2-positive locally advanced breast cancer. Our meta-analysis undoubtedly gives evidence to guide the clinical research and practice of the concurrent use of trastuzumab plus anthracycline-based NAC for HER2-positive locally advanced breast cancer. Nonetheless, our meta-analysis has some limitations, which should be noted. First, five studies were of two arms and eight studies were of single arm; meanwhile, only four studies were randomized trials in spite of systematically searching all eligible studies. Second, the chemotherapy regimens were not strictly the same in the individual included studies, but the chemotherapy regimens were all anthracycline-based regimens. Furthermore, we could not analyze other side effects, such as diarrhea, vomiting, neutropenia, and dermatologic toxicity due to the lack of relevant data in the included studies. Further research should be designed to conduct a systematic study of the side effects of the concurrent use of trastuzumab plus anthracyclines.
Conclusion
Taken together, our study indicates that the concurrent use of trastuzumab and anthracycline-based NAC for HER2-positive locally advanced breast cancer significantly improves the pCR rates without obvious increase in the cardiotoxicity events. During the period of follow-up, the concurrent use of trastuzumab and anthracycline-based NAC was superior to the nonconcurrent use of trastuzumab and anthracycline-based NAC in terms of RFS and OS. Our results support the efficacy and cardiac safety of the concurrent use of trastuzumab plus anthracycline-based NAC for certain patients with HER2-positive locally advanced breast cancer.
Acknowledgment
This study was funded by the Graduate Student’s Science Innovation Project of Chongqing (CYS16124) and National Natural Science Foundation of China (NSFC) (81372851).
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Disclosure
The authors report no conflicts of interest in this work.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7–30. | ||
Rubovszky G, Horváth Z. Recent Advances in the Neoadjuvant Treatment of Breast Cancer. J Breast Cancer. 2017;20(2):119–131. | ||
Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384(9938):164–172. | ||
Untch M, Fasching PA, Konecny GE, et al. Pathologic complete response after neoadjuvant chemotherapy plus trastuzumab predicts favorable survival in human epidermal growth factor receptor 2-overexpressing breast cancer: results from the TECHNO trial of the AGO and GBG study groups. J Clin Oncol. 2011;29(25):3351–3357. | ||
Uriarte-Pinto M, Escolano-Pueyo A, Gimeno-Ballester V, Pascual-Martinez O, Abad-Sazatornil MR, Agustin-Ferrandez MJ. Trastuzumab, non-pegylated liposomal-encapsulated doxorubicin and paclitaxel in the neoadjuvant setting of HER-2 positive breast cancer. Int J Clin Pharm. 2016;38(2):446–453. | ||
Goldhirsch A, Wood WC, Coates AS, et al; Panel members. Strategies for subtypes – dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22(8):1736–1747. | ||
Goldhirsch A, Winer EP, Coates AS, et al; Panel members. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol. 2013;24(9):2206–2223. | ||
Buzdar AU, Ibrahim NK, Francis D, et al. Significantly higher pathologic complete remission rate after neoadjuvant therapy with trastuzumab, paclitaxel, and epirubicin chemotherapy: results of a randomized trial in human epidermal growth factor receptor 2-positive operable breast cancer. J Clin Oncol. 2005;23(16):3676–3685. | ||
Valachis A, Mauri D, Polyzos NP, Chlouverakis G, Mavroudis D, Georgoulias V. Trastuzumab combined to neoadjuvant chemotherapy in patients with HER2-positive breast cancer: a systematic review and meta-analysis. Breast. 2011;20(6):485–490. | ||
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269, W64. | ||
Booth A, Clarke M, Dooley G, et al. The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Syst Rev. 2012;1:2. | ||
Buzdar AU, Valero V, Ibrahim NK, et al. Neoadjuvant therapy with paclitaxel followed by 5-fluorouracil, epirubicin, and cyclophosphamide chemotherapy and concurrent trastuzumab in human epidermal growth factor receptor 2-positive operable breast cancer: an update of the initial randomized study population and data of additional patients treated with the same regimen. Clin Cancer Res. 2007;13(1):228–233. | ||
Huang L, Chen S, Yang W, et al. Efficacy and safety analysis of trastuzumab and paclitaxel based regimen plus carboplatin or epirubicin as neoadjuvant therapy for clinical stage II–III, HER2-positive breast cancer patients: a phase 2, open-label, multicenter, randomized trial. Oncotarget. 2015;6(21):18683–18692. | ||
