Back to Journals » International Journal of General Medicine » Volume 14
Effects of Surgical Intervention for Bone Metastases on Survival in Patients with Advanced Cancer: A Nationwide Population-Based Cohort Study
Authors Shih JT, Yeh TT, Shen PH, Wang CC, Wang SH, Chien WC, Chung CH, Wu CC
Received 20 February 2021
Accepted for publication 12 April 2021
Published 3 May 2021 Volume 2021:14 Pages 1661—1671
DOI https://doi.org/10.2147/IJGM.S307547
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Jen-Ta Shih,1,2 Tsu-Te Yeh,1 Pei-Hung Shen,1 Chih-Chien Wang,1 Sheng-Hao Wang,1 Wu-Chien Chien,3– 6 Chi-Hsiang Chung,3– 5 Chia-Chun Wu1
1Department of Orthopedics, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan; 2Graduate Institute of Injury Prevention and Control, College of Public Health, Taipei Medical University, Taipei, Taiwan; 3School of Public Health, National Defense Medical Center, Taipei, Taiwan; 4Department of Medical Research, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan; 5Taiwanese Injury Prevention and Safety Promotion Association, Taipei, Taiwan; 6Graduate Institute of Life Sciences, National Defense Medical Center, Taipei, Taiwan
Correspondence: Chia-Chun Wu
Department of Orthopedics, Tri-Service General Hospital, National Defense Medical Center, No. 325, Sec. 2, Chenggong Road, Neihu Dist, Taipei City, 11472, Taiwan
Tel +886-953-086-492
Fax +886-2-8792-7186
Email [email protected]
Purpose: With recent advances in surgical techniques and instruments, orthopedic surgeons are better equipped to treat metastatic bone disease. There has also been considerable progress in the non-surgical treatment of cancers, specifically in improving the survival rate of patients with advanced cancer. However, it remains unclear whether surgical resection of a metastatic bone lesion poses additional risk to the survival of patients with advanced cancer.
Patients and Methods: This study utilized data from the National Health Insurance Research Database (NHIRD) in Taiwan between 2000 and 2015. Patients aged ≥ 18 years, who had been recently diagnosed with bone metastases (BM), were enrolled and assigned to either the surgery or non-surgery groups. The demographic characteristics were analyzed, and the adjusted hazard ratios (aHR) of mortality were calculated using Cox regression analysis.
Results: Of the 4,549,226 individuals in the inpatient database of the NHIRD, 83,536 patients with BM were enrolled in this study. Among them, 8802 underwent surgical resection for skeletal metastatic lesion and 66,098 did not. Altogether, 28,691 patients died, including 2798 (31.8%) in the surgery group and 25,893 (39.2%) in the non-surgery group. The aHR for mortality was 0.7-fold lower in the surgery group (p < 0.001).
Conclusion: This study demonstrates that surgical resection of metastatic bone lesions did not pose any additional risk to survival outcomes. Thus, we believe that surgery, if indicated, could have a competitive role in the management of metastatic bone disease.
Keywords: bone metastasis, surgical resection, mortality, bone resorption inhibitor
Introduction
Bone metastases (BM) is a devastating condition that adversely affects the lives of patients with advanced cancer. Patients may experience limitations in the activities of daily living, decreased quality of life (QOL), threat to survival, and increased medical expenses. Management of skeletal metastatic disease has attracted increasing attention in the last few years. In the past, 50% of patients with cancer would die within 6 months of surgery owing to a pathologic fracture or paraplegia due to spinal metastases.1 Most surgeons hesitate to perform surgical resection for cancer patients with BM despite the poor QOL, owing to comorbidities and limited life expectancy. Currently, with the advancement of surgical techniques and instruments, orthopedic surgeons are better equipped to restore function in cancer patients with skeletal complications. Further, systemic treatment of cancers, such as chemotherapy and targeted therapy, has contributed to the increased survival rate of patients with advanced cancer. Recently, the number of breast and colorectal cancer survivors has increased globally. In numerous countries, the 5-year survival rate for prostate cancer is > 95%.2
Better management of the primary cancer increases the survival rate of patients; hence, there is an increased demand for surgical intervention to treat metastatic bone lesions. However, the risks and possible complications associated with surgery may have a negative effect on the patient’s health. It is also unclear whether surgical resection of metastatic bone lesions is an additional risk factor in the overall survival outcomes of patients with advanced cancer. In fact, the reported survival rates vary widely between different studies because of the difference in primary tumor selection.3,4 Studies that have demonstrated survival rates of patients presenting with BM from a variety of primary tumors with short-term follow-up also showed heterogeneous results.5,6 Thus, this study aimed to conduct a long-term investigation on the difference in mortality rates between patients who underwent surgical resection for skeletal metastases and those who did not, while considering sex, age, comorbidities, and use of bone resorption inhibitors (BRIs).
