Back to Journals » Nutrition and Dietary Supplements » Volume 8
Effects of vegetarian diets on blood pressure
Authors Yokoyama Y, Tsubota K , Watanabe M
Received 12 September 2015
Accepted for publication 18 February 2016
Published 28 April 2016 Volume 2016:8 Pages 57—64
DOI https://doi.org/10.2147/NDS.S74715
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Gary Johanning
Yoko Yokoyama,1,2 Kazuo Tsubota,2,3 Mitsuhiro Watanabe1,2,4,5
1Graduate School of Media and Governance, Keio University, Fujisawa, Kanagawa, 2Health Science Laboratory, 3Department of Ophthalmology, 4Department of Internal Medicine, Keio University School of Medicine, Tokyo, 5Faculty of Environment and Information Studies, Keio University, Fujisawa, Kanagawa, Japan
Abstract: Hypertension is a major independent risk factor for coronary artery diseases, and the prevalence of hypertension is continuously increasing. Diet is an important factor that can be modified to prevent hypertension. According to the US Department of Health and Human Services, dietary patterns are defined as the quantities, proportions, and variety or combinations of different foods and beverages in diets and the frequency with which they are habitually consumed. In this review, the vegetarian dietary pattern is introduced with a focus on the effect on blood pressure (BP). Although the available evidence is limited, according to a previous meta-analysis of controlled trials, vegetarian dietary patterns significantly reduced systolic and diastolic BPs. One of the common features of a vegetarian diet is weight loss, which might, at least partially, explain the effect on BP. Other possible factors such as sodium, potassium, protein, amino acids, vitamin B-12, antioxidants, fiber, and the microbiome are introduced as possible mechanisms. Further studies are needed with non-Western populations to determine the most effective vegetarian dietary pattern and to explore the exact mechanisms by which these dietary patterns affect BP.
Keywords: vegetarian diet, plant-based diet, blood pressure, hypertension, meta-analysis
Introduction
Hypertension is a major independent risk factor for coronary artery diseases, irrespective of age, race, or sex.1 According to the World Health Organization, hypertension is the cause of at least 45% of deaths due to heart disease and 51% of deaths due to stroke.2 The number of people with hypertension has gradually increased from 600 million in 1980 to 1 billion in 2008.3 According to the Centers for Disease Control and Prevention, 32.5% of adults aged ≥20 years have hypertension, defined as high blood pressure (BP) and/or are taking antihypertensive medications.4 This high prevalence highlights the importance of utilizing public health approaches for the prevention of hypertension.
Diet is an important factor that can be modified to prevent hypertension. Sufficient evidence supports the role of modifiable factors, including diet, body weight, physical activity, and alcohol intake in the development of hypertension. Dietary modifications have been shown to be particularly effective in preventing and managing hypertension.5 Nutritional epidemiology typically examines diseases while considering a single or few nutrients or foods.6 Hu indicated that the results of nutrient analysis can be difficult to interpret as individuals do not consume nutrients in isolation. Dietary interventions may be easier to implement and more comprehensive when they are initiated as changes in the overall dietary pattern.6
Vegetarian dietary pattern and BP
Dietary patterns are defined as “the quantities, proportions, variety, or combinations of different foods and beverages in diets, and the frequency with which they are habitually consumed” by the US Department of Health and Human Services.7 In this paper, vegetarian dietary patterns are introduced while considering their influence on BP.
According to the position statement issued by the American Dietetic Association, now called the Academy of Nutrition and Dietetics, a vegetarian diet is defined as “one that does not include meat (including fowl) or seafood, or products containing those foods.”8 Although this is considered the standard definition, it has not been used by all researchers reporting the outcomes of vegetarian diets. Therefore, in this paper, vegetarian diets are defined as dietary patterns that exclude or rarely include meats; some vegetarian diets include dairy products, egg, and fish. All vegetarian diets emphasize the consumption of foods of plant origin, particularly vegetables, grains, legumes, and fruits. The definition used in this paper was based on articles included in a recent meta-analysis and prospective cohort studies with a high percentage of vegetarian participants.
Results from cross-sectional studies
The information in this section is based on three cross-sectional studies with high percentages of vegetarian participants:9 the Adventist Health Study-210 (36%), European Prospective Investigation into Cancer and Nutrition-Oxford (EPIC-Oxford)11 (33%), and the UK Women’s Cohort Study12 (29%; Table 1).