Bayraktar S, Gonzalez-Angulo AM, Lei X, et al. Efficacy of neoadjuvant therapy with trastuzumab concurrent with anthracycline- and nonanthracycline-based regimens for HER2-positive breast cancer. Cancer. 2012;118(9):2385–2393. | ||
Pizzuti L, Barba M, Giannarelli D, et al. Neoadjuvant Sequential Docetaxel Followed by High-Dose Epirubicin in Combination With Cyclophosphamide Administered Concurrently With Trastuzumab. The DECT Trial. J Cell Physiol. 2016;231(11):2541–2547. | ||
Dawood S, Gonzalez-Angulo AM, Peintinger F, et al. Efficacy and safety of neoadjuvant trastuzumab combined with paclitaxel and epirubicin: a retrospective review of the M. D. Anderson experience. Cancer. 2007;110(6):1195–1200. | ||
Wenzel C, Hussian D, Bartsch R, et al. Preoperative therapy with epidoxorubicin and docetaxel plus trastuzumab in patients with primary breast cancer: a pilot study. J Cancer Res Clin Oncol. 2004;130(7):400–404. | ||
Gavilá J, Guerrero Á, Climent MÁ, et al. Efficacy and safety of neoadjuvant chemotherapy with concurrent liposomal-encapsulated doxorubicin, paclitaxel and trastuzumab for human epidermal growth factor receptor 2-positive breast cancer in clinical practice. Int J Clin Oncol. 2015;20(3):480–489. | ||
Untch M, Rezai M, Loibl S, et al. Neoadjuvant treatment with trastuzumab in HER2-positive breast cancer: results from the GeparQuattro study. J Clin Oncol. 2010;28(12):2024–2031. | ||
Gianni L, Eiermann W, Semiglazov V, et al. Neoadjuvant chemotherapy with trastuzumab followed by adjuvant trastuzumab versus neoadjuvant chemotherapy alone, in patients with HER2-positive locally advanced breast cancer (the NOAH trial): a randomised controlled superiority trial with a parallel HER2-negative cohort. Lancet. 2010;375(9712):377–384. | ||
Untch M, Loibl S, Bischoff J, et al; German Breast Group (GBG); Arbeitsgemeinschaft Gynäkologische Onkologie-Breast (AGO-B) Study Group. Lapatinib versus trastuzumab in combination with neoadjuvant anthracycline-taxane-based chemotherapy (GeparQuinto, GBG 44): a randomised phase 3 trial. Lancet Oncol. 2012;13(2):135–144. | ||
Tuxen MK, Cold S, Tange UB, Balslev E, Nielsen DL. Phase II study of neoadjuvant pegylated liposomal doxorubicin and cyclophosphamide ± trastuzumab followed by docetaxel in locally advanced breast cancer. Acta Oncol. 2014;53(10):1440–1445. | ||
Hamy-Petit AS, Belin L, Bonsang-Kitzis H, et al. Pathological complete response and prognosis after neoadjuvant chemotherapy for HER2-positive breast cancers before and after trastuzumab era: results from a real-life cohort. Br J Cancer. 2016;114(1):44–52. | ||
Petrelli F, Borgonovo K, Cabiddu M, Ghilardi M, Barni S. Neoadjuvant chemotherapy and concomitant trastuzumab in breast cancer: a pooled analysis of two randomized trials. Anticancer Drugs. 2011;22(2):128–135. | ||
Chen YY, Wang LW, Chen FF, Wu BB, Xiong B. Efficacy, safety and administration timing of trastuzumab in human epidermal growth factor receptor 2 positive breast cancer patients: A meta-analysis. Exp Ther Med. 2016;11(5):1721–1733. | ||
Clarke M, Collins R, Darby S, et al; Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;366(9503):2087–2106. | ||
van Maaren MC, de Munck L, de Bock GH, et al. 10 year survival after breast-conserving surgery plus radiotherapy compared with mastectomy in early breast cancer in the Netherlands: a population-based study. Lancet Oncol. 2016;17(8):1158–1170. | ||
Friedrich MJ. Cardiotoxicity concerns prompt data review in breast cancer trial. J Natl Cancer Inst. 2002;94(9):650–651. | ||
Guenancia C, Lefebvre A, Cardinale D, et al. Obesity As a Risk Factor for Anthracyclines and Trastuzumab Cardiotoxicity in Breast Cancer: A Systematic Review and Meta-Analysis. J Clin Oncol. 2016;34(26):3157–3165. | ||
Vogel CL, Cobleigh MA, Tripathy D, Gutheil JC, et al. Efficacy and safety of trastuzumab as a single agent in first-line treatment of HER2-overexpressing metastatic breast cancer. J Clin Oncol. 2002;20(3):719–726. | ||
Chen X, Ye G, Zhang C, Li X, Shen K. Non-anthracycline-containing docetaxel and cyclophosphamide regimen is associated with sustained worse outcome compared with docetaxel, anthracycline and cyclophosphamide in neoadjuvant treatment of triple negative and HER2-positive breast cancer patients: updated follow-up data from NATT study. Chin J Cancer Res. 2016;28(6):561–569. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.