Patients and Methods
Database
We analyzed all the inpatient data included in Taiwan’s National Health Insurance Research Database (NHIRD), which was established in 1995. The health insurance system in Taiwan enrolls > 99% of the population (around 23,000,000 insurants per year). Cancer with BM was considered to be in the advanced stage; therefore, most patients were hospitalized for medical treatment. The study data was obtained from January 1, 2000 (index date) to December 31, 2015. The composition and characteristics of the individuals were normally distributed.
Study Design, Patients, and Ethics
We used the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) coding system to identify diagnoses and related procedures. BM was defined as ICD-9-CM code 198.5, corresponding to the following ICD-9-CM codes for primary cancer, eg, ICD-9-CM: 162 for lung cancer, ICD-9-CM: 174 for breast cancer, and ICD-9-CM: 185 for prostate cancer. Patients with BM before the index date, those who were lost to follow-up, those with unknown sex information, and pediatric patients (< 18 years old) were excluded from the study. Surgical resection for skeletal metastases was defined using the National Health Insurance order code, 64204B and 64205B for wide excision of malignant bone tumors. The use of BRIs, such as zoledronic acid, pamidronate disodium, clodronate tetrahydrate, and denosumab, was also analyzed. The utilization of NHIRD data was legally authorized and complies with relevant data protection and privacy regulations. The study protocol was approved by Institutional Review Board of the Tri-Service General Hospital (approval No. B202005037).
Comorbidities
The following comorbidities and associated complications were assessed using the corresponding ICD-9-CM codes: hypertension (HTN, ICD-9-CM: 401–405), diabetes mellitus (DM, ICD-9-CM: 250), chronic obstructive pulmonary disease (COPD, ICD-9-CM: 490–496), chronic kidney disease (CKD, ICD-9-CM: 585), ischemic heart disease (IHD, ICD-9-CM: 410–414), congestive heart disease (CHD, ICD-9-CM: 428–429), stroke (ICD-9-CM: 430–438), pneumonia (ICD-9-CM: 480–486), injury (ICD-9-CM: 800–999), hyperthyroidism (ICD-9-CM: 242), liver disease (ICD-9-CM: 571), depression (ICD-9-CM: 296.2–296.3, 300.4, 311), and sepsis (ICD-9-CM: 003.1, 036.1, 038). All presented ICD-9-CM codes and National Health Insurance order codes are displayed in the appendix (Table S1).
Statistics
Statistical analysis was performed using SPSS software, version 22 (IBM Corp., Armonk, N.Y., USA). The chi-square and Fisher’s exact tests were used to compare categorical variables and the t-test was used to compare continuous variables between the surgery and non-surgery groups. Kaplan–Meier curve analysis and the Log rank test was employed to demonstrate the cumulative risk of mortality. The adjusted hazard ratios (aHRs) of mortality and other covariates of interest were calculated using multivariate Cox regression analysis. A p-value < 0.001 was considered statistically significant.
Results
Of the 4,549,226 individuals in the inpatient database of NHIRD, 83,536 patients with BM were enrolled in this study. On applying the exclusion criteria, 8636 patients were excluded. Thus, 74,900 patients were selected for subsequent analysis; all were at least 18 years old and had BM that was recently diagnosed between 2000 and 2015. Among these, 8802 patients underwent surgical resection for skeletal metastatic lesion and 66,098 did not. At the end of the follow-up period, a total of 28,691 patients died: 2798 (31.8%) in the surgery group and 25,893 (39.2%) in the non-surgery group. The research algorithm is presented in Figure 1.