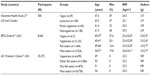  | Table 1 Characteristics of the observational studies included in the review |
BP was compared according to the dietary pattern in 500 white participants in the Adventist Health Study-2 cohort. The dietary patterns were determined using a validated food frequency questionnaire that asked their usual or average diet during the past year. Individuals consuming a vegan–vegetarian diet (consume meat, fish, and dairy products less than once a month) had a lower prevalence of hypertension (defined as systolic BP >139 mmHg, diastolic BP >89 mmHg, or taking prescribed antihypertensive medications) than omnivorous individuals (odds ratio [OR] =0.37; 95% confidence interval [CI], 0.19–0.74). Moreover, lacto-ovo vegetarians (consume meat and/or fish less than once a month and dairy products more than once a month) also had a lower estimated odds of hypertension (OR =0.57; 95% CI, 0.36–0.92).10 However, after adjusting for body mass index (BMI), the ORs were not statistically significant, suggesting that the effect of vegetarian diets on BP is partly mediated by the effect on BMI.
In the EPIC-Oxford study, BP was evaluated in 1,790 men and 6,873 women. Participants were allocated to four diet groups according to the answers to questions regarding their dietary habits for meat, fish, dairy products, and egg. Systolic and diastolic BPs were significantly lower in the vegan group than in any other group (meat eaters, fish eaters, lacto-ovo vegetarian) after adjustment for age. However, the relationships were not significant after adjustment for age and BMI.11 Other dietary factors, including saturated fat intake and polyunsaturated fat to unsaturated fat ratio, were associated with BP in both sexes; alcohol intake and carbohydrate intake were related to BP only in men, and calcium intake was associated with BP only in women.
The prevalence of hypertension was compared between vegetarians and omnivores in the UK Women’s Cohort Study. Vegetarians were defined as participants who ate meat or fish less than once a week, as determined using a food frequency questionnaire. Vegetarians had a lower prevalence of hypertension than meat eaters (11.4% vs 19.6%)12 and also had lower BMIs (23.3 kg/m2 vs 25.0 kg/m2) and alcohol intake (45% vs 54%).
These three cross-sectional studies, with high percentages of vegetarian participants, showed that vegetarian diets were related to not only lower prevalence of hypertension or BP but also lower BMI. After adjustment for BMI, the relationships between a vegetarian diet and BP were no longer significant in some studies. Therefore, BMI might be a very important factor for the relationship between vegetarian diets and BP. Although the results from cross-sectional studies cannot indicate causality, they might reflect the relatively longer effects of vegetarian diets.
Results from a meta-analysis
A recent meta-analysis was conducted, for which the MEDLINE and Web of Science databases were searched for articles published in English. Seven clinical trials and 32 observational studies were included. The details of the inclusion and exclusion criteria are provided elsewhere.13 An overview of the seven trials14–20 included in the meta-analysis, representing 311 participants (mean age, 44.5 years), are provided in Table 2. All the studies were open (non-masked) controlled trials conducted for 6–52 weeks (mean, 15.7 weeks). Vegan diets were examined in two trials,19,20 a lacto-vegetarian diet in one trial,16 and lacto-ovo-vegetarian diets in four trials.14,15,17,18 The intervention methods differed among the studies. For instance, Hakala and Karvetti counseled participants to follow a specific dietary pattern.16 In other studies, some food was provided for each participant to consume. Results from studies that counseled participants on diet might be useful in that they also test the ability of humans to adhere to a diet. However, studies that provided food are useful to elucidate biologic mechanisms because they ensure that the patient is exposed to the specific vegetarian dietary pattern.
The consumption of vegetarian diets was associated with a reduction in mean systolic BP (−4.8 mmHg; 95% CI, −6.6 to −3.1; P<0.001) and diastolic BP (−2.2 mmHg; 95% CI, −3.5 to −1.0; P<0.001) compared with the consumption of omnivorous diets.13 According to Whelton et al, a reduction in systolic BP of 5 mmHg resulted in a 14% overall reduction in mortality due to stroke, 9% reduction in mortality due to cardiovascular heart disease, and 7% decrease in all-cause mortality.21 Consistent results were observed in another meta-analysis of observational studies (N=21,604), in which the consumption of vegetarian diets was associated with a lower mean systolic BP (−6.9 mmHg; 95% CI, −9.1 to −4.7).13 Because of statistically significant heterogeneity in the meta-analysis of observational studies, the heterogeneous factors were examined using meta-regression. The number of men, baseline systolic and diastolic BPs, and BMI were significant, indicating that the associations between vegetarian diets and BP were stronger among men and participants with higher baseline systolic and diastolic BPs and higher BMIs.