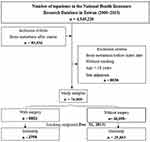 |
Figure 1 Flowchart of the study design and participant selection. |
The final study participants were divided into two groups: “surgery” and “non-surgery.” Patient characteristics included sex, age, the location of BM, length of hospital stay, adjunctive radiotherapy and chemotherapy, distribution of hospital levels, comorbidities, and the use of BRIs (Table 1). Most patients with BM (> 50%) were aged ≥ 65 years in both the surgery and non-surgery groups. We divided the patients into the following three age subgroups: 18–44 years, 45–64 years, and ≥ 65 years; the distribution of patients in each subgroup was similar in both groups. However, patients in the surgery group were significantly older. There were more male patients than female patients enrolled in this study (52.4% versus 47.6%) and in the non-surgery group (53.2% versus 46.8%); however, the number of male patients was lower than that of female patients in the surgery group (46% versus 54%). According to the location of BM, we also divided the patients into the following three subgroups: axial skeleton, appendicular skeleton, and multiple sites. There was significant difference in the composition between the surgery and non-surgery groups. The non-surgery group included more patients with multiple sites of BM than the surgery group (90.8% versus 65.5%). Several differences in the accompanying comorbidities were found: the prevalence of HTN, DM, IHD, CHD, injury, liver disease, and depression was higher in the surgery group, while that of pneumonia was higher in the non-surgery group. No significant difference in the prevalence of COPD, CKD, stroke, hyperthyroidism, and sepsis was observed. Overall, accompanying comorbidities were more prevalent in the surgery group. The proportion of patients using BRIs (except for denosumab) was significantly higher in the non-surgery group.
 |
Table 1 Patient Characteristics Based on the Longitudinal Health Insurance Database |
The follow-up period from surgery to death ranged from 1 to 15 years. Kaplan–Meier curves of survival for the surgery and non-surgery groups are shown in Figure 2. A significant difference in survival was noted based on the Log rank test (p < 0.001). Most deaths that occurred during the study period were within 5 years of surgery, and particularly within the first year. The number of surgeries for BM by years of follow-up are shown in Figure 3. It exhibits an upward trend over the study period. After adjustment for sex, age, and comorbidities using multivariate Cox regression analysis, the aHRs of surgery, sex, age subgroups, and comorbidities were identified (Table 2). The aHR of mortality was significantly lower in the surgery group than in the non-surgery group (aHR = 0.7, p < 0.001). As expected, old age and comorbidities were associated with a higher aHR or mortality. None of the BRIs had significant influence on the aHR of mortality.
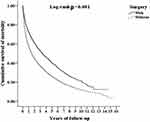 |
Figure 2 Kaplan–Meier curves for cumulative survival and the Log rank test. The inpatients with bone metastases were aged ≥ 18 years and stratified by whether they underwent surgery. |
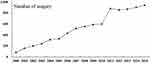 |
Figure 3 The number of surgeries done for BM by years of follow-up presents an upward trend. |
We also performed a stratified analysis for sex, age subgroups, each comorbidity, and certain cancers to compare the aHRs of mortality between the surgery and non-surgery groups (Table 3). Results were comparable between all age subgroups, sexes, and when the analysis was restricted to certain comorbidities and cancers. Patients with skeletal metastases who underwent surgical resection were at no extra risk of death when compared with those who did not.