These findings from cross-sectional studies and meta-analyses are consistent with those of a previous review of observational studies; compared with the BPs of nonvegetarians, the systolic BP of vegetarians was 3–14 mmHg lower, and diastolic BP was 5–6 mmHg lower.22 In addition, randomized controlled trials (RCTs) have shown that BP is lower when animal products are replaced with plant-based products in both normotensive and hypertensive participants.22 The Dietary Approaches to Stop Hypertension (DASH) study showed that a diet rich in vegetables and fruits reduced systolic BP by −5.5 mmHg (P<0.001) and diastolic BP by −3 mmHg (P<0.001).23 The DASH study was partly based on the observation that vegetarian diets are associated with a significantly reduced risk of hypertension.24
Possible mechanisms
Dietary pattern analysis focuses on the overall diet rather than individual nutrients. Although an approach utilizing a dietary pattern reveals the effectiveness of a real-world diet on diseases, it cannot identify the particular nutrients responsible for the disease. Therefore, Hu recommended that an observed association with a dietary pattern should be evaluated with the results from individual nutrient analyses.6 According to the Academy of Nutrition and Dietetics, the characteristics of a vegetarian dietary pattern include lower saturated fat and cholesterol levels and higher dietary fiber, magnesium, potassium, vitamins C and E, folate, carotenoid, flavonoid, and other phytochemical levels.8 In this paper, we discuss possible mechanisms of the distinctive characteristics in a vegetarian dietary pattern.
Energy intake
Particularly, the low energy intake in vegetarian diets might be attributable to the lower energy density of the diet, owing to higher fiber and lower fat content.
According to a recent meta-analysis of clinical trials, body weight decreases with the consumption of a vegetarian diet.25 Because obesity is one of the main diet-related risk factors of hypertension,9 reducing body weight could be an important intermediate variable. However, because studies controlling for body weight have still demonstrated a BP-lowering effect of vegetarian diets, weight differences do not fully explain the observed BP differences.14
Sodium
Compared with the Western diet, vegetarian diets might be lower in sodium;26,27 however, no clear differences in sodium intake between nonvegetarians and vegetarians have been reported,28 or some vegetarians have a higher sodium intake.29 Sodium intake among studies included in this paper is shown in Tables 1 and 2. Overall, sodium intake was lower in the vegetarian diets.
In a recent meta-analysis of 107 RCTs, there was a strong dose–response relationship between reduced sodium intake and BP.30 A 2.3 g reduction in sodium per day was associated with a 3.82 mmHg reduction in BP (95% CI, 3.08–4.55).30 The DASH dietary pattern also focuses on vegetable and fruit consumption; in trials that controlled sodium intake, the DASH diet had a BP-lowering effect beyond sodium reduction alone.23,31 Further studies are needed to investigate the effects of vegetarian diets, with controlled sodium intake, on BP.
Potassium
Potassium is abundant in vegetarian diets,28 and a meta-analysis of RCTs reported that potassium supplementation decreases BP.32,33 Moreover, a high potassium intake increases vasodilation and the glomerular filtration rate, while decreasing renin levels, renal sodium reabsorption, reactive oxygen species production, and platelet aggregation.34 Other minerals, such as magnesium and calcium, were inversely associated with BP in the INTERMAP (INTERnational collaborative study of MAcronutrients, micronutrients and blood Pressure) study, which was conducted in four countries (USA, UK, People’s Republic of China, and Japan).35 In a meta-analysis of magnesium supplementation, both systolic (3–4 mmHg) and diastolic (2–3 mmHg) BPs decreased.36
Protein source
The INTERMAP study suggested that plant protein intake (2.8% energy) was associated with a 2.1 mmHg reduction in systolic BP.37 Other prospective cohort studies also indicated that plant protein intake is associated with BP reduction38 or a lower risk of incident hypertension.39 A recent meta-analysis of trials that were stratified by plant protein or animal protein indicated no differences with protein from plant or animal sources.40 However, the sample size of this meta-analysis was small (three trials, N=327 for plant protein; four trials, N=574 for animal protein), and the effects of plant or animal protein were not directly compared. Hence, further intervention studies and meta-analyses are needed to understand the effects of different sources of protein on BP.
Amino acids
Previous studies have suggested that plasma concentrations and intake of amino acids were different among vegetarians and omnivores.41,42 In the INTERMAP study, glutamic acid intake was higher among those consuming predominantly plant protein, as compared with those consuming predominantly animal protein.43 A two-standard deviation higher intake of glutamic acid (4.7% of total protein) was associated with a 1.5 mmHg lower systolic BP.43 Glutamic acid is a precursor of arginine, which is itself a precursor for the vasodilator nitrous oxide (NO)44,45 and may contribute to lowering of BP.
In the EPIC-Oxford cohort, plasma amino acid concentrations were compared between vegetarians and meat eaters in 392 men, aged 30–49 years. Amino acids such as lysine, methionine, tryptophan, and tyrosine were significantly lower, and alanine and glycine were higher in vegans than in meat eaters.46 Lysine competes with arginine for transport into the cell,47,48 and arginine deficiency is associated with endothelial inflammation and immune dysfunction in humans.49 Therefore, the lysine/arginine ratio may be important in understanding the BP-lowering effect. Compared with animal protein, plant proteins contain lower lysine levels and a low lysine/arginine ratio.50 Therefore, plant protein, with a low lysine/arginine ratio, could reduce BP by stimulating NO production. A recent, small (N=30), randomized crossover trial was conducted to clarify the effect of changing the dietary lysine/arginine ratio on cardiovascular risk factors,50 by providing 30 healthy adults with a low (0.7) or high (1.4) lysine/arginine ratio diet. After 35 days of the intervention, no difference was observed in BP.50 However, the effectiveness of long-term consumption of a low lysine/arginine ratio diet has not been clarified.
A 2-year prospective cohort study (N=92) showed that dietary intake of methionine and alanine is associated with increased BP.51 Methionine is a homocysteine precursor that can increase BP by increasing the levels of asymmetric dimethylarginine – a competitive inhibitor of NO.52 Methionine is abundant in animal protein and scarce in plant protein;53 therefore, a predominantly plant-based protein diet might have a lower methionine content. A metabolic phenotyping analysis, as part of the INTERMAP study, showed that urinary alanine excretion was associated with higher BP.54 In the same study, dietary alanine was higher in people consuming a predominantly animal diet than in people ingesting a predominantly plant diet.37
Vitamin B-12
In addition to the nutrients already described, vegans and vegetarians may have lower intakes of some nutrients such as vitamin B-12, vitamin D, calcium, zinc, and long-chain n-3 fatty acids.8 Vitamin B-12 deficiency is highly prevalent in vegetarians, particularly in vegans who do not consume vitamin B-12 fortified food or supplements.55 Woo et al highlighted that, despite the protective effects of vegan diets on cardiovascular-related risk in some studies, vegan diets can have an adverse effect on arterial endothelial function and carotid intima-media thickness in Chinese vegetarians with suboptimal vitamin B-12 levels and normal or high salt intake.55 Vitamin B-12 deficiency results in increased homocysteine levels, which are related to arterial endothelial dysfunction and are an independent risk factor for cardiovascular disease.56 Pawlak suggested that vitamin B-12 deficiency may ameliorate the benefit of a vegetarian diet for cardiovascular diseases.57 Therefore, interactions with nutrients that are often deficient in some vegetarians should also be considered.
Antioxidants
Vegetables and fruits are rich in antioxidants. A 6-month RCT revealed that increased consumption of vegetables and fruits was related to increased antioxidant intake such as alpha-carotene, beta-carotene, lutein, b-cryptoxanthin, and ascorbic acid.58 In addition, when compared with a control group, the group with a higher consumption of vegetables and fruits had significantly greater reductions in systolic (−4.0 mmHg; P<0.0001) and diastolic (−1.5 mmHg; P=0.02) BPs.58
Fiber
Fiber is predominantly present in plant-based foods, and vegetarian diets have the largest amount of fiber. A recent meta-analysis of 24 RCTs revealed that dietary fiber supplementation (average dose, 11.5 g/d) reduced diastolic BP by −1.26 mmHg (95% CI, −2.04 to −0.48) and nonsignificantly reduced systolic BP by −1.13 mmHg (95% CI, −2.49 to 0.23).59 Another meta-analysis of 25 RCTs indicated that dietary fiber intake was associated with a −1.65 mmHg (95% CI, −2.70 to −0.61) reduction in diastolic BP and a nonsignificant −1.15 mmHg (95% CI, −2.68 to 0.39) reduction in systolic BP.21 The effect of dietary fiber supplementation on both systolic and diastolic BPs was stronger and more significant in hypertensive patients.21 Although data are not sufficient to determine the effectiveness of dietary fiber supplementation for the reduction in BP, dietary fiber might explain part of the effectiveness of dietary pattern interventions.