 |
Table 3 Factors for Mortality Stratified by Sex, Age Groups, Comorbidities, and Certain Cancers Based on Multivariate Cox Regression Analysis |
 |
Table 2 Factors for Mortality Based on Multivariate Cox Regression Analysis |
Discussion
In this study, we performed a large-scale investigation using data from the NHIRD. The results demonstrated that the overall mortality is lower in the surgery group than in the non-surgery group; moreover, the surgery group is associated with a significantly lower risk of mortality (aHR = 0.7) than the non-surgery group after adjustment for sex, age, and comorbidities. The stratified analysis in our study also demonstrated that the risk of mortality in the surgery group decreased consistently in certain cancers and each comorbidity subgroup, except in those of hyperthyroidism and sepsis. These findings could be attributed to the following: first, the goals of surgery for BM include local tumor control, providing structural stability, and restoration of function; therefore, patients in the surgery group may have had a better QOL and ability to perform daily functions, which possibly protected them from the risk of mortality due to diseases other than their primary cancer. Second, the patients possibly had good control of the primary malignancy and a relatively healthy status. Thus, they were willing to undergo surgery, or were suitable for surgery, thereby leading to a better prognosis. The location of BM also played a significant role. Surgeons tend to operate on lesions that are solitary, surgically accessible, and could cause less morbidity post-operatively. Up to 98.9% of patients in the non-surgery group had BM of the axial skeleton or multiple sites, while that for patients in the surgery group was 93.5%. Hence, there may have been a bias in selection. Even so, with the advancement of medical instruments and surgical techniques, the location of lesions may not be a limiting factor. The trend of surgery for BM has increased steadily in the present study (Figure 3). In our study, comorbidities (except for pneumonia and sepsis) were more prevalent in the surgery group. Additionally, the average age of the patients in the surgery group was higher than that of those in the non-surgery group. There was no evidence that patients in the surgery group had better health status than those in the non-surgery group.
There have been numerous studies attempting to investigate the prognostic factors among patients with BM and identify candidates suitable for surgery. In a previous prospective study, pathological fracture, visceral metastases, hemoglobin < 7 mmol/L, and lung cancer were identified as independent negative prognostic factors for 1-year survival. Myeloma was the only positive factor identified, based on the skeletal metastasis registry of the Scandinavian Sarcoma Group.6 Recently, non-surgical treatments, such as targeted therapy (eg, gefitinib for epidermal growth factor receptor mutant non-small cell lung cancer), have improved the survival of cancer patients,7 with pertuzumab and trastuzumab increasing the median overall survival of patients with HER2-positive metastatic breast cancer.8 Evidence of prolonged survival time after surgery may change the attitude of both surgeons and patients towards surgical intervention, leading to an increased demand for surgery, particularly in cases with BM. Although a cure for metastatic bone disease remains a challenge, our study shows that surgery produces promising results.
Surgical strategies for BM must be individualized. For spinal metastases of breast cancer or prostate cancer, hormone therapy or radiotherapy is usually the first line of treatment before surgery.9,10 However, total en bloc spondylectomy may be beneficial when the lesion is solitary, and a long survival time is expected.11 Nonetheless, operative methods for spinal metastases differ according to the sites and sizes of metastases. After the axial skeleton, the pelvic bone is the second most common site of BM.12 Pelvic bone surgery is a demanding operation both for the surgeons and the patients. A retrospective study of 83 patients who underwent surgery for metastases to the pelvis concluded that primary cancer type, serum albumin level, and visceral metastases influence survival.13 Considering that no standard procedures have been established, en bloc resection is generally performed with the intent to reduce tumor burden and cure patients with solitary metastases at accessible sites. Moreover, surgery is also beneficial for the repair of mechanical instability, pain relief, and the improvement of limb function and QOL in pathological long bone fractures.14,15 However, a retrospective study showed that the surgical outcomes, including blood loss, period of hospitalization, and recovery of function, are better for at-risk fractures than for pathologic fractures.16 Operative methods include internal fixation and prosthesis replacement.
Studies have shown that BRIs provide clinical benefits to patients with BM.17,18 To date, zoledronic acid is the most promising bisphosphonate, while denosumab is another potent agent that prevents bone destruction. However, these agents are associated with adverse events, such as osteonecrosis of the jaw, renal toxicities, and hypocalcemia.19,20 In our study, the proportion of patients using zoledronic acid, pamidronate disodium, and clodronate tetrahydrate was significantly lower in the surgery group than in the non-surgery group; however, there was no difference in the use of denosumab between the groups. This finding could be attributed to the requirement of BRIs in the non-surgery group since most patients had multiple BMs that could not be resolved by surgery, while most patients in the surgery group had solitary or oligometastatic disease. Moreover, surgery for BM may decrease the need for BRIs. Nevertheless, the administration of BRIs did not show a significant influence on mortality after adjustment for age, sex, surgery, and comorbidities.