Microbiome
The human gut microbiota can rapidly change with dietary fiber supplementation60 or by excluding animal-based foods.61 The gut microbiota might contribute to the development of cardiovascular disease, including arteriosclerosis and hypertension.62 Toxic metabolites, such as p-cresol sulfate, indoxyl sulfate, and trimethylamine N-oxide (TMAO) are produced by gut microbiota through the fermentation of proteins.63–65 Previous trials showed that the average p-cresol sulfate excretion was 62% lower and average indoxyl sulfate secretion was 58% lower in participants consuming a vegetarian diet than in those consuming an omnivorous diet.66 p-Cresol sulfate and indoxyl sulfate are associated with vascular disease and mortality in patients with chronic kidney disease (CKD).67,68 The plasma TMAO concentration in patients with CKD was significantly higher than that in patients without CKD, and the plasma TMAO level was associated with a 2.8-fold increased risk of mortality. TMAO is produced by the metabolism of dietary choline, phosphatidylcholine, and l-carnitine by microbiota.64,69–71 A higher plasma TMAO level is primarily due to gut microbial action, as genes play only a minor role in determining TMAO levels in humans.72 However, a direct association between TMAO and BP has not been investigated. Recent basic research using a rat model showed that the TMAO level does not affect BP in normotensive animals, but it contributed to the hypertensive effect of angiotensin II.73
Conclusion
Although the available evidence is not sufficient for robust conclusions, the results from cross-sectional studies with a higher prevalence of vegetarian diets or meta-analyses of trials indicate that a vegetarian dietary pattern is related to a lower BP. The effectiveness of a vegetarian dietary pattern might partly be explained by weight reductions. Any dietary pattern is composed of several nutrients or foods; therefore, its effect may reflect the synergetic effects of several nutrients or foods. Further studies are needed with a higher intake of sodium or animal products in non-Western populations. In addition, we were unable to determine which vegetarian dietary pattern (eg, vegan, lacto-vegetarian, lacto-ovo vegetarian, pesco-vegetarian) is better. Studies to clarify the possible mechanisms of typical nutrients in vegetarian diets and their synergetic effects are also needed.
Acknowledgment
Financial support for this study was provided by the Nestlé Nutrition Council, Japan.
Disclosure
The authors report no conflicts of interest in this work.
References
Rosendorff C, Lackland DT, Allison M, et al; American Heart Association; American College of Cardiology; American Society of Hypertension. Treatment of hypertension in patients with coronary artery disease: a scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. J Am Coll Cardiol. 2015;65(18):1998–2038. | |
World Health Organization [webpage on the Internet]. Causes of Death 2008 [Online Database]. Geneva: World Health Organization; 2011. Available from: http://www.who.int/healthinfo/global_burden_disease/cod_2008_sources_methods.pdf. Accessed August 5, 2015. | |
World Health Organization. Global Status Report on Noncommunicable Diseases 2010. Geneva: World Health Organization; 2011. | |
National Center for Health Statistics. Health, United States, 2014: With Special Feature on Adults Aged 55–64. Hyattsville, MD: National Center for Health Statistics; 2015. | |
James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520. | |
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13(1):3–9. | |
U.S. Department of Health and Human Services [webpage on the Internet]. Scientific Report of the 2015 Dietary Guidelines Advisory Committee, Part D. Chapter 2: Dietary Patterns, Foods and Nutrients, and Health Outcomes. Available from: http://health.gov/dietaryguidelines/2015-scientific-report/07-chapter-2/. Accessed August 26, 2015. | |
Craig WJ, Mangels AR; American Dietetic A. Position of the American Dietetic Association: vegetarian diets. J Am Diet Assoc. 2009;109(7): 1266–1282. | |
Appleby PN, Key TJ. The long-term health of vegetarians and vegans. Proc Nutr Soc. Epub 2015 Dec 28. | |
Pettersen BJ, Anousheh R, Fan J, Jaceldo-Siegl K, Fraser GE. Vegetarian diets and blood pressure among white subjects: results from the Adventist Health Study-2 (AHS-2). Public Health Nutr. 2012;15(10):1909–1916. | |
Appleby PN, Davey GK, Key TJ. Hypertension and blood pressure among meat eaters, fish eaters, vegetarians and vegans in EPIC-Oxford. Public Health Nutr. 2002;5(5):645–654. | |
Cade JE, Burley VJ, Greenwood DC; UK Women’s Cohort Study Steering Group. The UK women’s cohort study: comparison of vegetarians, fish-eaters and meat-eaters. Public Health Nutr. 2004;7(7):871–878. | |
Yokoyama Y, Nishimura K, Barnard ND, et al. Vegetarian diets and blood pressure: a meta-analysis. JAMA Intern Med. 2014;174(4):577–587. | |
Rouse IL, Beilin LJ, Armstrong BK, Vandongen R. Blood-pressure-lowering effect of a vegetarian diet: controlled trial in normotensive subjects. Lancet. 1983;1(8314–8315):5–10. | |
Margetts BM, Beilin LJ, Vandongen R, Armstrong BK. Vegetarian diet in mild hypertension: a randomised controlled trial. Br Med J (Clin Res Ed). 1986;293(6560):1468–1471. | |
Hakala P, Karvetti RL. Weight reduction on lactovegetarian and mixed diets. Changes in weight, nutrient intake, skinfold thicknesses and blood pressure. Eur J Clin Nutr. 1989;43(6):421–430. | |
Kestin M, Rouse IL, Correll RA, Nestel PJ. Cardiovascular disease risk factors in free-living men: comparison of two prudent diets, one based on lactoovovegetarianism and the other allowing lean meat. Am J Clin Nutr. 1989;50(2):280–287. | |
Sciarrone SE, Strahan MT, Beilin LJ, Burke V, Rogers P, Rouse IL. Biochemical and neurohormonal responses to the introduction of a lacto-ovovegetarian diet. J Hypertens. 1993;11(8):849–860. | |
Nicholson AS, Sklar M, Barnard ND, Gore S, Sullivan R, Browning S. Toward improved management of NIDDM: a randomized, controlled, pilot intervention using a lowfat, vegetarian diet. Prev Med. 1999;29(2):87–91. | |
Ferdowsian HR, Barnard ND, Hoover VJ, et al. A multicomponent intervention reduces body weight and cardiovascular risk at a GEICO corporate site. Am J Health Promot. 2010;24(6):384–387. | |
Whelton SP, Hyre AD, Pedersen B, Yi Y, Whelton PK, He J. Effect of dietary fiber intake on blood pressure: a meta-analysis of randomized, controlled clinical trials. J Hypertens. 2005;23(3):475–481. | |
Berkow SE, Barnard ND. Blood pressure regulation and vegetarian diets. Nutr Rev. 2005;63(1):1–8. | |
Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH collaborative research group. N Engl J Med. 1997;336(16):1117–1124. | |
Sacks FM, Obarzanek E, Windhauser MM, et al. Rationale and design of the dietary approaches to stop hypertension trial (DASH). A multicenter controlled-feeding study of dietary patterns to lower blood pressure. Ann Epidemiol. 1995;5(2):108–118. | |
Barnard ND, Levin SM, Yokoyama Y. A systematic review and meta-analysis of changes in body weight in clinical trials of vegetarian diets. J Acad Nutr Diet. 2015;115(6):954–969. | |
Larsson CL, Johansson GK. Dietary intake and nutritional status of young vegans and omnivores in Sweden. Am J Clin Nutr. 2002;76(1): 100–106. | |
Clarys P, Deliens T, Huybrechts I, et al. Comparison of nutritional quality of the vegan, vegetarian, semi-vegetarian, pesco-vegetarian and omnivorous diet. Nutrients. 2014;6(3):1318–1332. | |
Rizzo NS, Jaceldo-Siegl K, Sabate J, Fraser GE. Nutrient profiles of vegetarian and nonvegetarian dietary patterns. J Acad Nutr Diet. 2013;113(12):1610–1619. | |
Woo J, Kwok T, Ho SC, Sham A, Lau E. Nutritional status of elderly Chinese vegetarians. Age Ageing. 1998;27(4):455–461. | |