This study has several limitations. First, the severity of the patients’ disease could not be determined from the database. Even among patients with the same primary tumor and BM, the severity may still differ, particularly since some patients may have solitary BM while others may have multiple BM, with or without visceral metastases. Thus, this study focused on all-cause mortality rather than cancer-related mortality to minimize the confounding effect of these variables. Second, other treatments performed for BM, such as radiotherapy, chemotherapy, targeted therapy, and local ablation/cryoablation, might have influenced patient survival. Based on the results, the percentage of patients receiving radiotherapy or chemotherapy was higher in the surgery group than in the non-surgery group (83.1% versus 78.6%). The trends for cancer management were multidisciplinary. However, it was difficult to match individual courses of treatment in this study. We therefore selected lung, breast, and prostate cancer as subgroups, which are known for their strong association with BM. Most patients within the same cancer subgroup might have undergone similar non-surgical treatments (eg, chemotherapy and hormonal therapy) in the therapeutic protocols. There was no significant difference in the distribution of hospital levels between both groups, implying that the quality of treatment and care might be similar. Third, the socioeconomic and educational status of patients were not recorded in the database. Thus, we were unable to determine the extent to which this confounding factor influenced our results, given that the cost associated with surgical treatment is high. Nevertheless, most medical procedures were included in the National Health Insurance of Taiwan and were thus affordable (universal health coverage in Taiwan is > 99%).21 Finally, surgical outcomes were not only related to survival but also the health status of the survivors, including post-operative morbidities, the length of hospital stay, and discharge destination. In the present study, it was difficult to define post-operative complications in the database owing to the variety in timing, situation, duration, and influence. Coincidentally, the discharge destination code had not been established in the database. However, during the study period, the surgery group did not surpass the non-surgery group in the average length of hospital stay. It seemed that surgery had not elongated hospital stay, despite possible surgical complications. These focused issues require further investigation in the future studies.
Conclusion
To the best of our knowledge, this is the first nationwide cohort study investigating the effect of surgical intervention for BM on mortality in advanced cancer. Unique strengths of the study are the inclusion of a demographically broad population, a follow-up period substantially longer than that in previously published outcome studies, and an insight into the effect of surgical intervention for BM stratified by various subgroups.
This study, involving a large cohort of cancer patients with BM, revealed that surgical treatment had not resulted in any additional risk on survival, regardless of age, sex, certain cancer types, and comorbidities. Further, this study has the potential to reduce the use of BRIs. Although there are multiple factors that can influence the survival rate of cancer patients with BM, we believe surgical resection could have a competitive role in the management of metastatic bone disease if applied properly, and the management of BM will continue to improve.
Abbreviations
NHIRD, National Health Insurance Research Database; BM, bone metastases; aHR, adjusted hazard ratios; QOL, quality of life; BRI, bone resorption inhibitor; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; HTN, hypertension; DM, diabetes mellitus; COPD, chronic obstructive pulmonary disease; CKD, chronic kidney disease; IHD, ischemic heart disease; CHD, congestive heart disease.
Data Sharing Statement
The original data can be obtained exclusively under the authorization of NHIRD.
Acknowledgments
We appreciate the Health and Welfare Data Science Center, Ministry of Health and Welfare (HWDC, MOHW), Taiwan, for providing the National Health Insurance Research Database (NHIRD). We also thank Elsevier Language Editing Services for the English language editing.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Tri-Service General Hospital Research Foundation (TSGH-B-110012), and the sponsor had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bauer HC. Controversies in the surgical management of skeletal metastases. J Bone Joint Surg Br. 2005;87(5):608–617. doi:10.1302/0301-620X.87B5.16021
2. Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023–1075.