Mozaffarian D, Fahimi S, Singh GM, et al; Global Burden of Diseases Nutrition and Chronic Diseases Expert Group. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371(7):624–634. | |
Sacks FM, Svetkey LP, Vollmer WM, et al; DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344(1):3–10. | |
Whelton PK, He J, Culter JA, et al. Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. JAMA. 1997;277(20):1624–1632. | |
Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ. 2013;346:f1378. | |
McDonough AA, Nguyen MT. How does potassium supplementation lower blood pressure? Am J Physiol Renal Physiol. 2012;302(9):F1224–F1225. | |
Elliott P, Kesteloot H, Appel LJ, et al; INTERMAP Cooperative Research Group. Dietary phosphorus and blood pressure: international study of macro- and micro-nutrients and blood pressure. Hypertension. 2008;51(3):669–675. | |
Kass L, Weekes J, Carpenter L. Effect of magnesium supplementation on blood pressure: a meta-analysis. Eur J Clin Nutr. 2012;66(4):411–418. | |
Elliott P, Stamler J, Dyer AR, et al. Association between protein intake and blood pressure: the INTERMAP Study. Arch Intern Med. 2006;166(1):79–87. | |
Wang YF, Yancy WS Jr, Yu D, Champagne C, Appel LJ, Lin PH. The relationship between dietary protein intake and blood pressure: results from the PREMIER study. J Hum Hypertens. 2008;22(11):745–754. | |
Alonso A, Beunza JJ, Bes-Rastrollo M, Pajares RM, Martinez-Gonzalez MA. Vegetable protein and fiber from cereal are inversely associated with the risk of hypertension in a Spanish cohort. Arch Med Res. 2006;37(6):778–786. | |
Tielemans SM, Altorf-van der Kuil W, Engberink MF, et al. Intake of total protein, plant protein and animal protein in relation to blood pressure: a meta-analysis of observational and intervention studies. J Hum Hypertens. 2013;27(9):564–571. | |
Abdulla M, Andersson I, Asp NG, et al. Nutrient intake and health status of vegans. Chemical analyses of diets using the duplicate portion sampling technique. Am J Clin Nutr. 1981;34(11):2464–2477. | |
Krajcovicova-Kudlackova M, Simoncic R, Bederova A, Babinska K, Beder I. Correlation of carnitine levels to methionine and lysine intake. Physiol Res. 2000;49(3):399–402. | |
Stamler J, Brown IJ, Daviglus ML, et al; INTERMAP Research Group. Glutamic acid, the main dietary amino acid, and blood pressure: the INTERMAP study (International collaborative study of macronutrients, micronutrients and blood pressure). Circulation. 2009;120(3):221–228. | |
Luiking YC, Engelen MP, Deutz NE. Regulation of nitric oxide production in health and disease. Curr Opin Clin Nutr Metab Care. 2010;13(1):97–104. | |
Urschel KL, Rafii M, Pencharz PB, Ball RO. A multitracer stable isotope quantification of the effects of arginine intake on whole body arginine metabolism in neonatal piglets. Am J Physiol Endocrinol Metab. 2007;293(3):E811–E818. | |
Schmidt JA, Rinaldi S, Scalbert A, et al. Plasma concentrations and intakes of amino acids in male meat-eaters, fish-eaters, vegetarians and vegans: a cross-sectional analysis in the EPIC-Oxford cohort. Eur J Clin Nutr. Epub 2015 Sep 23. | |
Luiking YC, Deutz NE. Biomarkers of arginine and lysine excess. J Nutr. 2007;137(6 Suppl 2):1662S–1668S. | |
Li X, Bazer FW, Gao H, et al. Amino acids and gaseous signaling. Amino Acids. 2009;37(1):65–78. | |
Lorin J, Zeller M, Guilland JC, Cottin Y, Vergely C, Rochette L. Arginine and nitric oxide synthase: regulatory mechanisms and cardiovascular aspects. Mol Nutr Food Res. 2014;58(1):101–116. | |
Vega-Lopez S, Matthan NR, Ausman LM, et al. Altering dietary lysine:arginine ratio has little effect on cardiovascular risk factors and vascular reactivity in moderately hypercholesterolemic adults. Atherosclerosis. 2010;210(2):555–562. | |
Tuttle KR, Milton JE, Packard DP, Shuler LA, Short RA. Dietary amino acids and blood pressure: a cohort study of patients with cardiovascular disease. Am J Kidney Dis. 2012;59(6):803–809. | |
Stuhlinger MC, Oka RK, Graf EE, et al. Endothelial dysfunction induced by hyperhomocyst(e)inemia: role of asymmetric dimethylarginine. Circulation. 2003;108(8):933–938. | |
McCarty MF, Barroso-Aranda J, Contreras F. The low-methionine content of vegan diets may make methionine restriction feasible as a life extension strategy. Med Hypotheses. 2009;72(2):125–128. | |
Holmes E, Loo RL, Stamler J, et al. Human metabolic phenotype diversity and its association with diet and blood pressure. Nature. 2008;453(7193):396–400. | |
Woo KS, Kwok TC, Celermajer DS. Vegan diet, subnormal vitamin B-12 status and cardiovascular health. Nutrients. 2014;6(8):3259–3273. | |
Homocysteine Studies C. Homocysteine and risk of ischemic heart disease and stroke: a meta-analysis. JAMA. 2002;288(16):2015–2022. | |
Pawlak R. Is vitamin B12 deficiency a risk factor for cardiovascular disease in vegetarians? Am J Prev Med. 2015;48(6):e11–e26. | |
John JH, Ziebland S, Yudkin P, Roe LS, Neil HA; Oxford Fruit and Vegetable Study Group. Effects of fruit and vegetable consumption on plasma antioxidant concentrations and blood pressure: a randomised controlled trial. Lancet. 2002;359(9322):1969–1974. | |
Streppel MT, Arends LR, van ‘t Veer P, Grobbee DE, Geleijnse JM. Dietary fiber and blood pressure: a meta-analysis of randomized placebo-controlled trials. Arch Intern Med. 2005;165(2):150–156. | |
Holscher HD, Caporaso JG, Hooda S, Brulc JM, Fahey GC Jr, Swanson KS. Fiber supplementation influences phylogenetic structure and functional capacity of the human intestinal microbiome: follow-up of a randomized controlled trial. Am J Clin Nutr. 2015;101(1):55–64. | |
David LA, Maurice CF, Carmody RN, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505(7484): 559–563. | |
Jose PA, Raj D. Gut microbiota in hypertension. Curr Opin Nephrol Hypertens. 2015;24(5):403–409. | |
Ramezani A, Raj DS. The gut microbiome, kidney disease, and targeted interventions. J Am Soc Nephrol. 2014;25(4):657–670. | |
Wang Z, Klipfell E, Bennett BJ, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011;472(7341):57–63. | |
Tuso P, Stoll SR, Li WW. A plant-based diet, atherogenesis, and coronary artery disease prevention. Perm J. 2015;19(1):62–67. | |
Patel KP, Luo FJ, Plummer NS, Hostetter TH, Meyer TW. The production of p-cresol sulfate and indoxyl sulfate in vegetarians versus omnivores. Clin J Am Soc Nephrol. 2012;7(6):982–988. | |
Barreto FC, Barreto DV, Liabeuf S, et al; European Uremic Toxin Work Group (EUTox). Serum indoxyl sulfate is associated with vascular disease and mortality in chronic kidney disease patients. Clin J Am Soc Nephrol. 2009;4(10):1551–1558. | |
Liabeuf S, Barreto DV, Barreto FC, et al; European Uraemic Toxin Work Group (EUTox). Free p-cresylsulphate is a predictor of mortality in patients at different stages of chronic kidney disease. Nephrol Dial Transplant. 2010;25(4):1183–1191. | |
Koeth RA, Wang Z, Levison BS, et al. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med. 2013;19(5):576–585. | |
Tang WH, Wang Z, Levison BS, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013;368(17):1575–1584. | |
Tang WH, Wang Z, Kennedy DJ, et al. Gut microbiota-dependent trimethylamine N-oxide (TMAO) pathway contributes to both development of renal insufficiency and mortality risk in chronic kidney disease. Circ Res. 2015;116(3):448–455. | |
Hartiala J, Bennett BJ, Tang WH, et al; CARDIoGRAM Consortium. Comparative genome-wide association studies in mice and humans for trimethylamine N-oxide, a proatherogenic metabolite of choline and L-carnitine. Arterioscler Thromb Vasc Biol. 2014;34(6):1307–1313. | |
Ufnal M, Jazwiec R, Dadlez M, Drapala A, Sikora M, Skrzypecki J. Trimethylamine-N-oxide: a carnitine-derived metabolite that prolongs the hypertensive effect of angiotensin II in rats. Can J Cardiol. 2014;30(12):1700–1705. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