3. Ratasvuori M, Wedin R, Hansen BH, et al. Prognostic role of en-bloc resection and late onset of bone metastasis in patients with bone-seeking carcinomas of the kidney, breast, lung, and prostate: SSG study on 672 operated skeletal metastases. J Surg Oncol. 2014;110(4):360–365. doi:10.1002/jso.23654
4. Hansen BH, Keller J, Laitinen M, et al. The Scandinavian Sarcoma Group skeletal metastasis register. Survival after surgery for bone metastases in the pelvis and extremities. Acta Orthop Scand. 2004;75(Suppl 311):11–15. doi:10.1080/00016470410001708270
5. Camnasio F, Scotti C, Peretti GM, Fontana F, Fraschini G. Prosthetic joint replacement for long bone metastases: analysis of 154 cases. Arch Orthop Trauma Surg. 2008;128(8):787–793. doi:10.1007/s00402-007-0464-y
6. Sarahrudi K, Greitbauer M, Platzer P, Hausmann JT, Heinz T, Vécsei V. Surgical treatment of metastatic fractures of the femur: a retrospective analysis of 142 patients. J Trauma. Acute Care Surg. 2009;66(4):1158–1163. doi:10.1097/TA.0b013e3181622bca
7. Lee CK, Davies L, Wu YL, et al. Gefitinib or erlotinib vs chemotherapy for EGFR mutation-positive lung cancer: individual patient data meta-analysis of overall survival. J Natl Cancer Inst. 2017;109(6). doi:10.1093/jnci/djw279.
8. Swain SM, Clark E, Baselga J. Treatment of HER2-positive metastatic breast cancer. N Engl J Med. 2015;372(20):1964–1965. doi:10.1056/NEJMoa1413513
9. Patchell RA, Tibbs PA, Regine WF, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366(9486):643–648. doi:10.1016/S0140-6736(05)66954-1
10. Feiz-Erfan I, Rhines LD, Weinberg JS. The role of surgery in the management of metastatic spinal tumors. Semin Oncol. 2008;35(2):108–117. doi:10.1053/j.seminoncol.2007.12.005
11. Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976). 2001;26(3):298–306. doi:10.1097/00007632-200102010-00016
12. Kakhki VR, Anvari K, Sadeghi R, Mahmoudian AS, Torabian-Kakhki M. Pattern and distribution of bone metastases in common malignant tumors. Nucl Med Rev Cent East Eur. 2013;16(2):66–69. doi:10.5603/NMR.2013.0037
13. Krishnan CK, Han I, Kim HS. Outcome after surgery for metastases to the pelvic bone: a single institutional experience. Clin Orthop Surg. 2017;9(1):116–125. doi:10.4055/cios.2017.9.1.116
14. Talbot M, Turcotte RE, Isler M, Normandin D, Iannuzzi D, Downer P. Function and health status in surgically treated bone metastases. Clin Orthop Relat Res. 2005;438:215–220. doi:10.1097/01.blo.0000170721.07088.2e
15. Wedin R, Hansen BH, Laitinen M, et al. Complications and survival after surgical treatment of 214 metastatic lesions of the humerus. J Shoulder Elbow Surg. 2012;21(8):1049–1055. doi:10.1016/j.jse.2011.06.019
16. Johnson SK, Knobf MT. Surgical interventions for cancer patients with impending or actual pathologic fractures. Orthop Nurs. 2008;27(3):160–171. doi:10.1097/01.NOR.0000320543.90115.d5
17. Vadhan-Raj S, von Moos R, Fallowfield LJ, et al. Clinical benefit in patients with metastatic bone disease: results of a Phase 3 study of denosumab versus zoledronic acid. Ann Oncol. 2012;23(12):3045–3051. doi:10.1093/annonc/mds175
18. Scagliotti GV, Hirsh V, Siena S, et al. Overall survival improvement in patients with lung cancer and bone metastases treated with denosumab versus zoledronic acid: subgroup analysis from a randomized phase 3 study. J Thorac Oncol. 2012;7(12):1823–1829. doi:10.1097/JTO.0b013e31826aec2b
19. Stopeck AT, Lipton A, Body JJ, et al. Denosumab compared with zoledronic acid for the treatment of bone metastases in patients with advanced breast cancer: a randomized, double-blind study. J Clin Oncol. 2010;28(35):5132–5139. doi:10.1200/JCO.2010.29.7101
20. Bamias A, Kastritis E, Bamia C, et al. Osteonecrosis of the jaw in cancer after treatment with bisphosphonates: incidence and risk factors. J Clin Oncol. 2005;23(34):8580–8587. doi:10.1200/JCO.2005.02.8670
21. Lu JR, Chiang TL. Developing an adequate supply of health services: taiwan’s path to universal health coverage. Soc Sci Med. 2018;198:7–13. doi:10.1016/j.socscimed.2017.12.017
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
